Abstract
Radiation is the primary modality of therapy for all commonly occurring malignant brain tumors, including medulloblastoma and glioblastoma. These two brain tumors, however, have a distinctly different response to radiation therapy. Medulloblastoma is very sensitive to radiation therapy, whereas glioblastoma is highly resistant, and the long-term survival of medulloblastoma patients exceeds 50%, while there are few long-term survivors among glioblastoma patients. p53-mediated apoptosis is thought to be an important mechanism mediating the cytotoxic response of tumors to radiotherapy. In this study, we compared the response to radiation of five cell lines that have wild-type p53: three derived from glioblastoma and two derived from medulloblastoma. We found that the medulloblastoma-derived cell lines underwent extensive radiation-induced apoptotic cell death, while those from glioblastomas did not exhibit significant radiation-induced apoptosis. p53-mediated induction of p21BAX is thought to be a key component of the pathway mediating apoptosis after the exposure of cells to cytotoxins, and the expression of mRNA encoding p21BAX was correlated with these cell lines undergoing radiation-induced apoptosis. The failure of p53 to induce p21BAX expression in glioblastoma-derived cell lines is likely to be of biologic significance, since inhibition of p21BAX induction in medulloblastoma resulted in a loss of radiation-induced apoptosis, while forced expression of p21BAX in glioblastoma was sufficient to induce apoptosis. The failure of p53 to induce p21BAX in glioblastoma-derived cell lines suggests a distinct mechanism of radioresistance and may represent a critical factor in determining therapeutic responsiveness to radiation in glioblastomas.
Radiation therapy is used extensively in the primary management of patients with medulloblastoma (MB) and glioblastoma (GBM). The response to radiation of these two central nervous system tumors differs dramatically, however. MBs are considered radiosensitive and, after treatment, the 5-year survival of patients is greater than 50% (1–4). In contrast, GBMs are radioresistant and long-term survivors with this diagnosis are very rare (5, 6). Dee et al. have shown previously that p53-mediated apoptosis is an important response of MB cell lines to radiation (7). Although chromosome 17p alterations are seen in MBs, p53 is very rarely altered in these tumors (8–10). Unlike MBs, approximately 40–60% of GBMs have p53 mutations (11–13), suggesting that the lack of p53-mediated apoptosis may be a significant factor in determining the response of these tumors to irradiation and treatment outcome. No strong correlation, however, between a functional p53 and the cytotoxic response of GBM-derived cell lines to irradiation has been identified in vitro (14–16). Also, no consistent or convincing correlation between the presence of a p53 mutation and the outcome of GBM patients treated with radiation has been observed (17, 18). The wide variation in radiation-induced apoptosis in different tumor types is well illustrated by the differential apoptotic response of MBs and GBMs to radiation. MBs undergo extensive apoptosis after irradiation (7), and most GBMs exhibit little radiation-induced apoptosis (14, 15).
The identification of many proteins that modulate apoptosis within a cell has provided insights into the molecular events important for mediating radiation-induced apoptosis. Proteins encoded by the BCL-2 gene family are among the best characterized of these (for reviews see refs. 19 and 20). Products of this gene family can act either as promoters (e.g., p21BAX, bcl-xS, etc.) or inhibitors (e.g., bcl-2, bcl-xL, etc.) of apoptosis. A balance between the expression of these functionally antagonistic proteins is thought to determine whether a cell survives or undergoes an apoptotic death. The P53 tumor suppressor also plays a key role in regulating apoptosis, especially in the setting of radiation exposure (21–25). p53 is a very short-lived transcriptional activator that, when stabilized, can induce apoptosis (26). While transcription-independent mechanisms for p53-dependent apoptosis have been recognized, the apoptotic response of tumor cells to irradiation is thought to be closely related to the ability of p53 to activate transcription (27–30). The BAX gene recently has been shown to contain a p53-responsive element in its promoter (31). This makes it an attractive candidate as a downstream effector of p53-dependent apoptosis. Consistent with this possibility is the observation that some naturally occurring p53 mutants that have selectively lost the ability to activate transcription of BAX also appear to have lost the ability to induce apoptosis in many cell types (32, 33). Other bcl-2 family members also have been reported to be modulated by p53 after radiation exposure (34, 35).
Because the disparate apoptotic responses to radiation of MB and GBM cell lines appear to correlate with the observed clinical responses of these different tumors, the degree of radiation-induced apoptosis may be an important determinant of the initial response to therapy or even the ultimate outcome of patients with these tumors who are treated with radiation therapy. Understanding the molecular basis for the resistance of GBM cell lines to radiation-induced, p53-dependent apoptosis may provide insight into the clinical radioresistance of these tumors as well as suggesting future therapeutic interventions aimed at enhancing the apoptotic response. Because of these potential clinical implications, we sought to better understand the highly variant apoptotic response of MB- and GBM-derived cell lines to radiation. We observed that apoptosis is induced by ionizing radiation in MBs but not GBMs, even when p53 was not mutated and functioned normally to induce a G1 cell cycle arrest after irradiation. The differential apoptotic response of cell lines derived from these tumors correlates with the ability of p53 to induce expression of proapoptotic p21BAX. When p53 activity in MBs was repressed to varying extents through overexpression of a dominant-negative p53 mutant, the reduction in radiation-induced, p53-dependent apoptosis correlated with degree of reduction in p21BAX expression. Consistent with these observations, overexpression of p21BAX in a GBM cell line that did not undergo apoptosis after exposure to radiation resulted in high levels of apoptosis.
