Abstract
Objective
Irritability is a prominent symptom in the spectrum of female-specific mood disorders, and in some women, irritability is serious enough to disrupt their lives and warrant treatment. The objective of this research was to develop a new, female-specific state measure of irritability.
Methods
We constructed self-rating and observer rating scales using items derived from spontaneous descriptions of irritability by women with mood disturbances related to the menstrual cycle, childbearing or menopause. Following a pretest, the scales were shortened to the core items of irritability (annoyance, anger, tension, hostility, sensitivity to noise and touch) and tested on a new cohort of patients.
Results
The 14-item Self-Rating Scale and the 5-item Observer Rating Scale showed evidence for internal consistency (Self-Rating: n = 36 patients, Cronbach's α = 0.9257, mean interitem correlation = 0.4690; Observer Rating: Cronbach's α = 0.7418, mean interitem correlation = 0.3616), Self-Rating test–retest reliability (n = 29 patients, rs = 0.704, p = 0.01) and interrater reliability (n = 20 patients; τb = 1.000, p = 0.001).
Conclusion
This new, female-specific scale for rating irritability has the potential to further the evaluation of this prominent symptom cluster and increase specificity in clinical assessments of emotional disturbances related to reproductive cyclicity in women.
Medical subject headings: women's health, irritable mood.
Abstract
Objectif
L'irritabilité est un symptôme important dans le spectre des troubles thymiques particuliers aux femmes et, chez certaines, elle est assez sérieuse pour perturber leur vie et justifier un traitement. Cette recherche visait à mettre au point une nouvelle mesure de l'irritabilité spécifique à la femme.
Méthodes
Nous avons construit des échelles d'autoévaluation et d'évaluation par observateur au moyen de questions dérivées de descriptions spontanées de l'irritabilité données par des femmes atteintes de troubles thymiques liés au cycle menstruel, à l'accouchement ou à la ménopause. À la suite d'un prétest, on a raccourci les échelles pour les ramener aux éléments de base de l'irritabilité (agacement, colère, tension, hostilité, sensibilité aux bruits et au toucher) et nous en avons fait l'essai sur une nouvelle cohorte de patientes.
Résultats
L'échelle d'autoévaluation à 14 questions et l'échelle d'évaluation par observateur à 5 questions ont démontré une uniformité interne (autoévaluation : n = 36 patientes, α de Cronbach = 0,9257, corrélation moyenne entre questions = 0,4690; évaluation par observation : α de Cronbach = 0,7418, corrélation moyenne entre questions = 0,3616), rapidité du test-retest d'autoévaluation (n = 29 patientes, rs = 0,704, p = 0,01) et fiabilité entre évaluateurs (n = 20 patientes; τb = 1,000, p = 0,001).
Conclusion
Cette nouvelle échelle d'évaluation de l'irritabilité spécifique à la femme pourrait pousser plus loin l'évaluation de cette grappe de symptômes importants et accroître la spécificité des évaluations cliniques des troubles émotionnels liés au cycle de la reproduction chez la femme.
Introduction
Irritability is defined as a proneness to anger, annoyance or impatience.1 It is characterized by a state of physical and psychological tension that may suddenly and rapidly escalate and may include reduced control over temper, a heightened or excessive sensitivity to external stimuli and irascible verbal or behavioural outbursts — even explosive aggressiveness.2 In the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)3 and in the literature of the past 5 decades, irritability is an associated feature of, or criterion for, other mental conditions.
Clinically, irritability is a prominent symptom in the spectrum of female-specific mood disorders occurring from menarche to menopause, including premenstrual, perinatal and perimenopausal mood disorders.
Premenstrual syndromes
Irritability is a common feature of premenstrual syndrome (PMS)4 and a core symptom of premenstrual dysphoric disorder (PMDD).3 PMDD is notable for the “on again–off again” characteristic of its cardinal symptoms (i.e., irritability, dysphoria, lability of mood and tension). An expert group of clinicians and researchers has reached a consensus that PMDD is a distinct clinical entity and not a form of “masked depression” as was previously thought.5 A recent review of epidemiologic data has shown that up to 75% of women with regular menstrual cycles may experience some symptoms of PMS; between 3% and 8% are diagnosed with PMDD.6
In a cross-national survey on the impact of premenstrual symptomatology on functioning and treatment-seeking behaviour, Hylan and colleagues7 found irritability and anger to be the primary premenstrual mood symptoms in 80% of 1045 subjects from the United States, the United Kingdom and France. Respondents endorsed that PMS-related irritability and functional impairment is greatest at home. In case reports as well, women endorse fatigue and low energy, feeling “wiped out,” a lack of concentration and that small things bother them. In one illuminating example, a woman described her relationship with her family during the premenstruum: “I tend to flare up at my children, ‚bark' at my husband more and tend to ‚run off' at the mouth, being more opinionated. Ordinarily, I am basically a listener and very tolerant when it comes to the antics of my children.”8
Perinatal mood disorders
In prospective ratings of a nonpsychiatric population consisting of 182 pregnant women and 179 nonpregnant control women, O'Hara and colleagues9 have shown that there is some deterioration in women's psychological status across the second and third trimesters of pregnancy. Preliminary evidence suggests that high levels of depressive, anxiety and anger symptoms in pregnancy can have an adverse influence on neonatal physiological, neurobiological and behavioural measures and also on infant development.10,11
Irritability comprises one aspect of the clinical presentation in women with postpartum mood disorders — in particular, with maternity blues, postpartum depression and puerperal psychoses.
While postpartum blues are generally perceived as a period of emotional lability with frequent crying episodes occurring after delivery, one prospective study has shown that ratings of irritability rise from day 2 postpartum, peak about day 8 and remain steady for the next 2 weeks.12 Conversely, ratings of depression, crying, anxiety and mood lability rise during the first 5 days after delivery and then taper in the days thereafter.
