Abstract
Autogenous iliac crest has long served as the gold standard for anterior lumbar arthrodesis although added morbidity results from the bone graft harvest. Therefore, femoral ring allograft, or cages, have been used to decrease the morbidity of iliac crest bone harvesting. More recently, an experimental study in the animal showed that harvesting local bone from the anterior vertebral body and replacing the void by a radio-opaque β-tricalcium phosphate plug was a valid concept. However, such a concept precludes theoretically the use of posterior pedicle screw fixation. At one institution a consecutive series of 21 patients underwent single- or multiple-level circumferential lumbar fusion with anterior cages and posterior pedicle screws. All cages were filled with cancellous bone harvested from the adjacent vertebral body, and the vertebral body defect was filled with a β-tricalcium phosphate plug. The indications for surgery were failed conservative treatment of a lumbar degenerative disc disease or spondylolisthesis. The purpose of this study, therefore, was to report on the surgical technique, operative feasibility, safety, benefits, and drawbacks of this technique with our primary clinical experience. An independent researcher reviewed all data that had been collected prospectively from the onset of the study. The average age of the patients was 39.9 (26–57) years. Bone grafts were successfully harvested from 28 vertebral bodies in all but one patient whose anterior procedure was aborted due to difficulty in freeing the left common iliac vein. This case was converted to a transforaminal interbody fusion (TLIF). There was no major vascular injury. Blood loss of the anterior procedure averaged 250 ml (50–350 ml). One tricalcium phosphate bone plug was broken during its insertion, and one endplate was broken because of wrong surgical technique, which did not affect the final outcome. One patient had a right lumbar plexopathy that was not related to this special technique. There was no retrograde ejaculation, infection or pseudoarthrosis. One patient experienced a deep venous thrombosis. At the last follow up (mean 28 months) all patients had a solid lumbar spine fusion. At the 6-month follow up, the pain as assessed on the visual analog scale (VAS) decreased from 6.9 to 4.5 (33% decrease), and the Oswestry disability index (ODI) reduced from 48.0 to 31.7 with a 34% reduction. However, at 2 years follow up there was a trend for increase in the ODI (35) and VAS (5). The data in this study suggest that harvesting a cylinder of autograft from the adjacent vertebral body is safe and efficient. Filling of the void defect with a β-tricalcium phosphate plug does not preclude the use of posterior pedicle screw stabilization.
Keywords: Lumbar fusion, β-Tricalcium phosphate (β-TCP), Cage, Pedicle screw
Introduction
Circumferential spine fusion for the treatment of degenerative disease of the lumbar spine was popularized by O’Brien [10]. Recently, this has been achieved with interbody cages either inserted as anterior lumbar interbody fusion (ALIF), or posterior or transforaminal lumbar interbody fusion (PLIF/TLIF) [14, 20]. Filling of the interbody cages have in most cases been done with autologous iliac crest. However, harvesting autologous bone graft from the iliac crest often requires an additional incision and is associated with a significant morbidity that can reach 30–40% [2, 3, 7, 16]. To avoid the iatrogenic complications of iliac crest bone harvesting, femoral ring allograft and machined allograft cages have been designed [9, 11, 13]. However, they carry the potential risk of infectious disease transmission, infection, immunologic response, and mechanical complication such as graft resorption and pseudoarthrosis [12, 19]. More recently some investigators have relied on bone morphogenic protein (BMP) in anterior interbody fusion with controversial results ranging from excellent results [4] while other investigators have discouraged their use because of too many complications and/or pseudoarthroses [15].
