Abstract
Background
Empiric studies find that contextual factors affect individual weight status over and above individual socioeconomic characteristics. Given increasing levels of obesity, researchers are examining how the food environment contributes to unhealthy weight status. An important change to this environment is the increasing availability of away-from-home eating establishments such as restaurants.
Methods
This study analyzed the relationship between the restaurant environment and weight status across counties in the United States. Individual data from the 2002–2006 Behavioral Risk Factor Surveillance System (N=714,054) were linked with restaurant data from the 2002 U.S. Economic Census. Fast-food and full-service restaurant density, along with restaurant mix (the ratio of fast-food to full-service restaurants), were assessed. Analyses were conducted in 2006–2007.
Results
Fast-food restaurant density and a higher ratio of fast-food to full-service restaurants were associated with higher individual-level weight status (BMI and the risk of being obese). In contrast, a higher density of full-service restaurants was associated with lower weight status.
Conclusions
Area-level restaurant mix emerged as an important correlate of weight status, with components of the restaurant environment exhibiting differential associations. Hence, it is the availability of fast-food relative to other away-from-home choices that appears salient for unhealthy weight outcomes. Areas with a high density of full-service restaurants were indicative of a more healthful eating environment, suggesting a need for research into the comparative healthfulness of foods served at different types of restaurants. Future prospective studies are required to delineate causal pathways.
Introduction
With prevalence of obesity continuing to increase, much attention in public health has focused on the role of the physical and social environment in promoting higher weight status.1–4 In the United States, over 30% of adults are now obese and approximately 65% are categorized as overweight.5 Researchers have used terms such as “obesogenic”2 to describe environmental conditions that promote obesity, and recent empiric work has found that contextual factors (i.e., the social and physical attributes of communities) can independently influence weight status over and above individual-level social and economic factors.6–11
One behavior that is implicated in the changing weight status of Americans is the increasing patronage of restaurants.12–14 Restaurant food is known to possess higher calories and contain more fats and carbohydrates compared to foods prepared at home.15,16 Restaurants are generally classified as “fast food” if patrons pay before eating and as “full service” if patrons pay after eating (i.e., use waiters).15 Figure 1 shows how American eating patterns have shifted with a larger percentage of the overall food budget spent on restaurant food. The figure also highlights the increasing dominance of fast food, which has been of high concern to the public health community.17
Figure 1.
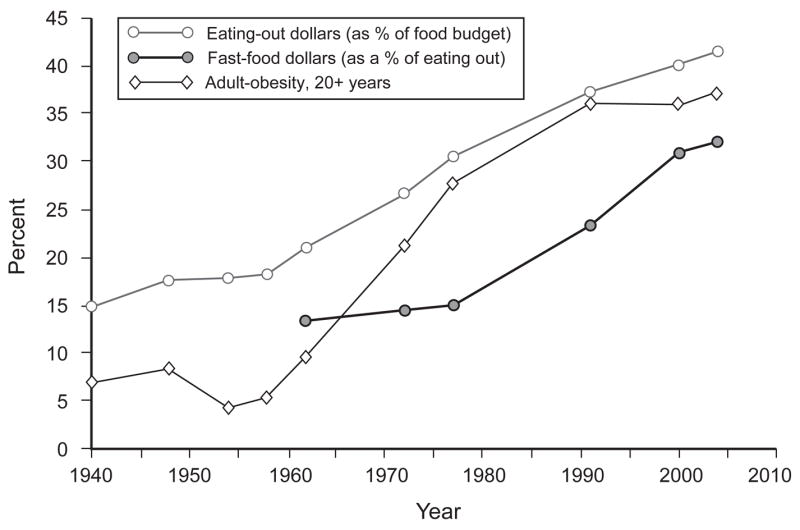
Trends in restaurant expenditures and obesity in the United States, 1940–2004. Sources: Obesity estimates obtained from Flegal et al.18 and Ogden et al.5 Food expenditure data are from U.S. Department of Agriculture Food Expenditure Tables.19
This study examines the relationship between the restaurant environment and weight status in U.S. adults. Weight status differs across communities and regions.20–22 For example, areas that are poor and more racially segregated have higher average weight status.10,20 Recent studies also have focused on how regional differences in weight status may be explained by the contextual restaurant environment.6,23–26 Research to date, however, has produced mixed results, and this study attempts to improve on prior methodologies. Two recent studies using state-level data found that a higher prevalence of restaurants is associated with higher weight status.6,23 In contrast, this study aggregates restaurant data to the county level rather than to the state level. The level of aggregation is important to modeling contextual factors because aggregation assumes that all individuals within each unit are subject to identical levels of exposure. Evidence shows that the distribution of restaurants is a function of local economic, social, and racial characteristics, suggesting that urban, suburban, and rural counties within a state exhibit substantial differences in the restaurant environment.27–29 Hence, using the county as the unit of aggregation likely poses a more suitable measure of restaurants.
