Abstract
Sporadic cases of colorectal cancer are primarily initiated by gene mutations in members of the canonical Wnt pathway, ultimately resulting in β-catenin stabilisation. Nevertheless, cells displaying nuclear β-catenin accumulation are nonrandomly distributed throughout the tumour mass and preferentially localise along the invasive front where parenchymal cells are in direct contact with the stromal microenvironment. Here, we discuss the putative role played by stromal cell types in regulating β-catenin intracellular accumulation in a paracrine fashion. As such, the tumour microenvironment is likely to maintain the cancer stem cell phenotype in a subset of cells, thus mediating invasion and metastasis.
Keywords: colorectal cancer, β-catenin, cancer stem cells, stroma, fibroblast
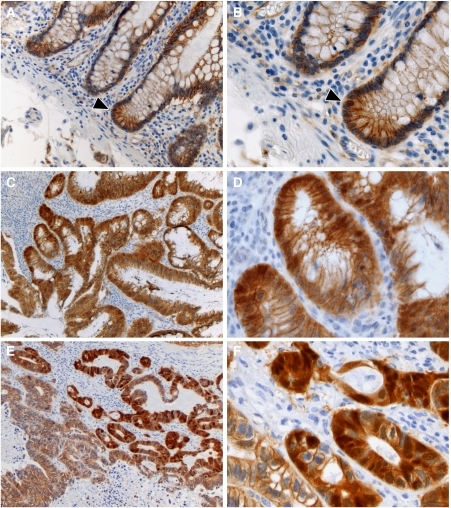
In the intestinal tissue architecture, epithelial cells lining the luminal surface are tightly regulated to ensure homeostasis. Epithelial cell renewal is fuelled by an adult stem cell compartment localised at the bottom of the crypt (Potten and Loeffler, 1990; Barker et al, 2007). As cells migrate upwards, after a transient proliferative phase, the epithelium differentiates into specialised cell types including absorptive enterocytes, mucus secreting goblet cells, and enteroendocrine cells. This migratory process with concomitant differentiation is finalised when cells reach the top of the crypt where they are exfoliated into the lumen upon apoptosis. In the upper gastrointestinal tract, Paneth cells represent an exception as they move downwards while differentiating. Overall, cell renewal, proliferation, and differentiation are coupled to positional localisation along the crypt-to-villus axis. In fact, this positional regulation of proliferation and differentiation can be correlated to gradients in the degree of activity of several signalling pathways known to govern stemness and differentiation, including Wnt/β-catenin, bone morphogenic protein (BMP), Notch, and transforming growth factor-β (TGFβ; Crosnier et al, 2006). The mesenchyme plays a complex role in the positional gradient of signalling ligand availability. Intestinal subepithelial myofibroblasts are specialised stromal cells that form a continuous sheet directly localised underneath the mucosa. These myofibroblasts contribute to epithelial cell function by providing mechanical support and secreting key signalling ligands. Thus, the intimate interaction between the parenchyme and mesenchyme ensures proper tissue function, balancing cell renewal, and differentiation. Activation of canonical Wnt signalling characterises the base of the intestinal crypt as shown by the nuclear β-catenin localisation crypt cells (Figure 1). Note that Paneth cells in the small intestine also show nuclear β-catenin accumulation as previously reported (Van Es et al, 2005). Moving upwards along the crypt-to-villus axis, terminal differentiation coincides with the more restricted membrane-bound β-catenin localisation and its absence in the nucleus and cytosol (Figure 1). Recently, it has been reported that the BMP antagonists, gremlin 1, gremlin 2, and chrodin-like 1, are selectively expressed by crypt-based myofibroblasts and smooth muscle cells (Kosinski et al, 2007). Moreover, Gremlin 1 was shown to activate Wnt/β-catenin signalling in normal rat intestinal epithelial cells, thus indicating that stromal-derived factors regulate Wnt/β-catenin-signalling activity in the intestinal stem cell niche.
Figure 1.
β-Catenin immunohistochemical staining of formalin-fixed, paraffin-embedded normal human colonic epithelia (panels A and B), and of a primary colorectal tumour (panels C and D) and a liver metastasis (panels E and F). The right panels contain magnifications (× 40) of specific areas from the left panels (× 20). The arrowheads in panels A and B indicate an epithelial cell localised at the base of the crypt with nuclear β-catenin accumulation. Both the primary colorectal tumour and liver metastasis (panels C–F) show nuclear β-catenin accumulation in cells invading the surrounding stroma, whereas other tumour cells display only membranous localisation.
Upon constitutive activation of the Wnt signalling route, intestinal homeostasis is disturbed, paving the way for pathogenesis. Indeed, the vast majority of sporadic colorectal cancer cases is caused by constitutive Wnt activation due to mutations in either the APC tumour suppressor or the β-catenin (CTNNB1) oncogene (Fodde et al, 2001). Loss of APC function leads to destabilisation of the ‘destruction complex’, a multiprotein complex encompassing three scaffold proteins, APC, Axin1, and Axin2 (conductin), and two kinases, glycogen synthase kinase-3β (GSK3β) and casein kinase 1 (CK1). The complex binds and phosphorylates β-catenin at serine and threonine residues, thus targeting it for ubiquitination and proteolytic degradation. In contrast, oncogenic mutations in β-catenin render it resistant to Ser/Thr phosphorylation and proteolytic degradation. Upon its cytoplasmic stabilisation and subsequent nuclear translocation, β-catenin binds to members of the TCF/LEF family of transcription factors, thus modulating expression of a broad range of target genes (http://www.stanford.edu/~rnusse/pathways/targets.html). Although the presence of these initiating mutations predicts nuclear β-catenin accumulation throughout the tumour mass, heterogeneous intracellular distributions are observed within primary colorectal tumours and their metastases. In particular, tumour cells located at the invasive front and those migrating into the adjacent stromal tissue are earmarked by nuclear β-catenin accumulation (Brabletz et al, 1998, 2001; Figure 1). Hence, different levels of Wnt/β-catenin-signalling activity are likely to reflect tumour heterogeneity and to underlie malignant behaviour (Gaspar and Fodde 2004; Brabletz et al, 2005a).
Several intrinsic (cell autonomous and/or autocrine) and extrinsic (paracrine, derived from the tumour microenvironment) factors may explain the observed heterogeneity of Wnt/β-catenin-signalling activity within the tumour mass (Fodde and Brabletz, 2007). Here, we discuss stromal factors likely to play a role in the heterogeneous β-catenin intracellular localisation and signalling activity in tumour cells. As such, the tumour microenvironment may drive tumour growth and even selectively support a subset of tumour cells, the cancer stem cells (CSCs), thus actively contributing to malignancy.
