Abstract
Supportive housing is subsidized housing with on-site or closely linked services for chronically homeless persons. Most literature describing the effects of supportive housing on health service utilization does not describe use across multiple domains of services. We conducted a retrospective cohort study of 249 applicants to a supportive housing program; 114 (45.7%) were housed in the program. We describe the pattern of service use across multiple domains (housing, physical health care, mental health care, substance abuse treatment). We examine whether enrollment in supportive housing was associated with decreased use of acute health services (emergency department (ED) and inpatient medical hospitalizations) and increased use of ambulatory services (ambulatory medical and generalist care, mental health, and substance abuse treatment) as compared to those eligible but not enrolled. Participants in both groups exhibited high rates of service utilization. We did not find a difference in change in utilization patterns between the two groups [those that received housing (intervention) and those that applied, were eligible, but did not establish residency (usual care group)] comparing the two years prior to the intervention to the two years after. The finding of high rates of maintenance of housing is, in itself, noteworthy. The consistently high use of services across multiple domains and across multiple years speaks to the level of infirmity of this population and the costs of caring for its members.
Keywords: Health, Homeless persons, Housing, Retrospective studies, San Francisco, Services.
Introduction
Homelessness is associated with increased mortality1–3 and morbidity4 and increased use of acute care services compared to the housed population.5 Homeless persons also are more likely to be impoverished, unemployed, underemployed, or disabled and, consequently, have low rates of rates of private medical insurance6 and limited access to ambulatory health care services.7 Furthermore, social and environmental living conditions for the homeless increase the risk of illness and illness severity and create multiple barriers to accessing and using timely care.8–10 Access to care and living conditions, as well as high rates of co morbidity, substance use, injuries, outdoor exposures, and admission thresholds that differ from those of the general population, help to explain homeless persons' higher emergency department (ED) services use and greater number of hospitalizations.5,11–13
While a greater proportion of homeless persons are hospitalized or visit the ED than the general population,5 among the homeless population, a small proportion account for the majority of acute care use.11 These “high utilizers” tend to have co-morbid mental illness, substance abuse, and physical health problems. They are more likely to be chronically homeless, with a history of over one year of homelessness.11 While this population's use of the ED and inpatient services has been described,11,14 less is known about whether this population accesses other services, including ambulatory (non-Emergency) health care, mental health care and substance abuse treatment.
Supportive housing, defined as subsidized housing with site-based social services or linkages to community-based social services, is a strategy designed to provide housing stability to chronically homeless persons.15,16 A secondary goal of supportive housing is to decrease reliance on institutional care, including hospitalization and incarceration.17 Among homeless people, the need for housing must be balanced against the need for other necessities, such as food and health care. The provision of housing with supportive social services reduces an important competing need that may interfere with the ability to obtain health care. Under the Behavioral Model for Vulnerable Populations, homelessness is an important predisposing factor that may affect a persons' ability to obtain needed medical care.18 Supportive services received at supportive housing facilities, such as case management and benefits counseling, provide assistance that should enable the use of timely medical care. Substance use and mental illness are both predisposing factors that can interfere with timely receipt of health care; they are also factors whose presence creates a need for specific medical services.18 Providing housing and other services should increase access to timely medical care and thus should increase access to ambulatory care and decrease acute care. Case management and other supportive services have been associated with greater use of supportive services, although not always with reduced unmet needs for medical care.19 Chronically homeless persons with mental illness and substance abuse are a priority population for supportive housing.
In this study, we describe the pattern of service use across multiple domains (housing, physical health care, mental health care, substance abuse treatment) in a cohort of chronically homeless persons. We then examine whether enrollment in supportive housing is associated with decreased use of acute health services (ED and inpatient medical hospitalizations) and increased use of ambulatory services (ambulatory medical, mental health, and substance abuse treatment) as compared to those in usual care. We hypothesized that persons placed in supportive housing (intervention group) would, by dint of decreasing their competing priorities for the receipt of ambulatory health care, increase their use of ambulatory physical and mental health care and drug treatment and decrease their use of acute care services (ED visits, hospitalizations) compared with the group who applied, were eligible, but were not enrolled in this program (usual care).
