Abstract
Background:
Monthly Thorough Skin Self-Examination (TSSE) is an important practice for early detection of melanoma that is performed by a small minority of the population.
Design:
A randomized trial to determine whether a multi-component intervention can increase performance of TSSE, and to describe the effects on performance of skin surgeries, compared to a similar control intervention focused on diet.
Setting/participants:
1356 patients attending a routine primary care visit in southeastern New England
Intervention:
Participants received instructional materials, including cues and aids, a video, and a brief counseling session and (at 3 weeks) a brief follow-up phone call from a health educator, and tailored feedback letters.
Main Outcome Measures:
Performance of TSSE assessed by telephone interview and having a surgical procedure performed on the skin confirmed by examination of medical records
Results:
TSSE was performed by substantially more participants at 2, 6, and 12 months in the intervention group than in the control group (55% vs. 35%, p<0.0001 at 12 months). We also noted that a substantially higher proportion in the intervention group had skin surgery in the first 6 months (8.0% vs. 3.6%, p=0.0005), but there was no difference at 6 to 12 months (3.9% vs. 3.3%, p=0.5).
Conclusions:
The TSSE intervention was effective in increasing performance TSSE, that it resulted in increased surgery on the skin, and that increase in skin procedures only persisted for 6 months. Intervention to increase TSSE may result in long-term benefit in early detection of melanoma while causing only a short-term excess of skin surgeries.
Melanoma continues to be an important public health problem, with over 60,000 cases of invasive disease diagnosed each year and approximately 8000 deaths annually in the United States1. It has been a problem of great public concern, and although mortality has stabilized in recent years, incidence continues to rise despite decades of information campaigns.2, 3 National surveys of trends in sun exposure and the popularity of commercial tanning parlors suggest that primary prevention has not yet been effective.4
Early detection may be key to reducing melanoma mortality. For melanoma, early detection consists of “look and see”—looking at the skin (inspection) and seeing potential problem lesions (recognition) that require intervention.5 Early detection is best accomplished by professional skin examination by suitably trained clinicians and by thorough, systematic, careful skin self-examination, on a monthly basis, by the general public. Monthly thorough skin self-examination (TSSE) has been associated with substantially reduced melanoma mortality, and has been studied from several perspectives.6, 7
Unfortunately, TSSE is performed by only about 9 to 18% of the population, even though a much larger proportion may examine some areas of their skin less often than monthly, or without a careful, systematic approach.8, 9 Can this performance rate be increased? Will an increase in skin inspection lead to greater numbers of surgeries on benign lesions of the skin, with attendant cost and the potential for morbidity? If an intervention increases the rate of TSSE performance, will that increase be sustained? If it is sustained, will an increase in surgeries also be sustained, with resulting morbidity and cost?
We addressed these issues with a randomized trial comparing two interventions: one directed at early detection of melanoma (and other skin cancers), and a control intervention directed at assessment of diet.
METHODS
Enrollment and Randomization
The Check-It-Out Project was a randomized trial of an intervention developed to increase performance of TSSE. The study participants were recruited from 11 primary care practices in Rhode Island and nearby areas of Massachusetts between May 2000 and December 20019. The 26 participating clinicians in these practices volunteered for this study, so were likely to be more prevention-oriented than the general community of primary care clinicians. All participating primary care clinicians attended a CME workshop prior to initiation of recruitment in their offices. The workshop focused on skin cancer early detection based on the Basic Skin Cancer Triage (BSCT) curriculum to prepare them to appropriately manage any concerns that participants may present as a result of the intervention regarding skin lesions. 10, 11.
Patients scheduled for a routine primary care visit were interviewed by telephone prior to that visit (i.e. the baseline interview) (Figure 1). At the time of the visit, and after seeing the primary care clinician, a health educator obtained written consent, randomized participants into the skin examination or diet intervention group, and provided intervention materials and training in their use. Patients contacted before the visit may have failed to participate further in the study because their primary care appointment was changed or they did not appear for that visit (n=387), study personnel were unavailable at the end of the visit or the participant could not stay after their visit for the study (n=199), they declined participation after the pre-visit contact (n=107), they were found to be ineligible after the pre-visit contact (n=16), or for other reasons (n=61). After consent was obtained, randomization was performed by participant selection of an opaque envelope with the assignment enclosed. Toward the end of recruitment for this study, recruitment of women was stopped in order to increase the proportion of male participants.
Figure 1.