Prior studies have measured the restaurant environment using units smaller than the state.24–26,30 These studies have been restricted to specific geographic regions using limited sample sizes. For example, Jeffery et al.25 reported no positive association between weight status and the number of fast-food and full-service restaurants within a 2-mile radius among a sample of approximately 1000 adults in Minnesota. Contextual effects on health-related outcomes have been found to be smaller than individual-level factors,31 and studies utilizing limited samples might not possess sufficient statistical power. In this study, data from a large and nationally representative cross-section of U.S. adults were utilized. Drawing from national data enabled the detection of population-level patterns that might not be identified with geographically limited data. Three other papers using smaller aggregated units also reported nonsignificant findings for the relationship between restaurant availability and weight status, although two were limited to children24,30 and one was conducted on an Australian sample.26 No large-scale study has previously examined this relationship using aggregation units smaller than the state.
This study models the independent contribution of both fast-food and full-service restaurants. Recent work indicates that consumers differentiate between fast-food and full-service restaurants in making choices about the nutritional content of meals,32 suggesting that these components of the restaurant environment have distinct relationships with weight status. Moreover, the association of each restaurant choice with weight status may be dependent on the availability of the alternate restaurant type. Stated another way, the restaurant mix may be a predictor of weight status because it most adequately describes the option set individuals face when choosing to eat outside the home. This study considers how the restaurant mix is associated with weight status by examining proportional measures (e.g., the ratio of fast-food to full-service restaurants) in addition to the independent contribution of fast-food and full-service restaurants.
Methods
Data
Individual-level data were drawn from the Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS is an annual telephone health survey representative of the non-institutionalized adult population of the U.S. aged 18 and over. Five years of BRFSS data (2002–2006) were linked with restaurant data from the 2002 U.S. Economic Census. The Economic Census is a census of economic activity in the U.S. conducted every 5 years. The Economic Census suppresses data on restaurants for less-populated counties. After linking the data, 544 counties were modeled, which represented approximately 75% of the 2002 U.S. population. In the BRFSS, a total of 876,091 respondents resided in the 544 counties. Pregnant women were excluded (~1%). Weight and/or height were unavailable in 5% of respondents, 12% were missing data on income, and an additional 1% had missing values on other variables, resulting in a final sample size of 714,054.
Measures
Restaurant density was measured as the number of restaurants per 10,000 individuals. Restaurants were further classified into fast-food or full-service categories consistent with prior studies in this area.6,27 BMI (kg/m2) and obese status (BMI≥30) served as dependent variables. Individual-level covariates included: age, age-squared, gender, race/ethnicity, education, and smoking status. Household income was measured in quartiles. County-level covariates were population size, median household income, and percentage of adults with a high school diploma.