Methods
Study Design
This is a retrospective cohort study that includes a comparison of two groups: one that was placed in one of three supportive housing buildings and another that applied, was eligible, but was not placed due to space limitations. All participants applied to at least one of three supportive housing sites that were studied. The comparison, or “usual care,” group may have received housing from other sources during the study period.
Participants and Setting
The San Francisco Department of Public Health (SFDPH) opened its first three supportive housing sites in 1999 and 2000 for homeless persons selected from public and private welfare agencies in the city. Two hundred forty-nine persons were referred to the program and met basic eligibility requirements in the initial “rent-up” period; 114 (45.8%) received housing. We examined the participants' public service use over a four-year period, the two years prior to and following the introduction of the housing program. Using the persons who were referred and eligible but not housed at these sites (usual care) as a comparison group, we explored differences in use of public services between the two groups.
Use of Publicly Funded Services and Vital Statistics
We obtained service records from the city-run health care, mental health care and substance abuse treatment systems by matching the records of all participants to records collected for services rendered from January 1, 1997, to July 1, 2001. We created measures of service utilization from the following sources:
Housing
We obtained move-in and move-out dates from the SFDPH Supportive Housing Program sites to find out how long participants maintained their housing.
Mortality
The San Francisco Coroner's Office provided mortality data from California death registries.
Medical Services
The Community Health Network (CHN) includes an inpatient acute care hospital and Emergency Department (San Francisco General Hospital), 13 health clinics, generalist and specialist hospital-based clinics, an 1,100-bed skilled nursing facility, and a long-term psychiatric nursing facility. The CHN maintains visit records, including types of services received, in a unified computer database.
Ambulatory Generalist Health Care
To assess generalist care utilization we examined all visits to non-ED generalist ambulatory care clinics (including HIV-focused providers), excluding visits to specialists such as orthopedists and gastroenterologists. We considered participants who saw the same clinician at least three times in a year to have a primary care provider.
Emergency Department
We assessed visits to the medical-surgical ED separately from those to the psychiatric ED. We did not include ED visits that resulted in a hospitalization as a separate visit.
Hospitalizations
We evaluated psychiatric hospitalizations separately from medical-surgical hospitalizations and, as a gross measure of appropriateness of ED use, whether or not the ED visits resulted in a hospitalization. We also measured the number of inpatient admissions and length of stay.
Ambulance use
The San Francisco Fire Department maintains records of all ambulances dispatched through the 911 system and includes data on ambulance ride destination. We assessed the participants' date of ambulance use and the destination, which could include EDs at hospitals that were not included in CHN data.
Community Substance Abuse Services (CSAS)
CSAS provided publicly funded counseling, residential drug treatment, day treatment, acute opiate and alcohol detoxification services and methadone maintenance.
Community Mental Health Services (CMHS)
CMHS operated the San Francisco Mental Health Plan (SFMHP), which is the responsible payer for specialty mental health services for San Francisco Medi-Cal beneficiaries and indigent residents. The CMHS database includes records on all visits to publicly funded mental health services, including counseling sessions, day treatment programs, 24 hour services, emergency psychiatric services and inpatient stays.
Analysis
We analyzed both intervention and usual care participants as members of a single cohort. In order to test our hypothesis that acute care utilization would be reduced more in the intervention group compared to the usual care group, we computed the average annual rate of service use over the entire study period and before and after the intervention. We compared the intervention and usual care groups' rates of service use over these three periods. Our main measure of change in service utilization was each participant's change in service utilization rate after the intervention. We assessed differences between the means in each group for statistical significance with t-tests. We analyzed individuals in the group to which they were initially assigned, regardless of whether they lost their housing (intervention group) or gained other housing (usual care). We assigned an intervention date based on, for the intervention group, the individual participants' move-in date and, for the usual care group, the mean date of housing for participants in the housing site to which they applied. We constructed the time period individually for each participant, defining two years prior to the intervention date as the “before” period (approximately 1997–1999) and two years after the intervention date as the “after” period (approximately 1999–2001).