In a sample of 230 women, Cox and colleagues13 showed that the patterns of irritability ratings were distinctive and significantly different from the ratings for depression or anxiety at 12 and 23 weeks antepartum and at 1 week and 5 months postpartum. In the subsequent development of the Edinburgh Postnatal Depression Scale (EPDS),14 2 items of irritability were included in the initial version. Following an item factor analysis, the authors of the EPDS reported that irritability formed “a separate ‚non-depression' factor” and hence did not form part of the final scale. This finding was congruent with Snaith's suggestion that irritability may be distinct from depression and anxiety.15
Irritability is also part of the clinical picture of puerperal psychosis, which occurs in about 1 out of 1000 women in the days after parturition. Descriptions of irritability, anger and even “Medusa-like rage” have been recorded in case reports dating back more than 4 centuries.16 In a sample of 50 pregnant and postpartum women referred to a perinatal psychiatry clinic, Mammen and colleagues found that 60% of subjects endorsed “anger attacks” at intake.17 Anger attacks were defined as becoming angry and enraged with other people, in a way that was thought to be excessive or inappropriate to the situation. Irritability is a hallmark feature of anger attacks.17 Mammen and colleagues reported that anger attacks are typically ego-dystonic and associated with a high degree of subjective distress (i.e., guilt, regret, worry).
Perimenopause-related mood disorders
Irritability is the primary mood complaint for up to 70% of women during the perimenopause, a phenomenon that has been observed cross-culturally.18–26 Some women may experience increased frequency and intensity of psychological complaints during this period. In a community-based cohort study of women aged 36–44 years, Harlow and colleagues27 found that about 23% of subjects up to age 41 years scored 16 or more on the Center for Epidemiologic Studies Depression Scale; the percentage climbed to 31.6% in the group aged 42–44 years. The authors subsequently noted that a lifetime history of major depression may be associated with an early decline in ovarian function (i.e., earlier perimenopausal transition).28
Existing measures of irritability
The existing measures of irritability were reviewed in a previous publication.2 The Buss–Durkee Hostility Inventory (BDHI),29 a trait measure of hostility with an Irritability subscale, has had an enormous impact on the measurement of irritability. The items for several of the more recent scales —the Irritability, Depression, Anxiety Scale,15 the Irritability and Emotional Susceptibility Scale30 and the Anger, Irritability, Assault Questionnaire31 — have been adopted without revision from the BDHI, now 50 years old.
Preliminary studies showed several striking findings. First, the terminology used by women to describe irritability notably differed from the phrasing of items in the existing measures, and irritability as a phenomenon is not wholly described. For example, women sometimes reported that, when they were irritable, noises were more bothersome. Further, sex-based differences in spontaneous descriptions were noted, with men using words such as “sore, grouchy, miserable, upset, critical, looking for trouble, power trip, cynical, sarcastic, mad,“ whereas women used words such as “less patience or impatient, intolerant, unsettled, weepy, moody, short, sharp, more emotional, unable to focus.”32
A new state measure of irritability will potentially further the evaluation of a prominent but underrecognized phenomenon and increase specificity in clinical assessments of emotional disturbances related to reproductive cyclicity in women. The aim of this paper is to report on the preliminary reliability and internal consistency data of a new, female-specific rating scale for irritability.
Development and design
The development and evaluation of the new measure occurred at the Women's Health Concerns Clinic (WHCC), a hospital-based outpatient psychiatric facility affiliated with McMaster University that provides clinical services to women who are at risk for, or have had, changes in mood related to the menstrual cycle, the perinatal or the perimenopause periods. Each year, the WHCC, staffed by a multidisciplinary team, screens about 300 new patients who are referred by community family physicians, obstetricians, midwives or public health nurses, or who are self-referred. The Research Ethics Board, St. Joseph's Healthcare Hamilton, approved the study.
We recruited women aged 20–60 years and presenting with emotional disturbances related to the menstrual cycle, childbearing or the time around menopause at their first visit to the WHCC. All subjects were able to read and write in English and to provide informed consent. We excluded patients with acute psychotic illness.
With the aid of flyers, we recruited control subjects from the hospital at large and from the community. As much as possible, the control subjects and patients were matched for the following characteristics: regular menstrual cycles, pregnancy, postpartum and less than 1 year after delivery or in the perimenopausal period (i.e., 45–60 years of age). Potential control subjects were excluded if they had a current medical or psychiatric illness or endorsed use of prescribed or over-the-counter medication. For all subjects, the first author (L.B.) introduced the study and obtained consent.
Item generation
Consenting subjects responded to a series of open-ended questions that elicited keywords and descriptive phrasing of irritability (e.g., “At times when you feel grouchy or irritable, how do you feel?”). Descriptions from 121 subjects (91 patients, 30 control subjects) were analyzed with NUD*IST Nvivo Version 1.1 (QSR International Pty Ltd).
We identified 12 content areas from the spontaneous descriptions. Annoyance, anger, tension, hostile behaviour and sensitivity (e.g., to noise) were most frequently cited as the core aspects of irritability, findings congruent with the historical literature. Depression or dysphoria, vulnerability, frustration, physical symptoms and impairments in self-esteem, social activities and daily activities were most frequently cited as consequences associated with the experience of markedly irritable mood.33
Respondents also rated their agreement with items from existing self-administered scales of irritability on a continuum from 0 (not at all) to 7 (very much so). We used the Wilcoxon Mann–Whitney U test to evaluate the responses and determine which of the items distinguished healthy subjects from WHCC patients. A pool of 36 items, with 3 items in each content area, was generated directly from the spontaneous descriptions (26 items) and from items in existing measures (10 items). Minor revisions were made to the phrasing of several items from the latter (e.g., “I feel like a powder keg ready to explode” was modified to “I feel ready to explode”).