MATERIALS AND METHODS
Cell Culture, Transfections, and Treatment with Ionizing Radiation.
The GBM cell lines U87, U343, and U563 and the MB cell lines D283, DAOY, and SNB40 were all cultured in DME H-21 medium (GIBCO/BRL) supplemented with 10% fetal calf serum/100 μg/ml streptomycin/100 units/ml penicillin G. The MB cell line D341 was cultured in MEM with Earle’s BSS (GIBCO/BRL) supplemented with nonessential amino acids, 1 mM sodium pyruvate, 15% fetal calf serum, 100 μg/ml streptomycin, and 100 units/ml penicillin G. The GBM cell lines were cultured as adherent cells, while the MB cell lines were cultured in suspension. Stable transfection of D283 using Lipofectamine (GIBCO/BRL) with plasmid DNA encoding a dominant-negative mutant of p53 (point mutation at codon 175) has been described previously (7). Transient transfection of U343 was accomplished by using Lipofectin (GIBCO/BRL) according to the manufacturer’s recommendations. pEGFP-N1 (CLONTECH), an expression plasmid containing green fluorescent protein (GFP), was cotransfected with DNA from either the expression vector pcDNA-3 (Invitrogen) or pcBAX, a pcDNA-3 derivative containing a murine bax cDNA at a ratio of 1:3 (GFP/pcDNA-3, wt/wt). GBM or MB cells (4–5 × 106) in approximately 10 ml of media in a 10-cm Petri dish were treated on a Philips RT-250 x-ray machine by 250-kVp x-rays at a dose rate of 250 cGy/min.
Apoptosis Assay.
Cells were harvested at the designated times postirradiation or posttransfection. Adherent cells were collected after trypsinization. For the detection of apoptosis, cells were fixed for a minimum of 1 hour in 70% EtOH at 4°C. The fixed cells were washed in PBS and incubated in PBS containing 2.5 μg/ml propidium iodide (PI) and 50 μg/ml RNase A. The PI-stained cells were analyzed by flow cytometry on a FACSort using cellquest software (Becton Dickinson), and the percentage of cells with subdiploid DNA content was determined. Based on preliminary experiments, the subdiploid fraction was designated as apoptotic. A minimum of 2 × 104 cells were counted per experiment. After transient transfection of DNA encoding p21BAX and GFP, cells were fixed with 1% paraformaldehyde in PBS for 30 min on ice, washed in PBS, and fixed with cold 70% EtOH for 1 hr on ice. The cells were then processed as described above with separate histograms generated for cells in which transfected DNA could be detected (GFP-positive) and those in which it could not be detected (GFP-negative). A minimum of 2 × 105 cells was counted per each transient transfection experiment.
Western Blotting.
Total cellular protein was prepared by lysing cells that had been treated as indicated in the text and washed with PBS. RIPA buffer (50 mM Tris⋅Cl, pH 7.4/150 mM NaCl/1% Nonidet P-40/0.5% deoxycholic acid/0.1% SDS) supplemented with protease inhibitors (1 mM EDTA/100 μg/ml phenylmethylsulfonyl fluoride/10 μg/ml aprotinin/10 μg/ml leupeptin) was used, and lysis was performed on ice. Protein concentration was quantitated by a Bradford protein assay (Bio-Rad). One hundred micrograms of total cellular protein was fractionated by SDS/PAGE and electrotransferred to Immobilon-P (Millipore) by standard techniques. Immunoblotting was performed using 5% nonfat dry milk in PBS containing 0.1% Tween-20 as the blocking agent. Filters were blocked overnight at 4°C. Anti-p21WAF1 antibody (C-19, Santa Cruz Biotechnology) was used at a concentration of 0.1 μg/ml in blocking solution. Primary antibody incubation was for 1 hr at room temperature. Filters subsequently were washed five times for 10–15 min per wash in PBS containing 0.1% Tween-20. Goat anti-rabbit IgG antibody conjugated to horseradish peroxidase (GIBCO/BRL) was used per the manufacturer’s recommendation. After the secondary antibody incubation, filters were washed again as described above. Detection was performed by enhanced chemiluminescence (ECL; Amersham) according to the manufacturer’s recommendation by using Hyperfilm ECL (Amersham). Detection of p53 by immunoblotting has been described previously (7).
Northern Blotting and Densitometry.
After the designated treatments, total RNA was isolated from cells by ultracentrifuge pelleting through cesium chloride using standard techniques. Twenty micrograms of total RNA was fractionated through a 1% formaldehyde agarose gel and transferred to Nytran (Schleicher & Schuell) by standard techniques. Serial probing of the Nytran membranes with cDNAs for human p21BAX, bcl-2, bcl-x, and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) labeled with [32P]dCTP using Rediprime (Amersham), a random primer-labeling kit, was performed according to the manufacturer’s recommendations. The membranes were stripped between each successive probing. The hybridization was performed by preincubating the membranes with a solution containing 50% formamide/5× SSPE (20× = 3.0 M NaCl/0.2 M NaH2PO4/20 mM disodium EDTA, pH to 7.4 using NaOH), 5× Denhardt’s reagent (100× = 2% Ficoll type 400/2% polyvinylpyrrolidone/2% BSA fraction V), 0.1% SDS, and 100 μg/ml denatured salmon sperm DNA at 42°C for a minimum of 3 hr. 32P-labeled DNA was added at a minimum concentration of 1 × 106 cpm/ml, and the membranes were incubated for a minimum of 20 hr at 42°C. Membranes were washed at high stringency before exposure on either Hyperfilm MP (Amersham) or Reflection autoradiography film (NEN). Densitometry of the autoradiograms was performed by using the IS-1000 Image Analysis System (Alpha Innotech, San Leandro, CA).
