ABSTRACT
Langerhans cell histiocytosis frequently manifests as lesions of the skull. The disease can present with a wide spectrum of forms, from an isolated eosinophilic granuloma to multiple lesions with diffuse systemic involvement. The authors report the case of a 12-year-old boy with a 1-month history of left temporal and periorbital pain and headaches. Noncontrast computed tomography of the head was done at the time of initial presentation and was interpreted as normal. Over the next month, the patient continued to have headaches and periorbital swelling and began having bloody discharge from his nose. Magnetic resonance imaging of the brain ordered by his pediatrician showed a lesion in the left infratemporal fossa, left orbit, and sphenoid bone. The lesion was biopsied and confirmed to be Langerhans cell histiocytosis. We describe a novel multidisciplinary approach for treatment of this tumor.
Keywords: Langerhans cell histiocytosis, eosinophilic granuloma, skull base tumor
Langerhans cell histiocytosis (LCH) includes a spectrum of lesions, ranging from the most common eosinophilic granuloma to forms with more extensive and systemic involvement.1,2 Although the pathogenesis of LCH is undetermined, the disease is likely a disorder of immune regulation, as evidenced by the presence of other immunologically active cells within the lesions in addition to the increased cytokines.1,3 Conversely, Langerhans cell histiocytes are monoclonal, implying that a neoplastic process cannot be ruled out.1 LCH usually manifests before puberty, and the skull is the most frequent site of involvement (60 to 80% of cases), although any bone may be involved. Multifocal involvement is seen in 20% of cases. LCH lesions may cause pain and adjacent soft-tissue swelling, but some lesions are asymptomatic. The most common presentation is a painful, immobile scalp mass that may have recently enlarged.
Radiographically these lesions appear as a classic “punched-out” or centrally destructive lesion within the diploic space without sclerotic margins on plain X-ray.4 Computed tomography (CT) is useful in providing anatomic detail with reconstruction algorithms. Magnetic resonance (MR) imaging may be useful to demonstrate the extent of intracranial involvement.2,4,5 Bone scintigraphy is recommended at diagnosis and on follow-up examination to reveal any additional sites of active disease, especially when the involvement is polyostotic.4
The histological diagnosis of LCH is based on the presence of Langerhans cells seen with light microscopy, in addition to other features including positive staining for protein S-100. An important characteristic is positive CD1a antigen staining with or without the appearance of intracytoplasmic organelles or Birbeck granules on electron microscopy.1,2,4 Complete resection is the traditional treatment of unifocal histiocytosis.
We report a case of a 12-year-old boy with a rapidly progressive LCH lesion of the left orbit and skull base. This report details a unique multidisciplinary approach to treatment of the patient utilizing the expertise of the pediatric neurosurgery, otolaryngology, and oncology teams.
CASE REPORT
A 12-year-old boy presented to the emergency room with a 1-week history of left temporal and periorbital pain and headaches. He reported no other neurological symptoms and his physical examination was normal. A noncontrast head CT study was done at that time and was read as negative (Fig. 1). Over the next month, the patient continued to have headaches and swelling around his left eye and began having bloody discharge from his nose. This prompted his pediatrician to order MR imaging of the brain and request pediatric neurosurgical consultation. On examination, the patient was otherwise healthy and taking only acetaminophen and ibuprofen for his headaches. He again denied neurological or constitutional symptoms. His examination at this time revealed periorbital and left temporal region swelling with significant tenderness to palpation. His vision and extraocular movements were intact. CT imaging of the head with coronal reconstructions was repeated and revealed a 3.2- × 3.7-cm mass within the greater wing of the left sphenoid bone and lateral wall of the left sphenoid sinus. The mass abutted the left lateral rectus muscle, left temporal lobe, and cavernous sinus and extended into the left pterygopalatine fossa (Fig. 2). MR imaging revealed a homogeneously contrast-enhancing extra-axial mass near the left temporal tip, eroding into the sphenoid sinuses and left lateral orbit (Fig. 3). There was a clear plane between the mass and the left temporal tip, left orbit, and left cavernous sinus.
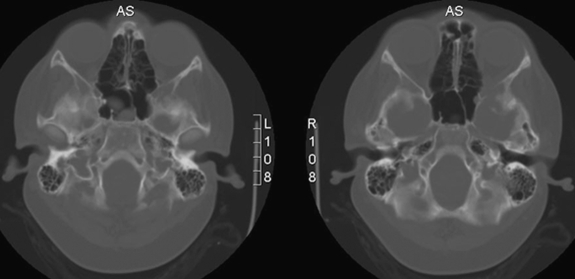
Figure 1.
Initial noncontrast axial head computed tomography (CT) bone windows show only minimal destruction of the left lateral orbital wall. This CT was initially interpreted as negative for any lesions when the patient presented with left temporal and periorbital pain.
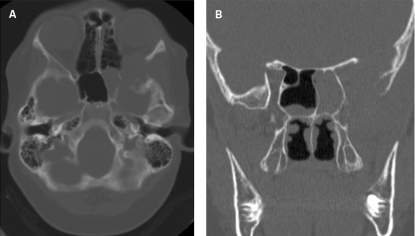
Figure 2.