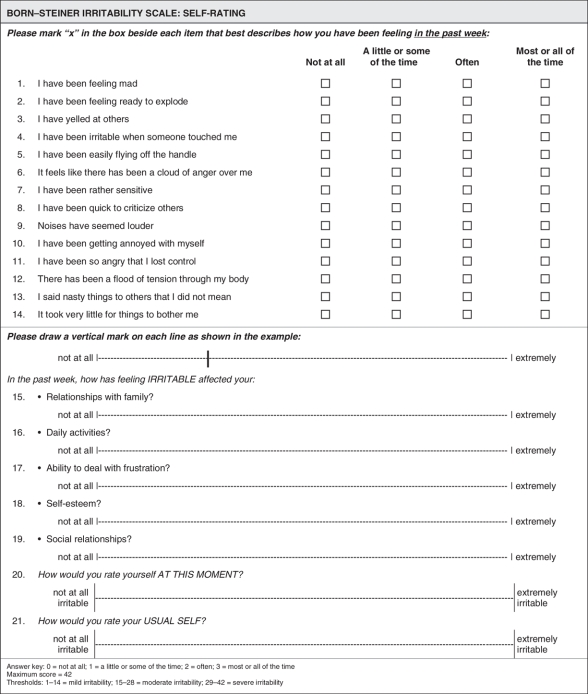
Self-Rating Scale format and administration
For the self-rating measure, we constructed a 36-item summative scale with equally weighted items and Likert response options. In the Likert system, the items are posited as analogous indicators of the phenomenon of irritability and, because the research on irritability is relatively new, are assumed to be equally important in contributing to the total score. Patients marked the box beside each item that best described how they were feeling in the past week. The response options were scored as follows: 0 = not at all, 1 = some of the time, 2 = often, 3 = most of the time.
To record a patient's impression of her irritability severity at presentation (state) and what level of irritability could be considered normal for her (trait), we added two 100-mm visual analog scales at the end of the Self-Rating Scale. The rationale for including visual analog scales is based on discussion of irritability as either a trait characteristic or a transient (state) phenomenon. The patient is given the opportunity to globally evaluate her irritability at that moment as compared with her usual premorbid self, and the clinician gains insight into how severe the patient's irritability is at presentation and how much irritability may be considered normal for the patient. The test–retest reliability and validity of visual analog scales has been established in multiple studies of depression and anxiety.34–36
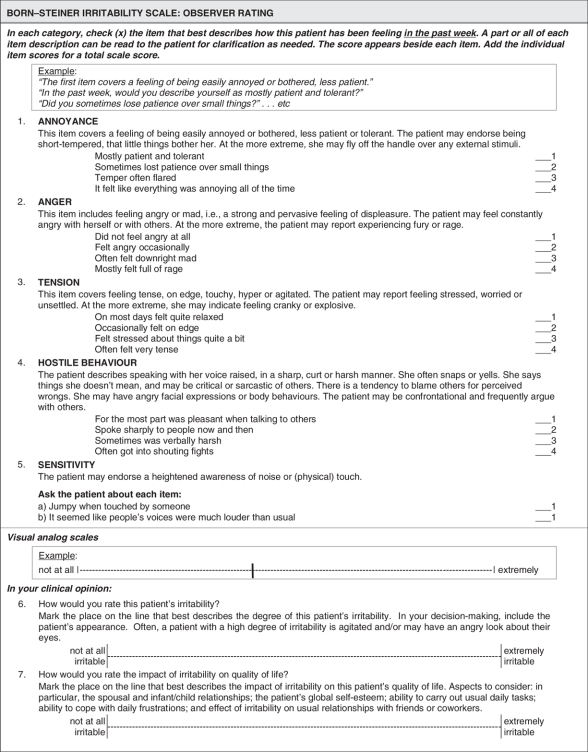
Observer Rating Scale format and administration
We constructed a 12-item, clinician-administered Observer Rating Scale that mirrored the content areas of the Self-Rating Scale. The rationale for developing mirror Self-Rating and Observer Rating Scales rests in part on the psychiatric literature: it is common practice in psychiatry to construct mirror-image instruments. This mirror design offers greater versatility for clinical use. Our aim for the Observer Rating Scale was to easily pinpoint core features of irritability but place little demand on clinicians' time.
The first 5 items covered the core symptoms of irritability (annoyance, anger, tension, hostile behaviour, sensitivity); the remaining 7 items characterized the burden of illness related to irritability (frustration, physical symptoms, symptoms of dysphoria and depression, vulnerability and impairments in self-esteem, social activities and daily activities). To assist the clinician, several descriptive sentences accompanied each item.
Using given prompts, the clinician asked the patient a series of questions about each item and selected the response option that best described how the patient was feeling in the past week; 10 of the 12 items were scored on a 4-point scale, with 0 = none of the time and 3 = most of the time. The items “sensitivity” and “physical symptoms” were each described by 3 symptoms, with each symptom, if present, receiving a score of 1. In addition, clinicians rated the patient's irritability on a 100-mm visual analog scale that included the patient's visual appearance (e.g., a patient with severe irritability may appear agitated or have an angry look about her eyes).
Pretest
Following a pilot test for readability of the content, the Irritability Scales were pretested with a new cohort of WHCC patients and control subjects to determine internal consistency, reliability and optimal scale length. Again, for all subjects, the first author (L.B.) introduced the study and obtained consent.
Control subjects were recruited from the St. Joseph's Healthcare Department of Obstetrics and Gynecology and from the hospital at large, with the aid of flyers. Potential control subjects were administered the Psychological General Well-Being Index.37 We excluded women whose scores classified them as suffering from moderate or severe distress or who were taking prescribed medications for a medical or psychiatric condition. Participating control subjects received a voucher for a muffin and beverage.
The scales were completed at the end of the first clinic visit. A minimum sample of 50 subjects representative of the population of interest is recommended to examine frequencies of endorsement.38 All statistical tests were analyzed with SPSS Version 11.09 (SPSS, Chicago, Ill., 2001).