RESULTS
Radiation-Induced Apoptosis in MB and GBM Cell Lines That Contain Wild-Type p53.
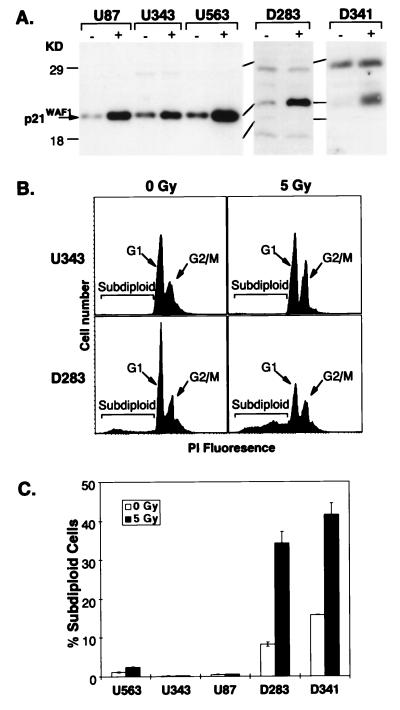
Two MB cell lines (D283 and D341) and three GBM cell lines (U87, U343 and U563) were examined. In each of these cell lines, a functional, wild-type p53 has been characterized previously and the response of some of these cell lines to irradiation has been reported previously (refs. 7, 13, 14, and 36; unpublished data). To confirm the presence of wild-type p53 in these cell lines, we probed for the induction of p21WAF1 after exposure of each of these cell lines to radiation. The p21WAF1 promoter has a strong p53-responsive element (37), and this gene is induced after radiation in the presence of wild-type p53 function (38). In each case, after exposure to 5 Gy ionizing radiation, the level of p21WAF1 protein increased compared with the untreated controls (Fig. 1A). The induction of p21WAF1 expression correlated with the induction of a G1 cell cycle arrest, which was detectable as early as 2 hr after irradiation (ref. 7; data not shown). We next examined the induction of apoptosis in these cell lines after exposure to radiation. Each of the five cell lines was treated with either 0 or 5 Gy ionizing radiation. Two days after the treatment, cells from each of the samples were fixed and DNA content was measured after staining with PI. Since apoptotic cells undergo extensive DNA fragmentation, they have a decreased DNA content and appear in the subdiploid fraction. The percentage of cells that have undergone apoptosis was determined by fluorescence-activated cell sorter counting of cells with subdiploid DNA content divided by the total number of cells present. Histograms plotting the amount of PI fluorescence and cell number after treatment with 0 Gy or 5 Gy are shown for representative GBM- and MB-derived cell lines U343 and D283, respectively (Fig. 1B). At 2 days after irradiation, no detectable increase in the percentage of cells with subdiploid DNA content is seen in U343, while a clear increase in the percentage of cells with subdiploid DNA content is seen in D283 (Fig. 1B). This assay was repeated in triplicate for each of the five cell lines (Fig. 1C). Spontaneous apoptosis in the GBM cell lines ranged from 0.1 to 2.5% with no significant increase after radiation, while spontaneous apoptosis in the MB cell lines ranged from 8 to 16% with increases to 34–42% after 5 Gy (Fig. 1C). These results were confirmed qualitatively by using a terminal deoxynucleotidyltransferase assay to examine the U343 and D283 cell lines (data not shown).
Figure 1.
Apoptotic response after irradiation of GBM- and MB-derived cell lines. (A) GBM-derived cell lines U87, U343, and U563 and MB-derived cell lines D283 and D341 were treated with either 0 Gy (−) or 5 Gy (+) of ionizing radiation, and lysates of total cellular protein were prepared 24 hr posttreatment. Total cellular protein was resolved on a 12.5% gel by SDS/PAGE and electrotransferred to a poly(vinylidene difluoride) membrane and examined by immunoblotting for p21WAF1 expression. (B) FACS histograms of U343 and D283 examined 2 days after irradiation with either 0 or 5 Gy of ionizing radiation plotting DNA content as measured by PI fluorescence and cell number are shown. Cells in the G1 or G2/M phase of the cell cycle with 2n or 4n DNA content, respectively, are noted on the histograms. Apoptotic cells comprise the subdiploid fraction to the left of each G1 peak. (C) Bar graph summarizing the results of experiments to determine the subdiploid, apoptotic fraction of U563, U343, U87, D283, and D341 2 days after treatment with 0 or 5 Gy. Each bar represents the mean ± SD of the results of three independent experiments. In each experiment, a minimum of 2 × 104 cells were counted.
Induction of BAX Correlates with Radiation-Induced Apoptosis.