STROMAL CELLS AFFECTING TUMOUR GROWTH, NUCLEAR β-CATENIN ACCUMULATION, AND CANCER STEMNESS
As stated above, stromal regulation significantly contributes to the preservation of normal tissue architecture. Myofibroblasts, for example, are not only tightly associated with the intestinal epithelium thus ensuring homeostasis through reciprocal interactions, but are also essential for wound healing upon tissue injury, when they are transiently enriched and activated (Gabbiani, 2003). Expression of α-smooth muscle actin (α-SMA) characterises these myofibroblasts and underlies contractile force tension that facilitates healing. Myofibroblasts produce a variety of growth factors, prostaglandins, cytokines, chemokines, and extracellular matrix components that facilitate tissue repair and survival. Myofibroblasts arise through a multitude of processes, including transdifferentiation of resident fibroblasts, epithelial-to-mesenchymal transition (EMT) of parenchymal cells, recruitment, and differentiation of pericytes (progenitor cells localised at vascular sinuses), and from bone marrow-derived circulating immature fibrocytes (Desmouliere et al, 2004). Upon completion of the wound healing process, myofibroblasts revert back to their dormant state. In fact, tumorigenesis has been described as a condition comparable to an open wound of chronic nature (Dvorak, 1986). Accordingly, fibroblasts are one of the most abundant cell types in the stromal microenvironment associated with solid tumours (Adegboyega et al, 2002; De Wever and Mareel, 2003; Kalluri and Zeisberg, 2006). In response to the malignant lesion within the epithelial compartment, stromal fibroblasts become morphologically ‘activated’. Similar to the wound-healing process, an activated response of the tumour stroma may initially be triggered in an attempt to restore tissue homeostasis. However, as the tumour progresses, the microenvironment is more likely to become a ‘partner in crime’ in malignancy. A subset of tumour stromal fibroblasts, also referred to as cancer-associated fibroblasts (CAFs), peritumoral fibroblasts, reactive stromal fibroblasts, tumour-associated fibroblasts, or myofibroblasts, acquire distinct phenotypic characteristics. These cells share many of the properties of normal myofibroblasts such as α-SMA expression and increased production of growth factors, and of a variety of matrix remodelling proteases, which facilitate migration and invasion of the tumour cells (De Wever and Mareel, 2003; Desmouliere et al, 2004; Mukaratirwa et al, 2005). In view of their specific growth promoting effects, CAFs are primary candidates for locally modulating Wnt/β-catenin signalling, resulting in heterogeneous patterns of β-catenin intracellular localisation within colorectal tumours (Brabletz et al, 2001). Convergence of CAFs in specific regions of the tumour may provide a local increase in ligand availability that directly, in the case of Wnt ligands, or indirectly, in the case of growth factors, prostaglandins, and chemokines, may cross talk with and increase Wnt/β-catenin signalling.
Cross talk of a variety of factors has been reported to modulate nuclear β-catenin accumulation. For instance, hepatocyte growth factor or scatter factor (HGF, SF) induces β-catenin stabilisation in colorectal cancer cells via c-MET-dependent inhibition of GSKβ activity and its Tyr phosphorylation (Rasola et al, 2007). Tyr phosphorylation of β-catenin leads to its stabilisation and nuclear signalling activity by decreasing its binding affinity to E-cadherin and the APC/GSKβ/Axin destruction complex (Coluccia et al, 2007). Platelet-derived growth factor (PDGF) stimulation of HT-29 colorectal cancer cells increases β-catenin activation via p68-dependent inhibition of Ser/Thr phosphorylation by GSK3β (Yang et al, 2006).
In addition to the secretion of growth factors capable of modulating β-catenin stabilisation during tumour growth and local invasion, CAFs may also play a significant role in the metastatic process. As stated above, these cells can originate from circulating precursor cells recruited from the bone marrow, often referred to as fibrocytes. Therefore, these mesenchymal cells may not only exert local effects within the tumour, but could also represent systemic effectors relevant for the metastatic process by functioning as carrier cells during extravasation of tumour cells and/or ‘landscaping’ secondary organ sites where circulating tumour cells can home to and form secondary outgrowths. This may be of particular importance in view of the CSC hypothesis, which predicts that only a subset of tumour cells, displaying stem cell characteristics, will be successful in invading surrounding tissues and forming metastases in secondary organs. We have previously postulated that cancer stemness may be conferred by specific levels of β-catenin activation in colorectal cancer (Brabletz et al, 2005a; Fodde and Brabletz, 2007). Stromal cells may play a significant role by providing a supportive microenvironment that maintains CSCs at the primary tumour site and also underlies their invasive behaviour and spreading to distant sites. Karnoub et al (2007) have recently shown that bone marrow-derived mesenchymal stem cells can indeed increase metastatic potency of breast tumour cells. In addition, Kaplan et al (2005) have reported that haematopoietic progenitor cells expressing vascular endothelial growth factor receptor-1 are recruited and home to premetastatic niches prior to the arrival of tumour cells in mice injected with Lewis lung carcinoma or B16 melanoma cells. This response directs the metastatic pattern and is triggered by tumour-specific secreted factors. These data indicate that stromal (precursor) cells are active coconspirators in malignancy by increasing metastatic potential of tumour cells and providing a ‘congenial soil’ for secondary growth.
As stromal cells may significantly modulate both tumour growth and nuclear β-catenin accumulation and thus represent a cancer stemness determinant, specific stromal cell characteristics may be selected during tumorigenesis to provide a supportive microenvironment for pathogenic events. For instance, selective pressure from the tumour promotes genetic loss of p53 in stromal fibroblasts giving rise to highly proliferative stromal compartments in a mouse model for prostate cancer (Hill et al, 2005). Transforming growth factor-βis also highly expressed in most solid tumours and is capable of transforming fibroblasts towards an activated phenotype (De Wever and Mareel, 2003; Mishra et al, 2005; Orimo and Weinberg, 2006). Accordingly, stromal expression of the TGF-β type II receptor (TGFRII) reflects its activation by TGFβ stimulation and directly correlates with prognosis and survival in human colorectal cancer (Bacman et al, 2007). Stromal abrogation of TGFRII leads to prostate and stomach tumours in a murine model (Bhowmick et al, 2004). Moreover, expression of PDGFR (platelet-derived growth factor receptor) in stromal cells directly correlates with advanced stage disease in human colorectal cancer (Kitadai et al, 2006a). Both a DNA vaccine against PDGFRβ (Kaplan et al, 2006) as well as PDGFR inhibition by imatinib alone or in combination with irinotecan (Kitadai et al, 2006b), suppressed growth and dissemination of human colorectal cancer cells injected into mice, suggesting that increased PDGF signalling to stromal cells is a determinant for malignancy. Therefore, reciprocal interactions between tumour cells and the microenvironment facilitate tumour growth, invasion, and metastasis, by selecting not only for tumour cells capable of invasion and metastasis, but also for a stromal cell compartment that optimally supports the malignant phenotype.
