Abstract
Background
Previous studies demonstrated a modest association between C-Reactive Protein (CRP), stenosis of carotid artery, and carotid Intima-Media Thickness (IMT) in general population. During present study, we aimed to evaluate the relationship between High Sensitivity C-Reactive Protein (hsCRP) and Common Carotid Intima-Media Thickness (CCIMT) in patients who candidate for Coronary Artery Bypass Grafting (CABG).
Methods
The study subjects were enrolled from patients with coronary arteries disease referred from Shahid Madani Hospital (Tabriz, Iran), who have been candidate for elective CABG from January 2005 to August 2007. The common carotid arteries were evaluated with high-resolution B-mode ultrasonography using a 7.5- MHz linear-array transducer to determine the IMT and grade of stenosis. Serum hsCRP level was measured using commercially available enzyme linked immunosorbent assay kit.
Results
Finally, information of 176 CABG candidates was analysed. The mean age of participants was 62.71 ± 9.45 years with 1.63 male to female ratio. The mean of CCIMT was 0.69 ± 0.54 mm. Although there was no significant correlation between serum hsCRP level and CCIMT in patients without carotid stenosis (p=0.113, r=0.186), participants with common carotid artery stenosis had higher levels of serum hsCRP than participants without stenosis (2.42+/-1.30 vs. 1.20+/-0.97 mg/dl; p=0.009).
Conclusion
Study results showed that there was no correlation between serum hsCRP level and CCIMT in patients without carotid stenosis, but patients with common carotid artery stenosis had higher levels of serum hsCRP than patients without stenosis.
Background
Assessment of carotid arteries stenosis and Intima-Media Thickness (IMT) by high resolution B-mode ultrasonography have been shown correlated with prevalence of cardiovascular disease, myocardial infarction, and stroke [1-3]. Some previous studies reported higher risk of myocardial infarction and stroke for patients who had higher levels of carotid arteries IMT [3,4]. In addition to these reports, results of other investigators demonstrated a modest association between C-Reactive Protein (CRP) and carotid artery stenosis and IMT [1,5,6]. As we know from previous studies, atherosclerosis considered to reflect chronic inflammation in arterial walls [7,8]. Patients cancidate for Coronary Artery Bypass Grafting (CABG) have higher level of atherosclerosis, so we aimed to determine the Common Carotid Intima-Media Thickness (CCIMT), High Sensitivity C-Reactive Protein (hsCRP) level, and their relationship in CABG candidates.
Methods
Study population
The study subjects were enrolled from consecutive patients of the Shahid Madani Hospital (Tabriz, Iran), who have been candidate for elective CABG from January 2005 to August 2007. In our referral center, all of CABG candidates underwent carotid and femoral arteries Doppler study, preoperatively.
Patients who had carotid endartrectomy, collagen-vascular diseases, diabetes, infection diseases history during recent month, inflammatory gastroenterology diseases, multiple sclerosis, liver diseases, end stage renal disease and previous stroke were excluded. The base-line examination included a medical history and laboratory testing.
Ethical consideration
The study was performed according to the guidelines of Helsinki declarartion and approved by the Tabriz University of Medical Sciences Ethics Committee. All participants gave informed consent before including to the study.
Carotid ultrasonographic evaluation
The common carotid arteries were evaluated with high-resolution B-mode ultrasonography using a 7.5- MHz linear-array transducer (Hitachi model EUB-525; Hitachi Medical Corp., Tokyo, Japan) to determine the IMT, site of plaques, and stenosis grade. Participants were examined in a supine position, with the head in the axis of the body slightly tilted to the either side. The IMT was measured in common carotid artery at sites 1.0 and 3.0 cm proximal from the beginning of carotid bulb and at the bottom of the bulb. The IMT was defined as the distance between two parallel echogenic lines corresponding to the blood-intima and media-adventitia interfaces. The average value of the 3 points was calculated for each side and the largest value (maximum IMT) was used for analysis.
The common carotid arteries were scanned cross-sectionally and longitudinally. All ultrasound measurements were recorded in end diastole and were measured by the investigator blinded to patients' clinical state. Plaque was defined as a regional intimal thickening, more than 1.2 mm in IMT height. In patients with plaque, carotid artery stenosis was graded using the peak systolic velocity measured after the plaque site according to the Society of Radiologists in Ultrasound Consensus Criteria [9].