(A) Axial and (B) coronal computed tomography scans obtained 1 month later show an expansile lesion with destruction of the left lateral orbit and sphenoid sinuses.
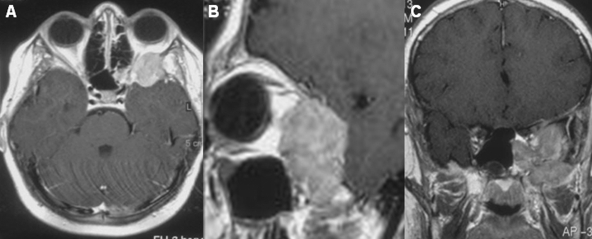
Figure 3.
Preoperative magnetic resonance imaging of the brain. (A) Axial, (B) sagittal, and (C) coronal T1 gadolinium-enhanced images show an enhancing lesion in the left infratemporal fossa with extension into the left orbit and sphenoid sinuses.
Physicians on the otolaryngology, neuroradiology, and oncology services were consulted for a multidisciplinary approach to the tumor. The tumor was initially thought most likely to be a rhabdomyosarcoma, and therefore biopsy was thought to be the most reasonable first step in management of the patient. The otolaryngologists performed the initial biopsy through a left Caldwell-Luc, transmaxillary approach; the initial pathological diagnosis was LCH. Therefore, the oncologists performed a complete work-up, including an osseous survey and CT imaging of the patient's chest, abdomen, and pelvis regions. This work-up revealed no additional lesions.
One week after the initial biopsy, the patient underwent a left subtemporal and middle fossa approach for tumor resection by the neurosurgeons, in conjunction with the otolaryngologists. A pterional craniotomy was performed with additional bone removal to unroof the middle fossa completely. Tumor was immediately observed within the sphenoid bone. The mass was found to be completely extradural but was encasing the contents of the superior orbital fissure, lateral orbital wall, left carotid artery, and left second and third divisions of the trigeminal nerve. The tumor was removed in piecemeal fashion from around all of the normal anatomical structures. Once most of the intracranial resection was complete, the otolaryngologist performed a transmaxillary-transfacial approach to the middle cranial fossa and endoscopic sphenoidectomy for further tumor resection. Near the end of the procedure, concurrent dissection by the otolaryngologist from below and the neurosurgeon from above aided in confirming anatomic landmarks and assured complete resection of the tumor (Fig. 4). The final pathological diagnosis of the tumor after the resection was LCH (Fig. 5).
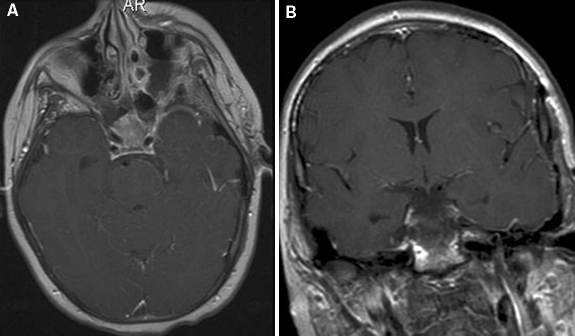
Figure 4.
(A) Axial and (B) coronal postoperative enhanced magnetic resonance imaging of the brain shows gross total resection of the intracranial portion of the tumor and tumor within the sphenoid sinuses and lateral orbit.
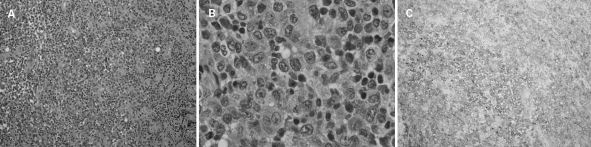
Figure 5.
Histological sections show sheets of histiocytoid mononuclear cells with moderate amounts of eosinophilic cytoplasm and pale staining nuclei. Occasional foamy histiocytes and scattered multinucleated giant cells and reniform nuclei are visible. (A) Hematoxylin and eosin (H & E) staining at × 20; (B) H & E staining at × 100; (C) CD1a staining at × 20 shows strong membranous staining of histiocytic cells.
The patient tolerated surgery well, without neurological deficit and with good recovery. After a short hospital stay, he began his chemotherapy and radiation treatment. Follow-up MR imaging obtained 3 months after surgery showed no local recurrence. The patient will continue to undergo serial imaging at 3-month intervals for a year.