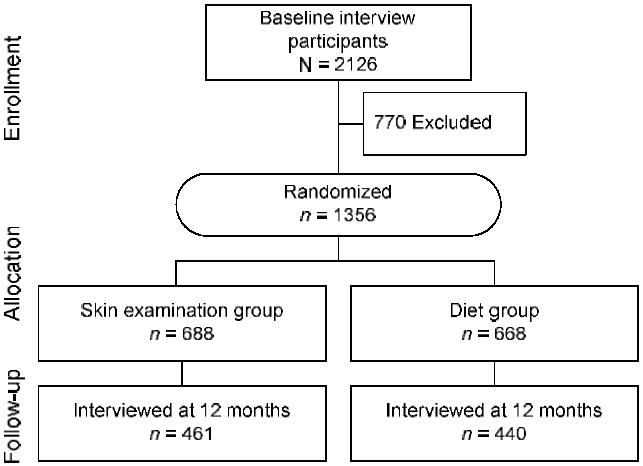
Participant flow in the Check-It-Out project
Approval was received from the three relevant Institutional Review Boards; verbal informed consent was obtained from all participants prior to initial pre-visit (baseline) telephone interview and signed informed consent was obtained from all participants prior to randomization.
Interventions
The “Skin Examination” group intervention was directed at increasing performance of TSSE for early detection of malignant melanoma (and other skin cancers). It involved giving participants educational materials, cues, aids, and a brief counseling intervention by a health educator; the physicians did not participate in the intervention and were not informed of the group to which the participant was randomized. The intervention was based on strategies known to promote behavior change (see below).
The educational materials advocated monthly TSSE with physician consultation for any new or changing skin lesions, and included the American Cancer Society booklet, “Why you should know about melanoma” and the 14-minute video produced for this project “Check It Out: Why and how to do Skin Self-Exam.”12 That video was created by the project team including physicians (dermatology and psychiatry), epidemiologists, medical educators, experts in health-related behavior change, and a professional video producer. The content was structured to address levels of commitment to TSSE, guided by the Transtheoretical Model stages-of-adoption perspective, and included motivation, information, and skills to address participants across stages of change with respect to total skin self-exam. Stages of change included (1) not considering the practice, (2) thinking about performing skin self-examinations, and (3) already performing skin self-examinations. The initial video segments were engaging and motivational; the final segment provided more concrete “how-to” guidance and demonstration. Environmental cues to action provided to patients (a key element of the Health Belief Model) included a refrigerator magnet in the shape of a hand mirror, with a reflective surface and the study logo, and a shower card that included directions for performing a TSSE on one side and warning signs for melanoma on the other. Aids to help patients perform self-examination procedures included a hand mirror and a body diagram for noting the location of individual lesions. All were created or adapted by the project team.
The comparison group received a diet intervention, which was intended to control for degree of contact, and was therefore preferable to a “usual care” condition. The diet intervention included a “Let's Eat Kit”, which has been previously described13, and included a “Rate Your Plate” instructional pamphlet as well as tips to improve diet. Similar to the skin examination intervention, a brief video was used to motivate, inform, and improve skills with respect to using the “Let's Eat Kit” to decrease dietary fat and to complete the “Rate Your Plate” approach.
The individually tailored brief counseling session for participants included a description of the justification and implementation of thorough skin self-examination performance (for those in the intervention group) or dietary modification (for those in the comparison group), and agreement on an action plan. The creation of an action plan was based on principles of Social Cognitive Theory that emphasizes the need to give people a clear plan for behavior change. The health educator made a follow-up call 3 weeks later to discuss the participant's success with the agreed-upon plan and to answer any questions that may have arisen.
After the 2 and 6 month interviews, each participant in the skin examination group also received a feedback letter individually tailored on their TSSE performance, perceived risk of skin cancer, intention to perform TSSE, and availability of a partner to help with TSSE. The diet group received corresponding tailored letters regarding “Rate Your Plate”.
Measures
All participants were asked to complete follow-up telephone interviews at 2, 6, and 12 months after randomization. These interviews asked questions relevant to behaviors targeted by both interventions, and interviewers were not informed of the respondent's intervention assignment prior to any of these interviews. Participants were asked how often in the prior 2 months they had carefully examined each of seven areas of the body (the front of you from the waist up, the front of your thighs and legs, the bottoms of your feet, your calves, the backs of your thighs, your buttocks and lower parts of your back, and your upper back). Those who responded “once” or more times to each of these 7 questions were considered to have performed TSSE 9.
Skin surgeries were determined by examination of medical records of patients who reported a procedure, and were analyzed by intention to treat. We determined the CPT code of each procedure from the treating physician's office and assigned it a dollar value based on the Fee Schedule for Physicians' Services for CY 2003. We were unable to determine the number of physician visits for the participants. Actual skin cancer risk was measured by the BRAT scale14. Perceived skin cancer risk was assessed on a 1 to 5 scale from “very high” to “very low”. Attitudes related to TSSE were measured by the two scales (“positive personal gain” and “bodily or social unease”)15.
Statistical Analysis
Comparison of groups on categorical variables were assessed using χ2 analyses. Comparison of intervention groups on number of areas of the body examined was assessed using t-tests, and on costs using Wilcoxon 2-sample tests. The association of baseline (pre-visit) variables with performance of TSSE was assessed using logistic regression. Based on our pre-study power calculations, we sought to retain 908 participants through the last telephone interview. Statistical analyses were performed in 2004–2006 using Statistical Analysis Package (SAS, Cary, NC). P-values are two-sided.
