Abstract
Background and purpose:
Sustained release niacin effectively lowers serum cholesterol, LDL and triglycerides, while raising HDL. However, 75% of patients experience cutaneous warmth and itching known as flush, leading to discontinuation. Acetylsalicylic acid (aspirin) reduces this flush only by about 30%, presumably through decreasing prostaglandin D2 (PGD2). We investigated whether niacin-induced flush in a rat model involves PGD2 and 5-HT, and the effect of certain flavonoids.
Experimental approach:
Three skin temperature measurements from each ear were recorded with an infrared pyrometer for each time point immediately before i.p. injection with either niacin or a flavonoid. The temperature was then measured every 10 min for 60 min.
Key results:
Niacin (7.5 mg per rat, equivalent to a human dose of 1750 mg per 80 kg) maximally increased ear temperature to 1.9±0.2 oC at 45 min. Quercetin and luteolin (4.3 mg per rat; 1000 mg per human), administered i.p. 45 min prior to niacin, inhibited the niacin effect by 96 and 88%, respectively. Aspirin (1.22 mg per rat; 325 mg per human) inhibited the niacin effect by only 30%. Niacin almost doubled plasma PGD2 and 5-HT, but aspirin reduced only PGD2 by 86%. In contrast, luteolin inhibited both plasma PGD2 and 5-HT levels by 100 and 67%, respectively.
Conclusions and implications.
Niacin-induced skin temperature increase is associated with PGD2 and 5-HT elevations in rats; luteolin may be a better inhibitor of niacin-induced flush because it blocks the rise in both mediators.
Keywords: acetylsalicylic acid, aspirin flavonoids, flush, luteolin, niacin, platelets, prostaglandin D2, 5-HT, quercetin
Introduction
In spite of a better knowledge of risk factors and better recognition and availability of more efficacious drugs for lowering serum cholesterol and triglycerides, mortality from cardiovascular disease continues to occur in 2/3 of patients treated with statins, and to increase worldwide by about 25% (Libby, 2005). Niacin (nicotinic acid) at 1–2 g day−1 decreases low-density lipoprotein and triglycerides, while increasing high-density lipoprotein levels (Carlson, 2005). Moreover, niacin and a statin together have superior lipoprotein-lowering profile (Brown et al., 2001), as also shown for slow-release niacin combined with lovastatin (Gupta and Ito, 2002). However, a limiting adverse effect in patients receiving immediate- or sustained-release niacin is the rapid development of significant cutaneous warmth and vasodilation, referred to as ‘flush', which severely limits compliance (Gupta and Ito, 2002).
Niacin-induced flush is thought to involve the release of prostaglandin D2 (PGD2) from the skin (Morrow et al., 1989, 1992), especially from antigen-presenting cells, macrophages (Urade et al., 1989; Meyers et al., 2007) or Langerhans cells (Benyo et al., 2006). However, co-administration of acetylsalicylic acid (aspirin) to reduce PGD2 levels has not been particularly effective in blocking niacin flush (Dunn et al., 1995; Jungnickel et al., 1997; Cefali et al., 2007). Consequently, molecules other than PGD2 may be involved and include histamine, vasoactive intestinal peptide and vascular endothelial growth factor (Boesiger et al., 1998; Grutzkau et al., 1998), as well as 5-HT released from platelets, enterochromaffin cells (Boushey and Dackiw, 2002) and mast cells (Kushnir-Sukhov et al., 2006). 5-HT is a prime candidate because it is known to be involved in the flush associated with carcinoid syndrome (Loong et al., 1968; Boushey and Dackiw, 2002).
We investigated the effect of certain flavonoids, molecules occurring naturally in plants and seeds, because they are known to inhibit mast cell (Middleton Jr et al., 2000) and platelet (Beretz et al., 1982; Mruk et al., 2000) secretion. We used a rat model previously reported to show that the phenothiazine haloperidol could block niacin-induced skin vasodilation (Turenne et al., 2001) to investigate (a) whether niacin can increase plasma 5-HT and (b) whether flavonoids such as luteolin can inhibit niacin-induced skin temperature increase, as well as any changes in plasma PGD2 and 5-HT levels.
Materials and methods
Animals
All animal procedures were approved by the Tufts-New England Medical Center Animal Care and Use Committee. Male Sprague–Dawley rats (300–350 g) were housed three per cage and were provided with food and water ad libitum. The room temperature was kept constant at 21±1 °C, with a 1410 hours light:dark schedule, with lights out at 1900 hours.
Assessment of niacin-induced skin temperature changes
Temperature measurements were recorded with a hand-held infrared pyrometer connected to a milli-voltmeter (Model OS613A, Omega Co., Stamford, CT, USA). The probe was held at a distance of 1–2 mm from the animal's skin, and temperature readings were taken from an ear area approximately 3 mm in diameter. Animals were habituated to handling and to the infrared probe for 3 days before use. On the day of the experiment, the animals were brought into the laboratory (0900–1000 hours). Three temperature readings from the top half of each ear were recorded for each time point without anaesthesia immediately before animals were injected i.p. with either niacin or the test flavonoid. The ear temperature was then measured every 10 min for a period of up to 60 min. The animals were returned to their cages between measurements. Animals were ‘rested' for 1 week and were used again; the effect of niacin was not changed in rats that were used more than once.
