Abstract
There is compelling evidence supporting the benefits of increased regular physical activity in older adults. The Experience Corps program in Baltimore MD was designed in part as a community based approach to increasing physical activity that would also appeal to older adults who have historically not utilized health promotion programs. The Baltimore Experience Corps program places older volunteers in public elementary schools for 15 h a week in roles designed to improve the academic outcomes of children and, simultaneously, increase the physical, cognitive and social activity of volunteers. This paper reports on the change in physical activity levels among older adults associated with participation in the Baltimore Experience Corps. In a pilot randomized controlled evaluation, older adults were randomly assigned to Experience Corps (EC participants) or a waiting list control group. Ages ranged from 59–86 years, 96% were African American, 94% were women, and 84% had annual incomes less than $15,000. EC participants were required to serve ≥15 h a week. At follow-up after 4–8 months, an analysis of 113 randomized volunteers revealed 53% of the EC participants were more active than the previous year by self-report, as compared to 23% of the controls (p<0.01). When adjusted for age, gender and education, there was a trend toward increased physical activity in the EC participants as calculated by a kilocalorie per week increase of 40%, versus a 16% decrease in the controls (p=0.49). EC participants who reported “low activity” at baseline experienced an average 110% increase in their physical activity at follow-up. Among the controls who were in the “low activity” group at baseline, there was, on average, only a 12% increase in physical activity (p=0.03). Among those who were previously active, there was no significant difference (p=0.30). The pilot results suggest that a high intensity volunteer program that is designed as a health promotion intervention can lead, in the short-term, to significant improvements in the level of physical activity of previously inactive older adult volunteers.
Keywords: Volunteerism, Retirement, Exercise, Health disparities, Randomized controlled trial, Experience Corps, African American, Physical activity, Task force on community preventive services, Intervention
Background
Despite the evidence that physical activity remains important to health outcomes through the oldest ages,1–8 and that previous research has demonstrated that moderate physical activity is as beneficial as more intense exercise,3,4,8 rates of regular physical activity are low, particularly for older adults.9 Additionally, physical activity interventions have been most successful in recruiting healthier and more highly functioning individuals from more financially well-off communities.10–13 America needs novel approaches to increase the physical activity of all older adults before the ranks of Americans aged 65 and older increases from 40 million in 2010 to 70 million in 2030.14,15 Further, campaigns to increase the physical activity of all Americans must include interventions that appeal to all communities so that health disparities are reduced—not increased.16
To address the need to expand the repertoire of community-based strategies for increasing physical activity in our aging population, we theorized that some older adults might be more readily attracted to the generative roles of an intergenerational volunteer program than to a health promotion program.17 Volunteering has a long tradition in the United States.18 Approximately 25% of Americans over the age of 65 currently engage in some volunteer work.19 Health promotion interventions that have been designed as civic engagement programs have the potential for broad appeal. Volunteering has been associated, in observational studies, with lower mortality and disability rates and improved self-assessed health.20–27 This could be a result of the psychosocial benefits associated with productive roles past retirement.28,29 However, volunteering can also serve as an intervention to enhance physical activity. When quantified as a multiple of the basal metabolic rate (METS), volunteer activities can compare favorably with traditional leisure activities in terms of energy expenditure. For example, moderate play with children as a volunteer activity has the same METS as T'ai ch'i, while weeding and planting trees or shrubs provides more METS than golfing.30 However, volunteering could simply be a marker for other characteristics that are predictive of good health outcomes, and the effectiveness of volunteering as a public health intervention needs to be evaluated in an experimental setting.
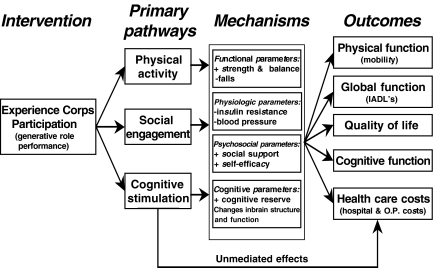
Experience Corps is a community-based model for health promotion in older adults that is embedded within a high-impact volunteer program that has the potential to simultaneously improve the academic outcomes for children in public elementary schools while supporting older adult volunteer adherence to a physically active lifestyle.14,31–34 A previously published study reported academic and behavioral benefits for children in schools with the Experience Corps.33 If intergenerational volunteer programs were to have just a small effect on the number of students graduating from high school, programs like Experience Corps could produce a net savings for society.35 This model has the additional potential to address disparities in health, as it has been successful in recruiting and retaining historically underserved minority group members, particularly African American older adults,31,36 a population that experiences higher rates of frailty, disability, morbidity and mortality.37–40 Increased physical activity is one of the primary pathways through which Experience Corps was theorized to benefit the health and function of older adults (See Figure 1),31 as a result of ambulation to and from and within schools three to five times a week. As previously published, a randomized controlled pilot trial demonstrated initial evidence of increased physical, social and cognitive activity among Experience Corps participants as compared to controls.31 We hypothesized that Experience Corps participants who were initially physically inactive might benefit most from the program, building on reports of previously successful physical activity interventions that specifically recruited sedentary adults.11,41 This paper offers the further evidence as to whether high intensity volunteering (15 h or more per week through a whole school year) can meaningfully increase physical activity in urban older adults who were previously inactive.
Figure 1.
