Abstract
We hypothesized that neighborhood socioeconomic context would be most stronly associated with risk of myocardial infarction (MI) for smaller “neighborhood” definitions. We used data on 487 non-fatal, incident MI cases and 1,873 controls from a case-control study in Washington State. Census data on income, home ownership, and education were used to estimate socioeconomic context across four neighborhood definitions: one-kilometer buffer, block group, census tract, and ZIP code. No neighborhood definition led to consistently stronger associations with MI. Although we confirmed the association between neighborhood socioeconomic measures and risk of MI, we did not find these associations sensitive to neighborhood definition.
Keywords: Case-Control Studies, Education, Income, Myocardial Infarction, Poverty, Residence Characteristics, Socioeconomic Factors
Socioeconomic disparities in health have received increasing attention by researchers (Adler and Ostrove, 1999) and policy makers (Mackenbach and Bakker, 2003) in recent decades. Socioeconomic status (SES) has been posited to be a “fundamental cause” of health disparities (Phelan et al., 2004, Williams and Collins, 2001), such that the association between SES and health is created when higher status individuals or groups mobilize flexible resources, such as money and prestige, to avoid illness and death. There is also evidence from human and animal studies that psychosocial stress in response to relative social status contributes to mortality and disease for low status individuals (Wilkinson,1999, Steptoe and Marmot, 2002) and those living in more deprived areas (Elliott, 2000). Socioeconomic characteristics measured for individuals and areas have commonly included the domains of education, employment, occupational status, income, and material resources (Braveman et al., 2005, Krieger et al., 2002a, Carstairs, 2000). The questionnaires or other methods used to ascertain such characteristics differ across settings and studies (Krieger et al., 1997), and area-based socioeconomic characteristics have the additional complication of being measured at different scales or levels of aggregation (Pickett and Pearl, 2001).
In studies of neighborhood socioeconomic context and health, several scales of measurement are used without consensus as to which is most relevant. The modifiable areal unit problem, like the ecological fallacy, is a concern for such studies because study results may be sensitive to the selected measurement scale (Guagliardo, 2004, Dungan, 2002, Haynes et al., 2007). A geographic definition of neighborhood that is too vast might mask relevant variation and be subject to large scale residual confounding. On the other hand, a restrictive geographic definition could exclude from consideration hazards and resources in the broader environment that affect health and behavior. The hypothesized mediators of the association between neighborhood context and health may dictate which geographic scale is most relevant (Diez Roux, 2003). For example, social interactions may be supported by the characteristics of a small area, such as one’s block, whereas restaurants and stores across a larger area may provide access to healthy foods. Measuring the effect of socioeconomic context on health at different scales in a single study may help researchers to establish the plausibility of proposed mediators, interpret studies testing similar hypotheses at different scales, and engage in informed discussion about the utility of convenient neighborhood definitions.
Neighborhood socioeconomic context has commonly been measured for existing administrative areas (van Lenthe et al., 2005, Haynes et al., 2007), such as census or enumeration districts and postal codes; such administrative areas have different sizes in each country, and often have considerable variation in size by region within a single country. In the United States, neighborhood socioeconomic characteristics have most commonly been measured for census block groups or census tracts (Krieger et al., 1997), but United States Postal Service ZIP codes have been used as well (Davey Smith et al., 1996, Mobley et al., 2004, Philbin et al., 2000). Census block groups in the US contain approximately 1,000 residents, census tracts 4,000 residents, and ZIP codes 30,000 residents (Krieger et al., 2002a). A comparison to administrative units used in other countries may be useful, even though the correspondence is not exact: US census block groups are larger than very small units such as Canadian dissemination areas, British enumeration districts, or Australian collector’s districts; US census tracts correspond approximately to medium sized areas such as Canadian census tracts, British election wards and postcode sectors, or Dutch postcode sectors; and US ZIP codes correspond to larger areas such as Canadian census sub-divisions or Swedish parishes (Schuurman et al., 2007, Carstairs, 2000, Brameld and Holman, 2005, Pickett and Pearl, 2001, Reijneveld et al., 2000, Kolegard Stjarne et al., 2002, Stjarne et al., 2006). Alternatively, the area within a specified distance of each address has also been used as a neighborhood definition, especially in studies of specific health-related behaviors such as physical activity (Duncan and Mummery, 2005, Frank et al., 2005) or smoking (Chuang et al., 2005).
Despite variation in the measurement of socioeconomic characteristics across studies (Braveman et al., 2005), SES has a well documented relationship with health (Adler and Ostrove, 1999, Macintyre, 1997, Feinstein, 1993) and cardiovascular health in particular (Kaplan and Keil, 1993, Mensah, 2005, Davey Smith et al., 1998). An effect of neighborhood socioeconomic characteristics on cardiovascular disease risk has been documented even after adjusting for individual socioeconomic characteristics (Geronimus et al., 1996, Davey Smith et al., 1998, Sundquist et al., 1999, Diez Roux et al., 2001b, Steenland et al., 2004, Horne et al., 2004, Cubbin and Winkleby, 2005, Stjarne et al., 2006).
In this analysis, we investigated the strength of the neighborhood SES – incident myocardial infarction (MI) association across selected socioeconomic characteristics and neighborhood definitions. Five neighborhood socioeconomic characteristics were investigated: median household income (MHI), percentage below poverty level, percentage home ownership, percentage with a high school degree, and percentage with a college degree. Each of these measures was estimated for one kilometer radial buffers, census block groups, census tracts, and ZIP codes. We hypothesized that the strength of the neighborhood context association with risk of MI would differ among the four neighborhood definitions considered. We hypothesized that socioeconomic characteristic associations with risk of MI would be stronger for relatively restrictive neighborhood definitions (e.g. block group), compared with larger geographic definitions of neighborhood (e.g. ZIP code). A relationship between neighborhood size and contextual association strength could be due to individual socioeconomic effects captured more accurately with a local contextual effect; alternatively one’s immediate surroundings may have a particularly strong effect on stress, social support, health-related behaviors, and exposure to hazards independent of individual SES. We examined associations between measures of neighborhood context at different scales before and after accounting for the participants’ education, employment, and household income.
MATERIALS AND METHODS
Study setting and population
We used data from a population-based case-control study within Group Health (GH), a large health maintenance organization in western Washington State. This case-control study (Koepsell and Weiss, 2003) collected information from medical records, telephone interviews, and a computerized pharmacy database. This study included all incident MI cases, as well as controls frequency-matched to cases on age (by decade), sex, treated hypertension status, and calendar year. Incidence density sampling was used to ensure that the odds ratios would be good estimates of the corresponding risk ratios. All subjects included in this analysis completed a telephone interview, were ages 30 to 79, and were selected as a case or control between 1995 and 2001. The study proposal and consent procedures were reviewed and approved by the GH Human Subjects Review Committee.
Cardiovascular event ascertainment
Potential MI cases were identified from the computerized discharge diagnostic codes from the GH hospitals, Washington State death tapes, and claims databases, which include bills for all services provided by non-GH physicians or health care facilities. Trained medical abstractors confirmed all eligible, incident cases. We excluded 102 fatal cases from this analysis because ascertainment of key characteristics, including educational attainment and household income, was done by telephone interview after the MI event. Fatal and nonfatal cases did not differ significantly on any of the neighborhood socioeconomic characteristics considered (t-test p > 0.2 for each characteristic).