Pretreatment with various flavonoids
Rats were randomly administered either (a) vehicle (olive seed oil) followed by niacin or (b) a flavonoid (4.3 mg per rat, equivalent to 1000 mg per 80 kg human) followed by niacin. This dose of flavonoids, the structure of which differs only by a hydroxyl group at certain positions, was chosen because it was previously shown to inhibit mast cell responses in vivo (Kimata et al., 2000a) and may reasonably be administered orally in humans.
Blood mediator measurements
In certain cases, blood was collected immediately after the end of the experimental period by killing (by asphyxiation with CO2), decapitation and collection from neck vessels. Blood was centrifuged at 350 g in a refrigerated centrifuge and the plasma collected and frozen at −20 °C until assay. Plasma levels of PGD2 (Cayman, Ann Arbor, MI, USA) and 5-HT were assayed using the ELISA kit (Biosource, Nivelle, Belgium). The lowest levels of sensitivity for each were 200 pg ml−1 (intra- and inter-assay variation 10–20%) and 0.5 ng ml−1 (intra-assay variation 26 and inter-assay variation 15), respectively.
Statistical analysis
The six ear temperature measurements (three from each ear) were averaged for each point. Any temperature change was calculated by subtracting from the mean value for each experimental point the baseline temperature obtained immediately before the vehicle/drug was injected or the baseline measured immediately before niacin administration, whichever was appropriate. All data are presented as mean±s.d. of the actual temperatures or percentage change from that recorded after niacin administration. Paired comparisons between niacin and control or niacin and drug pretreatment followed by niacin were analysed with either the paired t-test or the non-parametric Mann–Whitney U-test. Multivariant ANOVA analysis was performed on all other comparisons. Significance is denoted by P<0.05.
Materials
Aspirin, fisetin, kaempferol, luteolin, myricetin, niacin and quercetin were purchased from Sigma (St Louis, MO, USA). All drugs were first dissolved in olive kernel oil and then freshly diluted with 0.9% NaCl, on each day of the experiment.
Results
Effect of niacin on skin temperature
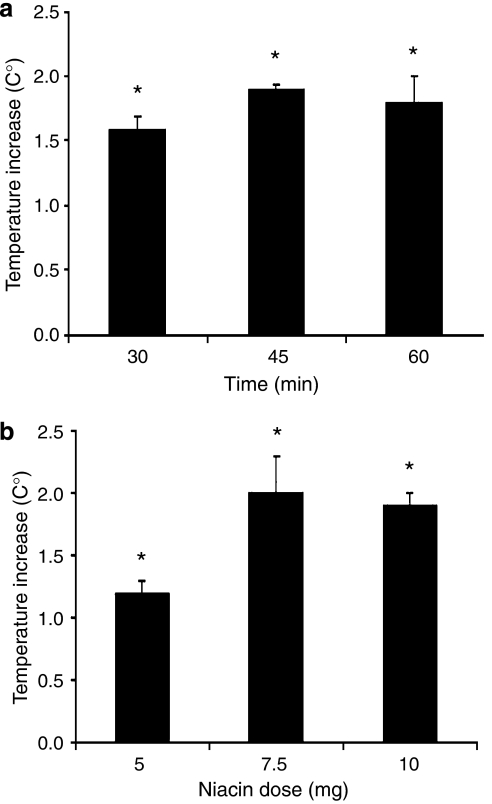
The basal mean ear temperature was 26.5–28.5 °C (n=5). Niacin (7.5 mg per rat, equivalent to 1750 mg per 80 kg human) injected i.p. in conscious rats induced a time-dependent temperature increase with a maximum of 1.9±0.2 °C (n=5, P=0.0002) at 45 min (Figure 1a). A dose–response study for niacin (5, 7.5 and 10 mg per rat, n=5) showed a maximal temperature increase of 2.0±0.1 °C (P=0.001) at 45 min with 7.5 mg per rat (Figure 1b).
Figure 1.
(a) A time course of ear temperature increase (n=5) in response to a single i.p. niacin (7.5 mg per rat) injection. The increase at all time points was significant (*P=0.0002). (b) Dose–response of the effect of a single i.p. niacin injection on ear temperature increases recorded 45 min later (n=5; *P=0.0001). Niacin rat doses correspond to the doses in an 80 kg human as follows: 5.0 mg per rat=1167 mg per human; 7.5 mg per rat=1750 mg per human; 10 mg per rat=2334 mg per human.