In line with the above, EMT drives tumour cells towards a more mesenchymal phenotype and is implicated in invasive and malignant behaviour. It has been shown that colorectal cancer cells with nuclear β-catenin accumulation clustered along the invasive front undergo EMT as they detach from the tumour mass and invade the surrounding stroma (Brabletz et al, 2005b). Moreover, hepatocytes that have undergone TGFβ-induced EMT and have acquired a fibroblastoid phenotype, show nuclear β-catenin accumulation, proliferation, and migration upon PDGF treatment (Fischer et al, 2007). S100A4, a mesenchymal gene expressed during EMT and associated with poor prognosis in colorectal cancer, is in itself a target gene of Wnt/β-catenin signalling (Stein et al, 2006). Therefore, EMT may determine a ‘double jeopardy’ effect: CSCs earmarked by nuclear β-catenin accumulation can transdifferentiate, thus generating a permissive niche capable of eliciting nuclear β-catenin translocation in other parenchymal cells located in direct contact with the stromal tumour microenvironment.
IMMUNE CELLS AND ADIPOCYTES MODULATING TUMOUR GROWTH
Besides stromal fibroblasts, the tumour microenvironment consists of a variety of cell types capable of modulating tumour growth and possibly cancer stemness. Tumour-infiltrating innate and adoptive immune cells may confer both tumour-growth-promoting and -inhibiting effects (de Visser et al, 2006). Intuitively, increased infiltration of T cells should correlate with improved tumour clearance and prognosis, as recently reported in colorectal cancer cohorts (Pages et al, 2005; Clarke et al, 2006; Galon et al, 2006). However, a subtype of T cells, termed regulatory T cells (Tregs), are likely to exert tumour-growth-promoting effects due to their immune suppressive function to mediate self-tolerance, prevent autoimmunity, and enable the presence of a commensal bacterial flora in the intestine (Powrie, 2004). Regulatory T cells have been reported to be increased in peripheral blood and infiltrating lymphocytes among colorectal cancer patients (Ling et al, 2007). The increased presence of these Tregs sets the stage for immune evasion by tumour cells.
Several other tumour-infiltrating immune cells have been reported to support tumour growth, including tumour-associated macrophages, and immature myeloid and dendritic cells (Lizee et al, 2006). Also, it has been reported that specific functional aspects of innate immune cells are pivotal for intestinal homeostasis, inflammation, and tumorigenesis. Exemplary, a T-cell-specific knockout mouse model of Smad4, a downstream component of TGFβ and BMP signalling, resulted in intestinal tumorigenesis (Kim et al, 2006). Recently, Kitamura et al (2007) showed that immature myeloid cells (iMCs) are recruited from the bone marrow to the tumour invasion front of compound heterozygous cis-Apc+/Δ716;Smad4+/− mice with invasive intestinal adenomacarcinoma. These CD34+ iMCs promote tumour growth by expression of the matrix metalloproteinases, MMP9 and MMP2, and the CC-chemokine receptor 1 (CCR1), and migrate towards the CCR1 ligand CCL9, highly increased in the tumour epithelium. Greten et al (2004) reported that activation of the transcription factor NFκB (nuclear factor-κB), a key mediator of inflammation, has a critical role in the development of tumours resulting from chronic inflammation or exogenous mutagens, induced by exposure to dextran sulphate sodium salt and Azoxymethane (AOM). Moreover, genetic ablation of MyD88, a signalling adaptor of Toll-like receptors in the innate immune system, was shown to reduce mortality due to intestinal tumorigenesis in Apc+/Min mice (Rakoff-Nahoum and Medzhitov, 2007). In fact, Auguste et al (2007) have shown that liver metastases formation coincides with an inflammatory, TNFα-mediated, host organ response. This inflammatory reaction upregulates cell adhesion molecules in the liver stromal microvasculature and supports tumour cell arrest and extravasation in a metastatic mouse model induced by intrasplenic injection of the highly metastatic human colorectal cancer cell line, CX-1. Finally, adipocytes have also been reported to promote proliferation of colon cancer cells (Amemori et al, 2007).
Overall, these data indicate that the host inflammatory response is a key mediator of tumour survival, extravasation, and metastasis formation. In fact, a broad spectrum of diverse cell types from within the tumour microenvironment may contribute to the modulation of β-catenin activation and cancer stemness, thus promoting intestinal tumour progression and even initiation. In this regard, tumour progression and cancer stemness may significantly be determined by a context-dependent modulation of β-catenin activity in colorectal cancer.
HYPOXIA- AND OXIDATIVE STRESS-INDUCED SELECTION OF TUMOUR CELLS DISPLAYING NUCLEAR β-CATENIN ACCUMULATION AND CANCER STEMNESS
Besides the specific stromal cell types, other factors from within the tumour microenvironment are likely to play significant roles in promoting cancer stemness and malignant behaviour through β-catenin nuclear accumulation and signalling. Hypoxia underlies progressive tumour growth in the majority of solid tumours (Sullivan and Graham, 2007). During tumour growth, certain areas are exposed to reduced oxygen tension due to a disturbed microcirculation and inadequate blood supply. Hypoxic conditions are often found in the invasive front of colorectal carcinomas in association with stabilisation of the HIF1α (hypoxia-inducible factor-1α) transcription factor (Sivridis et al, 2005). HIF1α stabilisation results in transcriptional regulation of a variety of target genes, including the proangiogenic factors vascular endothelial growth factor and PDGF (Koukourakis et al, 2006). In fact, Cleven et al (2007), showed that expression of HIF1α in the stromal compartment correlates with poor prognosis in colorectal cancer. Moreover, loss of MUTYH function, a DNA glycogylase involved in base excision repair caused by oxidative stress, results in increased susceptibility to spontaneous and oxidative stress-induced (by the oxidative reagent KbrO3) intestinal tumorigenesis (Sakamoto et al, 2007). These data indicate that hypoxia and oxidative stress play a pivotal role in colorectal cancer progression. Notably, Kaidi et al (2007) reported that HIF1α binds directly to β-catenin in the nucleus, thus linking hypoxia-induced cellular changes to β-catenin activation.