A repeated measures analysis using GEE-based mixed effects models was also performed as a supplement to the cross-sectional analysis that was done at each of the observed time-points. Specifically, TSSE performance was modeled with fixed effects ‘time’, ‘(intervention) group’, and their interaction. The subject or patient-specific effect was incorporated via a random intercept term. A similar model was used for analyzing the response variable ‘surgical procedures on skin’. By combining data across time-points, such an analysis allows us to examine the effect of intervention over time, in a comprehensive manner. The results from this line of analysis are summarized at the end of the Results section.
RESULTS
Participation and Group Assignment
The Check-It-Out project enrolled 1356 participants (688 in the skin group and 668 in the diet group) during April 2000 through November 2001, in 11 practices with 56 to 230 participants per practice, and 26 primary care clinicians in those practices. Those who were randomized were 2.7 years older on average, slightly more educated, and more likely to be unemployed or retired, to have had a skin surgery, to have received physician advice to perform TSSE, and to perceive their risk of skin cancer to be greater than those who participated in the baseline interview but were not randomized (Table 1). However, those randomized were not more likely to report performing TSSE and did not differ from those not randomized in our measures of attitudes and self-efficacy.
Table 1.
Baseline characteristics
| Randomized | Group assignment | Retained at 12 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | No | Yes | p | Skin* | Diet | p | Yes | No | p |
| n | 770 | 1356 | 688 | 668 | 901 | 455 | |||
| Proportion performing TSSE at baseline | 19% | 17% | 0.3 | 18% | 17% | 0.7 | 17% | 18% | 0.7 |
| Number of areas examined | 2.7 | 2.5 | 0.2 | 2.6 | 2.5 | 0.4 | 2.6 | 2.4 | 0.4 |
| Procedure in 6 months before baseline | 6% | 5% | 6% | 0.6 | 6% | 6% | 0.9 | ||
| Age in years (mean) | 50.5 | 53.2 | <.0001 | 54.0 | 52.5 | 0.056 | 53.9 | 52.0 | 0.04 |
| Age in years (SD) | 15.5 | 14.8 | 14.7 | 15.0 | 14.3 | 15.8 | |||
| Proportion men | 40.7% | 41.7% | 0.7 | 44.0% | 39.2% | 0.08 | 41.6% | 41.8% | 1.0 |
| Education | 0.02 | 0.4 | 0.014 | ||||||
| Less than high school | 9% | 6% | 7% | 5% | 6% | 6% | |||
| High school graduate | 26% | 28% | 27% | 28% | 28% | 27% | |||
| Some after high school | 28% | 29% | 29% | 29% | 26% | 33% | |||
| College graduate | 37% | 38% | 37% | 38% | 40% | 33% | |||
| % employed | 66% | 61% | 0.02 | 60% | 62% | 0.5 | 61% | 61% | 0.8 |
| Advice from MD office to SSE | 27% | 31% | 0.03 | 32% | 30% | 0.4 | 34% | 26% | 0.003 |
| Wall mirror | 79% | 81% | 0.3 | 80% | 82% | 0.4 | 81% | 81% | 1.0 |
| Need glasses or contacts to examine | 56% | 60% | 0.12 | 26% | 27% | 0.8 | 62% | 56% | 0.08 |
| Someone helps or could help with TSSE | 80% | 83% | 0.12 | 83% | 83% | 0.8 | 84% | 80% | 0.08 |
| Estimated skin cancer risk (BRAT) | 0.12 | 0.13 | 0.4 | ||||||
| High | 21% | 24% | 25% | 24% | 24% | 24% | |||
| Moderate | 36% | 36% | 33% | 38% | 37% | 34% | |||
| Low | 43% | 40% | 42% | 38% | 39% | 42% | |||
| Perceived skin cancer risk | 3.36 | 3.26 | 0.05 | 3.28 | 3.25 | 0.6 | 3.23 | 3.32 | 0.15 |
| Confidence (on 1 to 10 scale) | |||||||||
| in performing TSSE | 8.0 | 7.9 | 0.6 | 8.0 | 7.9 | 0.6 | 8.0 | 7.9 | 0.4 |
| in detecting a serious problem | 6.8 | 6.8 | 0.7 | 6.8 | 6.9 | 0.5 | 6.9 | 6.7 | 0.4 |
| Attitude towards TSSE (on 1 to 4 scale) | |||||||||
| Positive personal gain | 3.3 | 3.3 | 0.2 | 3.4 | 3.3 | 0.5 | 3.4 | 3.3 | 0.6 |
| Bodily or social unease | 1.7 | 1.7 | 0.8 | 1.7 | 1.7 | 0.6 | 1.7 | 1.7 | 0.3 |
SD, standard deviation; TSSE, thorough skin self-examination
The two randomized intervention groups (“skin examination” and “diet”) were equivalent in baseline demographic and TSSE performance characteristics (Table 1). In each practice, 45-54% of the participants were assigned to the skin intervention. Of those randomized, 1084 (80%) were followed at 2 months, 1017 (75%) were followed at 6 months, and 901 (66%) were followed at 12 months. There was no differential follow-up in the skin examination vs. diet group (80% vs 80%, p=.8 at 2 months; 77% vs 73% at 6 months, p=.13; and 67% vs 66% at 12 months, p=.7). Participants were more likely to be retained for the entire 12 months of follow-up if prior to the randomization visit they had been advised by their provider or his/her office staff to examine their skin regularly (Table 1). Also, retention was associated with education: those who were college graduates were somewhat more likely to be retained in the study and others with some education after high school were less likely to be retained. Those retained were also 1.9 years older. There were no differences in retention by performance of TSSE at baseline or in other characteristics examined. Of those not retained, 19% refused, one had died, and the remainder could not be reached during the interviewing window.