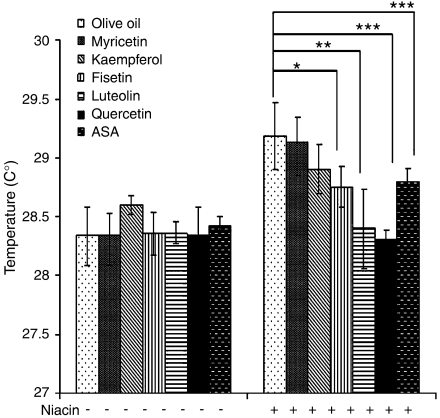
Effect of aspirin and flavonoids on niacin-induced skin temperature increase
We investigated whether pretreatment for 2 h with aspirin (1.22 mg per rat, equivalent to 325 mg per 80 kg human) or various flavonoids (4.3 mg per kg, equivalent to 1000 mg per human) could inhibit the effect of niacin (7.5 mg per rat) in this animal model. Aspirin inhibited this effect by 30% (n=6, P=0.0193; Figure 2). Myricetin and kaempferol had no effect; fisetin inhibited the effect of niacin by 50% (n=6, P=0.0204; Figure 2). Quercetin and luteolin were the most effective in reducing ear temperatures by 96 and 88%, respectively (n=6, P=0.0002 and P=0.0041; Figure 2); there was no statistical difference between the effects of quercetin and luteolin.
Figure 2.
Comparison of the inhibitory effect of fisetin, kaempferol, luteolin, myricetin, quercetin (4.3 mg per rat=1000 mg per human) and aspirin (ASA; 1.22 mg per rat; 325 mg per human), administered i.p. 10 min prior to niacin on the ear temperature increase recorded 45 min after a single i.p. dose of niacin (7.5 mg per rat) in olive oil (n=6, *P=0.0204; **P=0.0041; ***P=0.0002; ****P=0.0193). The percentage inhibition was calculated after the corresponding baseline temperature was subtracted.
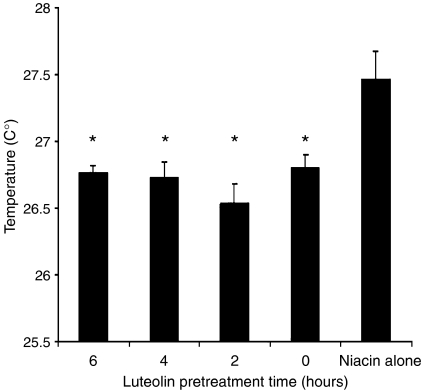
Effect of duration of pretreatment with luteolin
We then investigated whether the length of pretreatment with luteolin affected its ability to inhibit the niacin flush. Luteolin significantly decreased the niacin-induced temperature increase even when added together with niacin (time=0) and remained significant at all time points from 0 to 6 h. There was no significant difference between the 2, 4 and 6 h pretreatment time points among the luteolin-pretreated samples (Figure 3).
Figure 3.
Time course of the inhibitory effect of pretreatment with luteolin (4.3 mg per rat). Luteolin was given at the time points shown before, or at the same time as (shown as 0 h), the single i.p. niacin injection (7.5 mg per rat). Increases in ear temperature (n=3) were measured 45 min after niacin treatment. All pretreatments produced statistically significant inhibition, compared to a control rat injected with 0.5 ml olive oil and 7.5 mg niacin (*P<0.001).
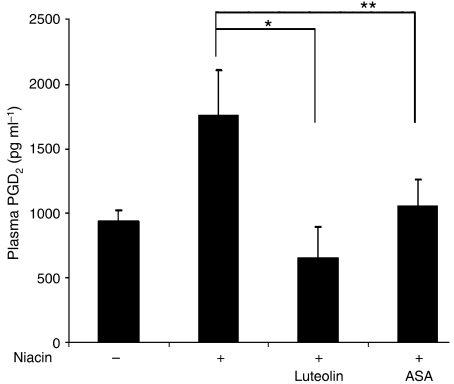
Effect of niacin on plasma PGD2 and 5-HT levels
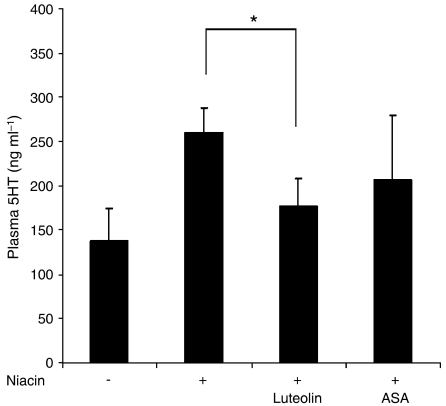
We then investigated the effect of niacin on plasma PGD2 and 5-HT levels. Niacin (7.5 mg per rat) increased plasma PGD2 by 88% at 45 min (n=3, P=0.0178; Figure 4) and plasma 5-HT by 90% (n=4, P=0.0101; Figure 5).
Figure 4.