Addresses and geocoding
We obtained each subject’s address from the year before their selection as a case or control. Addresses came from GH end of year membership files. These addresses were linked only to a study identification number during the collection of data on neighborhood characteristics. The addresses and other geographic identifiers were removed before linking neighborhood data to health data in compliance with the requirements of the GH Human Subjects Research Committee.
We included subjects living in King, Kitsap, Pierce, Snohomish, and Thurston counties, all of which are in the Puget Sound metropolitan region of western Washington. Geocoding was done using enhanced Topologically Integrated Geographic Encoding and Referencing street maps and Maptitude software (Corporation, 2004). Ninety-seven percent of addresses were geocoded using automated processes, and an additional two percent were geocoded after being manually cleaned, for a final geocoding match rate of 99 percent. Participants were geocoded to 1,446 different census block groups, with a mean of two participants per block group; 651 different census tracts, with a mean of four per census tract; and 151 ZIP codes with a mean of 16 participants per ZIP code (Table 1). By definition, the one kilometer buffers were unique to each participant, although there was substantial overlap. We excluded participants without available address information or with only a Post Office box (n = 227), with addresses that we could not be geocoded (n = 12), and with addresses outside of the five-county study area (n = 140).
TABLE 1.
Comparison of neighborhood definitions
| Neighborhood | Number of areas with study participants | Mean (range) number of participants per area | ICC for MI status | 95% CI |
|---|---|---|---|---|
| One-kilometer buffer | 2,360 | 1* | N/A | N/A |
| Census block group | 1,446 | 2 (1 to 9) | 0.095 | 0.026, 0.164 |
| Census tract | 651 | 4 (1 to 17) | 0.058 | 0.020, 0.097 |
| ZIP code | 151 | 16 (1 to 55) | 0.013 | 0.000, 0.031 |
Each participant was within their own one-kilometer buffer, but these buffers were allowed to overlap
Notes: ICC indicates intraclass correlation coefficient; MI indicates myocardial infarction; CI indicates confidence interval
Census variables
Data on SES characteristics of census block groups and census tracts were taken from the 2000 census, including MHI, proportion of individuals below the federal poverty line, proportion of occupied housing units that were owner occupied, proportion of adults at least 25 years old with a high school education or higher, and proportion of adults at least 25 years old with a bachelor’s degree or higher.
For each participant, variables were created to describe neighborhood socioeconomic characteristics for each of the four potential neighborhood definitions (Figure 1). Variables for census block group and census tract characteristics were assigned uniformly to each participant residing in a given census block group or census tract. The approximate socioeconomic characteristics of the area within one kilometer of each residence (one-kilometer buffers) were calculated as weighted averages using the overlay feature in Maptitude (Corporation, 2004). For example, a subject might have 30 percent of their one-kilometer buffer in census block group A, and 70 percent in census block group B. The estimated MHI for the one-kilometer buffer would then be 0.3 * (MHI of A) + 0.7 * (MHI of B). Similarly, for the ZIP code definition we calculated the population-weighted average of all intersecting or contained census block groups.
Figure 1. Illustration of Selected Scales of Socioeconomic Context Measurement.
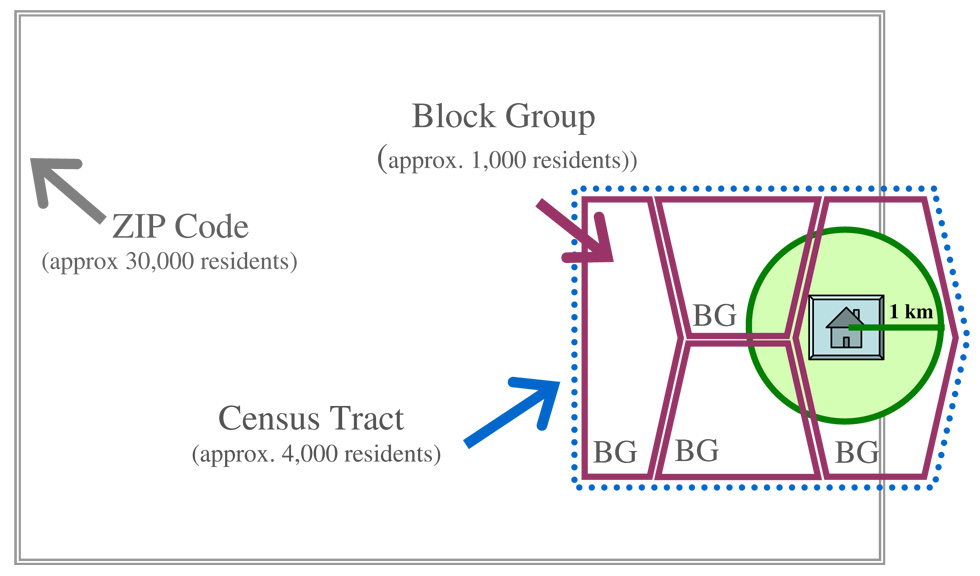
Four scales were considered for measurement of “neighborhood” socioeconomic characteristics. As illustrated here, ZIP codes were the largest area considered, with boundaries that do not necessarily correspond to the census area boundaries. Census tracts were divided into smaller census block groups. One-kilometer airline buffers were by definition circular and of a fixed size, while for other neighborhood definitions the shape and size varied.
Individual characteristics
An index date was available for each participant: the date of MI for cases and a random date in the same year for controls. Telephone interviews took place an average of two years after each participant’s index date. Approximately 78 percent of non-fatal cases and 76 percent of eligible, contacted controls agreed to participate in a telephone interview.
During the telephone interview, participants were asked to describe their health, health-related behaviors, and SES immediately prior to their index date. Questions covering marital status, race, education (seven categories), annual household income (seven categories), and employment status were based on questions from the Behavioral Risk Factor Surveillance System questionnaire (CDC, 2005). Leisure-time physical activity questions were derived from the Minnesota Leisure-Time Activity questionnaire (Taylor et al., 1978, Lemaitre et al., 1995). Subjects reported the frequency and duration of their participation in 26 types of physical activity during the month before their index date (Lemaitre et al., 1995). Participants were also asked to categorize their health as excellent, very good, good, fair, or poor. Additional questions covered current smoking, alcohol consumption, and aspirin use.
Data on prior cardiovascular disease and cardiovascular risk factors were abstracted from participants’ medical records. We excluded subjects with a documented history of MI, stroke, congestive heart failure or angina prior to their index date to limit the possibility of confounding by prior cardiovascular disease. Professional abstractors also recorded the most recent resting heart rate, high-density lipoprotein (HDL) and total cholesterol levels, and weight before each participant’s index date. To calculate body mass index (BMI), most recent weight was used with adult height. Diagnoses in the medical record were used to classify participants as having treated hypertension or diabetes.
Statistical analysis
Intraclass correlation coefficients (ICCs) were used to assess variation in MI risk between versus within the different neighborhood definitions. These ICCs can be interpreted as the maximum proportion of variation in MI risk explained at each neighborhood level. If risk was strongly correlated within neighborhoods, the only variation would be between neighborhoods and the ICC would be close to 1.0. In contrast, if MI cases and controls were randomly distributed through the study area, most variation would be within the neighborhoods and the ICC would be close to zero. Unadjusted ICCs were calculated using the ANOVA estimator in STATA 8.2 (StataCorp, 2003). Matching variable adjusted ICCs were calculated in a parallel fashion using the mean squared errors from multi-variable models with and without neighborhood indicator variables. Although the ANOVA ICC estimator is generally intended for use with normally distributed variables, its use for binary variables is asymptotically valid and unbiased (Ridout et al., 1999).