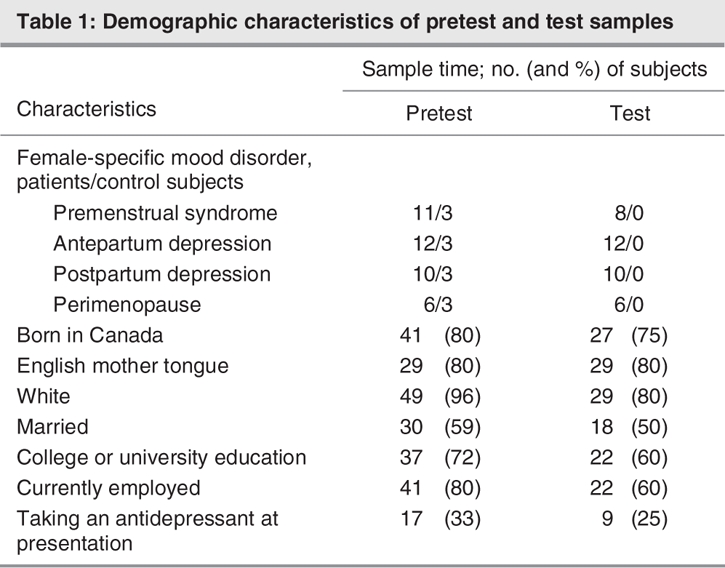
Self-Rating Scale: internal consistency reliability and optimal scale length
We collected data from 39 consenting patients and 12 control subjects at their first clinic visit. Their demographic characteristics are shown in Table 1. The frequencies of endorsement for the 36-item Self-Rating Scale showed a range of responses to each item. The statistical analyses revealed a mean interitem correlation of 0.4928 (minimum = 0.0419, maximum = 0.8635) and Cronbach's α = 0.9717. All items were positively and significantly correlated with each other and with the total scale score at the 0.005 level, with the exception of the item “It is hard for me to sit still.”
Table 1
To shorten the item pool, we used clinical judgment combined with statistical methods and the conceptualization of irritability as a construct in the literature. The WHCC clinicians (a psychiatrist, a social worker and 2 psychiatric nurses) indicated that the selected core items of irritability are accurate and distinct from symptoms of depression, although the psychiatrist noted that patients with generalized anxiety disorder or posttraumatic stress disorder might also endorse some of these items.
The statistical selection of items was based on item–total score correlation; that is, each item was correlated with the scale total omitting that item, any item with Pearson's r less than 0.20 was eliminated, the remaining items were rank-ordered and items were selected starting with the highest correlation (not shown).38 Examination of plots showed that the 5 items representing the core symptoms of irritability (annoyance, anger, tension, hostile behaviour, sensitivity to noise and touch) distinguished the 12 least irritable from the 12 most irritable subjects.
Several items were removed from the pool. Both clinicians and subjects noted that the item about increased body temperature could relate either to pregnancy or to irritability. With regard to dysphoria or depression, patients who were primarily depressed (i.e., feeling low was their foremost complaint) were unable to distinguish between depression and depressive symptoms resulting from being irritable. In the case of vulnerability, clinicians noted considerable overlap between items of vulnerability and frustration.
Visual analog scales are a simple, reliable method for documenting subjective experience, and we replaced the items on the Self-Rating Scale pertaining to the burden of illness with visual analog scales for relationships with family, daily activities, self-esteem, social relationships and ability to deal with frustration.
The Self-Rating Scale was thus shortened to 14 items representing the core aspects of irritability, 5 visual analogue scales representing the burden of illness associated with irritability, and 2 visual analog scales representing “at this moment” (state) and “usual general self” (trait) dimensions of irritability (Fig. 1).
Fig. 1: Born–Steiner Irritability Scale: Self-Rating.
Observer Rating Scale: internal consistency reliability and optimal scale length
The frequencies of endorsement for the 12-item Observer Rating Scale showed a range of responses to each item. The statistical analyses revealed a mean interitem correlation of 0.5364 (minimum = 0.2762, maximum = 0.7522) and Cronbach's α = 0.9315. All items of the Observer Rating Scale were positively and significantly correlated with each other and with the total scale score (p = 0.05).
After reduction of the Self-Rating Scale, the Observer Rating Scale was shortened to 5 items (with item 5 divided into 5a and 5b), representing the core aspects of irritability, and 2 visual analog scales for documenting the clinician's impression of the severity of the patient's irritability and the impact of irritability on the patient's quality of life (Fig. 2).
Fig. 2: Born–Steiner Irritability Scale: Observer Rating
Evaluating the shortened measure
The psychometric properties of the Self-Rating (14 items) and Observer Rating (5 items) Scales were evaluated on a third sample of WHCC patients. The inclusion criteria, recruitment and consent procedures were similar to the pretest; however, in this phase, we limited recruitment to WHCC patients only. To assess interrater reliability with a minimal acceptable reliability of 0.6039 and an expected reliability of about 0.9, an estimated minimum sample size, based on 2 raters per patient, is 12 subjects (α = 0.05, β = 0.20).40
The scales were administered at the beginning of each subject's first scheduled clinic appointment (Time 1). The first author distributed the Self-Rating Scale. The first author and the attending WHCC clinician (a psychiatric nurse, a social worker or a psychiatrist) simultaneously completed the Observer Rating Scale, with the author asking the questions.
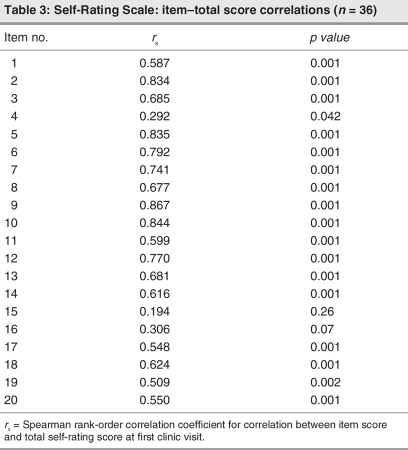
Self-Rating Scale: internal consistency and test–retest reliability
Data were collected from 36 consecutive patients; the characteristics of the sample are shown in Table 1. An item correlation matrix was generated for the 14 items. The item–total score correlations were examined with the Spearman rank order correlation coefficient, with a 1-tailed test of significance. The statistical analyses revealed a mean interitem correlation of 0.4690 (minimum = –0.0195, maximum = 0.8203) and Cronbach's α = 0.9257. Each item showed a range of responses and was significantly correlated with the total scale score (p ≤ 0.05) (Table 2, Table 3).