In an effort to reduce the morbidity of iliac crest bone graft, Steffen and Aebi came up with the concept of harvesting the corticocancellous autologous from the vertebral body itself [17, 18]. Their concept relies on harvesting a cylinder bone autograft from the adjacent vertebral body and filling the void with a β-tricalcium phosphate (β-TCP) radio-opaque porous plug (Chronos® Synthes, Paoli, PA, USA). The autologous corticocancellous plug obtained from the vertebral body is used to fill the inside and outside of the cage. The β-TCP plug is a ceramic void filler that contains calcium and phosphorus, two of the main mineral constituents of the bone. This osteoconductive material has been used in Europe for more than 20 years, mostly as a void filler in general orthopedic indications. The effect on the mechanical strength of the lumbar vertebra, with a cylindrical regional bone graft removed, was studied in a cadaveric model by Steffen and his coauthors [17]. After plug removal and TCP plug filling, the vertebral body’s strength in flexion/compression loading was increased compared to its intact values. Another paper demonstrated complete osteointegration to the TCP plug at 6 months post-op by a biochemical and histological animal study in sheep and baboons [18]. However, because of the presence of the TCP plug, the use of pedicle screw fixation for stabilization is theoretically contraindicated. The goal of the study was, therefore, to report our initial experience looking at the feasibility of such techniques in vivo, taking into account the need of an extended dissection of the vertebra, the intraoperative complications and blood loss, and to assess the functional and radiographic result during the minimum 2-year follow up interval.
Materials and methods
This is a report on our first 21 consecutive patients who were planned to undergo circumferential spine fusion with an anterior cage filled with autologous bone coming from the adjacent vertebral body and a Chronos® plug to fill the void. Nine patients were classified as having a spondylolisthesis, eight with discogenic low back pain, two with degenerative scoliosis, one with post-traumatic kyphosis at L5, and one revision of previous non-union at L4–L5. There were 16 females and 5 males. The average age of the patients was 39.9 years (range 26–57). All of the patients underwent posterior pedicle screw fixation. All of these cases were performed at the same university institution by four trained spine surgeons. Data collection had been done prospectively. After a minimum of 2 years follow up, our initial 21 patients were reviewed for quality insurance of this technique and publication. The patients’ office and hospital medical charts, as well as radiographs before surgery, after surgery and at the final follow up were reviewed by an independent surgeon (L.J.).
To assess the intraoperative feasibility, all OR reports were reviewed with special attention to difficulties of exposure, blood loss from the anterior surgery, vascular complications, end plate fracture or other possible side effects.
The radiologic results were assessed on standing lumbar spine X-rays AP and lateral and flexion extension dynamic radiographs at 6, 12 and 24 months. The fusion was judged solid when less than 4° of difference was measured on the flexion–extension lateral X-rays, when there was an absence of radiolucency around the pedicle screws, and/or there was presence of bone trabeculae in front of or behind the cage. A pseudoarthrosis was defined as any motion superior to 4° on flexion–extension and or radiolucency around the pedicle screws.
Other radiographic parameters, such as vertebral disc space height, were measured to assess for subsidence. Other characteristics such as endplate fracture or plug fracture were also assessed. Likewise, integration of the β-TCP plug was judged on AP and lateral X-rays by its radiographic disappearance. We measured the posterior vertebral body height on the lateral radiograph as controlled parameter to obviate the bias from radiological magnification.
The clinical results were assessed by looking at the Oswestry disability index (ODI) and the visual analog scale (VAS) at 6 months, 1 year, 2 years, and at final follow up.
Surgical techniques (Figs. 1, 2, 3, 4, 5)
Fig. 1.
Surgical technique. After exposure of the vertebral body a K-wire guide for the trephine system is inserted in the vertebral body
Fig. 2.
The trephine is mounted over the K-wire guide and preset for removing a 25 mm long by 15 or 17 mm wide core
Fig. 3.
The trephine system will harvest the 25 mm by 15 or 17 mm core cancellous plug
Fig. 4.
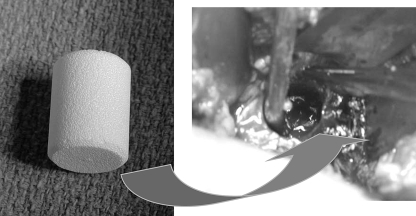
The β-TCP plug is inserted in the void defect
Fig. 5.