Covariance among neighborhood socioeconomic characteristics was evaluated using Pearson product-moment correlation coefficients. For each neighborhood definition and socioeconomic characteristic, we created quartiles based on the distribution among controls.
Logistic models with quartiles of neighborhood socioeconomic characteristics were constructed for the different potential neighborhood definitions using robust variance estimates, adjusting for matching variables (age, sex, hypertension status, and calendar year) and individual demographic characteristics (race and marital status). We also created models with further adjustment for socioeconomic characteristics (education, employment status, and household income) and then cardiovascular risk factors (smoking, treated diabetes, family history of coronary heart disease, heart rate, total and high-density lipoprotein cholesterol, systolic and diastolic blood pressure, and body mass index) that could mediate or confound the association of interest. Quartile odds ratios were estimated using indicator variables, with the highest SES quartile as the reference. Pseudo r-squared values from these models were presented as indicators of model fit; a higher pseudo r-squared would indicate that a model fit the data more closely.
Missing data on individual characteristics, including education (less than one percent), employment status (less than one percent), marital status (less than one percent), race (three percent), and income (10 percent), were filled in by multiple imputation. We imputed the data five times using switching regression; resulting confidence intervals reflect uncertainty due to missing data (Royston, 2004). Multiple imputations and all regression models and were run in STATA 8.2 (StataCorp, 2003).
RESULTS
Our final sample included 2,360 participants with addresses throughout the five-county study area (Figure 2). The average age was 64 and more than 90 percent of the participants were white (Table 2). Characteristics of cases and controls differed as expected.
Figure 2. Study Addresses and Socioeconomic Characteristics in the Puget Sound Region of Washington State.
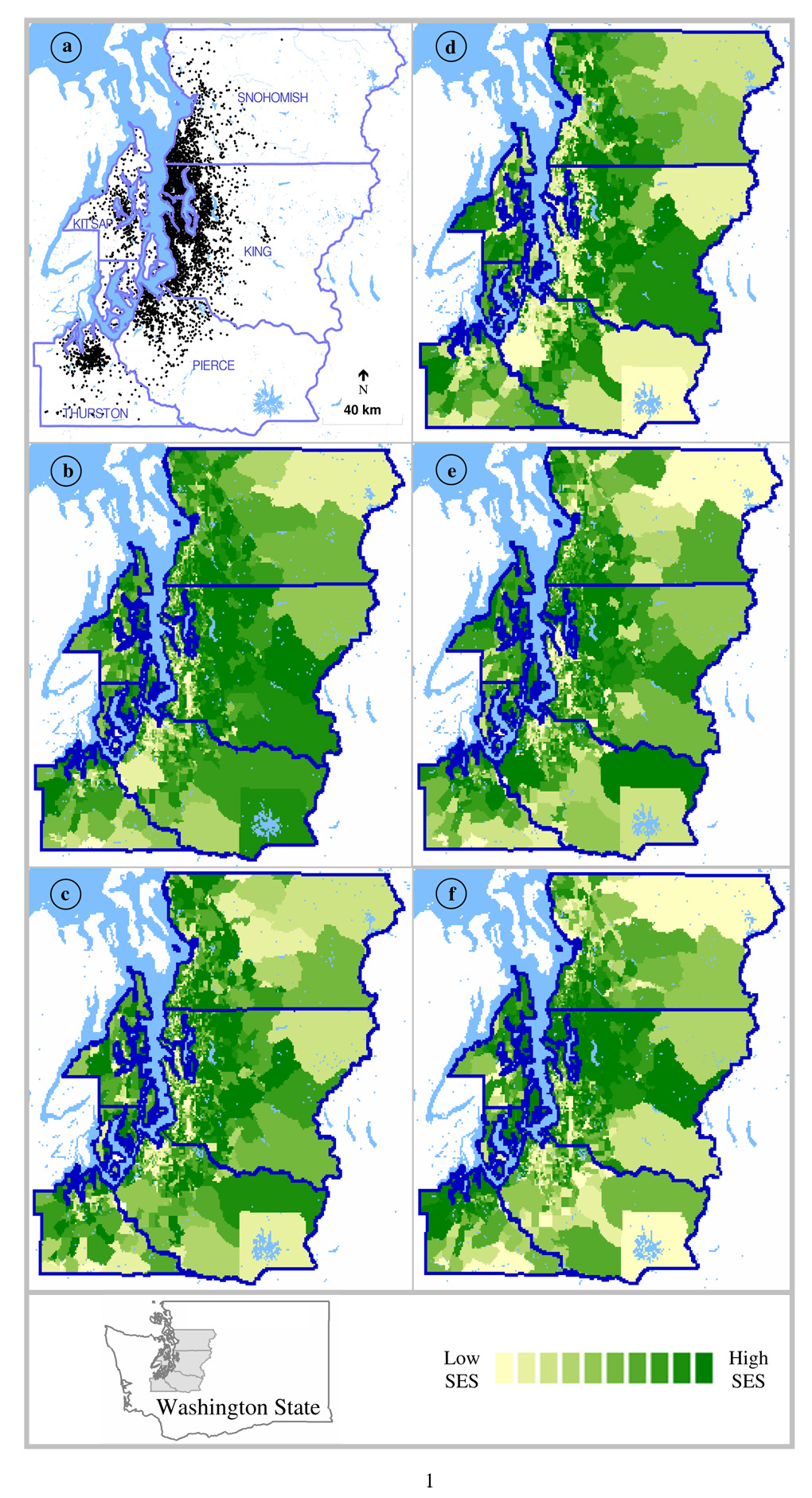
Address locations (a) have been jittered to protect participant confidentiality; median household income (b), proportion of individuals below the federal poverty line (c), proportion of homes that were owner-occupied (d), proportion of adults who graduated from high school (e) and proportion of adults who graduated from college (f) are shown for census block groups, with darker shades indicate census block groups with higher socioeconomic status (higher median household income, less poverty, more home ownership, higher educational attainment), approximately equal area for each of 10 shades
TABLE 2.
Participant characteristics for myocardial infarction cases and controls
| mean (SD) or percent | ||
|---|---|---|
| cases N = 487 | controls N = 1,873 | |
| Matching Variables | ||
| Age, years | 64(10) | 64(10) |
| Female sex | 63% | 61% |
| Treated hypertension | 64% | 70% |
| Socioeconomic characteristics | ||
| White race | 92% | 90% |
| Retired | 46% | 46% |
| Employed | 40% | 42% |
| Low income(<$20,000) | 22% | 15% |
| College education | 58% | 64% |
| Marital status | 64% | 68% |
| Health-related behaviors | ||
| Amount LTPA if any (hours/wk) | 6.0(5.7) | 7.2(6.5) |
| Any LTPA | 84% | 88% |
| Any aspirin use | 49% | 59% |
| Any alcohol consumption | 61% | 72% |
| Current smoker | 22% | 11% |
| Health indicators | ||
| Self-reported health good or better | 75% | 86% |
| Diabetes mellitus | 18% | 10% |
| Obesity (BMI≥30) | 43% | 39% |
| Adult height (m) | 1.7 (0.1) | 1.7 (0.1) |
| HDL cholesterol | 49 (16) | 54 (17) |
| Heart rate (bpm) | 77 (12) | 75 (12) |
| Total cholesterol | 237 (46) | 223 (40) |
Notes: LTPA indicates leisure-time physical activity; BMI, body mass index; bpm, beats per minute; HDL, high-density lipoprotein; SD, standard deviation
Myocardial infarction status ICCs indicated a detectable spatial pattern, with approximately ten percent of the variation at the census block group level and six percent at the census tract level (Table 1). Correlation in MI status was not detectable within ZIP codes, as shown by an ICC confidence interval that includes zero. After adjusting for matching variables, the ICCs for the census block groups, census tracts, and ZIP codes were slightly increased: 0.104, 0.065, and 0.015, respectively.