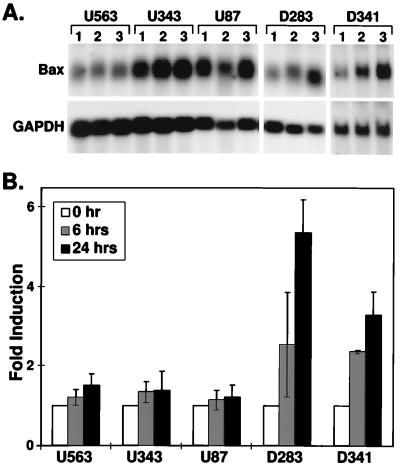
We sought to assess the expression of bcl-2 family members after irradiation of these cell lines. A p53-responsive element in the promoter of the proapoptotic gene BAX has been described previously (31). In addition, expression of the antiapoptotic gene BCL-2 has been shown to be repressed after p53 activation in some cell types (34), and the balance of proapoptotic and antiapoptotic family members is thought to be important in determining whether or not a cell undergoes apoptosis (39). Expression of BCL-XL, another antiapoptotic gene product, has also been reported to be altered after irradiation, although the mechanism regulating expression is unknown (35). Therefore, we examined the expression levels of BAX, BCL-2, and BCL-X in the GBM and MB cell lines after exposure to ionizing radiation. We treated the three GBM and two MB cell lines with 5 Gy ionizing radiation, and RNA was harvested at 0, 6, and 24 hr after exposure. Northern blots were then serially probed with cDNA for p21BAX, bcl-2, bcl-x, and GAPDH. We were not able to detect an induction of p21BAX mRNA in any of the GBM-derived cell lines, while the MB cell lines exhibited a significant induction after radiation treatment (Fig. 2A). We could not identify a consistent pattern of change in bcl-2 or bcl-x mRNA expression after irradiation (data not shown). To quantitate the degree of bax induction, densitometry was performed on autoradiograms of bax and GAPDH Northern blots from three independent experiments. GAPDH expression was used for normalization. The level of induction of p21BAX mRNA in D341 and D283 ranged from 4- to 6-fold, while no significant induction of p21BAX mRNA was evident in U87, U343, and U563 (Fig. 2B).
Figure 2.
BAX induction after irradiation of GBM- and MB-derived cell lines. (A) Representative Northern blot analysis of the expression BAX. Total RNA prepared from U563, U343, U87, D283, and D341 at 0 (1), 6 (2), and 24 (3) hr after treatment with 5 Gy of ionizing radiation was examined by Northern blot analysis for expression of BAX and GAPDH mRNA. (B) The densitometric intensity of bands corresponding to BAX mRNA was divided by the intensity of the GAPDH bands for each time point and expressed as fold induction on the bar graph. The expression of BAX mRNA at the 0-hr time point was arbitrarily set at one for each cell line, and the degree of induction was determined by comparing the level of expression at 6 and 24 hr after irradiation. Each bar represents the mean ± SD of the results of three independent experiments.
Expression of Dominant-Negative p53 in D283 Antagonizes Radiation-Induced Apoptosis and BAX Induction.
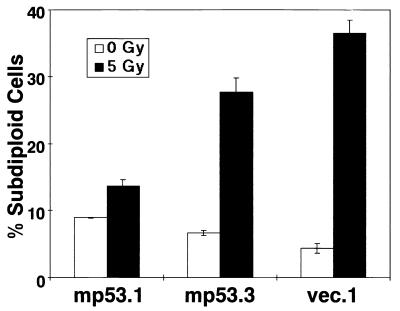
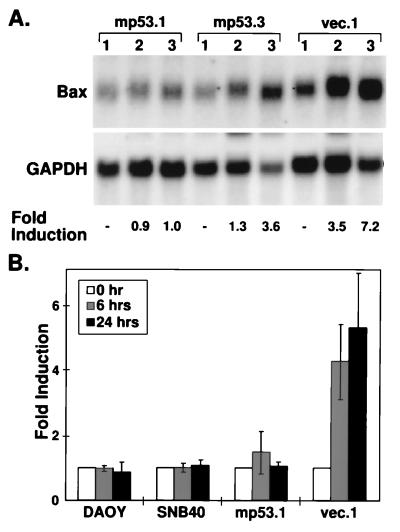
Dee et al. (7) previously reported that D283 clones expressing a dominant-negative p53 mutant exhibited decreased radiation-induced apoptosis. We utilized two D283 clones transfected with a mutant p53 expression construct (mp53.1 and mp53.3) as well as a D283 clone transfected with only expression vector DNA (vec.1), which were described in that report (7). We confirmed that the two clones expressing mutant p53 protein display a lower level of apoptosis after treatment with 5 Gy ionizing radiation when compared with the response of the vector-transfected clone (Fig. 3) (7). mp53.1 had almost complete repression of the radiation-induced apoptosis (13% subdiploid fraction), while mp53.3 had a partial repression (27% subdiploid fraction) compared with that observed in the vec.1 clone, which showed a level of radiation-induced apoptosis similar to the parental D283 cell line (Figs. 1C and 3). We next examined BAX induction after exposure to ionizing radiation in the three clones (mp53.1, mp53.3, and vec.1). As expected, the vec.1 clone shows a high level of p21BAX mRNA induction, while the mp53.1 and mp53.3 clones show a reduced induction of p21BAX mRNA (Fig. 4A). Similarly, p21BAX mRNA was not induced after irradiation in two additional medulloblastoma cell lines DAOY and SNB40 (Fig. 4B), which we characterized previously as having a mutant p53. Densitometric analyses of autoradiograms of BAX and GAPDH Northern blots indicate that 24 hr after exposure to ionizing radiation, mp53.1 had complete loss of BAX induction and mp53.3 had a reduction in the degree of BAX induction, while vec.1 had normal BAX induction (Fig. 4 A and B). These data demonstrate a correlation between the repression of p21BAX mRNA and the extent of radiation-induced apoptosis in these transfected MB-derived cell lines.