If a participant died we censored our analysis at time of death or at the last date for which we had data from all providers, July 1, 2001. Our analyses compared annual rates of service use, adjusted for follow-up time. We also examined the intervention and usual care groups for differences in the number of days in inpatient care (acute care hospitalization and skilled nursing facilities) and jail to assess whether hospitalization or incarceration could have lowered the use of other services.
Results
Demographics
African Americans and non-Hispanic whites comprised 77.5% of the overall study group. White participants were less likely than other ethnic groups to be in the intervention group (p < 0.005). Men comprised 73.5% of the group but were not more likely to receive housing. The average age of participants was 51 (See Table 1.)
Table 1.
Demographic attributes of study group
| Group | Usual care | Intervention | Total | |||
|---|---|---|---|---|---|---|
| n = 135 | n = 114 | n = 249 | ||||
| n | (Percent) | n | (Percent) | n | (Percent) | |
| Race/ethnicity | ||||||
| Black | 54 | (40.0) | 53 | (46.5) | 107 | (43.0) |
| White | 56 | (41.5) | 30 | (26.3) | 86 | (34.5) |
| Latino | 10 | (7.4) | 16 | (14.0) | 26 | (10.4) |
| Other | 3 | (2.2) | 10 | (8.8) | 13 | (5.2) |
| Asian | 5 | (3.7) | 5 | (4.4) | 10 | (4.0) |
| Unknown | 7 | (5.2) | 0 | (0.0) | 7 | (2.8) |
| Total | 135 | (100.0) | 114 | (100.0) | 249 | (100.0) |
| Gender | ||||||
| Men | 104 | (77.0) | 79 | (69.3) | 183 | (73.5) |
| Women | 29 | (21.5) | 33 | (29.0) | 62 | (24.9) |
| Transgender | 1 | (0.7) | 2 | (1.8) | 3 | (1.2) |
| Unknown | 1 | (0.7) | 0 | (0.0) | 1 | (0.4) |
| Total | 135 | (100.0) | 114 | (100.0) | 249 | (100.0) |
| Age | ||||||
| Minimum | 22.8 | 22.0 | 22.0 | |||
| Maximum | 86.0 | 87.7 | 87.7 | |||
| Mean | 50.0 | 52.1 | 51.0 | |||
| Std Dev | 12.7 | 12.4 | 12.6 | |||
Mortality and Length of Stay in Housing
A total of 16 participants (6.5%) died during the study period. The mean age of death was 57.6 (range: 37.8–82.2). Of the 114 people who were in the intervention group, eight (7.0%) died. Of the 106 surviving, 78 (73.5%) remained housed as of July 2001, either in supportive housing or other housing. Twenty-three (21.6%) were evicted, incarcerated, or moved to unknown conditions. The remaining 5 (12.2%) moved for health reasons into a higher level of care (such as a skilled nursing facility).
Use of Services
Participants in both groups exhibited high rates of service utilization. Participants had service contact rates (defined as some use of one of the defined services) of 70.1 per year before the intervention and 76.1 after, which is more than one service per week. Intervention and usual care groups did not differ in average service utilization rates prior- or post-intervention or in change in utilization. Groups did not differ significantly in the amount of follow-up time. Mean number of days between each participant's last contact in any of the services studied was 129 in the usual care group and 100 days in the intervention group, a difference that was not statistically significant (p = 0.19).
Ambulatory (Non-Emergency Care)
Ambulatory Generalist Care
The intervention and usual care groups did not differ in their use of ambulatory services in the pre- or post-intervention periods, nor did the groups differ in their average difference between periods. One hundred ninety-eight (79.5%) of participants had at least one visit to an ambulatory care generalist provider during the study period. The rate of visits increased from 3.41 to 4.09 per year following the intervention, although this was a marginally significant increase (p = 0.06). (See Table 2.)
Table 2.