Depending on neighborhood definition, controls had a median neighborhood MHI of $54 to $56 thousand per year; a median of five to seven percent of neighborhood residents below the federal poverty line; a median of 63 to 78 percent owner occupancy in their neighborhood; a median of 91 to 93 percent high school graduation in their neighborhood; and a median of 34 percent college degree attainment in their neighborhood (Table 3). The neighborhood socioeconomic characteristics were correlated with each other in the expected direction, except for the negative correlation found between owner occupancy and college degree attainment at the ZIP code level (Table 3). Positive correlations ranged from 0.08 to 0.78. Correlations between college degree attainment and poverty or owner occupancy, and between high school graduation and owner occupancy, were consistently the lowest.
TABLE 3.
Neighborhood socioeconomic characteristics in controls
| One-kilometer buffer | |||||
|---|---|---|---|---|---|
| MHI | Poverty | Homes owned | High school | College | |
| Median | $56K | 6% | 71% | 91% | 34% |
| (IQ range) | ($47K, $66K) | (4%, 9%) | (58%, 83%) | (88%, 95%) | (22%, 48%) |
| Correlation with | |||||
| MHI | 1.00 | ||||
| Poverty | 0.71 | 1.00 | |||
| Homes owned | 0.67 | 0.68 | 1.00 | ||
| High school | 0.65 | 0.65 | 0.33 | 1.00 | |
| College | 0.63 | 0.35 | 0.08 | 0.72 | 1.00 |
| Census block group | |||||
| MHI | Poverty | Homes owned | High school | College | |
| Median | $56K | 5% | 78% | 93% | 34% |
| (IQ range) | ($45K, $69K) | (3%, 9%) | (57%, 88%) | (87%, 96%) | (21%, 49%) |
| Correlation with | |||||
| MHI | 1.00 | ||||
| Poverty | 0.61 | 1.00 | |||
| Homes owned | 0.66 | 0.60 | 1.00 | ||
| High school | 0.55 | 0.54 | 0.30 | 1.00 | |
| College | 0.60 | 0.34 | 0.14 | 0.66 | 1.00 |
| Census tract | |||||
| MHI | Poverty | Homes owned | High school | College | |
| Median | $54K | 6% | 70% | 92% | 34% |
| (IQ range) | ($46K, $65K) | (4%, 9%) | (56%, 83%) | (88%, 95%) | (23%, 48%) |
| Correlation with | |||||
| MHI | 1.00 | ||||
| Poverty | 0.72 | 1.00 | |||
| Homes owned | 0.70 | 0.66 | 1.00 | ||
| High school | 0.63 | 0.63 | 0.30 | 1.00 | |
| College | 0.58 | 0.34 | 0.08 | 0.72 | 1.00 |
| ZIP code | |||||
| MHI | Poverty | Homes owned | High school | College | |
| Median | $54K | 7% | 63% | 91% | 34% |
| (IQ range) | ($47K, $62K) | (5%, 10%) | (57%, 74%) | (88%, 94%) | (23%, 47%) |
| Correlation with | |||||
| MHI | 1.00 | ||||
| Poverty | 0.78 | 1.00 | |||
| Homes owned | 0.56 | 0.67 | 1.00 | ||
| High school | 0.67 | 0.67 | 0.20 | 1.00 | |
| College | 0.62 | 0.33 | −0.09 | 0.74 | 1.00 |
Notes: IQ indicates interquartile; MHI indicates median household income for the given neighborhood definition, in thousands; poverty, percent of neighborhood residents above the federal poverty line; home owned, percent of neighborhood homes that are owner occupied; high school, percent of neighborhood residents over the age of 25 who have graduated from high school; college, percent of neighborhood residents over the age of 25 who have a college degree; Pearson correlation coefficients are shown, all are significantly different from zero (p < 0.001); N = 1,873 controls
Socioeconomic characteristics were also correlated across different neighborhood definitions, with correlations ranging from 0.46 to 0.95 (Table 4). Proportion with a college degree had the highest correlations across neighborhood definitions. For each socioeconomic characteristic, the highest correlation was between estimates for the one-kilometer buffer and for the census tract. This was true also for the subset within the most densely populated county (King County). In the other four counties, median household income and educational characteristics were just as highly correlated between the one-kilometer buffer and census block group definitions as between one-kilometer buffers and census tracts. The estimated population within a single one kilometer buffer ranged from 13 to 13,000 residents (interquartile range: 1,216 to 2,911 residents), suggesting that the one kilometer buffer had a variable relationship to the other neighborhood definitions, but was usually intermediate between census block groups and census tracts (Figure 1).
TABLE 4.
Correlations between neighborhood socioeconomic characteristics measured at different levels among controls
| Median Household Income | ||||
|---|---|---|---|---|
| One-km buffer | Census block group | Census tract | ZIP code | |
| Correlation with | ||||
| One-km buffer | 1.00 | |||
| Census block group | 0.83 | 1.00 | ||
| Census tract | 0.86 | 0.79 | 1.00 | |
| ZIP code | 0.72 | 0.57 | 0.69 | 1.00 |
| Percent Below Poverty | ||||
| One-km buffer | Census block group | Census tract | ZIP code | |
| Correlation with | ||||
| One-km buffer | 1.00 | |||
| Census block group | 0.70 | 1.00 | ||
| Census tract | 0.79 | 0.66 | 1.00 | |
| ZIP code | 0.67 | 0.46 | 0.66 | 1.00 |
| Home Ownership | ||||
| One-km buffer | Census block group | Census tract | ZIP code | |
| Correlation with | ||||
| One-km buffer | 1.00 | |||
| Census block group | 0.77 | 1.00 | ||
| Census tract | 0.82 | 0.75 | 1.00 | |
| ZIP code | 0.62 | 0.46 | 0.58 | 1.00 |
| High School Graduation | ||||
| One-km buffer | Census block group | Census tract | ZIP code | |
| Correlation with | ||||
| One-km buffer | 1.00 | |||
| Census block group | 0.84 | 1.00 | ||
| Census tract | 0.90 | 0.81 | 1.00 | |
| ZIP code | 0.82 | 0.66 | 0.81 | 1.00 |
| College Degree | ||||
| One-km buffer | Census block group | Census tract | ZIP code | |
| Correlation with | ||||
| One-km buffer | 1.00 | |||
| Census block group | 0.93 | 1.00 | ||
| Census tract | 0.95 | 0.92 | 1.00 | |
| ZIP code | 0.90 | 0.83 | 0.90 | 1.00 |
Notes: Pearson correlation coefficients are shown, all are significantly different from zero (p < 0.001); N = 1,873 controls
Neighborhood socioeconomic characteristics were associated with risk of MI before (Figure 3) and after (Figure 4) adjustment for individual and household socioeconomic characteristics. Education-based neighborhood measures, especially percent of residents with a college degree, had stronger and more consistent associations with MI risk than income-based and home-ownership measures. Extreme quartiles of college degree attainment had significantly different MI risk regardless of the neighborhood level considered, and odds ratios for the intermediate quartiles of college degree attainment were most suggestive of a linear trend. In contrast, extreme quartiles of owner occupancy were significantly different only for the census tract level. The pseudo r-squared values were slightly higher for models using college degree attainment, as compared with other neighborhood socioeconomic characteristics, to predict risk of MI. For the corresponding models without neighborhood socioeconomic characteristics, the pseudo r-squared was 0.016 when only matching and demographic variables were included and 0.033 with the addition of individual socioeconomic characteristics. There was no clear pattern showing stronger associations for a particular neighborhood definition.