Serum hsCRP assay
At baseline examination, a blood sample from every participant was drawn and centrifuged at 1500 rpm for 5 minutes, and then the serum samples were stored at -70°C. All of samples were thawed together, and hsCRP was determined using commercially available enzyme linked immunosorbent assay kit (Monobind, Inc., Lake Forest, CA, USA; Lot Num: EIA-31K2A1).
Statistical methods
Data analysis was performed using the SPSS package version 13 (Chicago, IL, USA). Continuous variables were compared between groups using parametric independent sample t-test, and oneway-ANOVA, or nonparametric Man-Whitney U test, and Kruskal walls. X2 test also was used to analysis significant difference of categorized data. Pearson correlation and multiple regression were applied to evaluate the relationship of hsCRP level with CCIMT in patients without stenosis. A value of p < 0.05 was considered significant.
Results
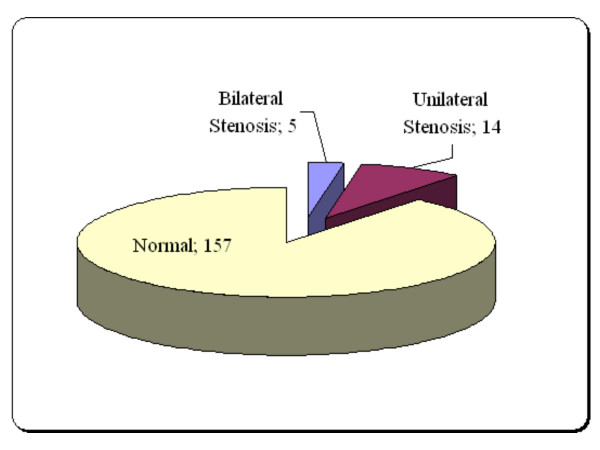
Finally, information of 176 CABG candidates was analysed. Demographic charcterstics of participants were listed in Table 1. Frequency of various grades of common carotid stenosis was shown in Table 2 based on right and left sides. Figure 1 demonstrated frequency of common carotid artery stenosis in study population. The mean of CCIMT was 0.69 ± 0.54 mm.
Table 1.
Demographic characteristics of participants.
| Variable | Value | |
| Age (years) | 62.71 ± 9.45 | |
| BMI (Kg/m2) | 28.31 ± 3.74 | |
| Gender | Male | 109 (61.93%) |
| Female | 67 (38.07%) | |
| Male/female ratio | 1.63 | |
| Smoking history | Male | 58 (54.12%) |
| Female | 6(8.95%) | |
| Smoking (Current/Former) | Male | 13(11.92%)/45(42.19%) |
| Female | 0(0.0%)/6(8.95%) | |
| Systolic blood pressure (mm Hg) | 148.32 ± 24.43 | |
| Diastolic blood pressure (mm Hg) | 91.54 ± 18.26 | |
| Anti-hypertensive therapy | 70.45% | |
| Lipid-lowering agent intake | 46.02% |
Table 2.
Categorization of patients according to the stenosis grade of Common Carotid Artery (CCA).
| Grade of stenosis | |||||
| Normal | < 50% | 50–69% | 70%-near to occlusion | Occlusion | |
| Right CCA | 166 | 7 | 2 | 1 | - |
| Left CCA | 162 | 10 | 2 | 2 | - |
Figure 1.
Frequency of common carotid artery stenosis in study population.
Although there was no significant correlation between serum hsCRP level and CCIMT (p = 0.113, r = 0.186), participants with stenosis had higher levels of serum hsCRP than participants without stenosis in common carotid artery (2.42 ± 1.30 vs. 1.20 ± 0.97 mg/dl; p = 0.009).
In comparison of serum hsCRP levels among the various stenosis grades of common carotid artery, there were no significant difference between patients with < 50% stenosis, 50–60% stenosis, and 70-to near occlusion (p > 0.05; Table 3).
Table 3.
hsCRP by stenosis grades.
| Stenosis grades of common carotid artery | ||||
| Normal | < 50% | 50–69% | 70% to near occlusion | |
| Serum hsCRP (mg/dl) | 1.21 ± 0.97 | 2.18 ± 1.22 | 2.49 ± 1.25 | 2.27 ± 1.42 |
There was a direct linear correlation between age and CCIMT (p = 0.016, r = 0.239) in participants whitout stenosis.