Figure 3.
Effect of p53 expression in D283 on apoptotic response after irradiation. Bar graph summarizing the subdiploid, apoptotic fraction of D283 clones, mp53.1, mp53.3, and vec.1 2 days after treatment with 0 or 5 Gy. Each bar represents the mean ± SD of the results of three independent experiments. In each experiment, a minimum of 2 × 104 cells were counted.
Figure 4.
Effect of p53 expression in D283 on BAX induction after irradiation. (A) Representative Northern blot analysis of BAX expression is shown. Total RNA prepared from D283 clones, mp53.1, mp53.3, and vec.1 at 0 (1), 6 (2), and 24 (3) hr after treatment with 5 Gy of ionizing radiation was examined by Northern blot analysis for expression of BAX and GAPDH mRNA. Densitometric evaluation of BAX mRNA induction after irradiation was determined as indicated in Fig. 2B and labeled as fold induction below the autoradiographs. (B) Densitometric evaluation of BAX mRNA induction after irradiation was determined for DAOY, SNB40, mp53.1, and vec.1 as indicated in Fig. 2B and expressed as fold induction on the bar graph. Each bar represents the mean ± SD of the results of three independent experiments.
Expression of p21BAX in U343 Results in Apoptosis.
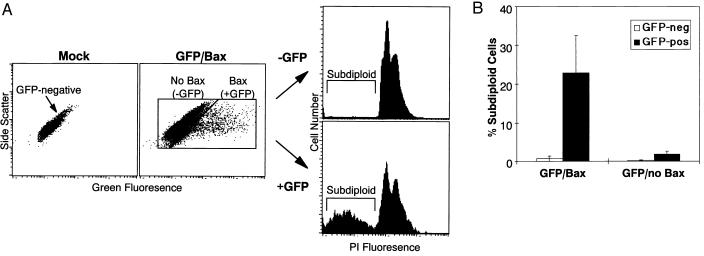
Since an otherwise functional p53 was not sufficient to induce p21BAX expression in the GBM cell lines after exposure to ionizing radiation (Fig. 3), we sought to determine whether apoptosis occurred with overexpression of p21BAX in GBM cell lines. We first tested this hypothesis by transfecting U343 with either recombinant vector DNA that mediated expression of p21BAX or the parental vector that does not contain p21BAX cDNA. After selection in the presence of G418, the vector-transfected U343 developed many resistant colonies, while there were very few colonies in the bax-transfected U343 cultures and these did not express detectable p21BAX mRNA from the recombinant vector (data not shown). While this result suggests that p21BAX overexpression led to growth suppression (possibly by inducing apoptosis) in U343, it did not show that apoptosis definitively was involved. We therefore transiently cotransfected U343 with recombinant plasmids encoding p21BAX and GFP. Since cells competent for gene transfer generally will acquire both expression constructs during the cotransfection procedure, the great majority of cells that express GFP will also express p21BAX. When the degree of apoptosis in the GFP-negative and GFP-positive cells after transfection was examined, we found very few subdiploid cells among the GFP-negative U343 transfectants, while the GFP-positive U343 transfectants had a high subdiploid fraction (Fig. 5A). Quantitation of apoptosis in the GFP-negative and GFP-positive population revealed 0.7 and 23.4% apoptotic cells among those not expressing or expressing p21BAX, respectively (Fig. 5B). GFP expression alone was insufficient to induce apoptosis in the U343 cells (Fig. 5B). We interpret these data to indicate that p21BAX expression can lead to apoptosis in the U343 GBM-derived cell line.
Figure 5.
Effect of transient overexpression of p21BAX on apoptosis in U343 cells. (A) U343 cells were either mock-transfected or cotransfected with two plasmid DNAs that expressed GFP and p21BAX stained with PI for DNA content 2 days posttransfection. Dot plots of green fluorescence vs. side scatter are shown. The plot describing mock-transfected cells indicates the distribution pattern of GFP-negative cells. The GFP/p21BAX cotransfected cells were separated into p21BAX-negative (GFP-negative) and p21BAX-positive (GFP-positive) populations as indicated and separately analyzed on a PI histogram. The subdiploid cell populations lie to the left of the G1 peak and are noted in each histogram. (B) Bar graph summarizing the subdiploid fraction of U343 cells 2 days after transient cotransfection with plasmids encoding GFP and p21BAX or after transient transfection with plasmid encoding GFP alone. The GFP-negative and GFP-positive populations were analyzed separately on PI histograms as detailed in A to determine the percentage of subdiploid, apoptotic cells. Each bar represents the mean ± SD of the results of three independent experiments.
DISCUSSION
Despite the widespread use of radiation therapy for the treatment of GBM, the uniformly poor response of these tumors remains a critical problem in the management of these patients (5, 6). In contrast, MB patients enjoy a markedly better prognosis after treatment with radiation (1–4). In previous studies, we have found that p53 function can enhance the clonogenic response of glioma-derived cells to irradiation (14–16), although no corresponding change in the number of chromosomal aberrations was detectable (40). In this study, we examined the response to irradiation of three GBM-derived and two MB-derived cell lines that each have wild-type p53 function to evaluate the differential effects of p53 function on apoptosis in these related, but different tumor types. We were unable to induce apoptosis in the GBM lines, but we induced significant levels of apoptosis in the MB lines after irradiation. In examining the expression of bcl-2 family members after irradiation, we found that p21BAX mRNA levels increased in the MB cell lines after treatment with radiation but not in the GBM cell lines. In none of these cell lines examined were we able to detect significant bcl-2 mRNA expression. Furthermore, if the activity of p53 is repressed to varying extents in the D283 MB cell line, the degree to which apoptosis is repressed correlates directly with the repression of p21BAX induction. Our finding that apoptosis was induced at a very high rate when p21BAX was overexpressed in the U343 GBM cell line is consistent with this observation and indicates the importance of p21BAX expression for apoptosis.