Effect of aspirin (ASA; 1.22 mg per rat) and luteolin (4.3 mg per rat) administered 2 h prior to a single i.p. injection of niacin (7.5 mg per rat) on plasma PGD2 levels measured 45 min later (n=3). Brackets indicate groups compared (*P=0.014; **P=0.0419). PGD2, prostaglandin D2.
Figure 5.
Effect of aspirin (ASA; 1.22 mg per rat) and luteolin (4.3 mg per rat) administered 2 h prior to a single i.p. injection of niacin (7.5 mg per rat) on plasma 5-HT levels measured 45 min later (n=3). Brackets indicate groups compared (*P=0.0263).
Effect of aspirin and luteolin on niacin-induced plasma PGD2 and 5-HT levels
Pretreatment for 2 h with aspirin (1.22 mg per rat) reduced plasma PGD2 by 86% (n=3, P=0.018; Figure 4), but had no statistically significant effect on plasma 5-HT levels (Figure 5). In contrast, luteolin (4.3 mg per rat) significantly reduced plasma PGD2 levels by 100% (n=3, P=0.014; Figure 4) and 5-HT levels by 32% (n=3, P=0.0263; Figure 5). If the baseline 5-HT of 137 ng ml−1 was to be subtracted from the niacin-induced level of 260 ng ml−1 and the level of 177 ng ml−1 in the presence of both luteolin and niacin, and then the inhibition re-calculated, luteolin inhibited by 97% the increase in 5-HT following niacin.
Discussion
Here, we report for the first time to our knowledge that quercetin and luteolin can effectively reduce immediate-release niacin-induced temperature increase in an established rat model of niacin-induced ‘flush'. The dose of niacin used in our study was equivalent to that previously used in the same rat model (Turenne et al., 2001) and within the range of doses given orally (1.5–2 g day−1) to treat hyperlipidaemia in humans (Gupta and Ito, 2002). We also show that, in addition to PGD2, niacin can increase plasma 5-HT levels and that luteolin can inhibit both PGD2 and 5-HT increase due to niacin. We used olive kernel oil instead of dimethyl sulphoxide to dissolve the flavonoids, in order to use an edible vehicle for possible future oral use, especially because luteolin is rich in olive oil (Botia et al., 2001; Morello et al., 2005).
Our results further indicate that aspirin has only a weak inhibitory effect on the flush, even though it lowers plasma PGD2 levels. In contrast, luteolin significantly inhibited the flush as well as both plasma PGD2 and 5-HT. The ability of luteolin and quercetin to inhibit niacin flush may be related to the anti-oxidant and anti-inflammatory activity of flavonoids (Middleton Jr et al., 2000). Quercetin inhibits mast cell secretion (Kempuraj et al., 2005) and so does luteolin (Kimata et al., 2000b; Hirano et al., 2004). Flavonoids also inhibit platelet aggregation, with quercetin being more potent than kaempferol (Gryglewski et al., 1987; Tzeng et al., 1991). Quercetin was specifically shown to inhibit platelet 5-HT release (Beretz et al., 1982). Luteolin inhibited cyclooxygenase 2 (Hu and Kitts, 2004) and platelet 5-HT release through the thromboxane A2 receptor (Guerrero et al., 2005); the structural requirements for this action (Guerrero et al., 2005) were apparently similar to those also required for mast cell inhibition (Alexandrakis et al., 1999). Luteolin also inhibited 5-HT-induced cutaneous irritant reactions (Baolin et al., 2005).
The exact source of 5-HT liberated by niacin (or some metabolite) in vivo is not presently known, but could derive from platelets (Vanhoutte and Cohen, 1983) or skin mast cells (Kushnir-Sukhov et al., 2006), and is the major vasodilatory amine in rodents (Gershon et al., 1975). Elevated plasma 5-HT levels (Matuchansky and Launay, 1995) are associated with the facial flush, characteristic of the carcinoid syndrome (Boushey and Dackiw, 2002). In fact, flushing in carcinoid was inhibited by anti-5-HT drugs (Loong et al., 1968; Plank and Feldman, 1975). The ability of the phenothiazine haloperidol to inhibit the niacin flush (Turenne et al., 2001) could involve antagonism of 5-HT receptors (Cosi and Koek, 2001). Tryptophan is the precursor of both 5-HT and niacin, implying that niacin may affect the action of 5-HT. Furthermore, prostaglandins may regulate plasma 5-HT levels (Utsunomiya et al., 1981), whereas 5-HT potentiates the effect of low concentrations of arachidonic acid on human platelet aggregation (Saeed et al., 2003). The exact molecular target of luteolin is not clear, especially because the source of 5-HT and PGD2 is not known. However, if these molecules are derived from skin mast cells, a possible target could be protein kinase C, as we had previously shown that protein kinase C-θ was inhibited by flavonoids, especially quercetin (Kempuraj et al., 2005).