The cancellous autograft harvested from the vertebral body is impacted in the cage
The lumbar spine was classically exposed through a left-sided retroperitoneal approach. Initially the approach was done lateral to the rectus sheet and then medial to the rectus sheet in order to prevent denervation of the rectus muscle. A fixed ring retractor system (Synframe, Synthes, Paoli, PA, USA) was routinely used in order to minimize the size of the incision and maximize the exposure [1]. At the L5 level, after ligation of the midsacral artery, the bifurcation was dissected in a cephalad direction and retracted with a blade of the ring retractor to allow exposure of the inferior 3/4 of the L5 vertebral body. At the L4–L5 level, the iliolumbar vein was exposed and ligated in all cases but three in order to mobilize safely the bifurcation to the right. For the three cases that did not require ligation the iliolumbar was either not found or judged not to be under tension during the retraction of the bifurcation. A combination of blades or Hohman retractors and/or Steinman pins was used to expose the inferior 3/4 of the L4 vertebral body. The L3–L4 level did not pose any surgical problem and was easiest to access.
Once sufficient exposure was obtained, a standard discectomy was performed. The rest of the technique is similar to the one described by Kumar [11]. A manual trephine was guided over a centrally placed K-wire and a 15 or 17 mm bone cylinder from the exposed vertebral body was removed. Only one case had a 17 mm core removed from the adjacent vertebral body (Figs. 1, 2, 3). The position of the K-wire was always checked under lateral C-arm fluoroscopy to make sure that drilling would not end in the disc space above or below. The K-wire was therefore placed centrally or slightly inferiorly. The depth of the core cylinder that was removed was always set at 25 mm. Due to the possible bleeding observed during removal of the cancellous bone plug, immediate filling of the defect was then carried out with a 15 or 17 mm diameter cylindrical TCP plug using the ancillary equipment of the trephine instrumentation (Fig. 4).
A titanium cage was filled with the bone coming from the harvested core cylinder and impacted in the disc space (Fig. 5). The retractors were then removed with careful attention to hemostasis.
After anterior surgery, under the same anesthesia the patient was positioned in the prone position and a posterior fusion with pedicle screws was done either through a Wiltse or a standard midline approach depending on the need of spinal decompression. Local bone graft and facet decortication were done for the posterior fusion. To avoid dislodging the Chronos® plug during our pedicle screw insertion, we were careful to either insert short pedicle screws or to insert them just above the Chronos® plugs underneath the endplate. This was best achieved under lateral C-arm fluoroscopy. However in one of our consecutive cases, the screws were inserted so they projected at the level of the TCP plug. This had no adverse effect. As our level of confidence increased, we inserted the screws regardless of the position of the plug without observing any adverse effects such as plug expulsion or plug fracture.
In the first three cases, posterior fixation was carried out as the first stage with special care for placement of the screws so they would not preclude the placement of the trephine anteriorly. This was judged too difficult and illogic after our first three cases. The sequence posterior fixation first with pedicle screws was therefore abandoned for this reason and the fact that the discectomy, the impaction of the cage and the restoration of optimum lordosis were made far more difficult than the anterior–posterior sequence.
Results
Feasibility
Twenty-one consecutive patients underwent this procedure. Two patients could not be reached after the 1-year follow up. All the other patients have been followed for at least 2 years. The results of the two patients who were followed after only 1 year were kept in the study as the clinical evolution and radiographs were identical to the other patients and their pain score was similar at 1 year follow up. The mean follow up was 28 months (range 12–41 months). Only one patient (5%) did not have the Chronos® plug harvested because of the difficulty of access to L5 vertebral body due to a low and large left iliac vein. In the other 20 cases, 33 cages were inserted and 28 β-TCP plugs were used to fill the cylinder vertebral body defects. For the corresponding five other five levels, additional filling of the cage was supplemented with Chronos® granules as there was not enough cancellous bone obtained from one vertebral body to fill two cages. The plug was always harvested from the vertebra above the fused intervertebral space: At L5 for seventeen L5/S1 fusions, at L4 for eight L4/L5 fusions and at L3 for three L3/L4 fusions. For the anterior surgery, the mean blood loss was 250 (range 50–350) ml. The mean operative time was 154 (range 80–240) min with the 240 min corresponding to the three-level anterior fusion. The mean hospitalization period was 6 (range 2–9) days.