Conceptual framework for the Experience Corps program.
Materials and Methods
Description of the Intervention, Subjects, and Data Source
In the Experience Corps Baltimore program, teams of volunteers aged 60 and older are placed in Kindergarten through third grades in Baltimore public elementary schools. Each of the volunteers serves for a minimum of 15 h a week with a commitment to complete the full school year, in such roles as one-on-one or small group literacy support, library support, violence prevention activities, attendance enhancement and/or other formal roles in which they are trained. To affect school climate and academic outcomes for entire grades, each school receives a critical mass of volunteers, averaging 20 per school. A summary of the design of the program and the analysis of the general findings have been previously published.14,31
This report analyzes data from an eight-month-long pilot randomized, controlled trial in which volunteers were placed in three intervention schools during the 1999–2000 school year. Volunteers agreed to be randomized to the Experience Corps program (EC participants) or to be on a waiting list for 1 to 2 years before being offered the opportunity to serve in Experience Corps (controls). Recruitment messages and strategies focused on opportunities for older adults to use their life experiences to make a difference for children in public elementary schools. Over 4 months, 297 potential volunteers were screened, of whom 159 agreed to be evaluated for eligibility. Of those that completed the baseline evaluation, 148 agreed to participate and were randomized to either be an EC participant or a control in three sequential groups of approximately 50. After randomization, 20 dropped out, leaving 70 as EC participants and 58 as controls. All participants were evaluated at baseline prior to randomization and were asked to return for follow-up after the end of the academic year (June or July). Length of follow-up in this first year was 4 to 8 months, depending on the date of enrollment. One hundred twenty-five older adults completed the first year follow-up. This included 69 EC participants and 56 controls. Of those that completed the follow-up, nine of the EC participants and two of the controls were missing physical activity data at either baseline or follow-up and were excluded from this analysis. One additional EC participant was wheelchair-bound at baseline and was not included in this analysis. Ultimately, 113 subjects were used for this analysis: 59 EC participants and 54 controls.
An analysis, stratified by original randomization assignment, was done comparing the baseline characteristics of the 113 used for this analysis and the 35 who were randomized but not included; among the latter 35, 17 were assigned to EC, while 18 were assigned to the control arm. When compared to the 18 control participants who were excluded in this analysis, the 54 controls were more likely to be female (78% of the excluded controls were women, as compared to 96% of those included, p=0.03) and more likely to be African American (78% of the excluded controls were African American, as compared to 96% of those included, p=0.03). However, there was no difference in the mean age, education or health status of the controls who were included and excluded from the analysis. When compared to the 17 EC participants who were excluded in this analysis, the 59 EC participants demonstrated no difference in terms of mean age, gender, race, education, or self-assessed health status (77% of the excluded EC participants were women, as compared to 92% of those included, p=0.09, while 94% of the excluded EC participants were African American, as compared to 97% of those included, p=0.54).
Measurement
Standardized evaluations at baseline and follow-up after the end of the academic school year consisted of physical measurements, self-administered questionnaires, and interviewer-administered questionnaires regarding demographic characteristics, health, functional status and physical activities in the prior 2 weeks. While research interviewers were blinded to the randomization assignment of subjects, the subjects were not blinded. The primary outcome, physical activity, was measured at baseline and follow-up using the modified Minnesota Leisure Time Physical Activity Questionnaire (MLTPAQ),42 which measures the frequency and duration of participation in the past 2 weeks in any of 15 physical activities that older adults are likely to engage in. These physical activities are walking for exercise, moderately strenuous housework, mowing the lawn, raking the lawn, gardening, dancing, aerobics/aerobic dance, bowling, golf, calisthenics/general exercise, and swimming. Each activity was characterized in terms of minutes per week and in kilocalories expended per week. Leisure time physical activity was summarized into four sub-categories: 1) walking for exercise; 2) household chores: moderately strenuous housework, mowing the lawn, raking the lawn; 3) exercise: hiking, jogging, biking, exercise cycle, aerobics/aerobic dance, calisthenics/general exercise, and swimming; and 4) recreational activity: dancing, bowling and golf. The following questions from the Paffenbarger physical activity questionnaire were also asked and analyzed: “During the last week about how many city blocks or miles did you walk?” and “In the last week, how many flights of stairs did you climb?” Overall perceived activity was assessed by asking “How would you describe your level of activity since last year?”43
Analyses
The effectiveness of randomization, baseline characteristics of the intervention volunteers and the controls, and the effects of the EC intervention were assessed using the t-test and chi-square test, as appropriate. Overall and specific activities were compared between intervention and control groups, analyzing change from baseline to follow-up in minutes per week and in kilocalories expended per week. Mean physical activity per week was calculated as a geometric mean, to discount the effect of outliers on the measurement of central tendency. To test the hypothesis that previously inactive older adults would demonstrate increased activity, analyses were stratified according to baseline activity level: Active EC participants and controls were defined as those who, at baseline, reported at least ten episodes in the last 2 weeks of moderate physical activity of at least 30 min duration; the remainder being classified as “low activity”. This cut-off reflects the physical activity goals for Healthy People 2010: five episodes per week of moderate physical activity for at least 30 min at a time.(2) Volunteers were evaluated with the same criteria on follow-up. Analyses were adjusted for confounders, including age, gender, race, education and self-reported health status, in multivariate linear regression models in which changes between baseline and follow-up were the outcome or in multivariate logistic regression models in which percentage that were more physically active than last year was the outcome.