TSSE Performance
There were no differences between the skin intervention group and the diet intervention control in TSSE performance at the pre-visit (baseline) interview (18% vs. 17%, p=.7), but a marked difference between the groups emerged at 2 months (53% vs. 31%, p<.0001), and was sustained at 6 months (55% vs. 35%, p<.0001) and 12 months (55% vs. 35%, p<.0001). A corresponding difference was noted in the number of areas of the body examined among the 7 specifically queried (Table 2). The largest difference between groups at all time points after intervention was in examination of the buttocks and low back, and generally smaller differences in examination of the front of the body and bottoms of the feet, although all areas showed substantial differences in the proportion who carefully examined them (data not shown).
Table 2.
Skin self-examination practices
| Months after randomization |
TSSE performance group |
Number of areas examineda group | |||||
|---|---|---|---|---|---|---|---|
| Skin | Diet | p | Difference (95% CI) | Skin | Diet | p | |
| 0 (baseline) | 18% | 17% | 0.7 | 0.7 (−3.4, 4.7) | 2.59 | 2.46 | 0.4 |
| 2 | 53% | 31% | <.0001 | 22.9 (17.2, 28.6) | 5.34 | 3.86 | <0.0001 |
| 6 | 55% | 35% | <.0001 | 19.8 (13.8, 25.8) | 5.22 | 4.00 | <0.0001 |
| 12 | 55% | 35% | <.0001 | 19.3 (13.0, 25.7) | 5.14 | 3.83 | <0.0001 |
of the 7 areas specifically queried
TSSE, thorough skin self-examination
Several baseline variables were examined for a possible association with TSSE performance and as possible moderators (effect modifiers) of the association between intervention and TSSE performance. There was no strong indicator of a main effect nor an effect modification for demographic factors including age, gender, education, and income. The sole exception was an association of TSSE performance with income and a weak moderation of the intervention effect by income, each at only one time point (the 6 month assessment).
Requiring glasses or contacts to perform the examination at baseline was not associated with TSSE performance at follow-up or with the magnitude of the intervention effect. However, those who indicated at baseline that they had been advised by their doctor or his/her office staff to regularly examine their skin (31%) were more likely to do so at all time points (Table 3). Those who had someone who either helped them or whom they would feel comfortable asking to help them were not consistently more likely to perform TSSE. Also, neither the performance of TSSE nor the effect of intervention was modified by our measures of actual (BRAT score) or perceived skin cancer risk. Our baseline measures of greater self-efficacy and attitudes (more positive personal gain and less bodily or social unease) were consistently predictive of greater TSSE performance at all time points.
Table 3.
Association of baseline variables with TSSE performance
| Odds ratio (95% CI) | |||
|---|---|---|---|
| Timepoint of TSSE | Physician advice (received vs not) |
Wall mirror (available vs. not) |
Someone to help (yes vs. no) |
| 0 (baseline) | 2.3 (1.5-3.4) | 3.9 (1.8-8.6) | 1.1 (0.6-1.9) |
| 2 months | 2.4 (1.6-3.5) | 1.7 (1.0-2.9) | 1.9 (1.1-3.4) |
| 6 months | 1.9 (1.3-2.8) | 1.3 (0.8-2.2) | 1.7 (1.0-3.0) |
| 12 months | 2.3 (1.5-3.5) | 1.3 (0.8-2.2) | 0.9 (0.6-1.6) |
CI, confidence interval; TSSE, thorough skin self-examination
Wall Mirrors
There was no difference between intervention groups in availability of a wall mirror at home at baseline. Throughout the trial about 17%–19% of the diet intervention group had no wall mirror available for examination of their skin. However, in the skin examination group, that proportion declined from 20% at baseline to 11%–12% at 6 and 12 months, and the difference between groups was significant at all time points after intervention (Table 4).
Table 4.