Table 2
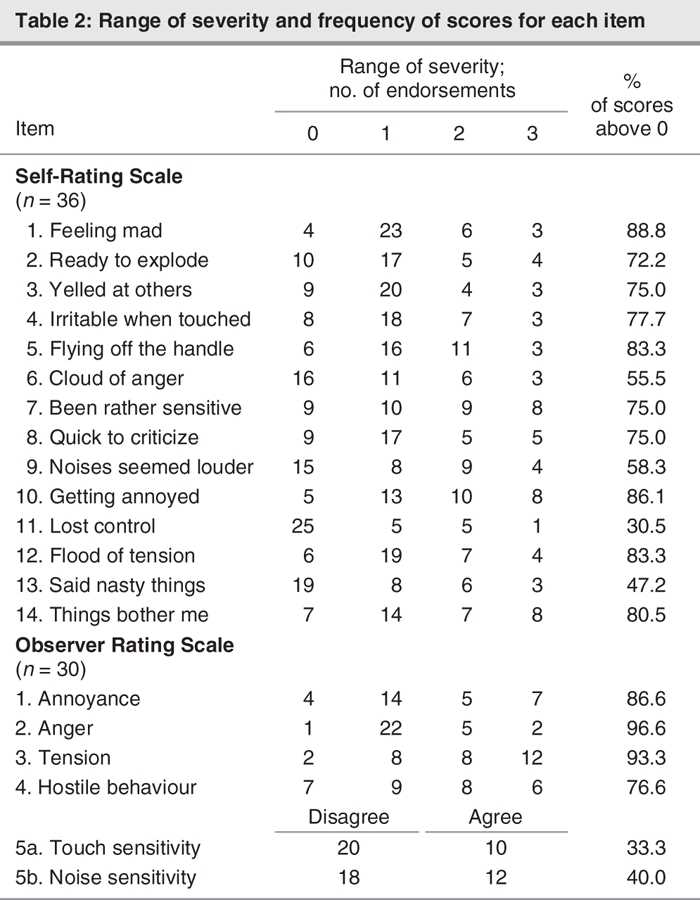
Table 3
The visual analogue scale scores (items 15–20) were also significantly correlated with the Self-Rating total score, although the correlations were not significant for items 15 (relationship with family) and 16 (daily activities). There was a significant correlation for item 20 (patients' visual analog scale score [state]) and the Self-Rating Scale total score (rs = 0.550, p = 0.001).
Subjects completed the Self-Rating Scale again at their second visit (Time 2) to evaluate test–retest reliability. An interval of at least 14 days between testing has been recommended.39 PMS clinic patients were tested in the luteal (symptomatic) phases of their menstrual cycle, 4 weeks apart. Perinatal and perimenopausal patients were retested at least 2 weeks after the first assessment.
The Self-Rating Scale was completed a second time by 33 patients; 3 patients were not seen after their first visit. An additional 4 patients were not included in the analysis because 2 had a notable change in clinical status due to treatment and 2 were seen antepartum and delivered before the retest occasion.
The results for 29 patients showed that the mean interval between scale completions was 21 (standard deviation [SD] 9.0) days, with the shortest interval being 7 days and the longest interval being 42 days. A histogram plot of the difference in scores between Time 1 and Time 2 showed that the assumption of symmetric distribution of scores using the Wilcoxon signed ranks test was met. The results of the Wilcoxon signed ranks test indicated that the median Irritability Scale scores were not significantly different from Time 1 (median score = 16) to Time 2 (median score = 18) (p = 0.18). A significant correlation was detected between the self-ratings at Time 1 and Time 2 (rs = 0.704, p = 0.01).
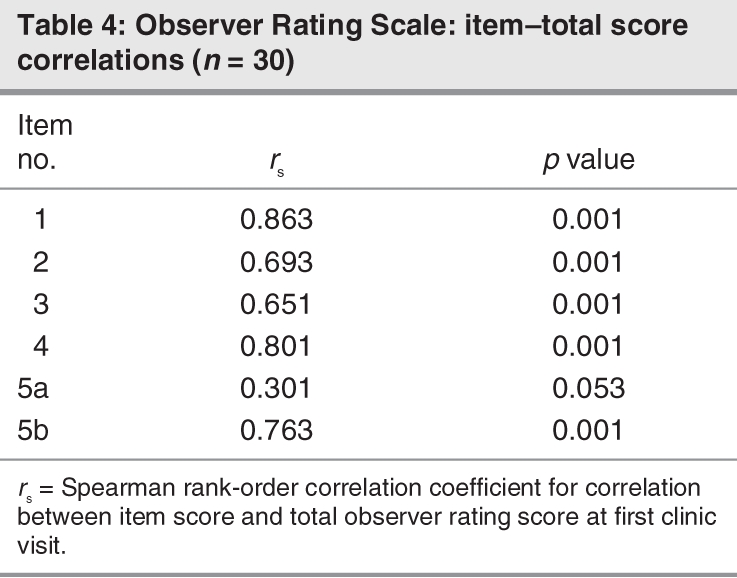
Observer Rating Scale: internal consistency and interrater reliability
The Observer Rating Scale was completed for 30 patients at their first assessment. An item correlation matrix was generated from the data of rater A (L.B.). For the 5-item Observer Rating Scale, the statistical analyses showed a mean interitem correlation of 0.3616 (minimum = –0.1343, maximum = 0.7172) and Cronbach's α = 0.7418. Evaluation of the item– total score correlations revealed that all items but 1 were significantly correlated with the total scale score at the 0.01 level. Item 5a (“jumpy when touched by someone”) was not significantly related to the total scale score (Table 4). Each item showed a range of responses (Table 2).
