ABSTRACT
Inflammatory pseudotumor is a non-neoplastic inflammatory process. Histologically these lesions appear as an inflammatory infiltrate with a fibrotic background. Clinical presentations vary from slow growth with minimal mass effect, to bony destruction that can mimic malignancy. Although they occur most commonly in the orbit, there are a growing number of case reports of tumors of the temporal bone and skull base. Inflammatory pseudotumors of the temporal bone are best treated by excision, with radiation and steroid therapy reserved for inoperable tumors. The clinical, histologic, and radiographic features of two patients with inflammatory pseudotumor of the temporal bone are presented.
Keywords: Pseudotumor, temporal bone
Inflammatory pseudotumor is a non-neoplastic inflammatory process. Histologically these lesions appear as an inflammatory infiltrate with a fibrotic background. Clinical presentations vary from slow growth with minimal mass effect to bony destruction that can mimic malignancy. Treatment of inflammatory pseudotumors varies with location and is controversial. Tumors of the orbit respond well to steroid therapy, but tumors in the temporal bone with bony destruction are best treated by excision, with radiation and steroid therapy reserved for inoperable tumors. Although these tumors occur most commonly in the lung, they have also been described in the liver, retroperitoneum, thorax, and abdominal viscera. In the head and neck they have been described in the larynx, trachea, nasopharynx, oropharynx, orbits, meninges, sinuses, salivary glands, thyroid, infratemporal fossa, skull base, and temporal bone.1,2,3,4,5 We present two patients with very rare inflammatory pseudotumors involving the temporal bone. We present the clinical, histologic, and radiographic features and compare them with previously reported cases.
CASE REPORTS
Case 1
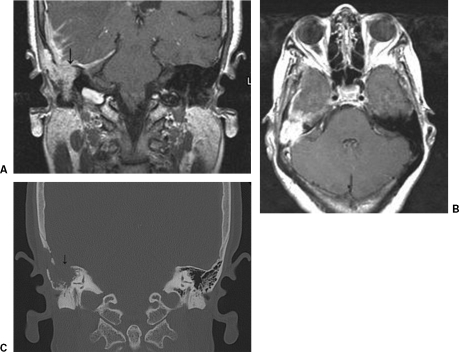
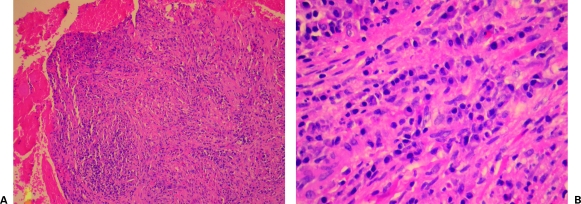
A 65-year-old female presented to an outside otolaryngologist with complaints of right-sided hearing loss, dizziness, and tinnitus. On exam both ears were clear with no evidence of fluid. The remainder of the patient's medical history and head and neck examination were unremarkable. Computed tomography (CT) and magnetic resonance imaging (MRI) showed an erosive lesion of the right temporal bone extending into the middle cranial fossa (Fig. 1). A mastoidectomy with biopsy was performed by the referring physician. Pathology showed reactive fibrous tissue with abundant lymphocytes and plasma cells with small regular nuclei, consistent with inflammatory pseudotumor (Fig. 2).
Figure 1.
(A) T1-weighted coronal magnetic resonance imaging shows a soft-tissue mass with reactive dural enhancement and cerebritis. (B) T1-weighted axial magnetic resonance imaging with gadolinium shows enhancing soft-tissue mass of the right temporal bone. (C) Coronal computed tomography image of the right temporal bone with erosion of the tegmen (arrow).
Figure 2.
Low- and high-power views of fibrous tissue with a lymphoplasmacytic and lymphohistocytic infiltrate. (A) Hematoxylin and eosin, magnification × 100. (B) Hematoxylin and eosin, magnification × 400.