Intervention effect on the availability of a wall mirror
| Skin Examination | Diet | Difference | ||||
|---|---|---|---|---|---|---|
| Available | n | Available | n | pa | % (95% CI) | |
| Baseline | 80% | 550 | 82% | 547 | .4 | −1.9 (−2.2, 6.1) |
| 2 months | 86% | 469 | 81% | 432 | .03 | +4.8 ( 0.4, 9.3) |
| 6 months | 89% | 471 | 82% | 399 | .0007 | +7.4 ( 3.1,11.8) |
| 12 months | 88% | 407 | 83% | 368 | .04 | +4.7 ( 0.1, 9.2) |
chi-square test
CI, confidence interval
Those with a wall mirror at baseline were more likely to perform TSSE at baseline, and to some extent at 2 months, but not at 6 or 12 months. However, in analyses that were stratified by intervention group, those with a wall mirror at each time point were more likely to perform TSSE at that time point (data not shown).
Skin Surgeries
We found no differences between groups in the proportion who had skin surgeries (biopsy, cut, or freeze) during the 6 months prior to randomization as verified by the treating clinician's report of the corresponding CPT code (Table 5). However, we did find a substantially higher proportion of participants who had these procedures in the skin examination group during the first 6 months after intervention, but not during later periods (Figure 2). Corresponding to this, the skin examination group had higher costs per participant for skin surgeries during the first 6 months after randomization. There were no differences in the costs per participant during the 6 months prior to randomization, or between 6 and 12 months after randomization.
Table 5.
Procedures performed on the skina
| Period in months (randomization=0) |
Patients with procedures % (n) | Difference % (95% CI) |
Cost per participant ($) |
||||
|---|---|---|---|---|---|---|---|
| Skin exam. | Diet | p | Skin | Diet | pb | ||
| −6 to 0 | 6.0% (41) | 5.2% (35) | 0 .6 | 0.7 (−1.7, 3.2) | 12.92 | 13.32 | 0.5 |
| 0 to 6 | 8.0% (55) | 3.6% (24) | 0.0005 | 4.4 (1.9, 6.9) | 16.81 | 4.96 | 0.0005 |
| 6 to 12 | 3.9% (27) | 3.3% (22) | 0.5 | 0.6 (−1.4, 2.6) | 7.62 | 9.22 | 0.6 |
based on intent to treat analysis
p-value calculated using Wilcoxon 2-sample test
CI, confidence interval
Figure 2.
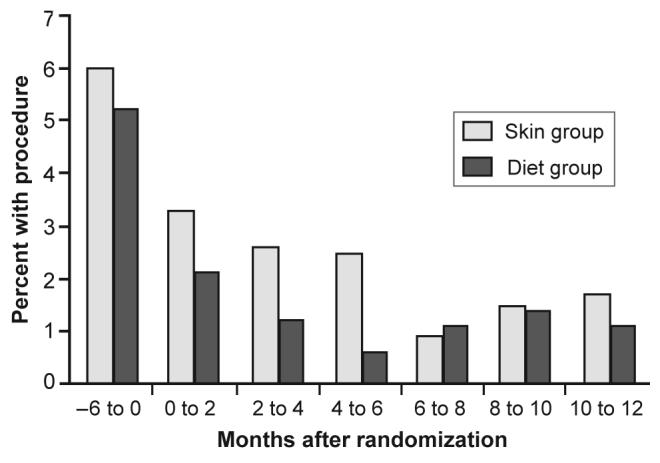
Proportion of patients with procedures performed on the skin
Skin Cancers and Severe Dysplasias Detected
We examined participants' pathology reports for evidence of cutaneous malignancies and severe melanocytic dysplasias diagnosed from 6 prior to randomization to12 months after randomization. We noted only one melanoma diagnosed in the study population (in the diet group), and two participants diagnosed with severely atypical nevi (one in each group). Squamous cell carcinoma of the skin, which generally occurs on the frequently seen areas of the face or ears, was diagnosed in the year after randomization in 3 participants in the skin examination group and 4 in the diet group. Basal cell carcinoma, which is the most likely of any of these to be diagnosed on the face, and also the most common, was diagnosed during the year after randomization in 7 skin examination group participants and 3 diet group participants. The remainder of the lesions biopsied or excised after randomization were benign.
Repeated Measures (GEE) Analyses
The intervention group had a significant influence over time on TSSE performance (p value < 0.0001). However, the significance did not carry over to the other response variable of interest, “surgical procedures on the skin” (p value = 0.6). This observation is entirely consistent with the substantial and significant difference observed between groups in skin surgeries during the six months after randomization that were absent during the other two six-month periods. We repeated the analyses, after adjusting for plausible covariates of interest, such as “education” and “availability of wall-mirror.” The former could be thought of as a surrogate for “income,” which had a sizeable amount of missing data, and the latter was entered as a time-varying covariate, since the availability of wall-mirror could change over the study period. There was no change in the overall significance (or non-significance) of either model after adjustment, and the adjusted p-values were not very different from the unadjusted ones mentioned earlier.
DISCUSSION
Melanoma is a major public health problem in the United States. The central irony in the melanoma epidemic is that most fatal melanomas were visible on the surface of the skin in a curable phase of their evolution, yet no one either noticed or responded to them in time. Given evidence suggesting that monthly skin self-examination can save lives, we sought to evaluate an intervention to encourage this practice, both for its efficacy as well as its possible effect on increasing the number and cost of skin surgeries.