Analysis
Two-level hierarchic regression models were employed.33 The linear equation was BMIij=β0+βxX+εij where BMIij was the predicted outcome for individual i in county j, β0 was the intercept, and βxX was a vector of level-1 coefficients and covariates. The intercept, β0, was treated as a random effect in the level-2 specification (β0= γ00+ γ0zZ+ μoj), where γ0zZ was a vector of level-2 coefficients and covariates. Logistic models were used to examine obese status. Dummy variables for census region were included as fixed effects to account for unmeasured regional characteristics.9,10 Model fit was assessed using chi-square likelihood ratio tests in HLM. Final models were tested against the null model and against models that contained only level-1 predictors. In each scenario the final models were significant at the p<0.001 level.
Some contextual variables were logarithmically transformed to produce a more normal distribution and reduce the effect of outliers. No evidence of interactions among the restaurant variables and individual characteristics were detected. Additionally, there were no significant interactions among the restaurant variables and other county-level characteristics including median household income, population size, and population density. Predictor variables were grand-mean centered. BRFSS sampling weights were used, and analyses were conducted with STATA, version 9.0 and HLM, version 6.03. The analysis was conducted in 2006–2007.
Results
Tables 1 and 2 summarize individual- and county-level variables, respectively. In the regression models, county-level variables were scaled by their inter-quartile range (the difference between the 25th and 75th percentiles) to aid in interpreting the magnitude of the estimated coefficients and allow for a standard comparison of effect sizes across contextual variables. Hence, Table 2 shows the 25th, 50th, and 75th percentile of the county-level predictors.
Table 1.
Individual characteristics (N=714,054)
| Variable | Mean (SD) or % |
|---|---|
| Outcomes | |
| BMI (kg/m2) | 26.9 (5.5) |
| Obese (BMI≥30 kg/m2) | 23% |
| Individual predictors | |
| Age (years) | 45.0 (16.5) |
| Female | 49% |
| Race/ethnicity | |
| Non-Hispanic white | 67% |
| Non-Hispanic black | 11% |
| Hispanics (all races) | 15% |
| Other race/ethnicity | 7% |
| Education | |
| Less than high school | 10% |
| High school graduate, no college | 26% |
| Some college/college graduate | 64% |
| Household income ($1000s) | 53.9 (39.5) |
| Smoking status | |
| Never smoked | 54% |
| Current smoker | 21% |
| Former smoker | 25% |
| No. respondents per county | 1313 (1472) |
Note: Data reflect BRFSS sampling weights. Number of respondents per county is unweighted.
Source: Behavioral Risk Factor Surveillance System (BRFSS), 2002–2006.
Table 2.
County-level variables—25th, 50th, and 75th percentiles (N=544)
| Variables | 25th | 50th | 75th |
|---|---|---|---|
| Restaurant variables (number per 10,000 individuals)a | |||
| Total restaurants (fast+full) | 13.3 | 15.1 | 17.3 |
| Fast food | 7.2 | 8.3 | 9.4 |
| Full service | 5.7 | 6.8 | 8.7 |
| Ratio (fast/full) | 1.0 | 1.2 | 1.4 |
| Other variables | |||
| Population sizeb (1000) | 122 | 199 | 439 |
| Median household incomec ($1000) | 37.1 | 41.9 | 50.3 |
| % High school diplomad | 80.1 | 83.3 | 87.2 |
Note: All variables measured in 2002 except % high school diploma, which is measured in 2000.
Sources: U.S. Economic Census, 2002;
Intercensal population estimates, U.S. Census, 2002;
Small area income & poverty estimates (SAIPE) U.S. Census, 2002;
U.S. Decennial Census, 2000
Table 3 presents regression coefficients for each variable without including the restaurant environment. Model I is a linear model predicting BMI, and Model II is a logistic model predicting obese status (BMI≥30). As expected, men, blacks, former smokers, the poor, and the least educated exhibit higher predicted BMI (Model I) and have increased odds of being obese (Model II). Since the county-level variables were scaled by their inter-quartile range, the β coefficients for each of these variables indicate the change in BMI (Model I) that is predicted to occur between the 25th and 75th percentile of the county-level predictor. For example, the difference in predicted BMI for counties with a median income of $37,100 (25th percentile) and $50,300 (75th percentile) is −0.13 kg/m2. In Model II, the β-coefficients for the county-level variables indicate the odds ratio of obesity between the 25th and 75th percentile of each county-level predictor.