Complications
We did not observe extrusion of any Chronos® plugs during the insertion of pedicle screws even when they were superimposed over the shadow of the plug under fluoroscopy. One patient had a right lumbar plexopathy which was thought to be the result of traction injury or misplaced Hohman retractor during the anterior surgery with the thighs in hyperextension. After this complication the thighs were kept in neutral position during the exposure. The patient’s lumbar plexopathy resolved almost completely after 12 months. There was no case of infection or retrograde ejaculation. One patient with spondylolisthesis was diagnosed with deep venous thrombosis at the calf level 2 weeks after surgery and was treated successfully with coumadine. There was no major vascular injury. In one case the vena cava was punched inadvertally by a K-wire, and the bleeding was stopped by compression with thrombine soaked sponge.
Radiographic results
There was no pseudoarthrosis: All flexion–extension radiographs showed less than 4° of mobility measured. There was no instance of halo ring sign around the pedicle screws. Bridging of the disc space with bone in front of behind the cage was present in 15 cases. One TCP plug was broken during its impaction as there was only an incomplete removal of the bone core (the removed core measured only 15 mm instead of the required 25 mm). One endplate was broken during the surgical insertion of the cage that was retrospectively judged too large for the disc space. This had no effect on the outcome as it was the inferior endplate included in the instrumentation. The integration of the TCP plug had typical characteristics with progression to a complete disappearance at 2 years in all the cases (Fig. 6).
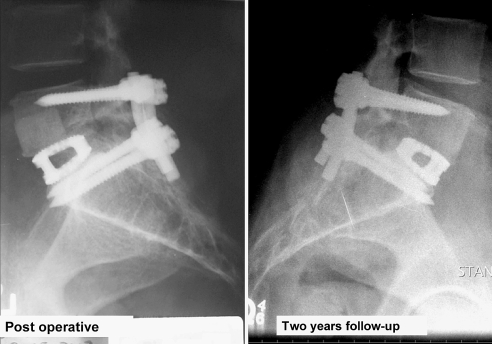
Fig. 6.
Radiographs after an anterior and posterior L5–S1 fusion for axial low back pain: the β-TCP plug is well visible on the postoperative X-rays (left) and is no longer visible at 2 years follow up (right)
The mean preoperative lordotic disc angle was −10.5° (−5° to 25°), which increased to −15.1° (−5° to 28°) post-operatively, and was −14.8° (−5° to 27°) at the final follow up. There was no case of cage settling during the follow up period as measured by the anterior and posterior disc space height. There was no case of cage migration.
Functional and clinical results
Back pain was reduced in this consecutive series of patients. Only 18 patients had a complete ODI and VAS score reported. For the two patients who were lost in follow up after 1 year, the final data was missing but was not different at the 1 year follow up so we decided to report the cases. Back pain as reported on the VAS decreased from a preoperative mean of 6.9 (4–9) to 4.5 at 6 months follow up, or a 33% decrease. Likewise the ODI reduced from 48 to 31.7 (34% decrease) at the same follow up. At 2 years follow up there was a trend for increase in the VAS and ODI (respectively 5 and 35). The improvement in pain was more dramatic in patients with spondylolisthesis than in patients with degenerative disc disease.
Discussion
The history of lumbar spine fusion has progressively moved from non-instrumented spine fusion to fusion with pedicle fixation and lately with circumferential fusion. To decrease the morbidity of iliac crest bone graft, cage technology and bone substitutes have progressively become more and more widespread [5, 9]. Harvesting autologous bone from the vertebral body itself and replacing the void by a TCP plug has been proven successful in the animal model [17, 18]. However, its validity in clinical practice has not been proven and the use of posterior screw fixation is theoretically a contraindication of the technique. The technique was originally described for translaminar screw fixation. However, in our hands the best restoration of a normal segmental lordosis is best achieved with anterior discectomy and anterior column support first followed by posterior screw fixation. This is the reason why we have used a posterior screw fixation in all our cases.