Full body skin examination by clinicians has been addressed by groups such as the U.S. Preventive Services Task Force that concluded “the evidence is insufficient to recommend for or against routine screening for skin cancer using a total-body skin examination for the early detection of cutaneous melanoma” although it did note that “clinicians should remain alert for skin lesions with malignant features noted in the context of physical examinations performed for other purposes”, and that “all of these organizations [whose recommendations were reviewed] advise public or patient education to change behaviors … including … skin self-examination”16
We do note that the evidence supporting the efficacy of TSSE for reducing morbidity and mortality from melanoma, although substantial, does not include randomized trials, and is limited in quality and quantity. We also note that TSSE differs from many other screening tests because the test itself does not require a professional examiner or expensive equipment and is free of significant cost and discomfort. The adverse effects associated with TSSE, such as skin surgeries, are not as severe as with other screening procedures, so one may consider that the standard of proof required for action should be correspondingly lower.
Reports of predictors of SSE have been published,9, 17-25 and reports of accuracy of those self-examinations.26-28 Two randomized trials of SSE interventions have also been reported. Oliveria et al intervened with high risk patients (five or more clinically dysplastic nevi) seeking care at a specialized clinic who received physician and nurse education on the conduct of SSE. The experimental intervention involved provision of a book of photographs covering all of the participants' skin and appropriate instructions on its use for SSE. A higher proportion of the intervention group reported at least 3 SSEs in the 4 months after intervention compared to controls (61% vs. 37%, p=0.03).29
Aitken et al. randomized 18 communities in Queensland, Australia, half of which received an intervention consisting of (1) community education regarding SSE and professional skin examination for early detection of melanoma delivered by seminars and by a self-help guide that was delivered to all members of the community, (2) physician education, and (3) free skin screening clinics. Although at the end of the 3-year intervention period, the residents of the intervention communities were more likely than residents of the control communities to report that their doctor had advised them to conduct a SSE (26% vs 19%) and had shown them how to do so (16% vs 9%), there was no difference in the proportion that reported conducting SSE despite an increase in professional examinations.30 Both of the above studies asked about thorough SSE with a single question.
We found that our intervention was quite successful at increasing the practice of TSSE, and that increase was sustained for the year of follow-up. Along with that was a sustained increase in the availability of a key tool for TSSE, the wall mirror. We also found that a smaller increase in TSSE occurred in the “diet” comparison group (without a change in the availability of a wall mirror), which we attribute to two factors. First, prior to initiating recruitment in their offices, the primary care clinicians from whose practices we recruited the study population were all educated with our Basic Skin Cancer Triage curriculum which includes education on TSSE. The physicians did not know the group assignments of the participants, but they could have spread a TSSE message to a wide range of patients. Second, all participants in both groups were questioned about conduct of TSSE and related issues during the study. Both of these factors may have influenced their TSSE performance.
The fact that self-efficacy and the two attitudinal variables were predictive of greater TSSE regardless of group membership implies that these areas merit additional attention in future interventions, whether separately or as added emphases in a revised version of this intervention's materials.
Skin surgeries were more often performed in the “skin examination” group than in the “diet” group during the 6 months after intervention, but not prior to or more than 6 months after intervention, and these additional surgeries were not associated with additional malignant diagnoses. This is a noteworthy finding because of its implications for campaigns directed at increasing TSSE. If the sustained increase in performance of TSSE were associated with a sustained increase in surgeries for benign conditions, it might indicate that there is a significant adverse long-term consequence in morbidity and cost to the TSSE intervention. However, our data suggest that the increase in surgeries is transient. We suspect that when people first examine their skin more closely they initially may seek medical attention for innocuous lesions that may have been present and unchanged, but also unnoticed, for many years. The medical attention may lead to surgical intervention that in retrospect is unnecessary. However, it appears that after 6 months of scrutinizing the skin they become sufficiently familiar with their skin lesions that observing these no longer arouses concern or provokes surgical interventions. Hence in the long run, there is increased scrutiny of the skin and thus presumably melanomas will be detected earlier - but the extra expense and morbidity of needless surgery is avoided.
Only 2% of surgeries revealed malignancies or severe dysplasias, half of which were basal cell carcinomas (BCCs). Delay in treatment of BCC, unless the delay is very long, generally has little or no impact on morbidity, and no impact on mortality.31 One may therefore suspect that the excess surgeries during the first 6 months after intervention had little or no long-term beneficial impact on the lives of these patients. We did not examine medical records to determine the circumstances for each surgery performed during follow-up.