Table 3.
Regression of weight status on individual and contextual predictors (N=714,054).
| Variable | Outcome: BMI (kg/m2) Model I β (95% CI) | Outcome: obese, BMI≥30 Model II OR (95% CI) |
|---|---|---|
| Individual predictors | ||
| Age (years) | 0.32 (0.31–0.33)*** | 1.12 (1.11–1.12)*** |
| Female | −1.03 (−1.10 to −0.96)*** | 0.92 (0.89–0.94)*** |
| Race/ethnicity (Ref: White) | ||
| Black | 1.93 (1.82–2.04)*** | 1.83 (1.75–1.93)*** |
| Hispanic | 0.75 (0.57–0.93)*** | 1.22 (1.14–1.30)*** |
| Other | −0.72 (−0.91 to −0.53)*** | 0.74 (0.68–0.81)*** |
| Education (Ref: < HS diploma) | ||
| HS graduate, no college | −0.24 (−0.34 to −0.15)*** | 0.90 (0.85–0.95)*** |
| Some college+ | −0.84 (−0.93 to −0.74)*** | 0.71 (0.68–0.75)*** |
| Income (Ref: Quartile 1) | ||
| Quartile 2 | −0.12 (−0.19 to −0.04)** | 0.95 (0.92–0.98)** |
| Quartile 3 | −0.29 (−0.37 to −0.21)*** | 0.87 (0.85–0.90)*** |
| Quartile 4 | −0.77 (−0.87 to −0.68)*** | 0.72 (0.69–0.75)*** |
| Smoking (Ref: never smoked) | ||
| Current smoker | −0.71 (−0.80 to −0.61)*** | 0.77 (0.74–0.81)*** |
| Former smoker | 0.39 (0.34–0.44)*** | 1.13 (1.11–1.17)*** |
| County-level predictors | ||
| Population size (log) | −0.18 (−0.25 to −0.10)*** | 0.93 (0.91–0.96)*** |
| Median household income | −0.13 (−0.20 to −0.05)** | 0.95 (0.92–0.98)** |
| % HS diploma+ | −0.14 (−0.23 to −0.05)** | 0.96 (0.93–0.99)** |
| Region (Ref: South) | ||
| Northeast | 0.05 (−0.10–0.20) | 1.00 (0.94–1.07) |
| Midwest | 0.45 (0.34–0.57)*** | 1.17 (1.12–1.22)*** |
| West | −0.09 (−0.28–0.11) | 0.96 (0.90–1.03) |
| Intercept | 27.06 (27.00–27.12)*** | 0.31 (0.30–0.31)*** |
| Intercept variance component | 0.18*** | 0.02*** |
p<0.05;
p<0.01;
p<0.001
Note: Model I is a linear model predicting BMI as a continuous measure. Model II is a logistic model predicting the odds of being obese (BMI≥30). All county-level variables are measured continuously and scaled by the value of their inter-quartile range. For the county-level variables, β indicates the predicted change in BMI, kg/m2, (Model I) and the odds ratio for obesity (Model II) between the 25th and 75th percentile of the indicated county-level variable. All models control for BRFSS sample year and a squared-term for age.