Results
The characteristics of older adults who volunteered for the Baltimore Experience Corps and were randomized (overall and by randomization status) and completed follow-up are shown in Table 1. Participants were 59 to 86 years of age, with a mean age of 69. There was no difference between the EC participants and controls in terms of age, gender, education, income, percentage married, or the percentage who were African American. While higher percentages of the controls reported fair or excellent health than did those in the intervention group, no one in either group reported poor health. Approximately two-thirds of each group reported difficulty with mobility, with no significant differences between the two groups: Overall 60% reported difficulty walking up stairs, and 35% reported difficulty walking several blocks, while 15% reported using a cane or walker.
Table 1.
Baltimore Experience Corps: characteristics of participants of the pilot randomized trial by treatment group
| Overall (N=113) % | EC participants (n=59) % | Controls (n=54) % | p value | ||
|---|---|---|---|---|---|
| Age | 59–65 | 31 | 30 | 32 | 0.05 |
| 66–70 | 35 | 25 | 46 | ||
| 71–75 | 28 | 37 | 18 | ||
| >75 | 7 | 9 | 4 | ||
| Gender | Female | 94 | 92 | 96 | 0.29 |
| Race | African-American | 96 | 97 | 96 | 0.91 |
| Other | 4 | 3 | 4 | ||
| Education | High school or less | 84 | 83 | 85 | 0.76 |
| Income | <$15,000 per year | 69 | 65 | 74 | 0.31 |
| Marital status | Married | 23 | 24 | 23 | 0.89 |
| Health status (self assessed) | Excellent/Very good | 27 | 24 | 30 | 0.03 |
| Good | 61 | 71 | 50 | ||
| Fair | 12 | 5 | 20 | ||
| Poor | – | – | – | ||
| Number of chronic conditions: mean | 2.6 | 2.6 | 2.6 | 0.95 | |
| Health conditions diagnosed by a physician | Hypertension | 66 | 64 | 69 | 0.59 |
| Arthritis | 53 | 48 | 59 | 0.26 | |
| Vision problems | 46 | 36 | 57 | 0.03 | |
| Diabetes | 24 | 28 | 18 | 0.24 | |
| Cancer | 6 | 7 | 4 | 0.54 | |
| Angina | 7 | 7 | 7 | 0.92 | |
| Hearing problems | 5 | 7 | 2 | 0.26 | |
| Lung disease | 11 | 12 | 10 | 0.71 | |
| Stroke | 2 | 4 | 0 | 0.18 | |
| Congestive heart failure | 4 | 4 | 4 | 0.85 | |
| Heart attack | 3 | 5 | 0 | 0.10 | |
| Hip fracture | 2 | 3 | 0 | 0.19 | |
| Difficulty in | Climbing stairs | 60 | 55 | 65 | 0.31 |
| Walk several blocks | 35 | 29 | 42 | 0.15 | |
| Managing money | 7 | 7 | 6 | 0.83 | |
| Used cane | 15 | 14 | 16 | 0.72 | |
| Mini-mental mean score | 25.4 | 25.5 | 25.3 | 0.71 | |
There was no significant difference in physical activity levels between the intervention and control groups overall at baseline. At baseline, 20 EC participants (39%) and 13 controls (24%) were physically active, while 48 EC participants and 41 controls were in the “low active” group (p=0.55).
At follow-up after 4 to 8 months, the EC participants reported an increase in the mean minutes expended per week in physical activities, from 220 to 270 min/week, while the controls decreased from 170 to 140. This was not a significant difference, although this pilot study was not powered to detect a difference. There were related trends in terms of kilocalories expended, increasing 40% in the EC participants, while there was a decrease of 16% in the controls; this was also not statistically different. Overall, the only area of “leisure time” activities assessed in which there was a significantly different change between intervention group and controls was in kilocalories expended on household chores each week, which doubled in the intervention group with no change in controls (p=0.02 unadjusted and p=0.07 adjusted). On follow-up, 40% of the EC participants met physical activity guidelines, compared with 25% of the controls (p=0.46) (Table 2a and Figure 2).
Table 2a.
Change in physical activity over 4–8 months follow-up, EC participants vs. controls, adjusted and unadjusted analysis, (N=113)
| EC participants n=59 | Controls n=54 | p value unadjusted | p value adjusted * | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||
| Physical activity/week in mean minutes/week | 220 | 270 | 170 | 140 | 0.17 | 0.44 |
| Physical activity/week in mean kcal/week | 810 | 1,130 | 670 | 560 | 0.29 | 0.52 |
| Walking for exercise/week1 (mean kcal/week) | 60 | 50 | 50 | 60 | 0.44 | 0.88 |
| Household chores/week2 (mean kcal/week) | 120 | 240 | 100 | 110 | 0.02 | 0.07 |
| Exercise/week3 (mean kcal/week) | 20 | 10 | 10 | 0 | 0.18 | 0.11 |
| Leisure activity/week4 (mean kcal/week) | 10 | 10 | 10 | 10 | 0.22 | 0.44 |
| Percentage who are active** | 34% | 40% | 24% | 25% | 0.46 | 0.70 |
Means were calculated as geometric means.