Figure 3. Odds Ratios for Myocardial Infarction by Quartiles of Neighborhood Socioeconomic Characteristics.
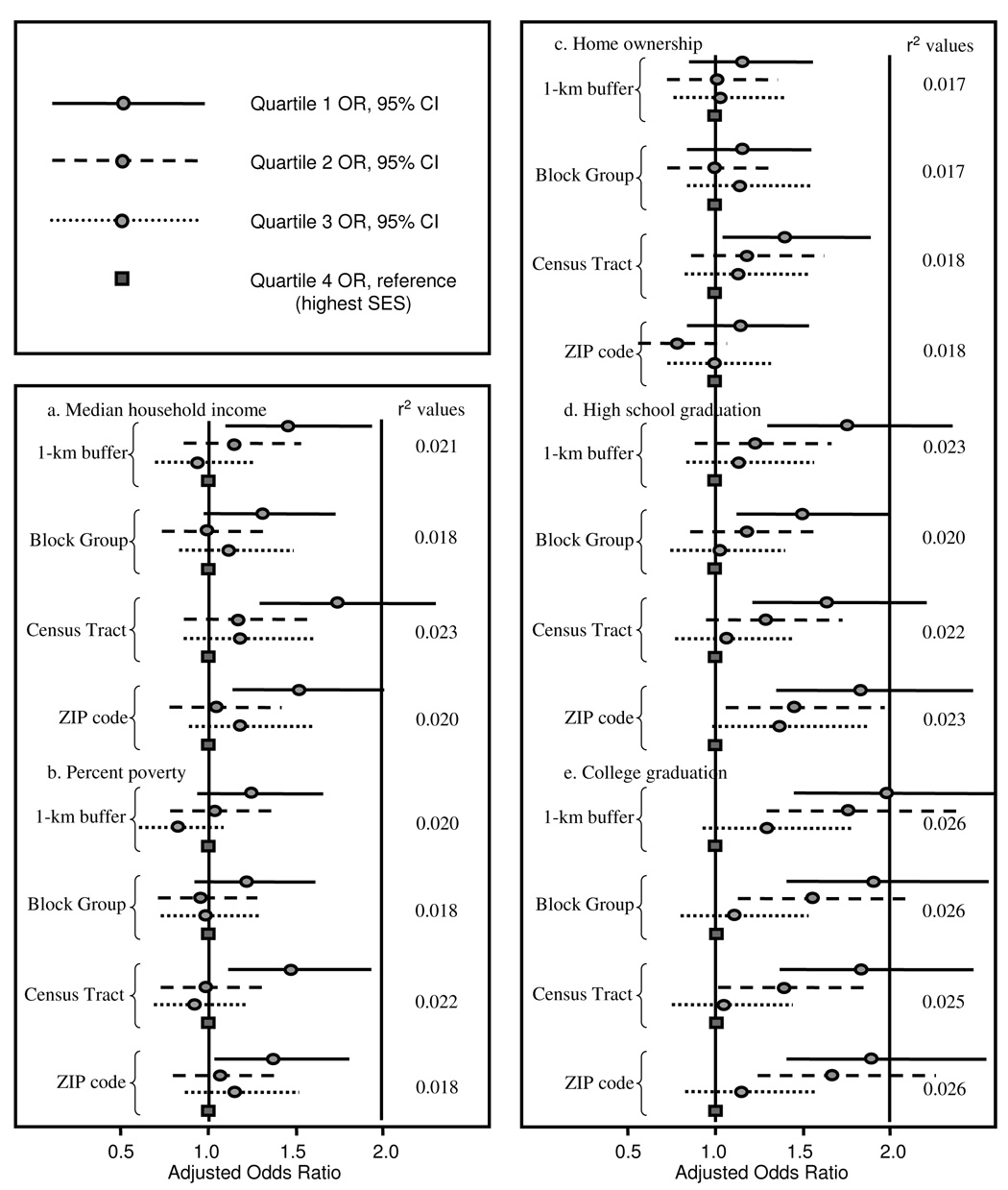
Models were adjusted for matching variables (age, sex, hypertension status, calendar year) and demographic characteristics (marital status, and race); pseudo r-squared values for these logistic regression models are shown
Figure 4. Odds Ratios for Myocardial Infarction by Quartiles of Neighborhood Socioeconomic Characteristics Adjusted for Individual Socioeconomic Characteristics.
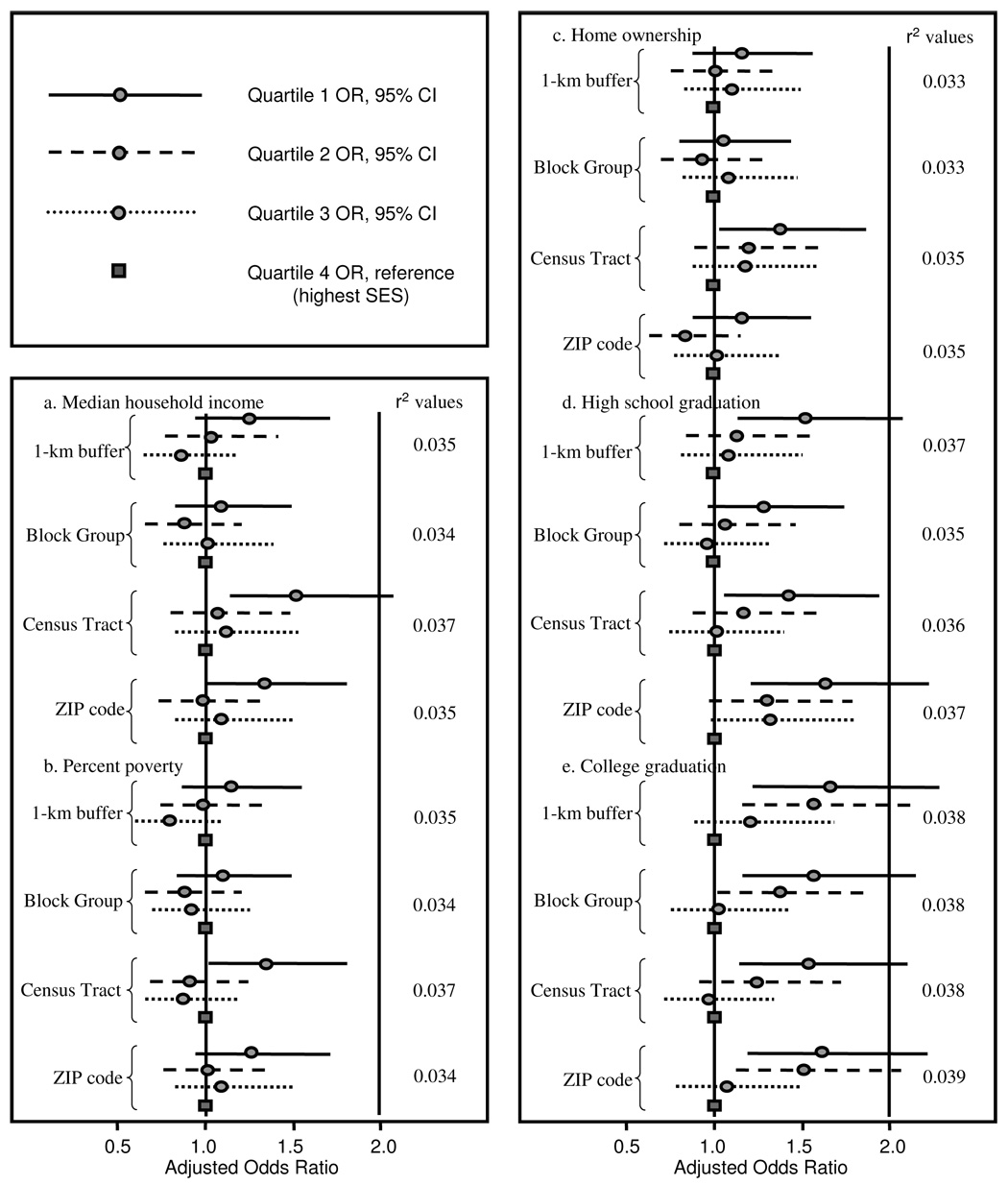
Models were adjusted for matching variables (age, sex, hypertension status, calendar year) and individual socioeconomic/demographic characteristics (household income, education, employment/retirement status, marital status, and race); pseudo r-squared values for these logistic regression models are shown
After further adjustment for cardiovascular risk factors that could mediate the relationship between neighborhood SES and risk of MI, odds ratios comparing extreme quartiles of neighborhood socioeconomic characteristics were attenuated toward one. Both education related measures remained statistically significant at the ZIP code level and college degree attainment remained significant for the one kilometer buffer; however, measurement error may have led to incomplete adjustment.