Table 4 presents results for the restaurant variables. In Models I and IV, the independent effect of total restaurant density (fast food + full service) is examined. These models show that a higher total restaurant density is significantly associated with lower weight status. Next, restaurants are split into components: fast food and full service (Models II and V). Like total restaurant density, a higher full-service restaurant density is significantly associated with lower weight status. In contrast, a higher fast-food density is associated with higher weight status. Finally, the restaurant mix is examined (Models III and VI) with the fast/full ratio measure. The BMI difference between the 25th and 75th percentiles of the fast/full ratio distribution is 0.20 kg/m2 (Model III). The difference between the 5th and 95th percentiles of the fast/full ratio distribution is 0.50 kg/m2 (not shown in table). Results from the logistic regression model (Model VI) indicate an 8% increase in the odds of being obese between the 25th and 75th percentiles of the fast/full ratio distribution and a 21% increase between the 5th and 95th percentile of the distribution. These effects are independent of the total restaurant density, which is controlled for in Models III and VI. In preliminary analysis, it was found that total restaurant density negatively correlated with the fast/full ratio (rho= −0.45), indicating that counties that have a high density of total restaurants also tend to have a relatively low number of fast-food restaurants as compared to the number of full-service restaurants. Given that total restaurant density has an independent effect on weight status, it is important to control for this variable when examining the relationship between the restaurant mix and weight status. The predicted increase in BMI of 0.20 kg/m2 (Model III) for the fast/full ratio variable across its inter-quartile range is comparable in magnitude to the effect of individual income across its inter-quartile range and is approximately one quarter of the predicted difference between those who have a college education versus those who did not complete high school. Multilevel studies on weight status show that individual-level factors are generally stronger predictors of health measures compared with contextual factors31 and the overall results shown here are consistent with prior findings.
Table 4.
Predicted difference in weight status between the 25th and 75th percentiles of the contextual restaurant environment (N=714,054)
| Outcome: BMI (kg/m2), β (95% CI)
|
Outcome: obese, BMI≥30, OR (95% CI)
|
|||||
|---|---|---|---|---|---|---|
| Variable | Model I | Model II | Model III | Model IV | Model V | Model VI |
| Total | −0.22*** (−0.30 to −0.14) | – | −0.15*** (−0.23 to −0.07) | 0.94*** (0.91 to 0.96) | – | 0.96** (0.93–0.99) |
| Fast food | – | 0.09* (0.02–0.16) | – | – | 1.05** (1.02–1.08) | – |
| Full service | – | −0.32*** (−0.40 to −0.24) | – | – | 0.89*** (0.87–0.92) | – |
| Ratio (fast/full) | – | – | 0.20*** (0.12, 0.27) | – | 1.08*** (1.05–1.11) | |
| Intercept | 27.05*** (26.99–27.10) | 27.07*** (27.02–27.12) | 27.07*** (27.02–27.12) | 0.30*** (0.30–0.31) | 0.30*** (0.30–0.31) | 0.31*** (0.30–0.31) |
| Intercept variance component | 0.14*** | 0.14*** | 0.14*** | 0.02*** | 0.02*** | 0.02*** |
p<0.05;
p<0.01;
p<0.001
Note: Models I–III show change in BMI (kg/m2) between the 25th and 75th percentile of the indicated contextual restaurant variable. Models IV–VI show the odds ratio of being obese between the 25th and 75th percentile of the indicated contextual restaurant variable. All models control for variables presented in Table 3.
Sensitivity Analyses
The results were checked using an alternative measure of restaurant density, namely per capita sales (dollars per 10,000 population). This specification did not alter the primary conclusions. Results also were checked for sensitivity to a broad set of county-level variables that might act as confounders. These included population density, the percent of adults in poverty, the percent adults employed, and the percent of black residents. Restaurant coefficients were not substantially affected in these models. Given the number of cases with missing income data, high and low incomes were alternately assigned to missing values (in separate models) to ensure that the patterning of missing information did not affect the conclusions. These models produced results consistent with those presented above. Regular moderate or vigorous physical activity might confound the relationship between restaurant availability and weight status. The BRFSS did not consistently collect this information for every state during the 2002–2006 surveys. Regressions limited to available data were conducted with adjustments for physical activity. These models produced coefficients and significance levels for the restaurant variables that were nearly identical to those in Table 4. Nearly identical results were found when combing 1997 Economic Census data with 1997–2001 BRFSS data suggesting that these results have been stable over a 10-year period.