*Adjusted by age, gender, race, education and health status in a multivariate linear regression model
**Active individuals were defined as those who, at baseline, reported at least ten episodes in the last 2 weeks of moderate physical activity of at least 30 min duration, while inactive or “low activity” individuals were those with less activity.
1) Walking for exercise; 2) House hold chores was comprised of moderately strenuous housework, mowing the lawn, raking the lawn; 3) Exercise was comprised of hiking, jogging, biking, exercise cycle, aerobics/aerobic dance, calisthenics/general exercise, and swimming; and 4) Recreational activity was comprised of dancing, bowling and golf.
Figure 2.
Box plot of change in physical activity from baseline to follow-up: (Mean increase or decrease in kilocalories expended per week).
We then stratified by baseline physical activity, distinguishing those whose baseline activity met guidelines for being physically active versus those who had lower (or “low”) activity. As shown in Table 2b and Figure 2, among those who had low activity at baseline, EC participants reported a doubling of time spent in physical activity per week at follow-up, compared to no change among controls (p=0.05 adjusted). Correspondingly, there was an increase of kilocalories expended from 420 to 880 kcal/week among the intervention group, again with no change among controls (p=0.03, adjusted). This amounted to an average increase of 460 kcal/week in the intervention group. Despite this increase in activity in the group with initially low activity, there was no difference at follow-up in the proportion of cases or controls who were meeting formal criteria for being “physically active”: both groups showed an increase from 0% to 26% (p=0.80 adjusted).
Table 2b.
Change in physical activity among subjects initially in the “low activity” group** over 4–8 months follow-up, EC participants vs. controls, adjusted and unadjusted analysis, (n=80)
| EC participants n=39 | Controls n=41 | p value unadjusted | p value adjusted * | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||
| Physical activity/week in mean minutes/week | 120 | 210 | 120 | 130 | 0.02 | 0.05 |
| Physical activity/week in mean kcal/week | 420 | 880 | 490 | 500 | 0.01 | 0.03 |
| Walking for exercise/week1 (mean kcal/week) | 20 | 30 | 20 | 60 | 0.66 | 0.95 |
| Household chores/week2 (mean kcal/week) | 70 | 240 | 90 | 110 | <0.01 | <0.01 |
| Exercise/week3 (mean kcal/week) | 10 | 10 | 0 | 0 | 0.72 | 0.83 |
| Leisure activity/week4 (mean kcal/week) | 0 | 10 | 10 | 10 | 0.85 | 0.84 |
| Percentage who are active** | 0% | 26% | 0% | 26% | 0.95 | 0.80 |
Means were calculated as geometric means.
*Adjusted by age, gender, race, education and health status in a multivariate linear regression model.
**Active individuals were defined as those who, at baseline, reported at least ten episodes in the last 2 weeks of moderate physical activity of at least 30 min duration, while inactive or “low activity” individuals were those with less activity.
1) Walking for exercise; 2) House hold chores was comprised of moderately strenuous housework, mowing the lawn, raking the lawn; 3) Exercise was comprised of hiking, jogging, biking, exercise cycle, aerobics/aerobic dance, calisthenics/general exercise, and swimming; and 4) Recreational activity was comprised of dancing, bowling and golf.
In contrast, among those who met physical activity guidelines at baseline, both those randomized as EC participants and controls reported decreases in their usual physical activity at follow-up, 4–8 months later. However, as shown in Table 2c and Figure 2, the intervention group reported less decline overall, with a 38% decrease in kilocalories per week expended in leisure activity while the controls reported a 70% decrease, on average. Despite the markedly lesser decrease in activity in the intervention group, there was no statistically significant difference between these changes, likely due to small sample sizes. There was a similar difference at follow-up in the proportion meeting criteria for physical activity guidelines, with less of a decline among the intervention group reporting meeting criteria, to 65%, compared to a decline to 20% of controls (p=0.02 unadjusted and 0.17 adjusted).
Table 2c.
Change in physical activity among subjects initially in the “active” group** over 4–8 months follow-up, EC participants vs. controls (n=33)
| EC participants n=20 | Controls n=13 | p value unadjusted | p value adjusted * | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||
| Physical activity/week in mean minutes/week | 690 | 430 | 530 | 160 | 0.62 | 0.49 |
| Physical activity/week in mean kcal/week | 2,970 | 1,840 | 2,130 | 640 | 0.92 | 0.37 |
| Walking for exercise/week1 (mean kcal/week) | 480 | 140 | 720 | 90 | 0.21 | 0.54 |
| Household chores/week2 (mean kcal/week) | 330 | 240 | 180 | 120 | 0.75 | 0.58 |
| Exercise/week3 (mean kcal/week) | 250 | 60 | 30 | 10 | 0.16 | 0.13 |
| Leasure activity/week4 (mean kcal/week) | 70 | 30 | 10 | 0 | 0.35 | 0.91 |
| Percentage who are active** | 100% | 65% | 100% | 20% | 0.02 | 0.17 |
Means were calculated as geometric means.
*Adjusted by age, gender, race, education and health status in a multivariate linear regression model
**Active individuals were defined as those who, at baseline, reported at least ten episodes in the last 2 weeks of moderate physical activity of at least 30 min duration, while inactive or “low activity” individuals were those with less activity.