Service utilization in cohort of applicants to supportive housing project
| Annual rate before intervention | Annual rate after intervention | Difference between periods | Difference between periods associated with intervention group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Service type | Percent with any use (%) | Mean | 75th Pctl | Max | Mean | 75th Pctl | Max | Mean | p value | Mean | p value |
| Ambulance | 51.1 | 1.14 | 1 | 56 | 1.18 | 0.60 | 31.9 | 0.04 | 0.86 | 0.38 | 0.41 |
| All CSAS* services | 47.8 | 22.67 | 6.5 | 500.5 | 22.32 | 2.77 | 696.3 | 0.65 | 0.82 | 2.33 | 0.69 |
| CSAS residential | 28.1 | 8.67 | 0 | 246 | 6.80 | 0 | 333.1 | −1.87 | 0.43 | −5.23 | 0.27 |
| CSAS outpatient | 30.5 | 1.40 | 0 | 86.5 | 2.85 | 0 | 101.3 | 1.45 | 0.06 | 1.38 | 0.39 |
| CMHS** outpatient | 44.6 | 19.97 | 7 | 359 | 23.15 | 9.70 | 460 | 3.17 | 0.24 | −8.08 | 0.14 |
| CMHS 24-h tmt. | 14.5 | 7.43 | 0 | 314.5 | 2.00 | 0 | 116.6 | −5.43 | 0.01 | −10.31 | 0.02 |
| Ambulatory care clinics | 79.5 | 3.41 | 5 | 26 | 4.09 | 6.0 | 39.5 | 0.67 | 0.06 | 1.05 | 0.15 |
| Inpatient visits | 53.0 | 0.61 | 1 | 6.00 | 0.34 | 0 | 8.43 | −0.27 | <0.001 | −0.01 | 0.96 |
| ED^ Use | 69.9 | 2.15 | 2.00 | 27.00 | 0.98 | 1.20 | 14.05 | −1.16 | <0.001 | −0.47 | 0.27 |
* Community Substance Abuse Services
** Community Mental Health Services
^ Emergency Department
Primary Care Provider
Forty-three percent of participants had a PCP before the intervention, and 46.6% did after, which was not a significant change. We detected no difference by study group. Among those who met our criteria for having a PCP, we found that 30.8% saw another provider at least three times before the intervention. In the period after the intervention, 28.5% of those with a PCP had three or more visits with another provider.
Emergency Services: Ambulance and Emergency Department Use
Ambulance Services
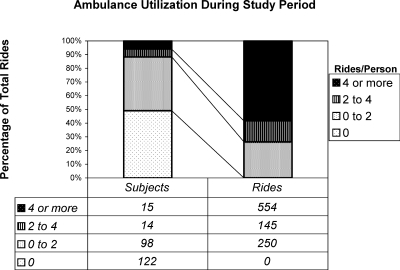
Of participants, 51.1% had at least one ambulance ride during the four years of the study (See Table 2), and there were no differences between study groups in ever use of an ambulance. Use was highly skewed, with the maximum rate of 56 rides per year before intervention and 31.9 per year after. Rates of ambulance use did not significantly decrease after the intervention, and there were no differences between the intervention and usual care groups either before or after the intervention. Six percent of all participants averaged at least four ambulances rides a year over the study period. This group of high utilizers accounted for 58.3% of the total ambulance usage of the group. Thus, while ambulance use was widespread throughout the group, most of the use was driven by a small group of people who used ambulance services repeatedly (See Figure 1).
Figure 1.
Ambulance utilization during study period
Emergency Department: Medical-Surgical Emergency Department
Seventy-one percent of participants in both groups used the SFGH ED at least once in the two-year period prior to the intervention. One in five of the overall group averaged four or more visits per year in the two-year period before the intervention. After the intervention, half of the participants had ED visits in the two-year period. One in ten had four or more visits. There were no differences between the two groups in their change in utilization before and after the intervention. Use of the SFGH ED decreased significantly by 1.16 visits per year (p < 0.0001), from 2.14 to 0.98 visits per year following the intervention, without regard to study group assignment.
Ninety percent (18/20) of participants with greater than three ED visits a year also visited a generalist clinic, compared to 96.4% (27/28) of those with 1–3 visits a year and 60.0% (45/75) of those without any ED visits.
We compared ED and ambulatory care utilization. We found 13 of 63 (20.6%) of those in the top quartile of ambulatory care were among the top quarter of ED users; conversely, 24 of 63 (38.1%) of those with the top quartile of ED use were among the top quarter of ambulatory care users; 30 participants had no use of either ED or ambulatory care.