BIOLOGICAL EFFECTS OF NUCLEAR β-CATENIN ACCUMULATION
The nuclear accumulation of β-catenin observed in colorectal cancer cells distributed along the invasive front may not only reflect a specific level of canonical Wnt activity but also indicate the activation of additional signalling pathways. It has been shown that, in the nucleus, β-catenin binds to a broad spectrum of transcription factors other than TCF and LEF and modulates a plethora of downstream targets possibly contributing to cancer stemness and malignancy (Table 1). As stated above, hypoxia induces stabilisation of HIF1α and its interaction with β-catenin, thereby competing with TCF/LEF1 transcription factors for β-catenin binding in colorectal cancer cells (Kaidi et al, 2007). Stabilisation and binding of HIF1α to β-catenin results in inhibition of Wnt reporter activity, induction of cell-cycle arrest, survival, and cellular adaptation, and is likely to contribute to the malignant and invasive behaviour of tumour cells exposed to reduced oxygen tension. Similarly, oxidative stress stimulates β-catenin binding to the Forkhead box O transcription factors, inducing cell-cycle arrest and survival (Essers et al, 2005).
Table 1. Nuclear β-catenin-binding partners.
| Protein | Interaction and biological significance | Reference |
|---|---|---|
| 14-3-3-z | Binds β-catenin and stabilises it, Akt dependent | Tian et al (2004) |
| Akt | Phosphorylates β-catenin at S552 and increases cytoplasmic pool, increases binding to 14-3-3, increases transcriptional activity | Fang et al (2007) |
| AR (androgen receptor) | Binds β-catenin, augments AR activity, inhibits TCF-dependent transcription | Yang et al (2002) |
| AP1 and Smad3/4 | Complex with β-catenin and TCF/Lef1 to activate gastrin target gene | Chakladar et al (2005) |
| BCL9 (Legless) | Binds β-catenin and TCF/LEF1, increases transcription, Pygopus dependent | Kramps et al (2002) |
| B9L/BCL9-2 (BCL9-like protein) | Binds β-catenin, increases transcription, induces EMT | Adachi et al (2004); Brembeck et al (2004) |
| Brg-1 (chromatin remodelling factor) | Binds β-catenin, increases transcription | Barker et al (2001) |
| c-Jun (phosphorylated) | Binds β-catenin and TCF/LEF1 in a JNK- and β-catenin-dependent manner, knockout decreases tumour multiplcity in Apcmin animals | Nateri et al (2005); Toualbi et al (2007) |
| c-Fos | Binds β-catenin, increases transcription | Toualbi et al (2007) |
| CARM1 (coactivator-associated arginine methyltransferase) | Binds β-catenin, increases transcription | Koh et al (2002) |
| CBP (CREB-binding protein) | Binds β-catenin | Takemaru and Moon (2000) |
| cdx1 and cdx2 (homeodomain transcription factors) | Decreases β-catenin Tyr phosphorylation, decreases transcription, induces E-cadherin adhesion | Guo et al (2004); Ezaki et al (2007) |
| Chibby (nuclear protein) | Binds β-catenin, inhibits transcription | Takemaru et al (2003) |
| CREB (cyclic AMP response element binding protein) | Binds β-catenin, induces expression of WISP-1 (Wnt-1-induced secreted protein 1) | Xu et al (2000) |
| cul4B (Cullin4B/E3-ubiquitin ligase) | Binds β-catenin and induces its proteolytic degradation | Tripathi et al (2007) |
| Duplin (axis duplication inhibitor) | Binds β-catenin in nucleus and inhibits transcription | Sakamoto et al (2000) |
| EBP50 (PDZ-containing protein) | Binds β-catenin, increases transcription | Shibata et al (2003) |
| emerin (type II inner nuclear membrane protein) | Binds β-catenin resulting in its cytoplasmic retention and decreased transcriptional activity | Markiewicz et al (2006) |
| ERα (estrogen receptor) | Binds β-catenin, increases transcription | Kouzmenko et al (2004) |
| ezh2 (enhancer of zeste homolog 2, polycomb group protein) | Binds β-catenin and ERα | Shi et al (2007) |
| FHL2 (four and a half of LIM-only protein 2, LIM coactivator) | Binds β-catenin, increases transcription | Wei et al (2003); Martin et al (2002) |
| FOXO (insulin- and oxidative stress signaling-induced transcription factor) | Binds β-catenin resulting in increased FOXO target gene transcription | Essers et al (2005) |
| FUS (fusion/translocated in liposarcoma, TLS) | Binds and increases β-catenin, regulates pre-mRNA splicing | Sato et al (2005) |
| GRIP1 (p160 coactivator of AR) | Binds β-catenin, augments AR activity | Li et al (2004) |
| Groucho/TLE (transcriptional repressor) | Binds β-catenin and is subsequently displaced from TCF/LEF1 | Daniels and Weis (2005) |
| HIF1α (hypoxia inducible factor) | Binds β-catenin, competes with TCF/LEF1, induces survival and cellular adaptation to hypoxia | Kaidi et al (2007) |
| hARD1 (human arrest defective 1, acetyltransferase) | Binds and acetylates β-catenin, increases transcription | Lim et al (2006) |
| I-mfa (inhibitor of MyoD Family a) | Binds β-catenin, relieving I-mfa-mediated gene repression | Pan et al (2005) |
| ICAT (inhibitor of β-catenin and TCF-4) | Binds β-catenin, represses transcription | Tago et al (2000) |
| IKKα (IκB kinase α) | Binds β-catenin, inhibits its ubiquitination, increases transcription | Lamberti et al (2001) |
| IKKβ (IκB kinase β) | Binds β-catenin, inhibits transcription | Lamberti et al (2001) |
| LRH-1 (orphan nuclear receptor) | Binds β-catenin, induces proliferation | Botrugno et al (2004) |
| LZTS2 (leucine zipper tumor suppressor 2) | Binds β-catenin, inhibits transcription | Thyssen et al (2006) |
| Mediator (MED12 subunit) | Binds β-catenin, increases transcription | Kim et al (2006) |
| Mitf (microphthalmia-associated transcription factor) | Binds β-catenin and competes with TCF/LEF1 to activate mitf target genes, important for melanocyte development | Schepsky et al (2006) |
| NFκB, p50 subunit | Binds β-catenin, decreases NFκB DNA binding, transactivation activity, regulates TNFα-induced CRP (C-reactive protein, acute-phase response protein) expression | Deng et al (2002); Sun et al (2005); Choi et al (2007) |