1) Walking for exercise; 2) House hold chores was comprised of moderately strenuous housework, mowing the lawn, raking the lawn; 3) Exercise was comprised of hiking, jogging, biking, exercise cycle, aerobics/aerobic dance, calisthenics/general exercise, and swimming; and 4) Recreational activity was comprised of dancing, bowling and golf.
Participants were asked at follow-up “How would you describe your level of activity since last year?” As seen in Table 3, a greater proportion of EC participants reported either being “a little more active” or “a lot more active” (53%), as compared to controls (23%); this difference was significant overall (p<0.01 adjusted). The difference was most notable for those who, at baseline, reported activity levels lower than recommended by current guidelines; 49% of the EC participants reported being more active, versus 18% of controls (p=0.05 adjusted). There were similar trends at follow-up among those whose activity levels met recommended guidelines at baseline, but this did not reach statistical significance.
Table 3.
Percentage reporting increased physical activity on follow-up as compared to the previous year, adjusted and unadjusted analysis
| EC participants | Control | p value unadjusted | p value adjusted* | |
|---|---|---|---|---|
| Total (N=113) | 53% | 23% | <0.01 | <0.01 |
| Stratified analysis | ||||
| “Low activity” group** (n = 80) | 49% | 18% | <0.01 | 0.05 |
| “Active” group** (n = 33) | 60% | 40% | 0.30 | 0.96 |
*Adjusted by age, gender, race, education and health status in a multivariate logistic regression model
**Active individuals were defined as those who, at baseline, reported at least ten episodes in the last 2 weeks of moderate physical activity of at least 30 min duration, while inactive or “low activity” individuals were those with less activity.
Finally, we sought to understand whether ambulation increased in association with program activities. To do this, we utilized questions at baseline and follow-up on number of blocks walked per week and number of flights of stairs climbed per week, theorizing that activity in the schools might be reflected in the latter and walking involved in getting to and from schools might be captured by the former. This approach sought to enhance the information on “walking for exercise” which is ascertained in the Minnesota Leisure Time Activities Questionnaire. As seen in Table 4, no significant difference was seen in these additional questions. However, there is a suggestion that mean number of blocks walked and stairs climbed increased in the EC participants, while it remained stable or declined in controls.
Table 4.
Mean number of blocks walked and stairs climbed per week at baseline and at 4–8 months follow-up, EC participants vs. controls, (N = 113)
| EC participants | Controls | p value unadjusted | p value adjusted * | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||
| Mean blocks walked/week | 29 | 34 | 20 | 18 | 0.46 | 0.99 |
| Mean flights of stairs climbed/week | 11 | 15 | 20 | 21 | 0.83 | 0.79 |
Means were calculated as geometric means.
*Adjusted by age, gender, race, education and health status in a multivariate linear regression model
Discussion
These results suggest that this high intensity volunteer program, Experience Corps—Baltimore, requiring 15 h of service per week through a full school year, may lead to substantive increases in the physical activity levels of older adults, even in the short term. These findings were particularly observed among those who, prior to service, had low levels of physical activity as defined by the Healthy Persons 2010 Guidelines.2 This pilot randomized, controlled trial observed a doubling in meaningful physical activity levels among older adult volunteers who were initially relatively inactive, while the controls reported no change. The clinically and statistically significant increase of 460 kcal/week, reported in this pilot trial, among those who initially inactive compares favorably to the 400–700 kcal/week improvements seen in other successful activity interventions.10,11 While these other trials were performed in predominantly white communities of relatively high socioeconomic status, the Baltimore Experience Corps program successfully engaged African American inner-city older adults. This model of a health promotion intervention embedded in an intergenerational volunteer program that serves children in public elementary schools therefore has the potential to increase the physical activity level of a group that is at higher risk for adverse health outcomes. The Experience Corps program in Baltimore is the first volunteer program to demonstrate increased physical activity among initially inactive participants, with an effect on physical activity that appears to be comparable to other intentional exercise trials in older adults.
Prior research has demonstrated that interventions that increase “usual physical activity” may be as effective as formal exercise programs in health promotion.6,41,44,45 This study indicates that high impact, high intensity volunteering may serve as an effective approach to increasing “usual physical activity”. By appealing to personal motivations of older adults to “give back” and make a difference for their communities and offering regular, structured activities that people are personally committed to and necessitate regular ambulation, programs like Experience Corps may circumvent barriers to activity and offer older adults more sustainable options that incorporate increased physical activity into their daily lives.
The Experience Corps was intentionally designed, through its high intensity commitment and the necessity of travel to and from and within schools 3 to 5 days/week, to lead to an increase in usual physical activity.31 These results provide additional evidence that a health promotion intervention that is embedded in an intergenerational volunteer program has the potential to increase physical activity. It further amplifies on the prior report from this pilot trial of an overall increase in activity levels and reported strength31 by delineating that those with low activity show the greatest short-term benefit. However, the sample size in this pilot study was small and the MLTAQ instrument did not specifically ask about physical activities we expected would be associated with Experience Corps volunteering: traveling to and from school three to five times a week and walking around the school and classroom and up the stairs with the students. Instead, the MLTAQ asked about “leisure time activity” (walking for exercise, household chores, exercise and recreational activities).42 However, there was a trend toward an increase in the number of blocks walked and stairs climbed by EC participants on follow-up, while there was a decline among controls. It is likely that EC participation is associated with more of an increase in ambulation-related physical activity than the MLTAQ captures.