Associations between neighborhood socioeconomic characteristics and MI risk were similar for a complete case analysis of the 2,063 participants without missing data. Restricting the sample to 1,677 participants who had lived at the same address for five years produced similar patterns and point estimates, but wider confidence intervals.
DISCUSSION
In this Washington State case-control study, we confirmed that neighborhood socioeconomic characteristics significantly predicted MI risk after adjustment for individual SES indicators and demographic characteristics. Neighborhood socioeconomic characteristics were moderately correlated across domains, and the correlations of the same measure across neighborhood definitions were moderate to strong. Education-based measures were the strongest and most consistent predictors of MI risk, followed by income and poverty measures. Owner occupancy rates were not consistently associated with MI risk. Contrary to our hypothesis, associations between neighborhood SES and risk of MI were found to be similar for all neighborhood definitions: one-kilometer buffers, census block groups, census tracts, and ZIP codes. We hypothesized that the block group definition would yield the strongest associations, but we did not observe any trends in that direction.
The scale of measurement for area-based socioeconomic indicators has been empirically evaluated using different criteria to judge optimality. As in our study, some research has previously investigated whether associations between area characteristics and health are stronger for theoretically better scales of measurement. Several such studies have reported stronger health effects for characteristics measured at a smaller level within the range being considered here (Hyndman et al., 1995, Krieger et al., 2002a, Franzini and Spears, 2003, Schuurman et al., 2007), while others have reported that results were similar across neighborhood definitions (Davey Smith et al., 1998, Diez Roux et al., 2001a, Fiscella and Franks, 2001, Thomas et al., 2006, Berke et al., 2007). In particular, while the use of US ZIP codes has been critiqued because of their instability over time, variability in size, and lack of correspondence with other political, statistical or administrative boundaries (Krieger et al., 2002b), others have recommended ZIP codes for ease of use (Fiscella and Franks, 2001). Variation in the evidence on whether the effect of neighborhood socioeconomic context on health is sensitive to the neighborhood definition may stem from differences in populations, individual characteristic measurement, geographic setting, and outcome among these studies (Pickett and Pearl, 2001). Our results showed neighborhood SES-MI associations at the ZIP code level that were similar to those at the census tract and census block group levels, suggesting little sensitivity to the neighborhood definition. Further, we did not find that using estimates for a one-kilometer buffer area to deal with border effects provided a detectable advantage over census areas; the weighted socioeconomic measures for one-kilometer buffers were highly correlated with census tract measures.
Importantly, however, there are other criteria by which one could choose the “best” scale for measurement. An optimal scale might correspond with participants’ subjective neighborhood boundaries, such that perceived neighborhood characteristics are well approximated (Diez Roux, 2001). Studies have reported that perceived and measured features are most highly correlated within small areas, such as one kilometer radial buffers (Moudon et al., 2006, Duncan and Mummery, 2005) or zones with 500 residents (Haynes et al., 2007). Investigators have also invited participants to draw their own neighborhood boundaries (Coulton et al., 2001), an approach that may prove important for understanding how people think about the place in which they live. However, the observable heterogeneity in perception offers a crucial challenge for researchers hoping to implement uniform measures. Yet another approach to selecting neighborhood scale might be based on the potential for intervention or the scale at which relevant service provision and regulatory decisions are made (Diez Roux, 2001). Areas related to health care provision or subject to funding constraints and collective action (community boards or townships) might be preferred for applied research, if the research findings are meant to inform actions at that level. While our study, along with others (Davey Smith et al., 1998, Diez Roux et al., 2001a, Fiscella and Franks, 2001, Thomas et al., 2006, Berke et al., 2007), suggests that the relationships between area-based socioeconomic characteristics and health may be robust to scale of measurement, theoretical or practical arguments should still be considered in study design. On the other hand, researchers and stakeholders might find studies like ours reassuring when logistics or confidentiality necessitates the selection of a relatively coarse scale of measurement.
Research on the effect of neighborhood deprivation on mortality has documented smaller effects for education-based measures than for economic measures of neighborhood deprivation in the US (Krieger et al., 2003, Geronimus and Bound, 1998). In contrast, we found the strongest, most graded, most consistent associations when neighborhood level measures of educational attainment, especially college degree attainment, were used to predict risk of MI. This contrast may be due in part to the education-based measures used: while Krieger and colleagues used a measure of low education, percent of residents not completing high school, we found more consistent associations for a measure of higher education, percent with a college degree, than for percent completing high school. When comparing our findings with other work, differences may arise from the narrow variation in neighborhood socioeconomic characteristics for western Washington State, and for our health maintenance organization-based population in particular. The extreme quartiles for percent of residents completing high school, for example, were less than 87 percent versus more than 96 percent in our study compared with less than 60 percent versus more than 85 percent in the study by Krieger (Krieger et al., 2003). The relative level of neighborhood educational attainment may be better captured by different measures in these two studies because of differences in the distributions. There may also be a threshold level of neighborhood educational attainment needed to marshal resources, sustain social support, and avoid hazards. Further work should consider the effect of neighborhood deprivation across geographic regions of the US and in other settings (Pickett and Pearl, 2001).