| Nurr1 (orphan nuclear receptor) | Binds β-catenin, increases transcription | Kitagawa et al (2007) |
| oct3/4 | Binds β-catenin in ES cells, upregulates Nanog | Takao et al (2007) |
| p68 (DEAD box family of RNA helicases) | Binds β-catenin upon PDGF-induced Tyr phosphorylation of p68, increases transcription and EMT | Yang et al (2006) |
| p300 | Binds and acetylates β-catenin, increases transcription | Sun et al (2000); Hecht et al (2000) |
| Parafibromin (component of polymerase-associated factor 1 (PAF1) complex) | Binds β-catenin, increases transcription, Pogypus dependent | Mosimann et al (2006) |
| Pin1 (prolyl isomerase) | Binds β-catenin, displaces it from APC, stabilises it and induces transcription, overexpressed in human tumours | Ryo et al (2001) |
| Pitx2 (bicoid-related transcription factor) | Induced by Wnt/Dvl/β-catenin, increases transcription | Kioussi et al (2002) |
| Pontin52 (nuclear protein) | Binds β-catenin | Bauer et al (1998) |
| PPARγ (peroxisome proliferator-activated receptor) | Binds β-catenin, decreases membrane bound and cytoplasmic fraction | Sharma et al (2004); Liu et al (2004) |
| PRA1 (Prenylated Rab acceptor 1) | Binds β-catenin, inhibits transcription | Kim et al (2006) |
| prop1 (Prophet of Pit1, homeodomain factor) | Binds β-catenin, activates expression of lineage-determining transcription factor Pit1, represses the lineage-inhibiting transcription factor Hesx1 via TLE/Reptin/HDAC1 corepressor complexes | Olson et al (2006) |
| Pygopus | Complexes with β-catenin and TCF/LEF1 in a Legless-dependent manner | Kramps et al (2002); Thompson et al (2002) |
| RanBP3 (Ran binding protein 3) | Cofactor of chromosome region maintenance 1 (CRM1)-mediated nuclear export binds β-catenin in a RanGTP-stimulated manner, inhibits transcriptional activity | Hendriksen et al (2005) |
| RAR (retinoid acid receptor) | Binds β-catenin in retinoid-dependent manner, competes for binding with TCF/LEF1 | Easwaran et al (1999) |
| Reptin52 (homologue of pontin52) | Binds β-catenin and Pontin52, inhibits transcription | Bauer et al (2000) |
| RXRα (retinoid X receptor) | Binds β-catenin, targets it for proteolytic degradation | Xiao et al (2003) |
| SHP-1 (protein-tyrosine phosphatase) | Binds β-catenin and inhibits transcription in intestinal epithelial cells | Duchesne et al (2003) |
| Smad1 | Complexes with β-catenin and TCF/LEF1 resulting in increased myc expression | Hu and Rosenblum (2005) |
| Smad3 | Binds β-catenin and TCF/LEF1 | Labbe et al (2000); Jian et al (2006) |
| Smad4 | Interacts with TCF/LEF1 (strong) and β-catenin (weak), coregulates TGFβ/Wnt common target genes | Nishita et al (2000) |
| Smad7 | Binds β-catenin, important for TGFβ-induced apoptosis and targets β-catenin for proteolytic degradation | Edlund et al (2005); Han et al (2006) |
| Sox4 | Binds and stabilises β-catenin and TCF/LEF1 | Sinner et al (2007) |
| Sox9 | Binds β-catenin and targets it for degradation | Akiyama et al (2004) |
| Sox17 | Binds β-catenin and TCF/LEF1, targets its for proteolytic degradation | Sinner et al (2007) |
| TAK1 (MAPKKK) and NLK (Nemo-like kinase) | Interact with and phosphorylate TCF/LEF1 and β-catenin, inhibit DNA binding capacity and transcription | Ishitani et al (1999) |
| Teashirt (zinc finger protein) | Binds to armidillo (Drosophila homologue of β-catenin), activated by Wingless | Gallet et al (1998) |
| TCFs | Bind β-catenin | Molenaar et al (1996) |
| TIF2/GRIP1 (transcriptional intermediary factor-2/glucocorticoid receptor interacting protein-1) | Binds β-catenin and increases binding affinity to AR | Song and Gelmann (2005) |
| TOPO IIα (DNA topoisomerase IIα) | Binds β-catenin, increases transcription | Sato et al (2005); Huang et al (2007) |
| VDR (vitamin D receptor) | Binds β-catenin in a vitamin D-dependent manner, competes for binding with TCF/LEF1 | Pálmer et al (2001) |
| XSox17α/β and Xsox3 | Bind β-catenin and inhibit transcription | Zorn et al (1999) |
EMT=epithelial-to-mesenchymal transition; FOXO=Forkhead box O; PDGF=platelet-derived growth factor; TGFβ=transforming growth factor-β.
Proteins previously shown to directly bind to β-catenin in the nucleus are listed in alphabetical order together with a brief description and corresponding literature references. Please note that the list is admittedly incomplete as only direct binding partners have been included. Many other proteins have been excluded that do not directly bind to β-catenin but participate to its many complexes and may yet significantly affect its function.
Through interaction with Smads (including Smad1, Smad3, and Smad4), β-catenin may also coregulate a subset of common TGFβ, BMP, and Wnt target genes (Nishita et al, 2000; Hussein et al, 2003; Chakladar et al, 2005; Hu and Rosenblum, 2005). Transforming growth factor-β and BMP signalling are known to be important regulators of epithelial cell function. Synergism among TGFβ, BMP, and Wnt signalling pathways may represent a significant determinant of malignant behaviour in tumour cells. β-Catenin binding to Smad7, an inhibitory molecule induced upon TGFβ pathway activation as part of a negative feedback loop, has also been reported to be rate limiting for TGFβ-induced apoptosis (Edlund et al, 2005) and induces proteolytic degradation of β-catenin (Han et al, 2006). When c-Jun, a stress- and growth factor-induced transcription factor, is recruited to the TCF/LEF1/β-catenin complex, synergistic effects on intestinal tumorigenesis are observed (Nateri et al, 2005). Also, gut-specific deletion of c-Jun decreased tumour multiplicity and increased life span in the ApcMin mouse model for intestinal cancer. Recently, both c-Jun and its known heterodimerisation partner, c-Fos, were reported to bind directly to β-catenin (Toualbi et al, 2007). Therefore, binding of β-catenin to different interaction partners in the nucleus may direct both TCF/LEF1-dependent and -independent transcriptional regulation.