Our results clearly demonstrate that the concept is valid clinically as we have obtained a 100% fusion rate with perfect maintenance of the lordosis. Further experience with an additional 25 cases with less than 2 years follow up has confirmed the validity of our technique as we have not encountered any major complications related to the technique itself.
One of the concerns of posterior screw fixation is the possibility of dislodging the TCP plug during pedicle screw insertion or breakage of the plug with subsequent collapse of the vertebral body. We did not observe any of this which could be explained by the fact that the screws are lateral in the vertebral body whereas the plug is central. Also, the screws and the plug are inserted in different orientation: straight sagittal for the TCP plug, toeing in 15°–25° for the pedicle screws. The risk of impinging on the TCP plug with the pedicle screw exists but is of little consequence in our opinion as the friable nature of the TCP plug would accept the pedicle screw. Since the TCP is contained within its cavity, we do not think this is an issue. During the posterior pedicle screw insertion, the possible expulsion of the TCP plug was watched carefully under lateral C-arm fluoroscopy, but it never occurred in any of our cases.
On the other hand, if machined cortical allograft like the Vertefill® (Synthes, Paoli, PA, USA) is used as a void filler in the vertebral body, the use of pedicle screw fixation is only possible if they are inserted above the Vertefill® plug, otherwise they may push the cortical allograft. For this reason we do not recommend the use of the Vertefill® if one uses pedicle screw fixation.
With the advent of BMP, one has seen a trend to generalization of its use. The success of lumbar spine fusion using BMP has been reported to be higher than the use of autograft [4], although BMP side effects seem to be very minimal, at least in the short term concern for heterotopic bone formation close to the neural elements, antibodies formation up to 38%, yet of unknown significance, and destruction of the bony endplate leading to subsidence being reported [8, 15]. Recently, the use of BMP in anterior cervical spine fusion has been discouraged due to inflammatory reaction and dysphagia (unpublished data at the time of writing). Uncertain long-term outcome of BMP-2 fusion and its high costs has kept us from its use in lumbar spine fusion [6]. The TCP plug is an attractive osteoconductive ceramic graft material that closely mimics the inorganic bone, acts as a scaffold for osteogenic cells, and slowly incorporates to be replaced by normal cancellous bone after implantation [6]. Furthermore, there is no risk of disease transmission or immunogenic response, the sterilization and shelf storage are easy, and there is infinite supply. Long-term clinical side effects of other bone substitute or osteoinductive material do not have such a track record. Our β-TCP plugs have all incorporated within 1–2 years on the lumbar spine radiographs (Fig. 6). This is consistent with their histological absorption and incorporation reported in the long bones [6].
The surgical exposure might be the most challenging part of this technique due to the increased possibility of neurovascular complications. Compared to the standard surgical approaches in performing an interbody arthrodesis, this technique requires more extensive exposure and is surgically more demanding. In our experience, the exposure could be more safely achieved with the help of a fixed ring retractor system. In one case (5%) access to the bifurcation was judged too dangerous to perform the anterior fusion and the case was converted to a posterior fusion with TLIF. In one case we had a small venous injury that could be stopped with thrombine soaked sponges. Such an injury may have been related to the extended dissection required to access the whole vertebral body. These two complications make us recommend this technique only to surgeons with extensive training in ALIF as the approach may be a little more challenging than the one required for a simple cage insertion.
Conclusion
The data in this pilot study suggest that harvesting with a trephine and autograft core from the adjacent vertebral body and filling the void with a β-TCP plug is safe and effective for ALIF with cage. Posterior stabilization with posterior pedicle screw fixation is not a contraindication of the technique.