Discussion
The results reported here demonstrate that the restaurant environment is associated with weight status net of individual- and county-level factors. The relationship is complex, suggesting that the restaurant environment’s influence goes well beyond a simple positive association between restaurant density and weight status. Rather, different components of the restaurant environment exhibit differential associations with weight status. Individuals residing in areas with a high density of total and full-service restaurants exhibit lower weight status, possibly indicating that these areas possess a more advantageous eating environment. Prior studies have not modeled the possible interdependence among different components of the eating environment and a contribution of this study is that area-level restaurant mix is an important determinant of weight status. Those who reside in areas possessing a higher relative number of fast-food to full-service restaurants have a higher weight status. Hence, the relative availability of alternative types of away-from-home eating establishments may most accurately capture the set of food choices available to individuals and may be salient in determining eating behaviors and ultimately weight status.
Results from this study support the notion that fast-food restaurants are a contributor to obesogenic environments. This study goes beyond prior work in this area by showing that a high relative number of fast-food restaurants are also positively associated with weight status. This suggests that in a culture where eating out is common, the type of restaurant food chosen is important to determining weight status. More patronage of full-service restaurants may be suggestive of less consumption of fast food, which may be serving meals that promote the highest weight gain. A higher density of full-service restaurants is independently associated with lower weight status, further suggesting that full-service restaurants are reflective of a more advantageous eating environment. These results highlight the need for further research into the comparative healthfulness of foods served at fast-food and full-service restaurants. One study found that individuals seeking healthier foods are more likely to eat at full-service restaurants over fast-food restaurants.32 It is unclear whether individuals actually consume fewer calories (and more nutritious food) when eating at full-service restaurants. A study that has compared the nutritional content of food from fast-food and full-service restaurants found that both types of restaurant meals contained similar amounts of total fat, but full-service foods had lower amounts of saturated fats and higher amounts of cholesterol and sodium.15 It did not compare carbohydrate and trans-fat composition or the average calories consumed per meal. Frequent fast-food consumption is associated with higher weight status.12,14,16,34 Less work has been conducted on actual full-service restaurant food consumption and weight status. One study25 reported no significant association between full-service patronage and weight status and another reported a positive association only in men.12
In contrast to this study, Chou et al.6 reported that both fast-food and full-service restaurant availability were positively associated with weight status. This discrepancy in results may have arisen from the different levels of aggregation and, as discussed above, a smaller unit may be more suitable for assessing the restaurant environment. Additionally, Chou et al. used data between 1984 and 1999, while restaurants in this study are measured in 2002. Eating behaviors and the restaurant landscape have been changing rapidly over this period and the relationship between restaurant availability and weight status may have shifted. Maddock et al.23 also reported a positive and significant association between fast-food density and weight status, but their analysis was ecologic while this study accounted for individual-level confounders in a multilevel framework.
This study has limitations. Data on supermarkets and grocery stores were not measured. The Economic Census does not differentiate between large supermarkets and smaller grocery stores, which may be more prevalent in impoverished communities.27,35 The quality of foods and prices offered across these types of stores differs,36–38 and it is not possible to capture these elements with per-capita number or per-capita sales measures. The total restaurant density has a negative relationship to weight status, controlling for the relative number of fast-food to full-service restaurants, which cannot be completely explained, and requires further study. Perhaps the prevalence of restaurants correlates with unobserved social attributes of communities (e.g., social capital and crime) that are themselves associated with weight status.11 Nonetheless, the results are robust to confounding by a wide set of structural factors associated with the socioeconomic and racial makeup of counties and these factors will partly account for unobserved social characteristics and the distribution of supermarkets/grocery stores. Height and weight are self-reported. There is continued debate as to the validity of self-reported weight status,39,40 but many have shown self-reports to be an excellent measure pointing to the high correlation between self-reported and clinically measured values.41–43
A challenge in measuring the relationship between restaurant availability and weight status is accounting for the possibility that latent eating and weight-status preferences of individuals determine the distribution of restaurant availability (a reverse causal process). Ideally, such preferences could be addressed with longitudinal data. For example, combining individual and contextual longitudinal data would make it possible to model the change in weight status and the change in restaurant density over time and to treat underlying eating and weight status preferences as unmeasured fixed-effect characteristics that cancel out of the regression equation. Future research delineating the causal processes associated with restaurant availability and weight status would benefit from these type of data.