Inpatient Hospitalizations: Medical-Surgical
One hundred thirty-two (53.0%) of participants had an inpatient stay at SFGH during the study period. The majority of those who were admitted at least once averaged less than one hospitalization a year.
On average, there were 0.6 inpatient admissions per year before the intervention and 0.3 after. This average change in utilization was statistically significant (p < 0.001); however, there was no difference between the intervention and usual care groups (p = 0.96) (See Table 2). Groups did not differ significantly in the number of days hospitalized. Only four participants had more than three weeks of inpatient care, and 90% had five days or fewer.
Proportion of ED Visits Resulting in a Hospitalization
Overall, 17% of participants' medical-surgical ED visits resulted in a hospitalization. The proportion did not differ significantly between intervention periods or housing status.
Mental Health and Substance Abuse Services
One hundred nineteen (47.8%) of participants had any use of substance abuse services. More participants had contact with outpatient services than with residential services or methadone or drug detoxification services. There were no differences between the study groups in ever use of substance abuse services. Outpatient substance abuse service use did appear to increase following the intervention, although the increase was marginally significant (p = 0.06). The groups did not differ in ever use of outpatient mental health services over the entire study period (See Table 2), and change in use following the intervention was not statistically significant.
Secular Trends in Ambulance Destination
We found that in the first two years of the study, half of all ambulance rides brought patients to the public hospital, SFGH. In the final two years of the study, 30% of ambulance rides ended at the hospital. This decrease was contemporaneous with an increase in rides to a private hospital located near the district of San Francisco where many of the homeless population congregate and where the supportive housing projects were located. Before the intervention, approximately one out of ten rides ended at this hospital; by the end of the study period more than two out of ten ended there. We did not have any information on ED visits or hospitalizations at hospitals other than SFGH; thus, the apparent decrease in ED utilization after the intervention could well represent a diversion of participants to other EDs. Intervention and usual care participants were equally likely to be taken to hospitals other than SFGH (p = 0.775).
Discussion
In this quasi-experimental study examining the public service utilization of a cohort of chronically homeless adults, half of whom were placed in supportive housing while the other half were deemed eligible but not placed, we found high rates of retention in supportive housing and high and consistent rates of utilization across multiple service domains. We did not find a difference in change in utilization patterns between those that received housing and those that did not (who may or may not have found other housing during the time period), comparing the two years prior to the intervention to the two years after.
The finding of high rates of maintenance of housing among those placed in supportive housing is, in itself, significant. Of those that survived the study period, three-quarters of those placed in supportive housing remained stably housed two years following the intervention. Being that the selection criteria for entry (chronically homeless, dual or triply diagnosed with medical illness, substance use, and mental illness) selected for persons who have traditionally been most difficult to house, this finding lends support to the feasibility and appropriateness of supportive housing as a model of care for the chronically homeless.
The consistently high use of services across multiple domains and across multiple years speaks to the level of infirmity of this population and the costs of caring for them. The cohort used public services (health, mental health and substance abuse treatment) consistently and regularly over a four-year period, with an average of over one service contact per week over four years. Few studies document utilization across systems of care, thus, it is difficult to compare these rates to the prior literature. The health services utilization observed in this cohort study is of a similar magnitude to that of the frail elderly.20–22 Although few other utilization studies examine use across multiple domains, it appears that the breadth and depth of use of public services of this group is higher than other vulnerable populations.
In the two-year follow-up period, we did not find any significant differences in usage patterns between the intervention and usual care groups. The intervention, while successful in maintaining housing, did not appear to decrease the use of acute care services among the intervention group compared to the usual care group. There are several potential explanations for this.
It is possible that the two-year time course was too short to provide medical stability and decrease medical utilization. The programs utilized a “housing first” model of care, not requiring sobriety or the attainment of “housing readiness” prior to enrollment.23 This strategy, while not interfering with the long-term success of housing (as determined by nearly three-quarters of participants in the housing group having maintained housing at two years), could have increased the time period necessary for medical and psychiatric stabilization. Understood through the lens of Gelberg's Behavioral Model for Vulnerable Populations,18 it may be that while the intervention may have reduced the predisposing vulnerability created by lack of housing, the participants' continued substance use and mental illness could have persisted in creating both a predisposing vulnerability that created a barrier to the receipt of timely care and a need factor that required acute care.