The neighborhood environment may play a role in mediating the effect of SES on health (Schulz et al., 2005, Adler and Ostrove, 1999), and may further offer opportunities for developing and targeting interventions to reduce health disparities. Low SES neighborhoods may affect cardiovascular risk because of exposure to hazards in the environment, such as air pollution (Kunzli et al., 2005, Miller et al., 2007), through supporting or impeding health-related behaviors (Cubbin and Winkleby, 2005), such as smoking (Chuang et al., 2005), diet (Morland et al., 2002), and physical activity (Ewing, 2005), or through social support and stress (Elliott, 2000). The scale of neighborhood measurement may be an important consideration as these processes continue to be studied, and as interventions are developed, targeted and tested. However, the results presented here suggest that some associations may be robust to different scales of measurement. Measurement across larger areas may sacrifice specificity in favor of stability, so that the robustness is a convenient numerical phenomenon, or neighborhood SES measurement at different scales may in fact be capturing multiple constructs and exposure patterns which are distinct but have similar relevance for cardiovascular health.
Limitations
We considered only four possible neighborhood definitions. The modifiable areal unit problem, which concerns both scale and boundary selection components (Jelinski, 1996), was not explored systematically for this study. Instead, we compared neighborhood definitions that might practically be considered as alternatives in a large study, and used census data as the basis for our neighborhood characteristics. These alternatives allowed us to simultaneously consider scale and boundary selection, but not to isolate their effects. Future research could examine alternative neighborhoods of the same size in order to systematically assess zoning effects, or use simple buffers of increasing radius to assess scale effects. Although not considered in the present study, systematic zone design could also be considered as a way to address the modifiable areal unit problem in studies of health (Cockings and Martin, 2005, Haynes et al., 2007).
Some additional limitations of our study should be taken into account when interpreting the findings. This study was observational, allowing for the possibility of residual confounding. Data on individual SES came from telephone interviews and may be subject to recall bias and social desirability bias. Residual individual level variation remains a possible explanation for the “independent” influence of neighborhood SES (Steenland et al., 2004). We did not include fatal MI cases or those refusing an interview. Even among those completing a telephone interview, we had missing data for some characteristics, such as household income and employment status, which were imputed under the assumption that these were non-informative missing data (Raghunathan, 2004). Further, we collected data on income, employment and education, but did not collect information on other socioeconomic domains such as wealth. We cannot exclude the possibility that neighborhood socioeconomic measures were associated with risk of MI were due to unmeasured variation in individual SES. The neighborhood socioeconomic characteristics considered here were correlated with each other, but represented several major domains of SES. Other domains such as occupational class (Krieger et al., 1997) and unemployment (van Lenthe et al., 2005) were not addressed in this study. Finally, the geographic span and characteristics of our sample limit the generalizability of our findings.
Conclusion
We found that selected census-based neighborhood socioeconomic characteristics predicted MI risk after adjustment for individual SES indicators. Contrary to our hypothesis, this association did not appear to be stronger when characteristics were estimated for smaller neighborhood definitions. Instead, the association was robust for the neighborhood definitions considered. The association did, however, appear stronger for education-based neighborhood characteristics, as compared with characteristics based on income or home ownership.
Further studies of neighborhood socioeconomic context measured at different scales may help to clarify how socioeconomic context shapes health. If our finding of robustness to neighborhood definition is replicated across other geographic areas and study populations, plausible explanations of socioeconomic context effects would need to operate at a range of scales without much attenuation. Future research should investigate the ways that socioeconomic health disparities across neighborhoods are generated and sustained, as well as ways to reduce these disparities.
Acknowledgments
This research was supported by a University of Washington Royalty Research Fund Award, and by grands R01-HL043201, R01-HL068639, and T32-HL07902 from the National Heart, Lung, and Blood Institute, and grant R01-AG09556 from the National Institute on Aging. GSL, a Health and Society Scholar at Columbia University, thanks the Robert Wood Johnson Foundation’s Health & Society Scholars Program for its financial support.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Gina S. Lovasi, Columbia University, Institute of Social and Economic Research and Policy gl2225@columbia.edu
Anne Vernez Moudon, University of Washington, Urban Design & Planning, Architecture, Landscape Architecture moudon@u.washington.edu.
Nicholas L. Smith, University of Washington, Department of Epidemiology nlsmith@u.washington.edu
Thomas Lumley, University of Washington, Department of Biostatistics tlumley@u.washington.edu.
Eric B. Larson, Group Health Cooperative, Center for Health Studies ebl@u.washington.edu
Dong W Sohn, University of Washington, Urban Design & Planning, Architeture, Landscape Architecture dwsohn@krihs.re.kr.
David S Siscovick, University of Washington, Departments of Epidemiology and Medicine dsisk@u.washington.edu.
Bruce M Psaty, University of Washington, Departments of Epidemiology, Medicine, and Health Services psaty@u.washington.edu.
References
- Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Berke EM, Gottlieb LM, Moudon AV, Larson EB. Protective association between neighborhood walkability and depression in older men. J Am Geriatr Soc. 2007;55:526–533. doi: 10.1111/j.1532-5415.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- Brameld KJ, Holman CD. The effect of locational disadvantage on hospital utilisation and outcomes in Western Australia. Health Place. 2005 doi: 10.1016/j.healthplace.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Carstairs V. Socio-economic factors at areal level and their relationship with health. In: Elliott P, Wakefield J, Best N, Briggs D, editors. Spatial Epidemiology: Methods and Applications. New York: Oxford University Press; 2000. [Google Scholar]
- CDC. United States Department of Health and Human Services; 2005 doi: 10.3109/15360288.2015.1037530. http://www.cdc.gov/brfss/questionnaires/english.htm. [DOI] [PubMed]
- Chuang YC, Cubbin C, Ahn D, Winkleby MA. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J Epidemiol Community Health. 2005;59:568–573. doi: 10.1136/jech.2004.029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockings S, Martin D. Zone design for environment and health studies using pre-aggregated data. Soc Sci Med. 2005;60:2729–2742. doi: 10.1016/j.socscimed.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Corporation C. Maptitude. 4.7 ed. Massachusetts: Newton; 2004. [Google Scholar]
- Coulton CJ, Korbin J, Chan T, Su M. Mapping residents' perceptions of neighborhood boundaries: a methodological note. Am J Community Psychol. 2001;29:371–383. doi: 10.1023/A:1010303419034. [DOI] [PubMed] [Google Scholar]
- Cubbin C, Winkleby MA. Protective and harmful effects of neighborhood-level deprivation on individual-level health knowledge, behavior changes, and risk of coronary heart disease. Am J Epidemiol. 2005;162:559–568. doi: 10.1093/aje/kwi250. [DOI] [PubMed] [Google Scholar]
- Davey Smith G, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley Study. J Epidemiol Community Health. 1998;52:399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey Smith G, Wentworth D, Neaton JD, Stamler R, Stamler J. Socioeconomic differentials in mortality risk among men screened for the Multiple Risk Factor Intervention Trial: II. Black men. Am J Public Health. 1996;86:497–504. doi: 10.2105/ajph.86.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Kiefe CI, Jacobs DR, JR, Haan M, Jackson SA, Nieto FJ, Paton CC, Schulz R. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001a;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001b;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Duncan M, Mummery K. Psychosocial and environmental factors associated with physical activity among city dwellers in regional Queensland. Prev Med. 2005;40:363–372. doi: 10.1016/j.ypmed.2004.06.017. [DOI] [PubMed] [Google Scholar]