So far, only PGD2 has been implicated in niacin flush (Morrow et al., 1989, 1992). Niacin stimulated PGD2 synthase in macrophages (Knowles et al., 2005), through activation of a unique G-protein-coupled receptor (Lorenzen et al., 2002), and resulted in a threefold PGD2 release after 30 min stimulation (Meyers et al., 2007). Niacin also increased the expression of prostanoid synthase in the epidermal Langerhans cells (Benyo et al., 2006) and resulted in PGD2 release (Maciejewski-Lenoir et al., 2006). Nevertheless, others considered that the major source of endogenous PGD2 is antigen-presenting cells (Urade et al., 1989). Mice lacking a nicotinic acid receptor did not show niacin-induced flush (Soudijin et al., 2007). However, blocking PGD2 receptors resulted in reduced, but still substantial flushing (Benyo et al., 2005). Moreover, an oral PGD2 receptor-1 antagonist could block niacin- and PGD2-induced vasodilation in female mice, but only partially in male mice (Cheng et al., 2006).
In one placebo-controlled study, 60% of subjects on placebo experienced flush after ingesting 500 mg immediate-release niacin, but this proportion dropped to 41% (30% decrease) when taking 325 mg aspirin daily for 4 days and further reduced to 29% in those subjects (50%) taking 650 mg aspirin, prior to niacin (Jungnickel et al., 1997). This effect translates to a 30% decrease of flush induced by a niacin dose of 500 mg, which is a quarter of the dose (2000 mg) needed for effective treatment. In another double-blinded, cross-over study, pretreatment with 325 mg niacin only partially reduced flush again due to 500 mg immediate-release niacin (Dunn et al., 1995). A new ‘optimized' extended-release niacin given as a single 2000 mg dose in 156 healthy male volunteers induced flush in 89% of the subjects instead of 98% of the subjects, with a 43% reduction in median flush duration (Cefali et al., 2006). Co-administration of aspirin (650 mg) with this extended-release niacin further reduced the number of subjects who experienced flush from 77 to 61% (Cefali et al., 2007). Finally, co-administration of the PGD2 receptor antagonist laropiprant with an extended-release niacin in humans did not reduce flush by more than 50% (Lai et al., 2007).
Niacin discontinuation due to flushing may involve as many as 75% of the patients even with extended-release niacin (Guyton et al., 1998; McCormack and Keating, 2005), and it increases over the course of treatment (McKenney, 2004). This is also true for the combination of lovastatin and extended-release niacin (Gupta and Ito, 2002), which is superior in reducing triglycerides, low-density lipoprotein, very low-density lipoprotein and Apo (a), while increasing high-density lipoprotein (Morgan et al., 1998; Gupta and Ito, 2002; Carlson, 2005).
The present findings suggest that plasma 5-HT may contribute substantially to niacin-induced flush in rodents. Other potential vasodilators may include vasoactive intestinal peptide, vascular endothelial growth factor as well as certain cytokines and chemokines (Castellani et al., 2007). Our findings also suggest that certain flavonoids can block niacin flush through inhibition of the increases in both plasma PGD2 and 5-HT in an animal model.
Acknowledgments
This work was supported by Theta Biomedical Consulting and Development Co., Inc. (Brookline, MA, USA). We thank Ms Jessica Christian for her word processing skills.
Abbreviations
- PGD2
prostaglandin D2
Conflict of interest
US patent nos. 6624148B2, 7115278 and EPO 1365777 have been awarded to one author (TCT), and one US patent application no. 10/811,828, submitted by the same author (TCT) covering drug-induced flush, is pending review.