The timing of the study was at the nascence of supportive housing efforts in San Francisco. Over time, partially based on early findings, the programs have adapted to employ more medical services that are easily accessible to program participants and other innovations which may serve to decrease acute care utilization.
Secondly, while prior research has shown supportive housing to decrease the use of expensive psychiatric inpatient hospitalizations for enrolled clients with severe persistent mental illness,24 there is less evidence for those with medical illness. The study population did not have extensive use of long-term psychiatric inpatient care; rather, their utilization consisted of high rates of physical health care and substance abuse related treatment. Based on the high hospitalization and mortality rates, it is likely that members of the cohort suffered severe medical illness at study entry.
It is possible that medical (as opposed to psychiatric) health care utilization may be less disposed to alteration through housing. It is also possible that, in order to improve physical health status and decrease use of acute medical care, housing interventions must occur prior to the point where enrollees have end-stage medical illnesses. Few health-care based interventions for high using populations have been shown to be effective at reducing utilization.25
An alternative explanation to our findings may be due to the selection of the control group. It is possible that a substantial proportion of the usual care group obtained housing during the follow-up period, as there was increased access to supportive housing during that time. While other supportive housing sites offered less intense supportive services than the ones we studied, it is possible that some members of the usual care group were able to obtain this housing and that this accounted for the lack of observed difference in changed utilization between the intervention group and usual care group. As persons in the usual care group had come to the attention of case managers, it is plausible that they were also among the first to receive housing offered by other programs. The participants' connection to case managers (who referred them to the program) may be a marker for the resources and perceived need necessary to obtain health services. If this tendency did not differ between the groups and there were adequate resources available outside of the intervention, then we would not expect to find a difference in health services outcomes.
Finally, our failure to find a decrease in most medical services may have resulted from an increased detection of medical need. While intensive case management has been shown to decrease utilization of inpatient psychiatric care in populations with persistent mental illness,26–29 few case management programs have been shown to decrease utilization of medical (as opposed to psychiatric) services.30–32 This has been attributed, in part, to increased detection of unmet need, which may increase, instead of decrease, utilization. Participants who received housing may have increased their contact with service providers and thus increased the surveillance of their needs, leading to increased acute care utilization. Our study could not discern appropriate from inappropriate utilization or preventable versus non-preventable utilization and was not powered to detect changes in mortality.
Our study demonstrates the methodological feasibility and advantages of studying utilization across multiple domains. By linking data from disparate systems (mental health, physical health, substance abuse treatment, ambulance), we were able to examine the extent of utilization by a cohort of chronically homeless persons with severe medical, mental health and substance abuse problems.
Limitations
This study has several important limitations. First, we have no data on whether participants in the usual care group were able to obtain housing during the study period. As the time period corresponded to a period of burgeoning availability of supportive housing (and attention to the needs of the chronically homeless) in San Francisco, it is possible that many of the usual care participants obtained some form of supportive housing over the study period.
Secondly, participants were not randomly assigned to the intervention group; referring agencies placed participants on priority lists to become housed. It is possible that participants who were viewed as more impaired were selectively assigned to the intervention group. Randomized studies of housing interventions are rare due to both perceived ethical and practical challenges.33 Because housing is a scarce resource, providers are reluctant to potentially withhold available housing while waiting for the randomization process.
Third, our power to detect differences in some outcomes was limited. This is a common problem with studies of housing; because of the costs involved and the limited availability of new housing, studies tend to be small, as ours was.16
We are also limited by not having data from all sources of health care in San Francisco; although we believe that we have captured the majority of outpatient services, we have reason to believe that our data have not captured a substantial proportion of ED visits and hospitalizations. Our analysis of ambulance destination data demonstrated that in the first two years of the study approximately 30% of ambulances brought participants to hospitals other than SFGH, but in the last two years this proportion had increased to one-half. This effect did not appear to differ between group assignments. Thus, while our estimates of ED use and hospitalizations should be seen as underestimates, our findings do not suggest a difference between the groups. It is, of course, possible that trends in private hospitals follow different patterns.