In conclusion, this study found that the restaurant environment was independently associated with weight status, including individual-level demographic and behavioral characteristics and county-level structural factors. In particular, the types of restaurants that are available may function as a highly salient determinant for weight outcomes. While a higher mix of fast-food to full-service restaurants may contribute to an obesogenic environment, the availability of full-service restaurants may contribute to a more healthful eating environment. Future studies should consider the restaurant mix as a pathway through which more general area–level factors can affect weight status differences. Future studies should also consider how actual eating behaviors are shaped by the availability of different types of restaurants.
Acknowledgments
The authors thank Irma Elo, PhD, for her guidance and suggestions with respect to the analyses. Neil Mehta is supported by a T32 predoctoral Institutional Training Grant from the National Institutes of Health (AG000177; PI: Dr. Beth Soldo). Dr. Chang is supported in part by grant K12HD043459 from the National Institutes of Health.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cummins S, Macintyre S. Food environments and obesity: neighbourhood or nation? Int J Epidemiol. 2006;35:100–4. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 2.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–80. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–35. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 4.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–5. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 6.Chou SY, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23:565–87. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Lopez R. Urban sprawl and risk for being overweight or obese. Am J Public Health. 2004;94:1574–9. doi: 10.2105/ajph.94.9.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poortinga W. Perceptions of the environment, physical activity, and obesity. Soc Sci Med. 2006;63:2835–46. doi: 10.1016/j.socscimed.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Chang VW, Christakis NA. Income inequality and weight status in US metropolitan areas. Soc Sci Med. 2005;61:83–96. doi: 10.1016/j.socscimed.2004.11.036. [DOI] [PubMed] [Google Scholar]
- 10.Chang VW. Racial residential segregation and weight status among US adults. Soc Sci Med. 2006;63:1289–303. doi: 10.1016/j.socscimed.2006.03.049. [DOI] [PubMed] [Google Scholar]
- 11.Cohen DA, Finch BK, Bower A, et al. Collective efficacy and obesity: the potential influence of social factors on health. Soc Sci Med. 2006;62:769–78. doi: 10.1016/j.socscimed.2005.06.033. [DOI] [PubMed] [Google Scholar]
- 12.Binkley JK, Eales J, Jekanowski M. The relation between dietary change and rising U.S. obesity. Int J Obes. 2000;24:1032. doi: 10.1038/sj.ijo.0801356. [DOI] [PubMed] [Google Scholar]
- 13.Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med. 2004;38:243–9. doi: 10.1016/j.ypmed.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 15.Lin BH, Frazão E, Guthrie J. Away-from-home food increasingly important to quality of American diet. Agricultural Information Bulletin. 1999;749 Available online at: http://www.ers.usda.gov/Publications/AIB749/
- 16.Bowman SA, Vinyard BT. Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23:163–8. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 17.United States Department of Health and Human Services (USDHHS) Statement by Julie L. Gerberding on the Centers for Disease Control and Prevention’s Role in promoting healthy lifestyles before the Senate Committee on Appropriations, Subcommittee on Labor, HHS, Education and Related Agencies. Available online at: http://www.hhs.gov/asl/testify/t030217.html.
- 18.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among U.S. adults, 1999–2000. JAMA. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 19.United States Department of Agriculture (USDA) Economic Research Service. Food Consumer Price Index, Prices and Expenditures: Food Expenditure Tables (Tables 7 and 17) Available online at: http://www.ers.usda.gov/Briefing/CPIFoodAndExpenditures/data.