References
- Alexandrakis M, Singh L, Boucher W, Letourneau R, Theofilopoulos P, Theoharides TC. Differential effect of flavonoids on inhibition of secretion and accumulation of secretory granules in rat basophilic leukemia cells. Int J Immunopharmacol. 1999;21:379–390. doi: 10.1016/s0192-0561(99)00018-1. [DOI] [PubMed] [Google Scholar]
- Baolin L, Weiwei W, Ning T. Topical application of luteolin inhibits scratching behavior associated with allergic cutaneous reaction in mice. Planta Med. 2005;71:424–428. doi: 10.1055/s-2005-864137. [DOI] [PubMed] [Google Scholar]
- Benyo Z, Gille A, Bennett CL, Clausen BE, Offermanns S. Nicotinic acid-induced flushings is mediated by activation of epidermal Langerhans cells. Mol Pharmacol. 2006;70:1844–1899. doi: 10.1124/mol.106.030833. [DOI] [PubMed] [Google Scholar]
- Benyo Z, Gille A, Kero J, Csiky M, Suchankova MC, Nusing RM, et al. GPR109A (PUMA-G/HM74A) mediates nicotinic acid-induced flushing. J Clin Invest. 2005;115:3634–3640. doi: 10.1172/JCI23626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beretz A, Cazenave JP, Anton R. Inhibition of aggregation and secretion of human platelets by quercetin and other flavonoids: structure-activity relationships. Agents Actions. 1982;12:382–387. doi: 10.1007/BF01965408. [DOI] [PubMed] [Google Scholar]
- Boesiger J, Tsai M, Maurer M, Yamaguchi M, Brown LF, Claffey KP, et al. Mast cells can secrete vascular permeability factor/vascular endothelial cell growth factor and exhibit enhanced release after immunoglobulin E-dependent upregulation of Fce receptor I expression. J Exp Med. 1998;188:1135–1145. doi: 10.1084/jem.188.6.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botia JM, Ortuno A, Benavente-García O, Baidez AG, Frias J, Marcos D, et al. Modulation of the biosynthesis of some phenolic compounds in Olea europaea L. fruits: their influence on olive oil quality. J Agric Food Chem. 2001;49:355–358. doi: 10.1021/jf9913108. [DOI] [PubMed] [Google Scholar]
- Boushey RP, Dackiw AP. Carcinoid tumors. Curr Treat Options Oncol. 2002;3:319–326. doi: 10.1007/s11864-002-0031-2. [DOI] [PubMed] [Google Scholar]
- Brown BG, Zhao XQ, Chait A, Fisher LD, Cheung MC, Morse JS, et al. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med. 2001;345:1583–1592. doi: 10.1056/NEJMoa011090. [DOI] [PubMed] [Google Scholar]
- Carlson LA. Nicotinic acid: the broad-spectrum lipid drug. A 50th anniversary review. J Intern Med. 2005;258:94–114. doi: 10.1111/j.1365-2796.2005.01528.x. [DOI] [PubMed] [Google Scholar]
- Castellani ML, Bhattacharya K, Tagen M, Kempuraj D, Perrella A, De Lutis M, et al. Anti-chemokine therapy for inflammatory diseases. Int J Immunopathol Pharmacol. 2007;20:447–453. doi: 10.1177/039463200702000303. [DOI] [PubMed] [Google Scholar]
- Cefali EA, Simmons PD, Stanek EJ, McGovern ME, Kissling CJ. Aspirin reduces cutaneous flushing after administration of an optimized extended-release niacin formulation. Int J Clin Pharmacol Ther. 2007;45:78–88. doi: 10.5414/cpp45078. [DOI] [PubMed] [Google Scholar]
- Cefali EA, Simmons PD, Stanek EJ, Shamp TR. Improved control of niacin-induced flushing using an optimized once-daily, extended niacin formulation. Int J Clin Pharmacol Ther. 2006;44:633–640. doi: 10.5414/cpp44633. [DOI] [PubMed] [Google Scholar]
- Cheng K, Wu TJ, Wu KK, Sturino C, Metters K, Gottesdiener K, et al. Antagonism of the prostaglandin D2 receptor 1 suppresses nicotinic acid-induced vasodilation in mice and humans. Proc Natl Acad Sci USA. 2006;103:6682–6687. doi: 10.1073/pnas.0601574103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosi C, Koek W. Agonist, antagonist, and inverse agonist properties of antipsychotics at human recombinant 5-HT(1A) receptors expressed in HeLa cells. Eur J Pharmacol. 2001;433:55–62. doi: 10.1016/s0014-2999(01)01493-5. [DOI] [PubMed] [Google Scholar]
- Dunn RT, Ford MA, Rindone JP, Kwiecinski FA. Low-dose aspirin and ibuprofen reduce the cutaneous reactions following niacin administration. Am J Ther. 1995;2:478–480. doi: 10.1097/00045391-199506000-00006. [DOI] [PubMed] [Google Scholar]