References
- 1.Aebi M, Steffen T (2000) Synframe: a preliminary report. Eur Spine J 9(Suppl 1):S44–S50 [DOI] [PMC free article] [PubMed]
- 2.Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P (2002) Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 84-A(5):716–720 [DOI] [PubMed]
- 3.Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20(9):1055–1060 [DOI] [PubMed]
- 4.Burkus JK, Sandhu HS, Gornet MF, Longley MC (2005) Use of rhBMP-2 in combination with structural cortical allografts: clinical and radiographic outcomes in anterior lumbar spinal surgery. J Bone Joint Surg Am 87(6):1205–1212 [DOI] [PubMed]
- 5.Fritzell P, Hägg O, Wessberg P, Nordwall A, the Swedish Lumbar Spine Study Group (2001) Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish Lumbar Spine Study Group. Spine 27:1131–1141 [DOI] [PubMed]
- 6.Gaasbeek RD, Toonen HG, van Heerwaarden RJ, Buma P (2005) Mechanism of bone incorporation of beta-TCP bone substitute in open wedge tibial osteotomy in patients. Biomaterials 26(33):6713–6719 [DOI] [PubMed]
- 7.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML (1997) Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop 339:76–81 [DOI] [PubMed]
- 8.Harwood PJ, Giannoudis PV (2005) Application of bone morphogenetic proteins in orthopaedic practice: their efficacy and side effects. Expert Opin Drug Saf 4(1):75–89 [DOI] [PubMed]
- 9.Janssen ME, Lam C (2001) Outcomes of allogenic cages in anterior and posterior lumbar interbody fusion. Eur Spine J 10(Suppl 2):S158–S168 [DOI] [PMC free article] [PubMed]
- 10.Kozak JA, O’Brien JP (1990) Simultaneous combined anterior and posterior fusion. An independent analysis of a treatment for the disabled low-back pain patient. Spine 15(4):322–328 [DOI] [PubMed]
- 11.Kumar N, Wild A, Webb JK, Aebi M (2000) Hybrid computer-guided and minimally open surgery: anterior lumbar interbody fusion and translaminar screw fixation. Eur Spine J 9(Suppl 1):S71–S77 [DOI] [PMC free article] [PubMed]
- 12.Lord CF, Gebhardt MC, Tomford WW, Mankin HJ (1988) Infection in bone allografts. Incidence, nature, and treatment. J Bone Joint Surg Am 70(3):369–376 [PubMed]
- 13.Pavlov PW, Meijers H, van Limbeek J, Jacobs WC, Lemmens JA, Obradov-Rajic M, de Kleuver M (2004) Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine 29(17):1893–1899 [DOI] [PubMed]
- 14.Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR (2005) Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. Spinal Disord Tech 18(4):337–346 [DOI] [PubMed]
- 15.Pradhan BB, Delamarter R, Patel V, Bae H, Dawson E. Can rhBMP-2 (InFuse) Enhance fusion rates in anterior lumbar interbody fusion using stand-alone femoral ring allografts? Presented at the Scoliosis Research Society Buenos Aeres 2004
- 16.Sasso RC, LeHuec JC, Shaffrey C, Spine Interbody Research Group (2005) Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech 18(Suppl):S77–S81 [DOI] [PubMed]
- 17.Steffen T, Downer P, Steiner B, Hehli M, Aebi M (2000) Minimally invasive bone harvesting tools. Eur Spine J 9(Suppl 1):S114–S118 [DOI] [PMC free article] [PubMed]
- 18.Steffen T, Stoll T, Arvinte T, Schenk RK (2001) Porous tricalcium phosphate and transforming growth factor used for anterior spine surgery. Eur Spine J 10(Suppl 2):S132–S140 [DOI] [PMC free article] [PubMed]
- 19.Sutherland AG, Raafat A, Yates P, Hutchison JD (1997) Infection associated with the use of allograft bone from the north east Scotland Bone Bank. J Hosp Infect 35(3):215–222 [DOI] [PubMed]
- 20.Tay BB, Berven S (2002) Indications, techniques, and complications of lumbar interbody fusion. Semin Neurol 22(2):221–230 [DOI] [PubMed]