These results also indicated that 15 h/week of service, which Experience Corps—Baltimore requires of its volunteers, does not detract from their usual physical activity outside the program. Thus, there appears to be no tradeoff of one activity for another, as has been demonstrated in aerobic activity interventions where “regular activity” decreases while aerobic exercise increases.4 Nelson's prior trial in perimenopausal women indicated that increases in strength as a result of participation in resistance training led to a 25% increase in other activities outside of the intervention. In this pilot, we have previously reported increased strength and a slower decline in walking speeds31 and, in this report, demonstrated a more than two-fold increase in time and kilocalories expended in household chores in the intervention group, compared to no change in the controls. This latter increased activity in housework, gardening, and home maintenance activities, in combination with previously reported increased strength, may support Nelson's findings, but in a substantially older and higher risk group. Older adults who become stronger due to Experience Corps participation may then take on more optional, energy, demanding activities such as increased household chores.
These findings suggest that high intensity volunteer programs, such as this intergenerational one, may have the potential to address persistent health disparities in African American and other disadvantaged older adults, while offering opportunities for preservation of activity in those already active. Healthy People 2010 identified several population groups with the lowest rates of physical activity: seniors, women of all ages, African Americans and Hispanics, people with disabilities, those with lower incomes and less education.2,46 These groups may have differential access to opportunities to be physically active.46 It has been pointed out by Adler16 that if opportunities for health promoting behaviors and community preventive services are not targeted to disadvantaged communities, health disparities will increase over time. The program in Baltimore has been successful in attracting older adults with a history of low physical activity who are from a high-risk community with lower access to health promotion and a higher burden of morbidity. In fact, 96% were African American, 84% had annual incomes less than $15,000, and there was a high prevalence of physical disability. The stipends that are provided to defray the out-of-pocket cost of this high commitment volunteering (carfare, lunches, etc), through support by local foundations and the Corporation for National Service, allowed volunteers living on fixed incomes to participate fully in Experience Corps. This suggests an approach needed to overcome barriers to being active and engaged. It is important to note further that these older volunteers are serving in schools in which 89% of the students were eligible for free or reduced cost school meals.33 Thus, mobilizing the social capital of an aging society has the potential to increase educational success of the next generation and, through this, possibly prevent or mitigate future health disparities of these students. Such mobilization, may, simultaneously, improve health and decrease health disparities in the older adult volunteers.
While the Center for Disease Control's Task Force on Community Preventive Services did not evaluate volunteer programs as an intentional physical activity intervention, four of the Task Force's strong recommendations are reflected in volunteer programs like Experience Corps. The Task Force recommended use of programs that are 1) are community-based; 2) promote individually adapted behavioral change; 3) provide social support in the community setting; and 4) offer enhanced access to activity.47 The Baltimore Experience Corps program was designed to be such a community-based intervention, in which volunteers can choose from a variety of meaningful roles based on their interests, and social networks and support are developed through training and working in teams. The elder/child relationships that volunteers in this—and other—programs develop a strong motivation for adherence to volunteering and long-term retention. Notably, Experience Corps Baltimore has only a 2–3% dropout rate during any given school year, and 80% return from 1 year to the next. 30 Finally, as noted above, the incentive stipends that volunteers receive make volunteering a viable option for financially challenged older adults. This combination of a high rate of retention and a high intensity commitment of 15 h a week provides volunteers a prolonged exposure to the health promoting behaviors. These initial findings suggest that high intensity older-adult volunteering programs should be components of the campaign that experts argue will be required to include all older adults in a society-wide increase in physical activity.48
Our study has several limitations. First, this was a pilot study. The number of volunteers was limited by available funding, and this pilot did not have the power to detect significant differences. We had not anticipated having sufficient power to measure an effect on physical activity, particularly in the stratified analyses, given the low power of this pilot trial, although differences by initial activity level were hypothesized a priori. An adequately powered randomized, controlled trial with larger sample sizes and longer follow-up time will be required to determine if there are sustained physical activity improvements over time, and to evaluate the potential for this increase in activity to contribute to health benefits and a compression of the morbidity associated with aging. Follow-up studies will also need to objectively quantitate the amount of physical activity that occurs within the volunteer program, something that we did not have the resources to do. It is possible that the modified MLTAQ is not adequately sensitive to change in activities engaged in by older adults, and it may not be the most culturally appropriate physical activity instrument for the majority of urban older adults. Additionally, while the interviewers were blinded to the subject's randomization assignment, the subjects were not, and EC participants may have expected to be more active, which could have affected the results found in Table 3. Also, while this model of volunteering may be attractive and effective for many older adults, it may not appeal to all older adults, and future studies should evaluate and refine social marketing messages and recruitment strategies to attract volunteers while also developing a broader array of meaningful roles that may maintain activity and attract older adults not interested in serving in schools. Finally, given the financial costs of volunteer recruitment, training and support, the sustainability of volunteer programs will benefit from evidence garnered from rigorous cost-effectiveness evaluations.