Because of high levels of utilization, it is possible that extended stays in inpatient services and incarceration limited the amount of time in which some participants were available to use other services. We detected no difference between the groups in the number of inpatient hospital or skilled nursing facility days and number of days in jail (analyses not shown). Additionally, to have a substantial effect on their time at-risk in comparison to the entire study period, participants would have had to remain hospitalized or incarcerated for a number of months. Incarcerations or hospitalizations longer than two months occurred in less than 5% of participants.
Finally, the data we have are limited to service utilization; we have no information on the rates of or severity of substance abuse problems, medical illness or mental health problems, service appropriateness, or quality of life. We were similarly unable to determine whether ED use and hospitalizations were potentially preventable. It is possible that acute care utilization was appropriate or that the appropriateness differed by group. Because our data are limited to service utilization, we do not know the impact of the housing on the recipient's quality of life.
Implications
Supportive housing is an effective means of reducing homelessness among chronically homeless persons who have serious medical, mental health and substance abuse problems. Despite high levels of morbidity, this population was usually able to remain in supportive housing or transition to other forms of housing during the two-year follow-up. Our finding of consistently high rates of use of public services across multiple domains confirms this population's high level of morbidity and makes the accomplishment of a high proportion of participants maintaining housing more striking. These findings suggest that supportive housing is a viable means of providing long-term housing stability to a difficult-to-serve population. This fulfills the primary goal of supportive housing: reducing homelessness.
Acknowledgements
This research was supported by funds from the California Program on Access to Care (CPAC), California Policy Research Center, University of California, Grant Number #02GT13. The views and opinions expressed do not necessarily represent those of the Regents of the University of California, CPAC, its advisory board, or any State or County executive agency represented thereon. Other support included: San Francisco Department of Public Health (SFDPH) which provided salary support for Rajiv Bhatia and Eric Kessell (during the study design, data collection and analysis phases)
and the Agency for Healthcare Research and Quality grant K08 HS011415-03 and the Hellman Family Award for early career development provided salary support for Margot Kushel.
We acknowledge the assistance of the following individuals for assistance with obtaining the data used in the study:
Margot Antonetty, Daisy Leyva, Marc Trotz, SFDPH: Client Data, Supportive Housing Program data.
Bill McConnell, SFDPH, Mental Health Services and Substance Abuse Services Utilization data.
Mario Trevino, SFFD: Ambulance Service data.
Joe Goldenson, MD, SFDPH: Jail data.
Footnotes
Kessell is with the University of California—Berkeley, Berkeley, CA, USA; Bhatia and Bamberger, are with the San Francisco Department of Public Health, San Francisco, CA, USA; Kushel is with the University of California—San Francisco, San Francisco, CA, USA and the Division of General Internal Medicine, UCSF/San Francisco General Hospital, Box 1364, San Francisco, CA 94143, USA.
References
- 1.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331(5):304–309. [DOI] [PubMed]
- 2.Barrow SM, Herman DB, Cordova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89(4):529–534. [DOI] [PMC free article] [PubMed]
- 3.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283(16):2152–2157. [DOI] [PubMed]
- 4.Breakey WR, Fischer PJ, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262(10):1352–1357. [DOI] [PubMed]
- 5.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. [DOI] [PubMed]
- 6.Kreider B, Nicholson S. Health insurance and the homeless. Health Econ. 1997;6(1):31–41. [DOI] [PubMed]
- 7.O'Toole TP, Gibbon JL, Hanusa BH, Fine MJ. Utilization of health care services among subgroups of urban homeless and housed poor. J Health Polit Policy Law. 1999;24(1):91–114. [DOI] [PubMed]
- 8.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–556. [DOI] [PubMed]
- 9.Padgett DK, Struening EL. Influence of substance abuse and mental disorders on emergency room use by homeless adults. Hosp Community Psychiatry. 1991;42(8):834–838. [DOI] [PubMed]
- 10.Duchon LM, Weitzman BC, Shinn M. The relationship of residential instability to medical care utilization among poor mothers in New York City. Med Care. 1999;37(12):1282–1293. [DOI] [PubMed]
- 11.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784. [DOI] [PMC free article] [PubMed]
- 12.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department's frequent users. Acad Emerg Med. 2000;7(6):637–646. [DOI] [PubMed]
- 13.Palepu A, Strathdee SA, Hogg RS, et al. The social determinants of emergency department and hospital use by injection drug users in Canada. J Urban Health. 1999;76(4):409–418. [DOI] [PMC free article] [PubMed]
- 14.D'Amore J, Hung O, Chiang W, Goldfrank L. The epidemiology of the homeless population and its impact on an urban emergency department. Acad Emerg Med. Nov 2001;8(11):1051–1055. [DOI] [PubMed]
- 15.Lipton FR, Siegel C, Hannigan A, Samuels J, Baker S. Tenure in supportive housing for homeless persons with severe mental illness. Psychiatr Serv. 2000;51(4):479–486. [DOI] [PubMed]
- 16.Rog D, Randolph F. A multisite evaluation of supported housing: lessons learned from cross-site collaboration. In: Herrell M, Straw R, eds. New Directions for Evaluations: No. 94. Conducting Multiple Site Evaluations in Real-world Settings. San Francisco: Jossey-Bass; 2002.