Hence, in view of this observed promiscuity for nuclear transcription factors (Table 1), β-catenin is likely to represent a central node where different signals converge and are subsequently coordinated to regulate tissue homeostasis under physiological conditions and cancer stemness in the context of tumour–stroma interactions. Because the putative β-catenin interaction partners are themselves regulated by extracellular stimuli, it is plausible that the subsequent effects on β-catenin activation and possibly cancer stemness are modulated in a context-dependent manner. In fact, β-catenin has been reported to interact directly with several growth factor receptors, including EGFR (epidermal growth factor receptor, ErbB1), Met (the receptor for HGF), TGFRII (the receptor that is activated upon TGF stimulation), and KIT (the receptor for stem cell factor; Hoschuetzky et al, 1994; Monga et al, 2002; Tian and Phillips, 2002; Kajiguchi et al, 2008). These interactions result in β-catenin Tyr phosphorylation, stabilisation, and increased transcriptional activity.
CONCLUSIONS
Despite the clear genetic prerequisite for mutations in downstream components of the Wnt/β-catenin-signalling pathway that result in its constitutive activation, heterogeneous intratumour expression and subcellular localisation of β-catenin is commonly observed in colorectal cancer. Tumour cells located at the invasive front display increased nuclear β-catenin accumulation, suggesting that this nonrandom intracellular distribution earmarks and underlies tumour heterogeneity and malignancy. Therefore, it has been postulated that β-catenin may play a significant role in cancer stemness, driving invasion and metastasis. β-Catenin regulation is already known to be important during homeostasis, as Wnt/β-catenin signalling governs several adult stem cell niches, including the intestinal crypt. The tumour microenvironment may play a central role in the malignant transformation of tumour cells by locally modifying β-catenin activity at the primary tumour site as well as preparing secondary organ sites for metastatic growth. Individual ‘stromal signatures’, that is, characteristic of stromal cell function, inflammation, and other stress-induced responses, may determine disease progression, responsiveness to different (adjuvant) therapeutic strategies, and, thus, prognosis and survival for colorectal cancer patients. Stromal cells have even been suggested as possible targets for tailor-made therapeutic interventions for intestinal tumorigenesis, rather than parenchymal cells. Here, we propose that the functional characterisation of additional β-catenin-binding partners in these alleged CSCs will improve our understanding of malignancy and invasion and open future perspectives for a metastasis-free survival to colorectal cancer patients.
Acknowledgments
We thank Frank van der Panne for his technical assistance in preparing the graphical images. RF is supported by grants from the Dutch Research Council (NWO-Vici), EU FP6 (MCSCs), and the Bsik (ICES/KIS-3) program of the Dutch Government (BSIK 03038).
References
- Adegboyega PA, Mifflin RC, DiMari JF, Saada JI, Powell DW (2002) Immunohistochemical study of myofibroblasts in normal colonic mucosa, hyperplastic polyps, and adenomatous colorectal polyps. Arch Pathol Lab Med 126: 829–836 [DOI] [PubMed] [Google Scholar]
- Amemori S, Ootani A, Aoki S, Fujise T, Shimoda R, Kakimoto T, Shiraishi R, Sakata Y, Tsunada S, Iwakiri R, Fujimoto K (2007) Adipocytes and preadipocytes promote the proliferation of colon cancer cells in vitro. Am J Physiol Gastrointest Liver Physiol 292(3): G923–G929 [DOI] [PubMed] [Google Scholar]
- Auguste P, Fallavollita L, Wang N, Burnier J, Bikfalvi A, Brodt P (2007) The host inflammatory response promotes liver metastasis by increasing tumor cell arrest and extravasation. Am J Pathol 170: 1781–1792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacman D, Merkel S, Croner R, Papadopoulos T, Brueckl W, Dimmler A (2007) TGF-beta receptor 2 downregulation in tumour-associated stroma worsens prognosis and high-grade tumours show more tumour-associated macrophages and lower TGF-beta1 expression in colon carcinoma: a retrospective study. BMC Cancer 7: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, Clevers H (2007) Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 449: 1003–1007 [DOI] [PubMed] [Google Scholar]
- Bhowmick NA, Chytil A, Plieth D, Gorska AE, Dumont N, Shappell S, Washington MK, Neilson EG, Moses HL (2004) TGF-beta signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science 303: 848–851 [DOI] [PubMed] [Google Scholar]
- Brabletz T, Hlubek F, Spaderna S, Schmalhofer O, Hiendlmeyer E, Jung A, Kirchner T (2005b) Invasion and metastasis in colorectal cancer: epithelial–mesenchymal transition, mesenchymal–epithelial transition, stem cells and beta-catenin. Cells Tissues Organs 179: 56–65 [DOI] [PubMed] [Google Scholar]
- Brabletz T, Jung A, Hermann K, Gunther K, Hohenberger W, Kirchner T (1998) Nuclear overexpression of the oncoprotein beta-catenin in colorectal cancer is localized predominantly at the invasion front. Pathol Res Pract 194: 701–704 [DOI] [PubMed] [Google Scholar]
- Brabletz T, Jung A, Reu S, Porzner M, Hlubek F, Kunz-Schughart LA, Knuechel R, Kirchner T (2001) Variable beta-catenin expression in colorectal cancers indicates tumor progression driven by the tumor environment. Proc Natl Acad Sci USA 98: 10356–10361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brabletz T, Jung A, Spaderna S, Hlubek F, Kirchner T (2005a) Opinion: migrating cancer stem cells – an integrated concept of malignant tumour progression. Nat Rev Cancer 5: 744–749 [DOI] [PubMed] [Google Scholar]
- Chakladar A, Dubeykovskiy A, Wojtukiewicz LJ, Pratap J, Lei S, Wang TC (2005) Synergistic activation of the murine gastrin promoter by oncogenic Ras and beta-catenin involves SMAD recruitment. Biochem Biophys Res Commun 336: 190–196 [DOI] [PubMed] [Google Scholar]