- Gershon RK, Askenase PW, Gershon MD. Requirement for vasoactive amines for production of delayed-type hypersensitivity skin reactions. J Exp Med. 1975;142:732–747. doi: 10.1084/jem.142.3.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grutzkau A, Kruger-Krasagakes S, Baumeister H, Schwarz C, Kogel H, Welker P, et al. Synthesis, storage and release of vascular endothelial growth factor/vascular permeability factor (VEGF/VPF) by human mast cells: implications for the biological significance of VEGF206. Mol Biol Cell. 1998;9:875–884. doi: 10.1091/mbc.9.4.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryglewski RJ, Korbut R, Robak J, Swies J. On the mechanism of antithrombotic action of flavonoids. Biochem Pharmacol. 1987;36:317–322. doi: 10.1016/0006-2952(87)90288-7. [DOI] [PubMed] [Google Scholar]
- Guerrero JA, Lozano ML, Castillo J, Benavente-García O, Vicente V, Rivera J. Flavonoids inhibit platelet function through binding to the thromboxane A2 receptor. J Thromb Haemost. 2005;3:369–376. doi: 10.1111/j.1538-7836.2004.01099.x. [DOI] [PubMed] [Google Scholar]
- Gupta EK, Ito MK. Lovastatin and extended-release niacin combination product: the first drug combination for the management of hyperlipidemia. Heart Dis. 2002;4:124–137. doi: 10.1097/00132580-200203000-00010. [DOI] [PubMed] [Google Scholar]
- Guyton JR, Goldberg AC, Kreisberg RA, Sprecher DL, Superko HR, O'Connor CM. Effectiveness of once-nightly dosing of extended-release niacin alone and in combination for hypercholesterolemia. Am J Cardiol. 1998;82:737–743. doi: 10.1016/s0002-9149(98)00448-2. [DOI] [PubMed] [Google Scholar]
- Hirano T, Higa S, Arimitsu J, Naka T, Shima Y, Ohshima S, et al. Flavonoids such as luteolin, fisetin and apigenin are inhibitors of interleukin-4 and interleukin-13 production by activated human basophils. Int Arch Allergy Immunol. 2004;134:135–140. doi: 10.1159/000078498. [DOI] [PubMed] [Google Scholar]
- Hu C, Kitts DD. Luteolin and luteolin-7-O-glucoside from dandelion flower suppress iNOS and COX-2 in RAW264.7 cells. Mol Cell Biochem. 2004;265:107–113. doi: 10.1023/b:mcbi.0000044364.73144.fe. [DOI] [PubMed] [Google Scholar]
- Jungnickel PW, Maloley PA, Vander Tuin EL, Peddicord TE, Campbell JR. Effect of two aspirin pretreatment regimens on niacin-induced cutaneous reactions. J Gen Intern Med. 1997;12:591–596. doi: 10.1046/j.1525-1497.1997.07118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempuraj D, Madhappan B, Christodoulou S, Boucher W, Cao J, Papadopoulou N, et al. Flavonols inhibit proinflammatory mediator release, intracellular calcium ion levels and protein kinase C theta phosphorylation in human mast cells. Br J Pharmacol. 2005;145:934–944. doi: 10.1038/sj.bjp.0706246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimata M, Inagaki N, Nagai H. Effects of luteolin and other flavonoids on IgE-mediated allergic reactions. Planta Med. 2000a;66:25–29. doi: 10.1055/s-2000-11107. [DOI] [PubMed] [Google Scholar]
- Kimata M, Shichijo M, Miura T, Serizawa I, Inagaki N, Nagai H. Effects of luteolin, quercetin and baicalein on immunoglobulin E-mediated mediator release from human cultured mast cells. Clin Exp Allergy. 2000b;30:501–508. doi: 10.1046/j.1365-2222.2000.00768.x. [DOI] [PubMed] [Google Scholar]
- Knowles HJ, Poole RT, Workman P, Harris AL. Niacin induces PPARgamma expression and transcriptional activation in macrophages via HM74 and HM74a-mediated induction of prostaglandin synthesis pathways. Biochem Pharmacol. 2005;71:646–656. doi: 10.1016/j.bcp.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Kushnir-Sukhov NM, Brown JM, Wu Y, Kirshenbaum A, Metcalfe DD. Human mast cells are capable of serotonin synthesis and release. J Allergy Clin Immunol. 2006;119:498–499. doi: 10.1016/j.jaci.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Lai E, De Leipeleire I, Crumley TM, Liu F, Wenning LA, Michiels N, et al. Suppression of niacin-induced vasodialation with an antagonist to prostaglandin D(2) receptor subtype 1. Clin Pharmacol Ther. 2007;81:849–857. doi: 10.1038/sj.clpt.6100180. [DOI] [PubMed] [Google Scholar]
- Libby P. The forgotten majority: unfinished business in cardiovascular risk reduction. J Am Coll Cardiol. 2005;46:1225–1228. doi: 10.1016/j.jacc.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Loong SC, Lance JW, Rawle KC. The control of flushing and diarrhoea in carcinoid syndrome by an antiserotonin agent, BC105. Med J Aust. 1968;2:845–848. [PubMed] [Google Scholar]
- Lorenzen A, Stannek C, Burmeister A, Kalvinsh I, Schwabe U. G protein-coupled receptor for nicotinic acid in mouse macrophages. Biochem Pharmacol. 2002;64:645–648. doi: 10.1016/s0006-2952(02)01220-0. [DOI] [PubMed] [Google Scholar]