- Dungan JL, P JN, Dale MRT, Legendre P, Citron-Pousty S, Fortin M-J, Jakomulska A, Miriti M, Rosenburg MS. A balanced view of scale in spatial statistical analysis. Ecography. 2002;25:626–640. [Google Scholar]
- Elliott M. The stress process in neighborhood context. Health Place. 2000;6:287–299. doi: 10.1016/s1353-8292(00)00010-1. [DOI] [PubMed] [Google Scholar]
- Ewing R. Can the physical environment determine physical activity levels? Exerc Sport Sci Rev. 2005;33:69–75. doi: 10.1097/00003677-200504000-00003. [DOI] [PubMed] [Google Scholar]
- Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q. 1993;71:279–322. [PubMed] [Google Scholar]
- Fiscella K, Franks P. Impact of patient socioeconomic status on physician profiles: a comparison of census-derived and individual measures. Med Care. 2001;39:8–14. doi: 10.1097/00005650-200101000-00003. [DOI] [PubMed] [Google Scholar]
- Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28:117–125. doi: 10.1016/j.amepre.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Franzini L, Spears W. Contributions of social context to inequalities in years of life lost to heart disease in Texas, USA. Soc Sci Med. 2003;57:1847–1861. doi: 10.1016/s0277-9536(03)00018-2. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples. Am J Epidemiol. 1998;148:475–486. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Neidert LJ. On the validity of using census geocode characteristics to proxy individual socioeconomic characteristics. Journal of the American Statistical Association. 1996;91:529–537. [Google Scholar]
- Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004;3:3. doi: 10.1186/1476-072X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes R, Daras K, Reading R, Jones A. Modifiable neighbourhood units, zone design and residents' perceptions. Health Place. 2007 doi: 10.1016/j.healthplace.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Horne BD, Muhlestein JB, Lappe DL, Renlund DG, Bair TL, Bunch TJ, Anderson JL. Less affluent area of residence and lesser-insured status predict an increased risk of death or myocardial infarction after angiographic diagnosis of coronary disease. Ann Epidemiol. 2004;14:143–150. doi: 10.1016/S1047-2797(03)00125-X. [DOI] [PubMed] [Google Scholar]
- Hyndman JC, Holman CD, Hockey RL, Donovan RJ, Corti B, Rivera J. Misclassification of social disadvantage based on geographical areas: comparison of postcode and collector's district analyses. Int J Epidemiol. 1995;24:165–176. doi: 10.1093/ije/24.1.165. [DOI] [PubMed] [Google Scholar]
- Jelinski DEW, J The modifiable areal unit problem and implications for landscape ecology. Landscape Ecology. 1996;11:129–140. [Google Scholar]
- Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Koepsell TD, Weiss NS. Epidemiologic Methods. New York: Oxford University Press, Inc; 2003. Case-control studies. [Google Scholar]
- Kolegard Stjarne M, Diderichsen F, Reuterwall C, Hallqvist J. Socioeconomic context in area of living and risk of myocardial infarction: results from Stockholm Heart Epidemiology Program (SHEEP) J Epidemiol Community Health. 2002;56:29–35. doi: 10.1136/jech.56.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health. 2003;93:1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002a;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas--the Public Health Disparities Geocoding Project. Am J Public Health. 2002b;92:1100–1102. doi: 10.2105/ajph.92.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Kunzli N, Jerrett M, Mack WJ, Beckerman B, Labree L, Gilliland F, Thomas D, Peters J, Hodis HN. Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect. 2005;113:201–206. doi: 10.1289/ehp.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaitre RN, Heckbert SR, Psaty BM, Siscovick DS. Leisure-time physical activity and the risk of nonfatal myocardial infarction in postmenopausal women. Arch Intern Med. 1995;155:2302–2308. [PubMed] [Google Scholar]
- Macintyre S. The Black Report and beyond: what are the issues? Soc Sci Med. 1997;44:723–745. doi: 10.1016/s0277-9536(96)00183-9. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Bakker MJ. Tackling socioeconomic inequalities in health: analysis of European experiences. Lancet. 2003;362:1409–1414. doi: 10.1016/S0140-6736(03)14639-9. [DOI] [PubMed] [Google Scholar]
- Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005;111:1332–1336. doi: 10.1161/01.CIR.0000158134.24860.91. [DOI] [PubMed] [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- Mobley LR, Finkelstein EA, Khavjou OA, Will JC. Spatial analysis of body mass index and smoking behavior among WISEWOMAN participants. J Womens Health (Larchmt) 2004;13:519–528. doi: 10.1089/1540999041281034. [DOI] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Moudon AV, Lee C, Cheadle AD, Garvin C, Johnson D, Schmid TL, Weathers RD, Lin L. Operational definitions of walkable neighborhood: theoretical and empirical insights. Journal of Physical Activity and Health. 2006;3:S99–S117. doi: 10.1123/jpah.3.s1.s99. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. "Fundamental causes" of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45:265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Philbin EF, Mccullough PA, Disalvo TG, Dec GW, Jenkins PL, Weaver WD. Socioeconomic status is an important determinant of the use of invasive procedures after acute myocardial infarction in New York State. Circulation. 2000;102:III107–III115. doi: 10.1161/01.cir.102.suppl_3.iii-107. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annu Rev Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- Reijneveld SA, Verheij RA, De Bakker DH. The impact of area deprivation on differences in health: does the choice of the geographical classification matter? J Epidemiol Community Health. 2000;54:306–313. doi: 10.1136/jech.54.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridout MS, Demetrio CG, Firth D. Estimating intraclass correlation for binary data. Biometrics. 1999;55:137–148. doi: 10.1111/j.0006-341x.1999.00137.x. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values. Stata Journal. 2004;4(3):227–241. [Google Scholar]
- Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen A, 3RD, James SA, House JS, Lepkowski J. Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environ Health Perspect. 2005;113:1817–1825. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurman N, Bell N, Dunn JR, Oliver L. Deprivation indices, population health and geography: an evaluation of the spatial effectiveness of indices at multiple scales. J Urban Health. 2007;84:591–603. doi: 10.1007/s11524-007-9193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STATACORP. Stata Statistical Software: Release 8.2. College Station, TX: Stata Corporation; 2003. [Google Scholar]
- Steenland K, Henley J, Calle E, Thun M. Individual- and area-level socioeconomic status variables as predictors of mortality in a cohort of 179,383 persons. Am J Epidemiol. 2004;159:1047–1056. doi: 10.1093/aje/kwh129. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Marmot M. The role of psychobiological pathways in socio-economic inequalities in cardiovascular disease risk. Eur Heart J. 2002;23:13–25. doi: 10.1053/euhj.2001.2611. [DOI] [PubMed] [Google Scholar]
- Stjarne MK, Fritzell J, De Leon AP, Hallqvist J. Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006;17:14–23. doi: 10.1097/01.ede.0000187178.51024.a7. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Malmstrom M, Johansson SE. Cardiovascular risk factors and the neighbourhood environment: a multilevel analysis. Int J Epidemiol. 1999;28:841–845. doi: 10.1093/ije/28.5.841. [DOI] [PubMed] [Google Scholar]
- Taylor HL, Jacobs DR, JR, Schucker B, Knudsen J, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- Thomas AJ, Eberly LE, Davey Smith G, Neaton JD. ZIP-code-based versus tract-based income measures as long-term risk-adjusted mortality predictors. Am J Epidemiol. 2006;164:586–590. doi: 10.1093/aje/kwj234. [DOI] [PubMed] [Google Scholar]
- Van Lenthe FJ, Borrell LN, Costa G, Diez Roux AV, Kauppinen TM, Marinacci C, Martikainen P, Regidor E, Stafford M, Valkonen T. Neighbourhood unemployment and all cause mortality: a comparison of six countries. J Epidemiol Community Health. 2005;59:231–237. doi: 10.1136/jech.2004.022574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. Ann N Y Acad Sci. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]