Discussion
This study examined the association of hsCRP with CCIMT. Study results showed that there was no correlation between hsCRP and CCIMT in CABG candidates with subclinical atherosclerosis. Despite this fact, patients with common carotid artery stenosis had higher levels of hsCRP than patients without stenosis. During present study, we strove to control conventional cardiovascular risk factors and diseases which may be affected hsCRP level. Furthermore, this study showed a lower incidence of severe carotid stenosis in Iranian population who candidate for CABG; like previous report of Tarzamni et al. for Iranian [10], and in contrast to the previous studies for other populations [11-14].
Several epidemiological studies have shown a link between serum hsCRP level and subsequent cardiovascular disease in general population [15-19]. In respect to the carotid atherosclerosis, an association between CRP levels and the presence of carotid plagues has been demonstrated by univariate analysis in a prospective studies conducted in general community, or in healthy middle aged women with a smoking history [20-22]. However, this relationship between IMT and CRP level appeared to be largely dependant on age or the presence of other cardiovascular risk factors. In contrast to the previous studies finding, other studies which carried out under controlled criteria failed to show a relation between CRP and carotid IMT and plaque formation [23,24].
To the best of our knowledge, this study is the first one that evaluated relationship of hsCRP and CCIMT among the CABG candidates. Study findings, in contrary with some previous reports [6,25], demonstrated that elevated level of hsCRP was not associated with increased IMT. While patients with carotid artery stenosis had higher level of serum hsCRP, there was not statistcally significant difference between various grades of stenosis. As we know, patients who candidate for CABG have higher grades of atherosclerosis in coronary arteries. Today, atherosclerosis consider as a chronic inflammatory process [7,8], and innate and adaptive immune responses participate in several phases of atherosclerosis [26]. CRP is a component of innate immunity that is actively participates in inflammatory process. Recent evidences have suggested a possible direct pathogenic role for CRP in atherosclerosis process and plaque formation [27-29] and increasing of CRP level promote arterial atherosclerosis. Alternatively, it may merely be an epiphenomena and an indicator of systemic inflammation which itself is associated with atherosclerosis.
Furthermore, some of conventional cardiovascular risk factors such as smoking, obesity may act to increase atherosclerosis partly through increasing systemic inflammation. The systemic inflammatory response is also increased in smokers according to the pack pear year of smoking [23]. This may be related to both of bacterial endotoxin and the increased risk of respiratory tract infection seen in smokers [30]. Therefore, elevated CRP may merely reflect an exaggerated inflammatory response associated with these conventional cardiovascular risk factors [31,32].
As well-known ligand of phosphorylcholine residues, CRP binds avidly to oxidized low-density lipoproteins and may induce foam cell formation in atherosclerosis [33,34]. In this case and by considering the patients with carotid artery stenosis had higher serum hsCRP levels, the CRP effect might be confirmed clinically by study results.
Despite these findings, one of our study limitations was limited population. So, we struggled to use proper statistical tests to analysis data and appropriate inclusion and exclusion criteria to control any factors may address any bias.
Conclusion
In conclusion, our study results showed that there was no correlation between serum hsCRP level and intima-media thickness of common carotid in patients without stenosis, but patients with common carotid artery stenosis had higher levels of serum hsCRP than patients without stenosis.
Abbreviations
IMT: Intima-Media Thickness; CRP: C-Reactive Protein, hsCRP: High-Sensitivity C-Reactive Protein; CABG: Coronary Artery Bypass Grafting; CCIMT: Common Carotid Intima-Media Thickness
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
PS designed study and performed Doppler ultrasonographic evaluation.
NN followed up the patients, performed data analysis, drafted and revised the manuscript
MKT conceived the paper, and carried out the Doppler ultrasound
RJR participated in coordination and enrolment of patients to the study
All authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
We are most grateful to the patients participating in this study. Written informed consent was also obtained for publication from the patients and/or their relatives.
Contributor Information
Parvin Shakouri, Email: Shakouriparvin@hotmail.com.
Nariman Nezami, Email: Dr.Nezami@gmail.com.
Mohammad Kazem Tarzamni, Email: Tarzamni@yahoo.com.
Reza Javad Rashid, Email: RJRashid@hotmail.com.