A p53-responsive element is found within the BAX promoter, and stabilization of p53 can increase the expression of p21BAX in some cell types (31). Given that p21BAX overexpression alone is capable of inducing apoptosis in the U343 GBM cell line, we can expect that p53-mediated apoptosis would occur in GBMs if p21BAX could be induced. Other investigators have observed that GBM cells lacking a functional p53 undergo BAX induction and apoptosis after transfer of a wild-type P53 gene, while such a transfer in GBM cells with endogenous wild-type P53 did not result in BAX induction and apoptosis (41, 42). These findings confirm that the BAX-mediated apoptosis pathway can be activated in p53−/− GBM cells, but is inhibited in GBM cells with wild-type p53, further strengthening our interpretation that the lack of p21BAX induction represents an important deficiency in the response of GBM cell lines to radiation. While in some normal cells types, radiation-induced, p53-dependent apoptosis can occur independent of BAX induction (23, 24, 43), it is clearly important in many other normal and tumor cells in which this has been examined (44–47).
A number of possibilities may account for the lack of BAX induction in GBM cell lines. The GBM-derived cell lines may contain genetic mutations within the BAX locus that could alter the transcriptional induction or the stability of p21BAX mRNA, but such alterations have never been reported and seem unlikely given the readily detectable basal levels of p21BAX mRNA we find in each of the GBM-derived cell lines examined. A second hypothesis invokes the presence of an MB- or GBM-specific factor that modulates the ability of p53 to activate transcription of BAX either positively or negatively, respectively. Friedlander et al. (33) found that the p53 element within the BAX promoter differed from that of the WAF1 promoter in that the responsive element in BAX had a lower affinity for p53 than the responsive element in the WAF1 promoter. This result suggests a third possible mechanism in which a lower p53 activity is present in GBMs compared with MBs. In the GBM cells, the p53 activity may lie below the threshold required to fully transactivate the BAX promoter. Though possible, this mechanism seems less likely since even high levels of induced p53 expression after recombinant p53-expressing adenovirus infection does not lead to apoptosis or bax induction in glioma cells that contain an endogenous wild-type P53 gene (42).
In addition to its potential role in mediating the “intrinsic” radioresistance of GBM, the differential activation of p21BAX also suggests a potential mechanism by which cellular fate is determined after p53 activation. Two important functional consequences of p53 activation are the arrest of cells in the G1 phase of the cell cycle and apoptosis (23, 24, 48, 49). These functions complement each other in mediating the role of p53 as the “guardian” of the genome (50). However, how a cell chooses to undergo G1 cell cycle arrest or apoptosis is not clearly understood. Our findings suggest that p21WAF1, the mediator of G1 arrest, is always activated by p53. However, whether G1 arrest is ultimately manifested depends on whether proapoptotic p53 targets such as p21BAX are also activated. If p21BAX is induced, then apoptosis will result irrespective of the induction of G1 arrest. If p21BAX is not induced, p21WAF1 will mediate the G1 arrest phenotype without interference from proapoptotic p53 targets. Examination of the activation of p21BAX in other cell types that respond to p53 activation by undergoing a G1 cell cycle arrest rather than apoptosis would give further support to this mechanism for determining the cellular response to p53 activation.
The poor response of patients with GBM and other “radioresistant” tumors to irradiation remains a significant clinical problem. Defining the molecular basis of radioresistance therefore is a foremost question of oncologic and biologic research. Differential apoptotic response may well account for the observed differences in the clinical responsiveness of these tumors after treatment with radiation therapy. With a better understanding of this process, manipulation of specific cellular targets can be pursued to improve the radioresponsiveness of tumors. It is possible that the pathway for p21BAX activation by the p53 may be such a target that eventually could improve therapeutic ratio and, ultimately, clinical outcome in this disease.
Acknowledgments
We thank Suzanne Dee for assistance in the construction of D283 clones and Lucy Avila for assistance in the preparation of the manuscript. This work was supported in part by the Preuss Foundation and Public Health Service Grants CA 13525 and CA 64898 to M.A.I. from the National Cancer Institute. H.-K.G.S. was supported by a fellowship from the American Society for Therapeutic Radiology and Oncology, a research resident award from the Radiological Society of North America, and National Institutes of Health Training Grant CA 09215.
ABBREVIATIONS
- MB
medulloblastoma
- GBM
glioblastoma
- GFP
green fluorescent protein
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase
- PI
propidium iodide
Footnotes
This paper was submitted directly (Track II) to the Proceedings Office.