These pilot findings suggest that this high intensity model of social engagement has the potential to meaningfully increase physical activity, although a formal randomized evaluation with a longer follow-up and sample size is required to determine the sustainability and health effects of this increase in physical activity. The results of this pilot trial suggests that EC participants have increased ambulation and demonstrated increased activity in household chores, which is an Instrumental Activity of Daily Living.49 Additional research will be required to determine if older adult volunteering might be effective in promoting the maintenance of functional status as postulated in Figure 131 and thus contribute to a compression of morbidity. Physical inactivity is also a leading cause of preventable death,50 with estimated economic costs of $76 billion in 2000 in direct medical costs alone.51 To be effective, programs for volunteering by older adults will require an investment in the infrastructure required for training, volunteer support, human resources administration, and ongoing sustainability. Additionally, if volunteering as a lifestyle is to be financially viable for all retired Americans, it will require continued community and government support that includes volunteer stipends. Volunteering by older adults represents a potentially important intervention in the effort to increase physical activity. America must develop, implement and evaluate new models for retirement that support a physically active lifestyle for all older adults before the 40 million Americans in the Baby Boom generation begin to retire en masse in 2010. The time to act is now.
Acknowledgements
This work was supported, in part, by funding from the following sources: The Retirement Research Foundation, the Erickson Foundation, the state of Maryland, the state of Maryland Department of Education, the City of Baltimore, the Baltimore City Public Schools, the Baltimore City Commission on Aging and Retirement Education, the Johns Hopkins Prevention Center, The John A. Hartford Foundation, The Pepper Older Americans Independence Center, and the Corporation for National and Community Service. We would like to thank AARP for crucial support with recruitment and Mrs. Sylvia McGill for all her work in the Experience Corps Pilot Randomized Controlled Trial.
Footnotes
Drs. Tan, Xue, Carlson, and Fried are with the Johns Hopkins University Center on Aging and Health; Tao Li is currently with the Social Security Administration.
References
- 1.Surgeon General's report on physical activity and health. From the centers for disease control and prevention. JAMA. Aug 21 1996;276(7):522. [PubMed]
- 2.Healthy People 2010: Understanding and Improving Health. 2nd ed. Department of Health and Human Services, Washington, DC: U.S. Government Printing Office; 2000.
- 3.Fiatarone MA, O'Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. Jun 23 1994;330(25):1769–1775. [DOI] [PubMed]
- 4.Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA. Dec 28 1994;272(24):1909–1914. [DOI] [PubMed]
- 5.Lazowski DA, Ecclestone NA, Myers AM, et al. A randomized outcome evaluation of group exercise programs in long-term care institutions. J Gerontol A Biol Sci Med Sci. Dec 1999;54(12):M621–M628. [DOI] [PubMed]
- 6.Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. Nov 13 2002;288(18):2300–2306. [DOI] [PubMed]
- 7.Lord SR, Castell S, Corcoran J, et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. J Am Geriatr Soc. Dec 2003;51(12):1685–1692. [DOI] [PubMed]
- 8.Simonsick EM, Guralnik JM, Volpato S, Balfour J, Fried LP. Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the women's health and aging study. J Am Geriatr Soc. Feb 2005;53(2):198–203. [DOI] [PubMed]
- 9.Leisure-time physical activity among adults: United States, 1997–1998. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2002.
- 10.Pereira MA, Kriska AM, Day RD, Cauley JA, LaPorte RE, Kuller LH. A randomized walking trial in postmenopausal women: effects on physical activity and health 10 years later. Arch Intern Med. Aug 10–24 1998;158(15):1695–1701. [DOI] [PubMed]
- 11.Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. Sep 2001;56(8):M465–M470. [DOI] [PMC free article] [PubMed]
- 12.Wagner EH, LaCroix AZ, Grothaus L, et al. Preventing disability and falls in older adults: a population-based randomized trial. Am J Public Health. Nov 1994;84(11):1800–1806. [DOI] [PMC free article] [PubMed]
- 13.Wagner EH, LaCroix AZ, Buchner DM, Larson EB. Effects of physical activity on health status in older adults. I: Observational studies. Annu Rev Public Health. 1992;13:451–468. [DOI] [PubMed]
- 14.Glass TA, Freedman M, Carlson MC, et al. Experience Corps: design of an intergenerational program to boost social capital and promote the health of an aging society. J Urban Health. Mar 2004;81(1):94–105. [DOI] [PMC free article] [PubMed]
- 15.U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin—Table 2. Projected Population of the United States, by Age and Sex: 2000 to 2050. Census Bureau Population Division, Population Projections Branch; 2004.
- 16.Adler NE. Community preventive services. Do we know what we need to know to improve health and reduce disparities? Am J Prev Med. Apr 2003;24(3 Suppl):10–11. [DOI] [PubMed]
- 17.Erikson E. Vital involvement in old age. New York: W.W. Norton and Company Inc; 1986.
- 18.De Tocqueville A. Democracy in America. New York: Knoph; 1945.
- 19.USDL 04-2503 Volunteering in the United States, 2004. U.S. Department of Labor, Bureau of Labor Statistics; 2004.