References
- Burke GL, Evans GW, Riley WA, Sharrett AR, Howard G, Barnes RW, Rosamond W, Crow RS, Rautaharju PM, Heiss G. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) study. Stroke. 1995:386–391. doi: 10.1161/01.str.26.3.386. [DOI] [PubMed] [Google Scholar]
- O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- Schillinger M, Exner M, Mlekusch W, Sabeti S, Amighi J, Nikowitsch R, Timmel E, Kickinger B, Minar C, Pones M. Inflammation and Carotid Artery–Risk for Atherosclerosis Study (ICARAS) Circulation. 2005:2203–2209. doi: 10.1161/01.CIR.0000163569.97918.C0. [DOI] [PubMed] [Google Scholar]
- Jarvisalo MJ, Harmoinen A, Hakanen M, Paakkunainen U, Viikari J, Hartiala J, Lehtimaki T, Simell O, Raitakari OT. Elevated serum C-reactive protein levels and early arterial changes in healthy children. Arterioscler Thromb Vasc Biol. 2002:1323–1328. doi: 10.1161/01.ATV.0000024222.06463.21. [DOI] [PubMed] [Google Scholar]
- Wang TJ, Nam BH, Wilson PW, Wolf PA, Levy D, Polak JF, D'Agostino RB, O'Donnell CJ. Association of C-reactive protein with carotid atherosclerosis in men and women: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2002:1662–1667. doi: 10.1161/01.ATV.0000034543.78801.69. [DOI] [PubMed] [Google Scholar]
- Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- Libby P. Molecular bases of the acute coronary syndromes. Circulation. 1995:2844–2850. doi: 10.1161/01.cir.91.11.2844. [DOI] [PubMed] [Google Scholar]
- Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI. Carotid artery stenosis: gray-scale and Doppler US diagnosis – Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003:340–346. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- Tarzamni MK, Afrasyabi A, Farhoodi M, Karimi F, Farhang S. Low prevalence of significant carotid artery disease in Iranian patients undergoing elective coronary artery bypass. Cardiovasc Ultrasound. 2007:1–5. doi: 10.1186/1476-7120-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berens ES, Kouchoukos NT, Murphy SF, Waering TH. Preoperative carotid screening in elderly patients undergoing cardiac surgery. J Vasc Surg. 1992:313–321. [PubMed] [Google Scholar]
- Rath PC, Agarwala MK, Dhar PK, Lakshmi C, Ahsan SA, Deb T, Kumar S, NarasimhamR RS, Rao PS, Dixit V. Carotid artery involvement in patients of atherosclerotic coronary artery disease undergoing coronary artery bypass. Indian Heart J. 2001:761–765. [PubMed] [Google Scholar]
- Salasidis GC, Latter DA, Steinmetz OK, Blair JF, Graham AM. Carotid artery duplex scanning in preoperative assessment for coronary artery revascularization : the association between peripheral vascular disease, carotid artery stenosis and stroke. J Vasc Surg. 1995:154–160. doi: 10.1016/S0741-5214(95)70254-7. [DOI] [PubMed] [Google Scholar]
- Gasera B, Angelis I, Weingartnet J, Neurmaier PP, Spiliopoulos K, Kemkes BM. Simultaneous carotid endarterectomy and cardiac surgery – additional risk factor or safety? Thrac Cardiovasc Surg. 2003:22–27. doi: 10.1055/s-2003-37282. [DOI] [PubMed] [Google Scholar]
- Thompson SG, Kienast J, Pyke SD, Haverkate F, Loo JC van de. Hemostatic factors and the risk of myocardial infarction or sudden death in patients with angina pectoris. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. N Engl J Med. 1995:635–641. doi: 10.1056/NEJM199503093321003. [DOI] [PubMed] [Google Scholar]
- Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996:537–547. doi: 10.1093/oxfordjournals.aje.a008963. [DOI] [PubMed] [Google Scholar]
- Tracy RP, Lemaitre RN, Psaty BM, Ives DG, Evans RW, Cushman M, Meilahn EN, Kuller LH. Relationship of C-reactive protein to risk of cardiovascular disease in the elderly. Results from the Cardiovascular Health Study and the Rural Health Promotion Project. Arterioscler Thromb Vasc Biol. 1997:1121–1127. doi: 10.1161/01.atv.17.6.1121. [DOI] [PubMed] [Google Scholar]