References
- 1.Evans A E, Jenkin R D, Sposto R, Ortega J A, Wilson C B, Wara W, Ertel I J, Kramer S, Chang C H, Leikin S L, Hammond G D. J Neurosurg. 1990;72:572–582. doi: 10.3171/jns.1990.72.4.0572. [DOI] [PubMed] [Google Scholar]
- 2.Jenkin D, Goddard K, Armstrong D, Becker L, Berry M, Chan H, Doherty M, Greenberg M, Hendrick B, Hoffman H, et al. Int J Radiat Oncol Biol Phys. 1990;19:265–274. doi: 10.1016/0360-3016(90)90533-p. [DOI] [PubMed] [Google Scholar]
- 3.Halberg F E, Wara W M, Fippin L F, Edwards M S, Levin V A, Davis R L, Prados M B, Wilson C B. Int J Radiat Oncol Biol Phys. 1991;20:651–654. doi: 10.1016/0360-3016(91)90004-n. [DOI] [PubMed] [Google Scholar]
- 4.Krischer J P, Ragab A H, Kun L, Kim T H, Laurent J P, Boyett J M, Cornell C J, Link M, Luthy A R, Camitta B. J Neurosurg. 1991;74:905–909. doi: 10.3171/jns.1991.74.6.0905. [DOI] [PubMed] [Google Scholar]
- 5.Sheline G E. Cancer. 1977;39:873–881. doi: 10.1002/1097-0142(197702)39:2+<873::aid-cncr2820390725>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 6.Chang C H, Horton J, Schoenfeld D, Salazer O, Perez-Tamayo R, Kramer S, Weinstein A, Nelson J S, Tsukada Y. Cancer. 1983;52:997–1007. doi: 10.1002/1097-0142(19830915)52:6<997::aid-cncr2820520612>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 7.Dee S, Haas-Kogan D A, Israel M A. Cell Death Differ. 1995;2:267–275. [PubMed] [Google Scholar]
- 8.Saylors R L, III, Sidransky D, Friedman H S, Bigner S H, Bigner D D, Vogelstein B, Brodeur G M. Cancer Res. 1991;51:4721–4723. [PubMed] [Google Scholar]
- 9.Biegel J A, Burk C D, Barr F G, Emanuel B S. Cancer Res. 1992;52:3391–3395. [PubMed] [Google Scholar]
- 10.Adesina A M, Nalbantoglu J, Cavenee W K. Cancer Res. 1994;54:5649–5651. [PubMed] [Google Scholar]
- 11.Ellison D W, Gatter K C, Steart P V, Lane D P, Weller R O. J Pathol. 1992;168:383–386. doi: 10.1002/path.1711680408. [DOI] [PubMed] [Google Scholar]
- 12.Wu J K, Ye Z, Darras B T. Neurosurgery. 1993;33:824–830. doi: 10.1227/00006123-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Chen P, Iavarone A, Fick J, Edwards M, Prados M, Israel M A. Cancer Genet Cytogenet. 1995;82:106–115. doi: 10.1016/0165-4608(94)00213-u. [DOI] [PubMed] [Google Scholar]
- 14.Haas-Kogan D A, Dazin P, Hu L, Deen D F, Israel M A. Cancer J Sci Am. 1996;2:114–121. [PubMed] [Google Scholar]
- 15.Haas-Kogan D A, Yount G, Haas M, Levi D, Kogan S S, Hu L, Vidair C, Deen D F, Dewey W C, Israel M A. Int J Radiat Oncol Biol Phys. 1996;36:95–103. doi: 10.1016/s0360-3016(96)00244-1. [DOI] [PubMed] [Google Scholar]
- 16.Yount G L, Haas-Kogan D A, Vidair C A, Haas M, Dewey W C, Israel M A. Cancer Res. 1996;56:500–506. [PubMed] [Google Scholar]
- 17.Rasheed B K, McLendon R E, Herndon J E, Friedman H S, Friedman A H, Bigner D D, Bigner S H. Cancer Res. 1994;54:1324–1330. [PubMed] [Google Scholar]
- 18.Chozick B S, Pezzullo J C, Epstein M H, Finch P W. Neurosurgery. 1994;35:831–837. doi: 10.1227/00006123-199411000-00005. ; discussion 837–838. [DOI] [PubMed] [Google Scholar]
- 19.Craig R W. Semin Cancer Biol. 1995;6:35–43. doi: 10.1006/scbi.1995.0005. [DOI] [PubMed] [Google Scholar]
- 20.Reed J C, Miyashita T, Takayama S, Wang H G, Sato T, Krajewski S, Aime-Sempe C, Bodrug S, Kitada S, Hanada M. J Cell Biochem. 1996;60:23–32. doi: 10.1002/(SICI)1097-4644(19960101)60:1%3C23::AID-JCB5%3E3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 21.Yonish-Rouach E, Resnitzky D, Lotem J, Sachs L, Kimchi A, Oren M. Nature (London) 1991;352:345–347. doi: 10.1038/352345a0. [DOI] [PubMed] [Google Scholar]
- 22.Debbas M, White E. Genes Dev. 1993;7:546–554. doi: 10.1101/gad.7.4.546. [DOI] [PubMed] [Google Scholar]
- 23.Clarke A R, Purdie C A, Harrison D J, Morris R G, Bird C C, Hooper M L, Wyllie A H. Nature (London) 1993;362:849–852. doi: 10.1038/362849a0. [DOI] [PubMed] [Google Scholar]
- 24.Lowe S W, Schmitt E M, Smith S W, Osborne B A, Jacks T. Nature (London) 1993;362:847–849. doi: 10.1038/362847a0. [DOI] [PubMed] [Google Scholar]