- 20.Harris AHS, Thoresen CE. Volunteering is associated with delayed mortality in older people: analysis of the longitudinal study of aging. J Health Psychol. 2005;10(6):739–752. [DOI] [PubMed]
- 21.Lum TY, Lightfoot E. The effects of volunteering on the physical and mental health of older people. Res Aging. January 1 2005;27(1):31–55. [DOI]
- 22.Oman D, Thoresen CE, McMahon K. Volunteerism and mortality among the community-dwelling elderly. J Health Psychol. 1999;4(3):301–316. [DOI] [PubMed]
- 23.Musick MA, Herzog AR, House JS. Volunteering and mortality among older adults: findings from a national sample. J Gerontol B Psychol Sci Soc Sci. 1999;54(3):S173–S180. [DOI] [PubMed]
- 24.Luoh M, Herzog AR. Individual consequences of volunteer and paid work in old age: health and mortality. J Health Behav. 2002;43(4):490–509. [DOI] [PubMed]
- 25.Shmotkin D, Blumstein T, Modan B. Beyond keeping active: concomitants of being a volunteer in old-old age. Psychol Aging. Jan 2003;18(3):602–607. [DOI] [PubMed]
- 26.Musick MA, Wilson J. Volunteering and depression: the role of psychological and social resources in different age groups. Soc Sci Med. 2003;56(2):259–269. [DOI] [PubMed]
- 27.Chambre S. Good Deeds in Old Age: Volunteering by the New Leisure Class. Lexington, Massachusetts: Lexington Books; 1987.
- 28.Okamoto K, Tanaka Y. Subjective usefulness and 6-year mortality risks among elderly persons in Japan. J Gerontol B Psychol Sci Soc Sci. Sep 2004;59(5):P246–P249. [DOI] [PubMed]
- 29.Pitkala KH, Laakkonen ML, Strandberg TE, Tilvis RS. Positive life orientation as a predictor of 10-year outcome in an aged population. J Clin Epidemiol. Apr 2004;57(4):409–414. [DOI] [PubMed]
- 30.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. Sep 2000;32(9 Suppl):S498–S504. [DOI] [PubMed]
- 31.Fried LP, Carlson MC, Freedman M, et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J Urban Health. Mar 2004;81(1):64–78. [DOI] [PMC free article] [PubMed]
- 32.Freedman M, Fried LP. Launching Experience Corps: findings from a two-year pilot project mobilizing older Americans to help inner-city elementary schools. Oakland, California: Civic Ventures; 1999.
- 33.Rebok GW, Carlson MC, Glass TA, et al. Short-term impact of Experience Corps participation on children and schools: results from a pilot randomized trial. J Urban Health. Mar 2004;81(1):79–93. [DOI] [PMC free article] [PubMed]
- 34.Frick KD, Carlson MC, Glass TA, et al. Modeled cost-effectiveness of the Experience Corps Baltimore based on a pilot randomized trial. J Urban Health. Mar 2004;81(1):106–117. [DOI] [PMC free article] [PubMed]
- 35.Fried LP, Frick K, Carlson M, Rebok G. Experience Corps: a social model for health promotion for older adults that, simultaneously, harness the social capital of an aging society. Gesundheit und Gesellschaft. Jan 2006:23–35.
- 36.Martinez I. Recruiting and retaining older volunteers to service that enhances health: successes and challenges of the Experience Corps TM in Baltimore. J Urban Health. 2006.
- 37.Fried LP TC, Walston J, Newman AB, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Med Sci. 2001;56A:M134–M135. [DOI] [PubMed]
- 38.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. Nov 14 2002;347(20):1585–1592. [DOI] [PubMed]
- 39.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. Mar 13 2002;287(10):1288–1294. [DOI] [PubMed]
- 40.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. Mar 2001;56(3):M146–M156. [DOI] [PubMed]
- 41.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. Jan 27 1999;281(4):327–334. [DOI] [PubMed]
- 42.Starling RD, Matthews DE, Ades PA, Poehlman ET. Assessment of physical activity in older individuals: a doubly labeled water study. J Appl Physiol. Jun 1999;86(6):2090–2096. [DOI] [PubMed]
- 43.Paffenbarger RS, Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Med Sci Sports Exerc. Jan 1993;25(1):60–70. [DOI] [PubMed]
- 44.Andersen RE, Wadden TA, Bartlett SJ, Zemel B, Verde TJ, Franckowiak SC. Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA. Jan 27 1999;281(4):335–340. [DOI] [PubMed]
- 45.Yaffe K, Barnes D, Nevitt M, Lui LY, Covinsky K. A prospective study of physical activity and cognitive decline in elderly women: women who walk. Arch Intern Med. Jul 23 2001;161(14):1703–1708. [DOI] [PubMed]
- 46.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. Am J Prev Med. Dec 1998;15(4):316–333. [DOI] [PubMed]
- 47.Increasing physical activity. A report on recommendations of the task force on community preventive services. MMWR Recomm Rep. Oct 26 2001;50(RR-18):1–14. [PubMed]
- 48.Buchner D, Miles R. Seeking a contemporary understanding of factors that influence physical activity. Am J Prev Med. Aug 2002;23(2 Suppl):3–4. [DOI] [PubMed]
- 49.Lawton M, Brody E. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed]
- 50.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: actual causes of death in the United States, 2000. JAMA. Jan 19 2005;293(3):293–294. [DOI] [PubMed]
- 51.Pratt M, Macera CA, Wang G. Higher direct medical costs associated with physical inactivity. Physician Sports Med. 2000;28(10):63–70. [DOI] [PubMed]