- Haverkate F, Thompson SG, Pyke SD, Gallimore JR, Pepys MB. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997:462–466. doi: 10.1016/S0140-6736(96)07591-5. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997:973–979. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- Makita S, Nakamura M, Hiramori K. The association of C-reactive protein levels with carotid intima-media complex thickness and plaque formation in the general population. Stroke. 2005:2138–2142. doi: 10.1161/01.STR.0000181740.74005.ee. [DOI] [PubMed] [Google Scholar]
- Willeit J, Kiechl S, Oberhollenzer F, Rungger G, Egger G, Bonora E, Mitterer M, Muggeo M. Distinct risk profiles of early and advanced atherosclerosis: prospective results from the Bruneck Study. Arterioscler Thromb Vasc Biol. 2000:529–537. doi: 10.1161/01.atv.20.2.529. [DOI] [PubMed] [Google Scholar]
- Hak AE, Stehouwer CD, Bots ML, Polderman KH, Schalkwijk CG, Westendorp IC, Hofman A, Witteman JC. Association of C-reactive protein with measures of obesity, insulin resistance, and subclinical atherosclerosis in healthy, middle-aged women. Arterioscler Thromb Vasc Biol. 1999:1986–1991. doi: 10.1161/01.atv.19.8.1986. [DOI] [PubMed] [Google Scholar]
- Tracy RP, Psaty BM, Macy E, Bovill EG, Cushman M, Cornell ES, Kuller LH. Lifetime smoking exposure affects the association of C-reactive protein with cardiovascular disease risk factors and subclinical disease in healthy elderly subjects. Arterioscler Thromb Vasc Biol. 1997:2167–2176. doi: 10.1161/01.atv.17.10.2167. [DOI] [PubMed] [Google Scholar]
- Lorenz MW, Karbstein P, Markus HS, Sitzer M. High-sensitivity C-reactive protein is not associated with carotid intima-media progression: the carotid atherosclerosis progression study. Stroke. 2007:1774–1779. doi: 10.1161/STROKEAHA.106.476135. [DOI] [PubMed] [Google Scholar]
- Blackburn R, Giral P, Bruckert E, Andre JM, Gonbert S, Bernard M, Chapman MJ, Turpin G. Elevated C-reactive protein constitutes an independent predictor of advanced carotid plaques in dyslipidemic subjects. Arterioscler Thromb Vasc Biol. 2001:1962–1968. doi: 10.1161/hq1201.099433. [DOI] [PubMed] [Google Scholar]
- Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- Clapp BR, Hirschfield GM, Storry C, Gallimore JR, Stidwill RP, Singer M, Deanfield JE, MacAllister RJ, Pepys MB, Vallance P, Hingorani AD. Inflammation and endothelial function: direct vascular effects of human C-reactive protein on nitric oxide bioavailability. Circulation. 2005:1530–1536. doi: 10.1161/01.CIR.0000159336.31613.31. [DOI] [PubMed] [Google Scholar]
- Sabatine MS, Morrow DA, Jablonski KA, Rice MM, Warnica JW, Domanski MJ, Hsia J, Gersh BJ, Rifai N, Ridker PM, Pfeffer MA, Braunwald E. Prognostic significance of the Centers for Disease Control/Am Heart Association high-sensitivity C-reactive protein cut points for cardiovascular and other outcomes in patients with stable coronary artery disease. Circulation. 2007:1528–1536. doi: 10.1161/CIRCULATIONAHA.106.649939. [DOI] [PubMed] [Google Scholar]
- Tsimikas S, Willerson JT, Ridker PM. C-reactive protein and other emerging blood biomarkers to optimize risk stratification of vulnerable patients. J Am Coll Cardiol. 2006:C19–C31. doi: 10.1016/j.jacc.2005.10.066. [DOI] [PubMed] [Google Scholar]
- Hasday JD, Bascom R, Costa JJ, Fitzgerald T, Dubin W. Bacterial endotoxin is an active component of cigarette smoke. Chest. 1999:829–835. doi: 10.1378/chest.115.3.829. [DOI] [PubMed] [Google Scholar]
- Lowe GD, Pepys MB. C-reactive protein and cardiovascular disease: weighing the evidence. Curr Atheroscler Rep. 2006:421–428. doi: 10.1007/s11883-006-0040-x. [DOI] [PubMed] [Google Scholar]
- Pepys MB. CRP or not CRP? That is the question. Arterioscler Thromb Vasc Biol. 2005:1091–1094. doi: 10.1161/01.ATV.0000169644.88847.28. [DOI] [PubMed] [Google Scholar]
- Chang MK, Binder CJ, Torzewski M, Witztum JL. C-reactive protein binds to both oxidized LDL and apoptotic cells through recognition of a common ligand: Phosphorylcholine of oxidized phospholipids. Proc Natl Acad Sci USA. 2002:13043–13048. doi: 10.1073/pnas.192399699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma S, Devaraj S, Jialal I. Is C-reactive protein an innocent bystander or proatherogenic culprit? C-reactive protein promotes atherothrombosis. Circulation. 2006:2135–2150. [PubMed] [Google Scholar]