- 25.Lowe S W, Ruley H E, Jacks T, Housman D E. Cell. 1993;74:957–967. doi: 10.1016/0092-8674(93)90719-7. [DOI] [PubMed] [Google Scholar]
- 26.Lowe S W, Ruley H E. Genes Dev. 1993;7:535–545. doi: 10.1101/gad.7.4.535. [DOI] [PubMed] [Google Scholar]
- 27.Caelles C, Helmberg A, Karin M. Nature (London) 1994;370:220–223. doi: 10.1038/370220a0. [DOI] [PubMed] [Google Scholar]
- 28.Haupt Y, Rowan S, Shaulian E, Vousden K H, Oren M. Genes Dev. 1995;9:2170–2183. doi: 10.1101/gad.9.17.2170. [DOI] [PubMed] [Google Scholar]
- 29.Chen X, Ko L J, Jayaraman L, Prives C. Genes Dev. 1996;10:2438–2451. doi: 10.1101/gad.10.19.2438. [DOI] [PubMed] [Google Scholar]
- 30.Haupt, Y., Rowan, S., Shaulian, E., Kazaz, A., Vousden, K. & Oren, M. (1997) Leukemia 11, Suppl. 3, 337–339. [PubMed]
- 31.Miyashita T, Reed J C. Cell. 1995;80:293–299. doi: 10.1016/0092-8674(95)90412-3. [DOI] [PubMed] [Google Scholar]
- 32.Ludwig R L, Bates S, Vousden K H. Mol Cell Biol. 1996;16:4952–4960. doi: 10.1128/mcb.16.9.4952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Friedlander P, Haupt Y, Prives C, Oren M. Mol Cell Biol. 1996;16:4961–4971. doi: 10.1128/mcb.16.9.4961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miyashita T, Harigai M, Hanada M, Reed J C. Cancer Res. 1994;54:3131–3135. [PubMed] [Google Scholar]
- 35.Zhan Q, Alamo I, Yu K, Boise L H, Cherney B, Tosato G, O’Connor P M, Fornace A J., Jr Oncogene. 1996;13:2287–2293. [PubMed] [Google Scholar]
- 36.Anker L, Ohgaki H, Ludeke B I, Herrmann H D, Kleihues P, Westphal M. Int J Cancer. 1993;55:982–987. doi: 10.1002/ijc.2910550618. [DOI] [PubMed] [Google Scholar]
- 37.el-Deiry W S, Tokino T, Velculescu V E, Levy D B, Parsons R, Trent J M, Lin D, Mercer W E, Kinzler K W, Vogelstein B. Cell. 1993;75:817–825. doi: 10.1016/0092-8674(93)90500-p. [DOI] [PubMed] [Google Scholar]
- 38.Dulic V, Kaufmann W K, Wilson S J, Tlsty T D, Lees E, Harper J W, Elledge S J, Reed S I. Cell. 1994;76:1013–1023. doi: 10.1016/0092-8674(94)90379-4. [DOI] [PubMed] [Google Scholar]
- 39.Chao D T, Korsmeyer S J. Annu Rev Immunol. 1998;16:395–419. doi: 10.1146/annurev.immunol.16.1.395. [DOI] [PubMed] [Google Scholar]
- 40.Gupta N, Vij R, Haas-Kogan D A, Israel M A, Deen D F, Morgan W F. Radiat Res. 1996;145:289–298. [PubMed] [Google Scholar]
- 41.Gomez-Manzano C, Fueyo J, Kyritsis A P, Steck P A, Roth J A, McDonnell T J, Steck K D, Levin V A, Yung W K. Cancer Res. 1996;56:694–699. [PubMed] [Google Scholar]
- 42.Gomez-Manzano C, Fueyo J, Kyritsis A P, McDonnell T J, Steck P A, Levin V A, Yung W K. J Natl Cancer Inst. 1997;89:1036–1044. doi: 10.1093/jnci/89.14.1036. [DOI] [PubMed] [Google Scholar]
- 43.Knudson C M, Tung K S, Tourtellotte W G, Brown G A, Korsmeyer S J. Science. 1995;270:96–99. doi: 10.1126/science.270.5233.96. [DOI] [PubMed] [Google Scholar]
- 44.Zhan Q, Fan S, Bae I, Guillouf C, Liebermann D A, O’Connor P M, Fornace A J., Jr Oncogene. 1994;9:3743–3751. [PubMed] [Google Scholar]
- 45.Kitada S, Krajewski S, Miyashita T, Krajewska M, Reed J C. Oncogene. 1996;12:187–192. [PubMed] [Google Scholar]
- 46.McCurrach M E, Connor T M, Knudson C M, Korsmeyer S J, Lowe S W. Proc Natl Acad Sci USA. 1997;94:2345–2349. doi: 10.1073/pnas.94.6.2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yin C, Knudson C M, Korsmeyer S J, Van Dyke T. Nature (London) 1997;385:637–640. doi: 10.1038/385637a0. [DOI] [PubMed] [Google Scholar]
- 48.Kuerbitz S J, Plunkett B S, Walsh W V, Kastan M B. Proc Natl Acad Sci USA. 1992;89:7491–7495. doi: 10.1073/pnas.89.16.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yin Y, Tainsky M A, Bischoff F Z, Strong L C, Wahl G M. Cell. 1992;70:937–948. doi: 10.1016/0092-8674(92)90244-7. [DOI] [PubMed] [Google Scholar]
- 50.Livingstone L R, White A, Sprouse J, Livanos E, Jacks T, Tlsty T D. Cell. 1992;70:923–935. doi: 10.1016/0092-8674(92)90243-6. [DOI] [PubMed] [Google Scholar]