Table 4
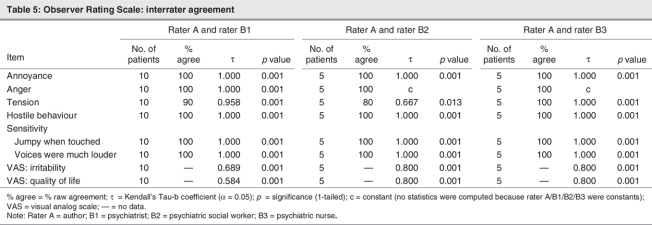
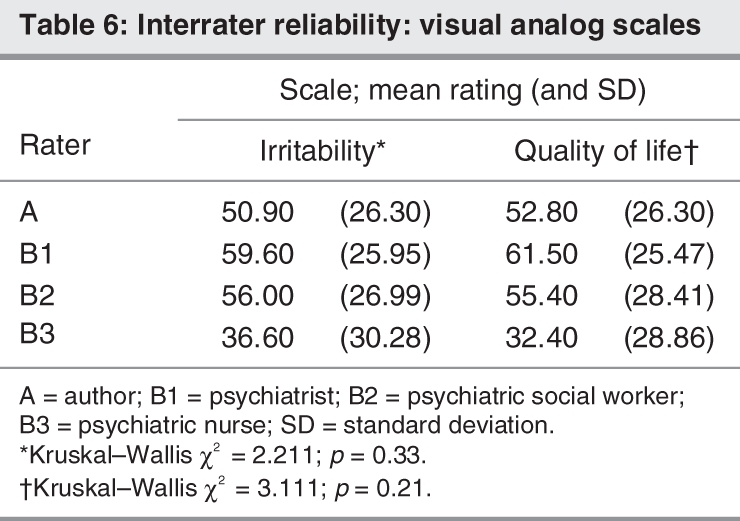
The Observer Rating Scale was completed by the lead author (rater A) simultaneously with a clinic psychiatrist (rater B1) (n = 10 patients) and subsequently with a clinic social worker (rater B2) (n = 5 patients) and a clinic nurse (rater B3) (n = 5 patients). Owing to the small sample size, interrater reliability was expressed as raw agreement rate (i.e., the percentage of times 2 raters agreed on the exact same rating, a format that is simple, intuitive and clinically meaningful). Kendall's τ coefficient was used to examine the degree of association between 2 raters.
The results are shown in Table 5. The pairs of clinicians had 100% agreement for the items of “annoyance,” “anger,” “hostile behaviour” and “sensitivity.” The results of the Kendall's τ analysis indicate that there was a significant correlation between each pair of raters for these items (τb = 1.000, p = 0.001). The analysis of the item “tension” showed 80%, 90% and 100% agreement for each pair of clinicians, respectively. For this latter item, the Kendall's τ analysis showed a significant correlation between rater A and rater B1 (90% raw agreement; τb = 0.958, p = 0.001) and also between rater A and rater B2 (80% raw agreement; τb = 0.667, p = 0.013).
Table 5
There was a significant correlation between raters on visual analog scale ratings of irritability, with Kendall's τ values ranging from 0.689 to 0.800, p = 0.001. Similarly, there was a significant correlation between raters on visual analog scale ratings of the effect of irritability on quality of life, with Kendall's τ values ranging from 0.584 to 0.800, p = 0.001.
We assessed rater bias by calculating the mean visual analog ratings of irritability and quality of life for each rater across all cases. High or low means relative to the means of other raters could indicate positive or negative rater bias, respectively. Treating the observers' ratings as independent samples, we used the Kruskal–Wallis 1-way analysis of variance by ranks test to compare differences in mean ranks between observers.
The mean visual analog scale ratings of irritability ranged from 36.60 (SD 30.28) by rater B3 (psychiatric nurse) to 59.60 (SD 25.95) by rater B1 (psychiatrist) (Table 6). The results of the Kruskal–Wallis 1-way analysis of variance by ranks test showed a nonsignificant difference between raters B1, B2 and B3 (χ2 = 2.211, p = 0.33). Similarly, the mean visual analog scale ratings of quality of life ranged from 32.40 (SD 28.86) by rater B3 to 61.50 (SD 25.47) by rater B1. The Kruskal–Wallis test showed a nonsignificant difference between raters A, B1, B2 and B3 (χ2 = 3.111, p = 0.21).
Table 6
Association between items of Self-Rating and Observer Rating Scales
All domains of the Self-Rating Scale (annoyance, anger, tension, hostile behaviour, sensitivity) correlated with the same domains of the Observer Rating Scale at the 0.05 level, with the exception of sensitivity to touch. The visual analog scale ratings of irritability at the time of assessment were significantly correlated between subjects and observer A (author) (rs = 0.420, p = 0.01), as were the Self-Rating and Observer Rating Scale total scores (rs = 0.643, p = 0.0001).
Scoring
A scale total of 42 points was divided into 3 equal subcategories: 1–14, 15–28 and 28–42, resulting in the categories of mild, moderate and severe irritability. The scoring thresholds, although speculative and needing confirmation through testing in larger samples and treatment trials, might assist with clinical decision making regarding treatment.
Discussion
The test samples comprised mainly English-speaking white women born in Canada, living in middle-class households, with postsecondary education and currently employed.
The pretest results indicated a high level of internal consistency reliability for both Self-Rating and Observer Rating Scales. A high α value is a prerequisite for internal consistency but may also suggest redundancy among the items.38,39 Alternatively, α can be inflated when there are more than 20 items on a scale, even if the correlation among items is small.39,41
The degree of item intercorrelation is also an indicator of internal consistency, with higher values reflecting increasing specificity of the target construct.42 The high mean interitem correlations for the Self-Rating (0.4928) and Observer Rating (0.5364) Scales suggest high internal consistency and hint at (but cannot alone determine) the unidimensionality of the scales.
For the shortened scales, the results indicated a moderate-to-high level of internal consistency for the Self-Rating and Observer Rating Scales. Preliminary evidence suggests that irritability may be a distinct and unidimensional construct. Further studies and a larger sample size are required to evaluate both the uniqueness and dimensionality of irritability.
The item “I have been irritable when someone touched me” has limited correlation with the other observer rating items or the scale total score but does, however, assess important information relevant to the construct of irritability. In the item-generation phase, about 1 in 4 women experienced a high sensitivity to touch when markedly irritable, and this had a notable impact on their intimate relationships. Therefore, we retained the item on touch in both scales.
The significant correlation between visual analog scale ratings of irritability completed by subjects and by observer A (L.B.) and the high correlation between total scale scores adds to the reliability of the mirror scales. Notwithstanding this, the results of the analysis of the correlation between items of the twin scales may be due to the sample size. Further, although semantic association links the items of the Self-Rating and Observer Rating Scales, they are not identical per se.
The reliability data have to some degree confirmed several hunches derived from the literature, clinical experience and the preliminary studies about irritability as a construct. The internal consistency of the Self-Rating Scale suggests that irritability may be a unidimensional construct even though there is a suggestion of heterogeneity among its aspects, as shown in the item “sensitivity to touch.”
The interpretability of the findings may be limited by the sample size. Although nonparametric statistical procedures are useful for nonnormal distributions and small sample sizes,43 the sample size may nonetheless hinder more general acceptance of the results. In addition, the sample was one of convenience and not a random sampling of this particular clinical population.