A major limitation of this study was its reliance on self-report of TSSE performance. We did not consider it feasible to verify TSSE performance by direct observation of this activity, since it typically occurs in the privacy of one's home when one is undressed. Also, our intervention did involve multiple components, and we cannot determine from our data which of these accounts for the intervention's success. Less intensive interventions may also be effective; we chose the more intensive approach to demonstrate that we can successfully intervene on this practice, which we have done. Due to funding constraints, we did not follow these patients long enough to determine the duration of the effect of this intervention on TSSE performance beyond one year, although this would have been desirable. Strengths of our effort include study of a population that was not restricted to very high risk individuals (since most melanomas do not develop among individuals recognized to be at very high risk). Therefore, our results are potentially quite broadly applicable and may have substantial impact on the overall societal burden of melanoma. We were also careful to use a definition of TSSE that involved sufficient detail that it excluded those who might say they thoroughly examine their skin even though they failed to scrutinize important areas for melanoma early detection.
The intervention we performed leads to a sustained increase in TSSE performance and a transient increase in skin surgeries. We hope that this performance of TSSE, in combination with public and professional awareness of warning signs for melanoma, will substantially reduce death from this disease.
ACKNOWLEDGEMENTS
This research was supported by grant R01CA78800 from the National Cancer Institute. Dr. Weinstock also is supported by grants CSP402 and CSP562 from the Department of Veterans Affairs, and grants R01CA106592, R01AR49342 and R01CA106807 from the National Institutes of Health. The authors thank Margaret Boyle, Aimee Bono, Erin Hunt, and David Upegui for their outstanding efforts on this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial conflict of interest was reported by the authors of this paper.
REFERENCES
- 1.Cancer Facts & Figures 2006 Available at: www.cancer.org. Accessed 2-14-2006.
- 2.Coory M, Baade P, Aitken J, Smithers M, McLeod GR, Ring I. Trends for in situ and invasive melanoma in Queensland, Australia, 1982-2002. Cancer Causes Control. 2006 Feb;17(1):21–27. doi: 10.1007/s10552-005-3637-4. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Devesa SS, Hartge P, Tucker MA. Recent trends in cutaneous melanoma incidence among whites in the United States. Journal of the National Cancer Institute. 2001;93:678–683. doi: 10.1093/jnci/93.9.678. [DOI] [PubMed] [Google Scholar]
- 4.Cokkinides V, Weinstock M, Glanz K, Albano J, Ward E, Thun M. Trends in sunburns, sun protection practices, and attitudes toward sun exposure protection and tanning among U.S. adolescents, 1998-2004. Pediatrics. 2006 Sep;118(3):853–864. doi: 10.1542/peds.2005-3109. [DOI] [PubMed] [Google Scholar]
- 5.Weinstock MA. Cutaneous melanoma: public health approach to early detection. Dermatol Ther. 2006 Jan-Feb;19(1):26–31. doi: 10.1111/j.1529-8019.2005.00053.x. [DOI] [PubMed] [Google Scholar]
- 6.Weinstock MA. Early detection of melanoma. Journal of the American Medical Association. 2000;284:886–889. doi: 10.1001/jama.284.7.886. [DOI] [PubMed] [Google Scholar]
- 7.Berwick M, Begg CB, Fine JA, Roush GC, Barnhill RL. Screening for cutaneous melanoma by skin self-examination. Journal of the National Cancer Institute. 1996;88:17–23. doi: 10.1093/jnci/88.1.17. [DOI] [PubMed] [Google Scholar]
- 8.Weinstock MA, Martin RA, Risica PM, et al. Thorough skin examination for the early detection of melanoma. American Journal of Preventive Medicine. 1999;17(3):169–175. doi: 10.1016/s0749-3797(99)00077-x. [DOI] [PubMed] [Google Scholar]
- 9.Weinstock MA, Risica PM, Martin RA, et al. Reliability of assessment and circumstances of performance of thorough skin self-examination for the early detection of melanoma in the Check-It-Out Project. Prev Med. 2004 Jun;38(6):761–765. doi: 10.1016/j.ypmed.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 10.Weinstock MA, Goldstein MG, Dub CE, Rhodes AR, Sober AJ. Basic Skin Cancer Triage for teaching melanoma detection. Journal of the American Academy of Dermatology. 1996;34:1063–1066. doi: 10.1016/s0190-9622(96)90287-x. [DOI] [PubMed] [Google Scholar]
- 11.Mikkilineni R, Weinstock MA, Goldstein MG, Dube CE, Rossi JS. The impact of the Basic Skin Cancer Triage Curiculum on Providers' skills, Confidence, and Knowledge in Skin Cancer control. Preventive Medicine. 2002;34:144–152. doi: 10.1006/pmed.2001.0961. [DOI] [PubMed] [Google Scholar]
- 12.American Cancer Society. The booklet “Why You Should Know About Melanoma” is downloadable from www.cancer.org. The video “Check It Out: Why and how to do Skin Self-Exam” can be ordered from the American Cancer Society (ACS code 2301.05).