- 17.Culhane M, Hadley. The impact of supportive housing or homeless people with severe mental illness on the utilization of the public health, corrections, and emergency shelter systems: the New York-New York Initiative. Fannie Mae Foundation. May 2001:1–47.
- 18.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed]
- 19.Heslin KC, Andersen RM, Gelberg L. Case management and access to services for homeless women. J Health Care Poor Underserved. 2003;14(1):34–51. [DOI] [PubMed]
- 20.Burton LC, Weiner JP, Stevens GD, et al. Health outcomes and medicaid costs for frail older individuals: a case study of a MCO versus fee-for-service care. J Am Geriatr Soc. 2002;50(2):382–388. [DOI] [PubMed]
- 21.Newcomer R, Maravilla V, Faculjak P, et al. Outcomes of preventive case management among high-risk elderly in three medical groups: a randomized controlled trial. Eval Health Prof. 2004;27(4):323–348. [DOI] [PubMed]
- 22.Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. J Am Geriatr Soc. 1999;47(7):775–783. [DOI] [PubMed]
- 23.Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. 2004;94(4):651–656. [DOI] [PMC free article] [PubMed]
- 24.Culhane DP, Metraux S, Hadley T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous Policy Debate. 2002;13(1):107–163.
- 25.Hastings SN, Heflin MT, Steele LS, et al. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med. 2005;12(10):978–986. [DOI] [PubMed]
- 26.Dincin J, Wasmer D, Witheridge TF, Sobeck L, Cook J, Razzano L. Impact of assertive community treatment on the use of state hospital inpatient bed-days. Hosp Community Psychiatry 1993;44(9):833–838. [DOI] [PubMed]
- 27.Wolff N, Helminiak TW, Morse GA, Calsyn RJ, Klinkenberg WD, Trusty ML. Cost-effectiveness evaluation of three approaches to case management for homeless mentally ill clients. Am J Psychiatr. 1997;154(3):341–348. [DOI] [PubMed]
- 28.Ziguras SJ, Stuart GW. A meta-analysis of the effectiveness of mental health case management over 20 years. Psychiatr Serv. 2000;51(11):1410–1421. [DOI] [PubMed]
- 29.Salkever D, Domino ME, Burns BJ, et al. Assertive community treatment for people with severe mental illness: the effect on hospital use and costs. Health Serv Res. 1999;34(2):577–601. [PMC free article] [PubMed]
- 30.Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162(6):705–712. [DOI] [PubMed]
- 31.Fitzgerald JF, Smith DM, Martin DK, Freedman JA, Katz BP. A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154(15):1721–1729. [DOI] [PubMed]
- 32.Curtis JL, Millman EJ, Struening E, D'Ercole A. Effect of case management on rehospitalization and utilization of ambulatory care services. Hosp Community Psychiatr. 1992;43(9):895–899. [DOI] [PubMed]
- 33.Rog DJ. The evidence on supported housing. Psychiatr Rehabil J. 2004;27(4):334–344. [DOI] [PubMed]