It is important to note that an instrument may be judged reliable or unreliable depending on the population in which it is evaluated.44 Our findings suggest that the new Born–Steiner Irritability Scale may be a promising measure to use in women with emotional problems related to the reproductive cycle. It will have to be tested in other populations to determine whether it is valuable in specific clinical subgroups of women only or whether it is more generalizable to broader groups of patients and conditions.
Mammen and colleagues'17 findings that anger attacks are typically ego-dystonic and associated with guilt, worry and regret, allude to the stigma associated with women regarding anger. Irritability and its close relation to anger pose a particular dilemma for women in our society: anger is often seen as a sign of weakness or emotional instability; it can ruin relationships, and it is seen as avoidable.45 Women learn early in life not to show anger, let alone discuss it. As the American Psychiatric Association Task Force on DSM-IV noted:
Displays of anger by men tend to be regarded as normative, even as evidence of strength and assertion, whereas women's anger is considered “masculine,” pathological, and/or negative and is actively discouraged and suppressed by society. This view is held by women as well as men.46
However, as Cox and colleagues45 assert, “there are no bad emotions.” All emotions have developed in our evolution as a species because they are helpful and necessary to our survival. This perspective is congruent with the literature on irritability as a phenomenon. Historically, irritability was viewed as a common trait in humans, and an increase in severity signalled physiologic imbalance (i.e., an increase in yellow bile). As such all emotions, including irritability, are natural and normal.
Nevertheless, as with the controversy surrounding the establishment of the entity termed late luteal phase dysphoric disorder, or PMDD as we now know it, raising the profile of irritability and linking it to women specifically may have potential to further stigmatize and denigrate women (especially outside the health care context). The intent of this research was not to suggest that all irritability or anger is pathological in either sex but to learn more about the parameters of the context — physiological, psychological and environmental — in which it occurs.
With use of the new measure, clinical intake has become more specific, and clinicians are now asking about irritability. Further, women are often relieved to be asked. They are also relieved to know that they are not isolated in their experience of irritability. Having a tool to measure irritability is useful and meaningful, particularly when a patient presents with irritability as a primary complaint with or without meeting DSM criteria for a depressive or anxiety disorder. Clinicians are able to discern how far from her usual self the patient feels and the impact of irritability on her quality of life.
The results showed that patients and clinicians complete this new scale easily and with no indication of harm. Use of the scale should always be at the discretion of the attending health care provider, depending on the presenting issue(s) and illness severity. Moreover, the scale should be piloted in any new clinical population or context before it is adopted for regular use.
The new, female-specific Born–Steiner Irritability Scale, one of a few instruments designed specifically for this clinical population, is poised to fill a large gap with respect to clinical assessment. With earlier detection, the sooner we, as mental health care providers, can offer effective, individually tailored treatment options and begin to knit the rents in intimate relationships that can occur because of suffering from irritability. Irritability, for too long “the forgotten dimension of female-specific mood disorders,”2 merits greater awareness and further investigation.
Acknowledgments
This research was supported in part by a grant from the Lilly Center for Women's Health, Indianapolis. Doctoral awards from the Father Sean O'Sullivan Research Centre, St. Joseph's Healthcare Hamilton and the Canadian Institutes of Health Research supported Dr. Born.
Footnotes
Presented at the 2nd World Congress of Women's Mental Health, Washington, Mar.17–21, 2004
Contributors: All authors designed the study. Drs. Born and Steiner acquired and analyzed the data and wrote the article, which Drs. Koren and Lin reviewed. All authors gave final approval for the article to be published.
The authors thank the participants for their kind cooperation, the Women's Health Concerns Clinic staff and students for their assistance in data collection and entry; Dr. Peter Bieling, Dr. Bruce Wainman, Irving Gold and Susan Barreca for their assistance with statistical analyses; the David Streiner seminar group for advice regarding scale format and testing; Drs. Shinya Ito, Sarah Romans and Bryanne Barnett for their comments related to the doctoral thesis; and Dr. Khrista Boylan for her comments related to the manuscript revision.
Competing interests: None declared.
Correspondence to: Dr. M. Steiner, Women's Health Concerns Clinic, St. Joseph's Healthcare Hamilton, 301 James St. S., Hamilton ON L8P 3B6; fax 905 521-6098; mst@mcmaster.ca
References
- 1.Irritability. The Oxford English Dictionary. 2nd ed. Oxford: Oxford University Press; 1989:102.
- 2.Born L, Steiner M. Irritability: the forgotten dimension of female-specific mood disorders. Arch Womens Ment Health 1999;2:153-67.
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Text revision. Washington: The Association; 2000.
- 4.Steiner M, Haskett RF, Carroll BJ. Premenstrual tension syndrome: the development of research diagnostic criteria and new rating scales. Acta Psychiatr Scand 1980;62:177-90. [DOI] [PubMed]
- 5.Endicott J, Amsterdam J, Eriksson E, et al. Is premenstrual dysphoric disorder a distinct clinical entity? J Womens Health Gender Based Med 1999;8:663-79. [DOI] [PubMed]
- 6.Born L, Palova E, Steiner M. Premenstrual syndromes: guidelines for treatment. In: Gaszner P, Halbreich U, editors. Women's mental health: an Eastern European perspective. Budapest: World Psychiatric Association; 2002. p. 56-72.