- Maciejewski-Lenoir D, Richman JG, Hakak Y, Gaidatov I, Behan DP, Connolly DT. Langerhans cells release prostaglandin D2 in response to nicotinic acid. J Invest Dermatol. 2006;126:2637–2646. doi: 10.1038/sj.jid.5700586. [DOI] [PubMed] [Google Scholar]
- Matuchansky C, Launay JM. Serotonin, catecholamines, and spontaneous midgut carcinoid flush: plasma studies from flushing and nonflushing sites. Gastroenterology. 1995;108:743–751. doi: 10.1016/0016-5085(95)90447-6. [DOI] [PubMed] [Google Scholar]
- McCormack PL, Keating GM. Prolonged-release nicotinic acid: a review of its use in the treatment of dyslipidaemia. Drugs. 2005;65:2719–2740. doi: 10.2165/00003495-200565180-00014. [DOI] [PubMed] [Google Scholar]
- McKenney J. New perspectives on the use of niacin in the treatment of lipid disorders. Arch Intern Med. 2004;164:697–705. doi: 10.1001/archinte.164.7.697. [DOI] [PubMed] [Google Scholar]
- Meyers CD, Liu P, Kamanna VS, Kashyap ML. Nicotinic acid induces secretion of prostaglandin D(2) in human macrophages: an in vitro model of the niacin flush. Atherosclerosis. 2007;192:253–258. doi: 10.1016/j.atherosclerosis.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Middleton E, Jr, Kandaswami C, Theoharides TC. The effects of plant flavonoids on mammalian cells: implications for inflammation, heart disease and cancer. Pharmacol Rev. 2000;52:673–751. [PubMed] [Google Scholar]
- Morello JR, Vuorela S, Romero MP, Motilva MJ, Heinonen M. Antioxidant activity of olive pulp and olive oil phenolic compounds of the arbequina cultivar. J Agric Food Chem. 2005;53:2002–2008. doi: 10.1021/jf048386a. [DOI] [PubMed] [Google Scholar]
- Morgan JM, Capuzzi DM, Guyton JR. A new extended-release niacin (Niaspan): efficacy, tolerability, and safety in hypercholesterolemic patients. Am J Cardiol. 1998;82:29U–34U. doi: 10.1016/s0002-9149(98)00732-2. [DOI] [PubMed] [Google Scholar]
- Morrow JD, Awad JA, Oates JA, Roberts LJ. Identification of skin as a major site of prostaglandin D2 release following oral administration of niacin in humans. J Invest Dermatol. 1992;98:812–815. doi: 10.1111/1523-1747.ep12499963. [DOI] [PubMed] [Google Scholar]
- Morrow JD, Parsons WG, Roberts LJ. Release of markedly increased quantities of prostaglandin D2 in vivo in humans following administration of nicotinic acid. Prostaglandins. 1989;38:263–274. doi: 10.1016/0090-6980(89)90088-9. [DOI] [PubMed] [Google Scholar]
- Mruk JS, Webster MW, Heras M, Reid JM, Grill DE, Chesebro JH. Flavone-8-acetic acid (Flavonoid) profoundly reduces platelet-dependent thrombosis and vasoconstriction after deep arterial injury in vivo. Circulation. 2000;101:324–328. doi: 10.1161/01.cir.101.3.324. [DOI] [PubMed] [Google Scholar]
- Plank J, Feldman JM. Adrenal function in the carcinoid syndrome: effects of the serotonin antagonist cyproheptadine. Metabolism. 1975;24:1035–1046. doi: 10.1016/0026-0495(75)90097-9. [DOI] [PubMed] [Google Scholar]
- Saeed SA, Rasheed H, Gilani AU. Synergism interaction between arachidonic acid by 5-hydroxytryptamine in human platelet aggregation is mediated through multiple signalling pathways. Acta Pharmacol Sin. 2003;24:958–964. [PubMed] [Google Scholar]
- Soudijin W, van Wijngssrden I, Ijzerman AP. Nicotinic acid receptor subtypes and their ligands. Med Res Rev. 2007;27:417–433. doi: 10.1002/med.20102. [DOI] [PubMed] [Google Scholar]
- Turenne SD, Seeman M, Ross BM. An animal model of nicotinic-acid-induced vasodilatation: effect of haloperidol, caffeine and nicotine upon nicotinic acid response. Schizophr Res. 2001;50:191–197. doi: 10.1016/s0920-9964(00)00082-7. [DOI] [PubMed] [Google Scholar]
- Tzeng SH, Ko WC, Ko FN, Teng CM. Inhibition of platelet aggregation by some flavonoids. Thromb Res. 1991;64:91–100. doi: 10.1016/0049-3848(91)90208-e. [DOI] [PubMed] [Google Scholar]
- Urade Y, Ujihara M, Hariguchi Y, Ikai K, Hayaishi O. The major source of endogenous prostaglandin D2 production is likely antigen-presenting cells: localization of glutathione-requiring PGD2 synthetase in histiocytes, dendritic and Kupffer cells in various rat tissues. J Immunol. 1989;143:2982–2987. [PubMed] [Google Scholar]
- Utsunomiya T, Krausz MM, Shepro D, Hechtman HB. Prostaglandin control of plasma and platelet 5-hydroxytryptamine in normal and embolized animals. Am J Physiol. 1981;241:H766–H771. doi: 10.1152/ajpheart.1981.241.5.H766. [DOI] [PubMed] [Google Scholar]
- Vanhoutte PM, Cohen RA. The elusory of serotonin in vascular function and disease. Biochem Pharmacol. 1983;32:3671–3674. doi: 10.1016/0006-2952(83)90134-x. [DOI] [PubMed] [Google Scholar]