- 20.Boardman JD, Saint Onge JM, Rogers RG, et al. Race differentials in obesity: the impact of place. J Health Soc Behav. 2005;46:229–43. doi: 10.1177/002214650504600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford ES, Mokdad AH, Giles WH, et al. Geographic variation in the prevalence of obesity, diabetes, and obesity-related behaviors. Obes Res. 2005;13:118–22. doi: 10.1038/oby.2005.15. [DOI] [PubMed] [Google Scholar]
- 22.Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the U.S. Soc Sci Med. 2004;59:2421–34. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 23.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19:137–43. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 24.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004;38:57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 25.Jeffery RW, Baxter J, McGuire M, et al. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simmons D, McKenzie A, Eaton S, et al. Choice and availability of takeaway and restaurant food is not related to the prevalence of adult obesity in rural communities in Australia. Int J Obes. 2005;29:703–10. doi: 10.1038/sj.ijo.0802941. [DOI] [PubMed] [Google Scholar]
- 27.Morland K, Wing S, Diez Roux A, et al. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–9. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 28.Reidpath DD, Burns C, Garrard J, et al. An ecological study of the relationship between social and environmental determinants of obesity. Health Place. 2002;8:141–5. doi: 10.1016/s1353-8292(01)00028-4. [DOI] [PubMed] [Google Scholar]
- 29.Cummins SC, McKay L, MacIntyre S. McDonald’s restaurants and neighborhood deprivation in Scotland and England. Am J Prev Med. 2005;29:308–10. doi: 10.1016/j.amepre.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 30.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119:1059–68. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 31.Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489. [Google Scholar]
- 32.Stewart H, Blisard N, Dean J. Let’s eat out: Americans weigh taste, convenience, and nutrition. Economic Information Bulletin. 2006;19 Available online at: http://www.ers.usda.gov/Publications/EIB19/
- 33.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. 1998;46:97–117. doi: 10.1016/s0277-9536(97)00148-2. [DOI] [PubMed] [Google Scholar]
- 34.French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention study: dietary, behavioral and demographic correlates. Int J Obes Relat Metab Disord. 2000;24:1353–9. doi: 10.1038/sj.ijo.0801429. [DOI] [PubMed] [Google Scholar]
- 35.Zenk SN, Schulz AJ, Israel BA, et al. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95:660–7. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baker EA, Kelly C, Barnidge E, et al. The Garden of Eden: acknowledging the impact of race and class in efforts to decrease obesity rates. Am J Public Health. 2006;96:1170–4. doi: 10.2105/AJPH.2004.049502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sloane DC, Diamant AL, Lewis LB, et al. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med. 2003;18:568–75. doi: 10.1046/j.1525-1497.2003.21022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chung C, Myers SL. Do the poor pay more for food? An analysis of grocery store availability and food price disparities. J Consum Aff. 1999;33:276. [Google Scholar]
- 39.Ezzati M, Martin H, Skjold S, et al. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99:250–7. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yun S, Zhu BP, Black W, et al. A comparison of national estimates of obesity prevalence from the behavioral risk factor surveillance system and the National Health and Nutrition Examination Survey. Int J Obes. 2006;30:164–70. doi: 10.1038/sj.ijo.0803125. [DOI] [PubMed] [Google Scholar]
- 41.Weaver TW, Kushi LH, McGovern PG, et al. Validation study of self-reported measures of fat distribution. Int J Obes Relat Metab Disord. 1996;20:644–50. [PubMed] [Google Scholar]
- 42.Jeffery RW. Bias in reported body weight as a function of education, occupation, health and weight concern. Addict Behav. 1996;21:217–22. doi: 10.1016/0306-4603(95)00050-x. [DOI] [PubMed] [Google Scholar]
- 43.Stewart AL. The reliability and validity of self-reported weight and height. J Chronic Dis. 1982;35:295–309. doi: 10.1016/0021-9681(82)90085-6. [DOI] [PubMed] [Google Scholar]