- 7.Hylan TR, Sundell K, Judge R. The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: experience from the United States, United Kingdom, and France. J Womens Health Gend Based Med 1999;8:1043-52. [DOI] [PubMed]
- 8.Cumming CE, Urion C, Cumming DC, et al. “So mean and cranky, I could bite my mother”: an ethnosemantic analysis of women's descriptions of premenstrual change. Women Health 1994;21:21-41. [DOI] [PubMed]
- 9.O'Hara MW, Zekoski EM, Philipps LH, et al. Controlled prospective study of postpartum mood disorders: comparison of childbearing and non-childbearing women. J Abnorm Psychol 1990;99:3-15. [DOI] [PubMed]
- 10.Field T, Diego M, Hernandez-Reif M, et al. Pregnancy anxiety and comorbid depression and anger: effects on the fetus and neonate. Depress Anxiety 2003;17:140-51. [DOI] [PubMed]
- 11.Huot RL, Brennan PA, Stowe ZN, et al. Negative affect in offspring of depressed mothers is predicted by infant cortisol levels at 6 months and maternal depression during pregnancy but not postpartum. Ann n Y Acad Sci 2004;1032:234-6. [DOI] [PubMed]
- 12.Kendell RE, McGuire RJ, Connor Y, et al. Mood changes in the first three weeks after childbirth. J Affect Disord 1981;3:317-26. [DOI] [PubMed]
- 13.Cox JL, Connor YM, Henderson I, et al. Prospective study of the psychiatric disorders of childbirth by self report questionnaire. J Affect Disord 1983;5:1-7. [DOI] [PubMed]
- 14.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. [DOI] [PubMed]
- 15.Snaith RP, Constantopoulos AA, Jardine MY, et al. A clinical scale for the self-assessment of irritability. Br J Psychiatry 1978;132:164-71. [DOI] [PubMed]
- 16.Brockington I. Puerperal psychosis. In: Motherhood and mental health. Oxford: Oxford University Press; 1996. p. 200-84.
- 17.Mammen OK, Shear MK, Pilkonis PA, et al. Anger attacks: correlates and significance of an under-recognized symptom. J Clin Psychiatry 1999;60:633-42. [PubMed]
- 18.Fava M, Anderson K, Rosenbaum JF. “Anger attacks”: possible variants of panic and major depressive disorders. Am J Psychiatry 1990;147:867-70. [DOI] [PubMed]
- 19.Holte A. Influence of natural menopause on health complaints: a prospective study of healthy Norwegian women. Maturitas 1992;14:127-41. [DOI] [PubMed]
- 20.von Muhlen DG, Kritz-Silverstein D, Barrett-Connor E. A community-based study of menopause symptoms and estrogen replacement in older women. Maturitas 1995;22:71-8. [DOI] [PubMed]
- 21.Hemminki E, Topo P, Kangas I. Experience and opinions of climacterium by Finnish women. Eur J Obstet Gynecol Reprod Biol 1995;62:81-7. [DOI] [PubMed]
- 22.Porter M, Penney GC, Russell D, et al. A population based survey of women's experience of the menopause. Br J Obstet Gynaecol 1996;103:1025-8. [DOI] [PubMed]
- 23.Goonaratna C, Fonseka P, Wijeywardene K. Perimenopausal symptoms in Sri Lankan women. Ceylon Med J 1999;44:63-9. [PubMed]
- 24.Obermeyer CM, Schulein M, Hajji N, et al. Menopause in Morocco: symptomatology and medical management. Maturitas 2002;41:87-95. [DOI] [PubMed]
- 25.Pan HA, Wu MH, Hsu CC, et al. The perception of menopause among women in Taiwan. Maturitas 2002;41:269-74. [DOI] [PubMed]
- 26.Stewart DE. Menopause in highland Guatemala Mayan women. Maturitas 2003;44:293-7. [DOI] [PubMed]
- 27.Harlow BL, Cohen LS, Otto MW, et al. Prevalence and predictors of depressive symptoms in older premenopausal women: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry 1999;56:418-24. [DOI] [PubMed]
- 28.Harlow BL, Wise LA, Otto MW, et al. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry 2003;60:29-36. [DOI] [PubMed]
- 29.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol 1957;21:343-9. [DOI] [PubMed]
- 30.Caprara G, Cinanni V, D'Imperio G, et al. Indicators of impulsive aggression: present status of research on irritability and emotional susceptibility scales. Pers Individ Dif 1985;6:665-74.
- 31.Coccaro EF, Harvey PD, Kupsaw-Lawrence E, et al. Development of neuropharmacologically based behavioral assessments of impulsive aggressive behavior. J Neuropsychiatry Clin Neurosci 1991;3:S44-51. [PubMed]
- 32.Born L, Steiner M. Gender differences in a self-report survey of irritability [abstract]. The 28th annual meeting of the North American Society for Psychosocial Obstetrics & Gynecology, 2000 Mar 9; St. Pete Beach (FL).
- 33.Born L, Steiner M, Koren G. Irritability: the burden of illness [abstract]. The 30th annual meeting of the North American Society for Psychosocial Obstetrics & Gynecology; 2002 Feb 20–23; Cancun (MX). Arch Women's Ment Health 2002;4:58.
- 34.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med 1988;18:1007-19. [DOI] [PubMed]
- 35.Ahearn EP, Carroll BJ. Short-term variability of mood ratings in unipolar and bipolar depressed patients. J Affect Disord 1996;36: 107-15. [DOI] [PubMed]
- 36.Ahearn EP. The use of visual analog scales in mood disorders: a critical review. J Psychiatr Res 1997;31:569-79. [DOI] [PubMed]
- 37.Dupuy HJ. The Psychological General Well-Being Index. In: Wenger NK, editor. Assessment of quality of life in clinical trials of cardiovascular therapies. New York: LeJacq; 1984. p. 170-83.
- 38.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 2nd ed. Oxford: Oxford University Press; 1995.
- 39.Streiner DL. A checklist for evaluating the usefulness of rating scales. Can J Psychiatry 1993;38:140-8. [DOI] [PubMed]
- 40.Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med 1998;17:101-10. [DOI] [PubMed]
- 41.Cortina JM. What is the coefficient alpha? An examination of theory and applications. J Appl Psychol 1993;78:98-104.
- 42.Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess 1995;7:309-19.
- 43.Pett MA. Nonparametric statistics for health care research: statistics for small samples and unusual distributions. Thousand Oaks (CA): Sage Publications; 1997.
- 44.Wilkinson L. The Task Force on Statistical Inference. Statistical methods in psychology journals. Guidelines and explanations. Am Psychol 1999;54:594-604.
- 45.Cox D, Bruckner KH, Stabb S. The anger advantage: the surprising benefits of anger and how it can change a woman's life. New York: Broadway Books; 2003.
- 46.American Psychiatric Association, Task Force on DSM-IV. Late luteal phase dysphoric disorder. In: DSM-IV sourcebook, volume 2. Washington: The Association; 1996. p. 317-94.