Several days before her referral to our institution, the patient developed complex partial seizures with periods of aphasia which were treated with Depakote (Abbott Laboratories, Abbott Park, IL) and steroids. She was then taken to the operating room 2 weeks later for a transmastoid and middle cranial fossa approach for tumor resection. A 2- × 3-cm defect in the floor of the middle cranial fossa into the mastoid was visible. The tumor had eroded through the superior semicircular canal. The middle ear space was free of disease. The sigmoid sinus had been completely obliterated by the tumor and fibrosed. The dura was intact, but extremely fibrotic. We were able to completely remove the tumor and repair the defect with a split calvarial bone graft.
Radiation therapy was administered over 2 weeks for a total of 2000 cGy of radiation in 10 fractions. Steroids were given during the patient's radiation therapy and then tapered to complete a 10-week course. She did well postoperatively with resolution of her seizure activity. She has continued to do well and is without evidence of tumor recurrence by MRI imaging, 8 years following her initial presentation.
Case 2
A 40-year-old African American male presented to our office 10 years ago. He complained of right facial pain, ear fullness, and decreasing hearing on the right side slowly progressive over a 1-year period. His medical history and physical examination were otherwise unremarkable. His hearing was intact and he had no vestibular symptoms. CT and MRI imaging were obtained. Imaging showed him to have a lesion of the right petrous apex with medial extension to the right sphenoid bone and anterior extension to the cavernous sinus, foramen rotundum, and pterygopalatine fossa. The lesion extended through the petrous portion of the temporal bone into the mastoid cavity.
The patient was taken for mastoidectomy and biopsy of the mastoid portion of the lesion, which returned marked inflammation with reactive plasmacytosis and foreign body reaction. He was returned to the operating room for definitive resection where he underwent a right mastoidectomy, middle fossa craniotomy, and subtotal apicectomy. Dense granulation-type tissue filled the entire mastoid cavity, middle ear, and petrous apex. Following a standard middle cranial fossa approach, the floor of the middle cranial fossa was intact and the partial petrous apicectomy was performed by following the air cells tracts superior and posterior to the labyrinth. Pathology from the resection showed fibrosis with marked acute and chronic inflammation with a predominately mature plasma cell infiltrate. Following surgery the patient was treated with radiation therapy and recovered well without difficulty. Repeat imaging done at a 10-year follow-up shows him to be without recurrence of the lesion.
DISCUSSION
Inflammatory pseudotumors of the petrous apex and temporal bone are exceedingly rare. The most common head and neck presentation is in the orbit. Treatment of these lesions is usually with steroids (prednisone) given as 1mg/kg/d for 14 days, followed by a taper.6,7 Although the literature reports a control rate for orbital tumors of up to 78%, recurrence can be high.4,5,6 In contrast to orbital tumors, inflammatory pseudotumors of the temporal bone and petrous apex present with more aggressive growth and bony destruction. A recent case series described nine patients with temporal bone involvement. Five occurred in the middle ear and four in the mastoid. Three of these extended to the petrous apex, and three of the patients also had involvement of the otic capsule and labyrinth. Bony erosions were common in these patients with erosions into the tegmentum, cochlea, internal auditory canal, ossicular chain, and semicircular canals reported (six patients). Eight of the nine patients were treated with surgery with the remaining patient treated with steroids and radiation for a tumor extending from the nasopharynx to the petrous apex.6
The pathophysiology of these tumors is unknown. Theories include a nonspecific inflammatory response to a chronic infection, an autoimmune response, vasculitis, or a lymphocytic infiltration of a benign neoplasm. Clinical presentation varies with location of the tumor. Patients can present with pain, hearing loss, dizziness, otorrhea, and/or cranial nerve palsies.3,7 Diagnosis is one of exclusion as these lesions can mimic malignancy with bone erosion and cranial nerve involvement. Tissue biopsy and culture are needed to exclude inflammatory, infectious, or neoplastic lesions of the temporal bone. Although there are no pathognomonic findings on histology, these lesions characteristically demonstrate fibroblastic proliferation, sclerosis, and a lymphoplasmacytic infiltration of plasma cells, lymphocytes, and eosinophils. Our patients demonstrated these same pathologic findings of fibrous tissue with a lymphocytic infiltrate. Treatment varies with location of the tumor, degree of local invasion, and the possibility of complete resection. While orbital tumors are fairly responsive to steroid therapy, tumors in the temporal bone should be excised due to the high incidence of bony destruction and progressive erosion of inner ear structures. Radiation therapy has also been used for unresectable disease, seventh nerve involvement, and for residual or recurrent disease.3,6,7 With the small number of case reports in the literature it is difficult to compare outcomes of patients treated with radiation therapy verses surgical resection. However, from our experience and that found in the literature, it appears that most patients can expect good long-term results with complete surgical resection. Steroids can be used to temporarily relieve symptoms prior to surgery.