- 13.Gans KM, Burkholder GJ, Risica PM, Harrow B, Lasater TM. Cost-effectiveness of minimal contact nutrition education strategies for cholesterol change. Ethnicity and Disease. 2006 Spring;16:443–451. [PubMed] [Google Scholar]
- 14.Glanz K, Schoenfeld E, Weinstock MA, Layi G, Kidd J, Shigaki DM. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detect Prev. 2003;27(4):311–315. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- 15.Smith KJ, Weinstock MA, Risica PM, et al. Evaluation of baseline attitudes toward thorough skin self-examination (TSSE) J Invest Dermatol. 2003;121:A457. [Google Scholar]
- 16.U. S. Preventive Services Task Force Screening for skin cancer: recommendations and rationale. Am J Prev Med. 2001;20(3S):44–46. [Google Scholar]
- 17.Oliveria SA, Christos PJ, Halpern AC, Fine JA, Barnhill RL, Berwick M. Evaluation of factors associated with skin self-examination. Cancer Epidemiol Biomarkers Prev. 1999 Nov;8(11):971–978. [PubMed] [Google Scholar]
- 18.Robinson JK, Fisher SG, Turrisi RJ. Predictors of skin self-examination performance. Cancer. 2002 Jul 1;95(1):135–146. doi: 10.1002/cncr.10637. [DOI] [PubMed] [Google Scholar]
- 19.Aitken JF, Janda M, Lowe JB, et al. Prevalence of whole-body skin self-examination in a population at high risk for skin cancer (Australia) Cancer Causes Control. 2004 Jun;15(5):453–463. doi: 10.1023/B:CACO.0000036451.39128.f6. [DOI] [PubMed] [Google Scholar]
- 20.Manne S, Fasanella N, Connors J, Floyd B, Wang H, Lessin S. Sun protection and skin surveillance practices among relatives of patients with malignant melanoma: prevalence and predictors. Prev Med. 2004 Jul;39(1):36–47. doi: 10.1016/j.ypmed.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 21.Arnold MR, DeJong W. Skin self-examination practices in a convenience sample of U.S. university students. Prev Med. 2005 Mar;40(3):268–273. doi: 10.1016/j.ypmed.2004.05.031. [DOI] [PubMed] [Google Scholar]
- 22.Manne S, Lessin S. Prevalence and correlates of sun protection and skin self-examination practices among cutaneous malignant melanoma survivors. J Behav Med. 2006 Oct;29(5):419–434. doi: 10.1007/s10865-006-9064-5. [DOI] [PubMed] [Google Scholar]
- 23.Hay JL, Oliveria SA, Dusza SW, Phelan DL, Ostroff JS, Halpern AC. Psychosocial mediators of a nurse intervention to increase skin self-examination in patients at high risk for melanoma. Cancer Epidemiol Biomarkers Prev. 2006 Jun;15(6):1212–1216. doi: 10.1158/1055-9965.EPI-04-0822. [DOI] [PubMed] [Google Scholar]
- 24.Robinson JK, Turrisi R, Stapleton J. Examination of mediating variables in a partner assistance intervention designed to increase performance of skin self-examination. J Am Acad Dermatol. 2006 Dec 2; doi: 10.1016/j.jaad.2006.10.028. [DOI] [PubMed] [Google Scholar]
- 25.Martin RA. Factors associated with thorough skin self-examination for the early detection of melanoma. Journal of the European Academy of Dermatology and Venereology. doi: 10.1111/j.1468-3083.2007.02199.x. in press. [DOI] [PubMed] [Google Scholar]
- 26.Hanrahan PF, Hersey P, Menzies SW, Watson AB, D'Este CA. Examination of the ability of people to identify early changes of melanoma in computer-altered pigmented skin lesions. Archives of Dermatology. 1997;133:301–311. [PubMed] [Google Scholar]
- 27.Oliveria SA, Chau D, Christos PJ, Charles CA, Mushlin AI, Halpern AC. Diagnostic accuracy of patients in performing skin self-examination and the impact of photography. Arch Dermatol. 2004 Jan;140(1):57–62. doi: 10.1001/archderm.140.1.57. [DOI] [PubMed] [Google Scholar]
- 28.Chiu V, Won E, Malik M, Weinstock MA. The use of mole-mapping diagrams to increase skin self-examination accuracy. J Am Acad Dermatol. 2006 Aug;55(2):245–250. doi: 10.1016/j.jaad.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 29.Oliveria SA, Dusza SW, Phelan DL, Ostroff JS, Berwick M, Halpern AC. Patient adherence to skin self-examination. effect of nurse intervention with photographs. Am J Prev Med. 2004 Feb;26(2):152–155. doi: 10.1016/j.amepre.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Aitken JF, Youl PH, Janda M, Lowe JB, Ring IT, Elwood M. Increase in skin cancer screening during a community-based randomized intervention trial. Int J Cancer. 2006 Feb 15;118(4):1010–1016. doi: 10.1002/ijc.21455. [DOI] [PubMed] [Google Scholar]
- 31.Eide MJ, Weinstock MA, Dufresne RG, Jr, et al. Relationship of treatment delay with surgical defect size from keratinocyte carcinoma (basal cell carcinoma and squamous cell carcinoma of the skin) J Invest Dermatol. 2005 Feb;124(2):308–314. doi: 10.1111/j.0022-202X.2004.23546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