- Clarke SL, Betts GJ, Plant A, Wright KL, El-Shanawany TM, Harrop R, Torkington J, Rees BI, Williams GT, Gallimore AM, Godkin AJ (2006) CD4+CD25+FOXP3+ regulatory T cells suppress anti-tumor immune responses in patients with colorectal cancer. PLoS ONE 1: e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleven AH, van Engeland M, Wouters BG, de Bruine AP (2007) Stromal expression of hypoxia regulated proteins is an adverse prognostic factor in colorectal carcinomas. Cell Oncol 29: 229–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coluccia AM, Vacca A, Dunach M, Mologni L, Redaelli S, Bustos VH, Benati D, Pinna LA, Gambacorti-Passerini C (2007) Bcr-Abl stabilizes beta-catenin in chronic myeloid leukemia through its tyrosine phosphorylation. EMBO J 26(5): 1456–1466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosnier C, Stamataki D, Lewis J (2006) Organizing cell renewal in the intestine: stem cells, signals and combinatorial control. Nat Rev Genet 7: 349–359 [DOI] [PubMed] [Google Scholar]
- de Visser KE, Eichten A, Coussens LM (2006) Paradoxical roles of the immune system during cancer development. Nat Rev Cancer 6: 24–37 [DOI] [PubMed] [Google Scholar]
- De Wever O, Mareel M (2003) Role of tissue stroma in cancer cell invasion. J Pathol 200: 429–447 [DOI] [PubMed] [Google Scholar]
- Desmouliere A, Guyot C, Gabbiani G (2004) The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. Int J Dev Biol 48: 509–517 [DOI] [PubMed] [Google Scholar]
- Dvorak HF (1986) Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 315: 1650–1659 [DOI] [PubMed] [Google Scholar]
- Edlund S, Lee SY, Grimsby S, Zhang S, Aspenstrom P, Heldin CH, Landstrom M (2005) Interaction between Smad7 and beta-catenin: importance for transforming growth factor beta-induced apoptosis. Mol Cell Biol 25: 1475–1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essers MA, de Vries-Smits LM, Barker N, Polderman PE, Burgering BM, Korswagen HC (2005) Functional interaction between beta-catenin and FOXO in oxidative stress signaling. Science 308: 1181–1184 [DOI] [PubMed] [Google Scholar]
- Fischer AN, Fuchs E, Mikula M, Huber H, Beug H, Mikulits W (2007) PDGF essentially links TGF-beta signaling to nuclear beta-catenin accumulation in hepatocellular carcinoma progression. Oncogene 26(23): 3395–3405 [DOI] [PubMed] [Google Scholar]
- Fodde R, Brabletz T (2007) Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr Opin Cell Biol 19(2): 150–158 [DOI] [PubMed] [Google Scholar]
- Fodde R, Smits R, Clevers H (2001) APC, signal transduction and genetic instability in colorectal cancer. Nat Rev Cancer 1: 55–67 [DOI] [PubMed] [Google Scholar]
- Gabbiani G (2003) The myofibroblast in wound healing and fibrocontractive diseases. J Pathol 200: 500–503 [DOI] [PubMed] [Google Scholar]
- Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313: 1960–1964 [DOI] [PubMed] [Google Scholar]
- Gaspar C, Fodde R (2004) APC dosage effects in tumorigenesis and stem cell differentiation. Int J Dev Biol 48: 377–386 [DOI] [PubMed] [Google Scholar]
- Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ, Kagnoff MF, Karin M (2004) IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell 118: 285–296 [DOI] [PubMed] [Google Scholar]
- Han G, Li AG, Liang YY, Owens P, He W, Lu S, Yoshimatsu Y, Wang D, Ten Dijke P, Lin X, Wang XJ (2006) Smad7-induced beta-catenin degradation alters epidermal appendage development. Dev Cell 11: 301–312 [DOI] [PubMed] [Google Scholar]
- Hill R, Song Y, Cardiff RD, Van Dyke T (2005) Selective evolution of stromal mesenchyme with p53 loss in response to epithelial tumorigenesis. Cell 123: 1001–1011 [DOI] [PubMed] [Google Scholar]
- Hoschuetzky H, Aberle H, Kemler R (1994) Beta-catenin mediates the interaction of the cadherin–catenin complex with epidermal growth factor receptor. J Cell Biol 127: 1375–1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu MC, Rosenblum ND (2005) Smad1, beta-catenin and Tcf4 associate in a molecular complex with the Myc promoter in dysplastic renal tissue and cooperate to control Myc transcription. Development 132: 215–225 [DOI] [PubMed] [Google Scholar]
- Hussein SM, Duff EK, Sirard C (2003) Smad4 and beta-catenin co-activators functionally interact with lymphoid-enhancing factor to regulate graded expression of Msx2. J Biol Chem 278: 48805–48814 [DOI] [PubMed] [Google Scholar]
- Kaidi A, Williams AC, Paraskeva C (2007) Interaction between beta-catenin and HIF-1 promotes cellular adaptation to hypoxia. Nat Cell Biol 9(2): 210–217 [DOI] [PubMed] [Google Scholar]
- Kajiguchi T, Lee S, Lee MJ, Trepel JB, Neckers L (2008) KIT regulates tyrosine phosphorylation and nuclear localization of beta-catenin in mast cell leukemia. Leuk Res 32(5): 761–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R, Zeisberg M (2006) Fibroblasts in cancer. Nat Rev Cancer 6: 392–401 [DOI] [PubMed] [Google Scholar]
- Kaplan CD, Kruger JA, Zhou H, Luo Y, Xiang R, Reisfeld RA (2006) A novel DNA vaccine encoding PDGFRbeta suppresses growth and dissemination of murine colon, lung and breast carcinoma. Vaccine 24: 6994–7002 [DOI] [PubMed] [Google Scholar]
- Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, MacDonald DD, Jin DK, Shido K, Kerns SA, Zhu Z, Hicklin D, Wu Y, Port JL, Altorki N, Port ER, Ruggero D, Shmelkov SV, Jensen KK, Rafii S, Lyden D (2005) VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 438: 820–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, Bell GW, Richardson AL, Polyak K, Tubo R, Weinberg RA (2007) Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 449: 557–563 [DOI] [PubMed] [Google Scholar]
- Kim BG, Li C, Qiao W, Mamura M, Kasprzak B, Anver M, Wolfraim L, Hong S, Mushinski E, Potter M, Kim SJ, Fu XY, Deng C, Letterio JJ (2006) Smad4 signalling in T cells is required for suppression of gastrointestinal cancer. Nature 441: 1015–1019 [DOI] [PubMed] [Google Scholar]
- Kitadai Y, Sasaki T, Kuwai T, Nakamura T, Bucana CD, Fidler IJ (2006b) Targeting the expression of platelet-derived growth factor receptor by reactive stroma inhibits growth and metastasis of human colon carcinoma. Am J Pathol 169: 2054–2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitadai Y, Sasaki T, Kuwai T, Nakamura T, Bucana CD, Hamilton SR, Fidler IJ (2006a) Expression of activated platelet-derived growth factor receptor in stromal cells of human colon carcinomas is associated with metastatic potential. Int J Cancer 119: 2567–2574 [DOI] [PubMed] [Google Scholar]