Work-up should include MRI and CT imaging. MRI imaging is the more characteristic, with tumors hypointense to brain on T1-imaging and either isointense or hypointense to brain on T2 images. Han and colleagues reported on five patients with skull-based lesions and noted three of five to be hypointense to brain on both T1 and T2 images and two of five to be isointense to brain on the T2 images.4 All five patients had homogeneous enhancement following contrast, with thickening and enhancement of adjacent intracranial dural structures.1,4,5 The T2 hypointensity is thought to be due to the fibrotic nature of inflammatory pseudotumors, with the relative lack of free water.4 The hypointensity of the T2 images can help differentiate these tumors from other primary malignant tumors of the skull base such as chordoma, chondrosarcoma, and invasion from nasopharyngeal carcinoma, which are hyperintense on T2.4 These finding were also noted in our patients who had tumors that were isointense to brain on both T1 and T2 images.
Although inflammatory pseudotumors are very rare in the head and neck, it is important for otolaryngologists to be aware of this disease process. Treatment of temporal bone and petrous apex lesions with surgery appears to provide the best outcome for the patients. Steroid and radiation therapy can be used for symptomatic relief, to help control bulky disease, or for poor surgical candidates. Although the number of cases in the literature is small, patients can expect good outcomes if these lesions are treated with complete surgical resection.
REFERENCES
- Lee J H, Kim K, Chung S W, Choi Y C, Lee A. A case report of inflammatory pseudotumor involving the clivus: CT and MRI finding. Korean J Radiol. 2001;2:231–234. doi: 10.3348/kjr.2001.2.4.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M W, Kim K H, Lee C H, Moh J H, Kim W H, Han M H. Fibrosing inflammatory pseudotumors of the central skull base. Laryngoscope. 1997;107:1651–1655. doi: 10.1097/00005537-199712000-00014. [DOI] [PubMed] [Google Scholar]
- Wiseman J B, Arriaga M A, Houston G D, Boyd E M. Facial paralysis and inflammatory pseudotumor of the facial nerve in a child. Otolaryngol Head Neck Surg. 1995;113:826–828. doi: 10.1016/S0194-59989570033-1. [DOI] [PubMed] [Google Scholar]
- Han M H, Kim M S, Chang K H, Kim K H, Yeon K M, Han M C. Fibrosing inflammatory pseudotumors involving the skull base: MR and CT manifestations with histopathologic comparison. AJNR Am J Neuroradiol. 1996;17:515–521. [PMC free article] [PubMed] [Google Scholar]
- Lee E J, Jung S L, Kim B S, et al. MR imaging of orbital inflammatory pseudotumors with extraorbital extension. Korean J Radiol. 2005;6:82–88. doi: 10.3348/kjr.2005.6.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson R A, Paucksakon R, Coker N J. Inflammatory pseudotumor of the temporal bone. Otol Neurotol. 2003;24:818–822. doi: 10.1097/00129492-200309000-00021. [DOI] [PubMed] [Google Scholar]
- Cho Y S, Kim S M, Chung W H, Hong S H. Inflammatory pseudotumor involving the skull base and cervical spine. J Laryngol Otol. 2001;115:580–584. doi: 10.1258/0022215011908298. [DOI] [PubMed] [Google Scholar]