DISCUSSION
This case illustrates the utility of a multidisciplinary approach for treatment of skull base lesions. At initial presentation, the most likely diagnosis, based on imaging and symptomatology, was rhabdomyosarcoma, which is seen more frequently by otolaryngologists. These tumors are typically treated by biopsy for diagnosis, followed by chemotherapy and radiation, with resection reserved only for residual tumor.6 Although rhabdomyosarcoma was high on our differential diagnosis, other lesions that manifest as rapidly progressive facial pain and swelling also include LCH, Ewing's sarcoma, osteogenic sarcoma, and metastatic neuroblastoma.7 Therefore, the otolaryngology staff began the work-up with biopsy of the lesion, from which an initial histological diagnosis of LCH was made. This lesion was thought to be aggressive because of the rapid progression of bony erosion as evidenced on CT imaging, and the pediatric oncologists were helpful in completing further work-up and discussing management options before resection was undertaken. Once it was determined that this lesion was isolated, it was decided by all physicians that surgery with the goal of gross total excision would be the first step in treating the lesion. This decision was made based on the fact that the lesion was symptomatic, rapidly progressive, intracranial, encroaching upon multiple cranial nerves, and surgically accessible.
The decision to resect the lesion with the assistance of the otolaryngologists was based on the regional anatomy affected by the tumor. It was clear that the tumor extending within the sphenoid bone and sphenoid sinuses could not be reached via the intracranial exposure. Moreover, at the time of surgery, the view offered by the endoscopic sphenoidectomy was pivotal in ensuring that the entire tumor had been removed from nearby structures, including the carotid artery and maxillary branch of the trigeminal nerve.
The natural history of LCH is poorly understood. In fact, spontaneous regression has been well reported and, therefore, the relative benefit of any of the treatment modalities including surgery, radiation, or chemotherapy has not been fully elucidated.7 However, recurrences and more aggressive courses have also been well described.
Treatment of unifocal bone lesions of the skull typically consists of complete resection of the lesion with clean margins. Local recurrence rate is ~6% and new lesions present in ~22% of patients.5 Most recurrences are seen within 2 years of treatment of solitary bone lesions.
Intralesional injection of corticosteroids has been reported to be successful. In 2004, Harris and Woo8 reviewed a series of seven patients with LCH of the orbit. Two patients were treated with biopsy and low-dose radiation and five patients had subtotal curettage at the time of biopsy; four of five received simultaneous intralesional corticosteroid injection. All of the lesions in the study were isolated, and no local recurrence or additional focus was noted in follow-up periods of 1 to 17 years.
Patients with multiple lesions or organ system involvement and those younger than 2 years of age are considered at high risk for disease recurrence, and those with multifocal, recurrent, or progressive disease may be treated with low-dose radiation or chemotherapy.9
The patient in our report presented a unique challenge in that he had intracranial extension with cranial nerve involvement as well as a radiographically documented rapid progression of the lesion over a 1-month interval. These factors suggested cause for concern and resulted in the decision to undertake more aggressive treatment, which included complete surgical excision and postoperative radiation and chemotherapy.
ACKNOWLEDGMENTS
The authors thank Kristin Kraus for her assistance in the editorial preparation of this article.
REFERENCES
- Leonidas J C, Guelfguat M, Valderrama E. Langerhans' cell histiocytosis. Lancet. 2003;361:1293–1295. doi: 10.1016/S0140-6736(03)12990-X. [DOI] [PubMed] [Google Scholar]
- Winn H. In: Winn H, Dacey R, editor. Youmans Neurological Surgery. 5th ed. Philadelphia: Elsevier; 2004. Benign tumors of the skull including fibrous dysplasia. pp. 3719–3720.
- Egeler R M, Annels N E, Hogendoorn P C. Langerhans cell histiocytosis: a pathologic combination of oncogenesis and immune dysregulation. Pediatr Blood Cancer. 2004;42:401–403. doi: 10.1002/pbc.10464. [DOI] [PubMed] [Google Scholar]
- Azouz E M, Saigal G, Rodriguez M M, Podda A. Langerhans' cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol. 2005;35:103–115. doi: 10.1007/s00247-004-1262-0. [DOI] [PubMed] [Google Scholar]
- Stromberg J S, Wang A M, Huang T E, Vicini F A, Nowak P A. Langerhans cell histiocytosis involving the sphenoid sinus and superior orbital fissure. AJNR Am J Neuroradiol. 1995;16(suppl):964–967. [PMC free article] [PubMed] [Google Scholar]
- Callender T A, Weber R S, Janjan N, et al. Rhabdomyosarcoma of the nose and paranasal sinuses in adults and children. Otolaryngol Head Neck Surg. 1995;112:252–257. doi: 10.1016/S0194-59989570246-6. [DOI] [PubMed] [Google Scholar]
- Khanna G, Sato Y, Smith R J, Bauman N M, Nerad J. Causes of facial swelling in pediatric patients: correlation of clinical and radiologic findings. Radiographics. 2006;26:157–171. doi: 10.1148/rg.261055050. [DOI] [PubMed] [Google Scholar]
- Harris G J, Woo K I. Eosinophilic granuloma of the orbit: a paradox of aggressive destruction responsive to minimal intervention. Trans Am Ophthalmol Soc. 2003;101:93–103. discussion 103–105. [PMC free article] [PubMed] [Google Scholar]
- Jubran R F, Marachelian A, Dorey F, Malogolowkin M. Predictors of outcome in children with Langerhans cell histiocytosis. Pediatr Blood Cancer. 2005;45:37–42. doi: 10.1002/pbc.20364. [DOI] [PubMed] [Google Scholar]