- Kitamura T, Kometani K, Hashida H, Matsunaga A, Miyoshi H, Hosogi H, Aoki M, Oshima M, Hattori M, Takabayashi A, Minato N, Taketo MM (2007) SMAD4-deficient intestinal tumors recruit CCR1+ myeloid cells that promote invasion. Nat Genet 39: 467–475 [DOI] [PubMed] [Google Scholar]
- Kosinski C, Li VS, Chan AS, Zhang J, Ho C, Tsui WY, Chan TL, Mifflin RC, Powell DW, Yuen ST, Leung SY, Chen X (2007) Gene expression patterns of human colon tops and basal crypts and BMP antagonists as intestinal stem cell niche factors. Proc Natl Acad Sci USA 104: 15418–15423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koukourakis MI, Giatromanolaki A, Harris AL, Sivridis E (2006) Comparison of metabolic pathways between cancer cells and stromal cells in colorectal carcinomas: a metabolic survival role for tumor-associated stroma. Cancer Res 66: 632–637 [DOI] [PubMed] [Google Scholar]
- Ling KL, Pratap SE, Bates GJ, Singh B, Mortensen NJ, George BD, Warren BF, Piris J, Roncador G, Fox SB, Banham AH, Cerundolo V (2007) Increased frequency of regulatory T cells in peripheral blood and tumour infiltrating lymphocytes in colorectal cancer patients. Cancer Immunol 7: 7. [PMC free article] [PubMed] [Google Scholar]
- Lizee G, Radvanyi LG, Overwijk WW, Hwu P (2006) Improving antitumor immune responses by circumventing immunoregulatory cells and mechanisms. Clin Cancer Res 12: 4794–4803 [DOI] [PubMed] [Google Scholar]
- Mishra L, Shetty K, Tang Y, Stuart A, Byers SW (2005) The role of TGF-beta and Wnt signaling in gastrointestinal stem cells and cancer. Oncogene 24: 5775–5789 [DOI] [PubMed] [Google Scholar]
- Monga SP, Mars WM, Pediaditakis P, Bell A, Mule K, Bowen WC, Wang X, Zarnegar R, Michalopoulos GK (2002) Hepatocyte growth factor induces Wnt-independent nuclear translocation of beta-catenin after Met-beta-catenin dissociation in hepatocytes. Cancer Res 62: 2064–2071 [PubMed] [Google Scholar]
- Mukaratirwa S, Koninkx JF, Gruys E, Nederbragt H (2005) Mutual paracrine effects of colorectal tumour cells and stromal cells: modulation of tumour and stromal cell differentiation and extracellular matrix component production in culture. Int J Exp Pathol 86: 219–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nateri AS, Spencer-Dene B, Behrens A (2005) Interaction of phosphorylated c-Jun with TCF4 regulates intestinal cancer development. Nature 437: 281–285 [DOI] [PubMed] [Google Scholar]
- Nishita M, Hashimoto MK, Ogata S, Laurent MN, Ueno N, Shibuya H, Cho KW (2000) Interaction between Wnt and TGF-beta signalling pathways during formation of Spemann's organizer. Nature 403: 781–785 [DOI] [PubMed] [Google Scholar]
- Orimo A, Weinberg RA (2006) Stromal fibroblasts in cancer: a novel tumor-promoting cell type. Cell Cycle 5: 1597–1601 [DOI] [PubMed] [Google Scholar]
- Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, Mlecnik B, Kirilovsky A, Nilsson M, Damotte D, Meatchi T, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Galon J (2005) Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med 353: 2654–2666 [DOI] [PubMed] [Google Scholar]
- Potten CS, Loeffler M (1990) Stem cells: attributes, cycles, spirals, pitfalls and uncertainties. Lessons for and from the crypt. Development 110: 1001–1020 [DOI] [PubMed] [Google Scholar]
- Powrie F (2004) Immune regulation in the intestine: a balancing act between effector and regulatory T cell responses. Ann NY Acad Sci 1029: 132–141 [DOI] [PubMed] [Google Scholar]
- Rakoff-Nahoum S, Medzhitov R (2007) Regulation of spontaneous intestinal tumorigenesis through the adaptor protein MyD88. Science 317: 124–127 [DOI] [PubMed] [Google Scholar]
- Rasola A, Fassetta M, De Bacco F, D’Alessandro L, Gramaglia D, Di Renzo MF, Comoglio PM (2007) A positive feedback loop between hepatocyte growth factor receptor and beta-catenin sustains colorectal cancer cell invasive growth. Oncogene 26: 1078–1087 [DOI] [PubMed] [Google Scholar]
- Sakamoto K, Tominaga Y, Yamauchi K, Nakatsu Y, Sakumi K, Yoshiyama K, Egashira A, Kura S, Yao T, Tsuneyoshi M, Maki H, Nakabeppu Y, Tsuzuki T (2007) MUTYH-null mice are susceptible to spontaneous and oxidative stress induced intestinal tumorigenesis. Cancer Res 67: 6599–6604 [DOI] [PubMed] [Google Scholar]
- Sivridis E, Giatromanolaki A, Koukourakis MI (2005) Proliferating fibroblasts at the invading tumour edge of colorectal adenocarcinomas are associated with endogenous markers of hypoxia, acidity, and oxidative stress. J Clin Pathol 58: 1033–1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein U, Arlt F, Walther W, Smith J, Waldman T, Harris ED, Mertins SD, Heizmann CW, Allard D, Birchmeier W, Schlag PM, Shoemaker RH (2006) The metastasis-associated gene S100A4 is a novel target of beta-catenin/T-cell factor signaling in colon cancer. Gastroenterology 131: 1486–1500 [DOI] [PubMed] [Google Scholar]
- Sullivan R, Graham CH (2007) Hypoxia-driven selection of the metastatic phenotype. Cancer Metastasis Rev 26: 319–331 [DOI] [PubMed] [Google Scholar]
- Tian YC, Phillips AO (2002) Interaction between the transforming growth factor-beta type II receptor/Smad pathway and beta-catenin during transforming growth factor-beta1-mediated adherens junction disassembly. Am J Pathol 160: 1619–1628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toualbi K, Guller MC, Mauriz JL, Labalette C, Buendia MA, Mauviel A, Bernuau D (2007) Physical and functional cooperation between AP-1 and beta-catenin for the regulation of TCF-dependent genes. Oncogene 26: 3492–3502 [DOI] [PubMed] [Google Scholar]
- van Es JH, Jay P, Gregorieff A, van Gijn ME, Jonkheer S, Hatzis P, Thiele A, van den Born M, Begthel H, Brabletz T, Taketo MM, Clevers H (2005) Wnt signalling induces maturation of Paneth cells in intestinal crypts. Nat Cell Biol 7: 381–386 [DOI] [PubMed] [Google Scholar]
- Yang L, Lin C, Liu ZR (2006) P68 RNA helicase mediates PDGF-induced epithelial mesenchymal transition by displacing Axin from beta-catenin. Cell 127: 139–155 [DOI] [PubMed] [Google Scholar]