Abstract
Objective
To investigate the financial burdens attributed to overweight and obesity on the U.S. health care system among elderly Americans.
Data Source
Longitudinal Cost and Use files of the Medicare Current Beneficiary Survey from 1992 to 2001.
Study Design
We constructed a simultaneous equation system to model the dynamic relationship between changes in body weight, chronic diseases, functional status, longevity, and health care expenditures using maximum likelihood estimation. Based on the estimation, we conducted a simulation of one cohort with different baseline weights at age 65 and followed to death or up to age 100 of their health outcomes and lifetime health care expenditures.
Principal Findings
The elderly men who were overweight or obese at age 65 had 6–13 percent more lifetime health care expenditures than the same age cohort within normal weight range at age 65. Elderly women who were overweight or obese at age 65 spent 11–17 percent more than those in a normal weight range. Both elderly men and women who were overweight or obese at age 65 had worse health outcomes than the normal weight cohorts. The average body mass index among survivors decreased by age.
Conclusion
Overweight and obesity could place significant financial burdens on the U.S. health care system.
Keywords: Obesity, dynamic, elderly
Approximately 35 percent of U.S. adults are overweight, and an additional 30 percent are obese (Flegal et al. 2002, 2004; Hedley et al. 2004). The increase in rates of overweight and obesity represents a major change in the biological and behavioral characteristics of the U.S. population, and has become a major focus of public health policy interventions (Ogden et al. 2006; Parikh et al. 2007). Because of the high prevalence of costly chronic diseases among the overweight and obese (e.g., diabetes, cancer), the epidemic of obesity could place heavy financial burdens on the U.S. health care system (Must et al. 1999). The central issues are, how much will this epidemic cost, and who will pay for it? (Finkelstein, Feibelkorn, and Wang 2003; Daviglus 2005; Lakdawalla, Goldman, and Shang 2005)
The magnitude of increase in health care expenditures associated with higher body weight differs by patient demographics, service type, and, more importantly, by health care payer. Among working adults, employer-provided health insurance and out-of-pocket payment by employees and their families are the major payers of health care. Previous research found that after controlling for educational achievement and work experiences, overweight and obese working adults are more likely to earn lower wages in the labor market relative to their normal weight peers. One major explanation for lower wages among the heavier adults is that they are more likely to suffer chronic diseases and/or related acute medical events that lead to more expensive medical bills to be paid by employer-provided insurance. Instead of raising the insurance premiums, employers are likely to shift the higher medical care cost to their heavier employees by offering lower wages in order to maintain actuarial fairness in insurance coverage (Cawley 2004; Bhattacharya and Bundorf 2005).
Among the elderly population, the major payers of health care are publicly financed health insurances. In 2003, for individuals 65 years and older, public health insurances (Medicare and Medicaid) payments accounted for approximately 62 percent of all health care payments (National Center for Health Statistics 2006). Unlike private insurance, Medicare and Medicaid cannot shift the higher health care expenditures associated with overweight or obesity to the heavier beneficiaries by increasing their premiums. Therefore, public funding (i.e., tax revenues) will bear the bulk of the financial burdens of higher health care expenditures associated with overweight or obesity among the elderly.
The majority of deaths in the United States occur after age 65. The elderly experience a comparatively faster rate of health deterioration, and have higher demand for health care than younger adults because of the natural aging process. From a public finance and policy point of view, what matters is not the extra health care expenditures among the heavier elderly per year, but their lifetime health care expenditures from age 65 to death. Previous research suggests that it is critically important to understand the dynamic relationship between bodyweight, the prevalence of chronic diseases, the development of functional disability, and longevity when investigating the health care expenditures associated with increased body weight among the elderly population. The higher health care expenditures among the overweight or obese elderly per year could be offset by their shorter life expectancy due to their higher mortality rates induced by the high prevalence of chronic diseases. Therefore, estimating cross-sectional relationships between body weight and health care expenditures could lead to overestimates of the financial burden of overweight or obesity (Newman et al. 2001; Finkelstein, Feibelkorn, and Wang 2003; Lubitz et al. 2003; Lakdawalla, Goldman, and Shang 2005).
On the other hand, although, an important issue that has stirred much discussion but has not been explored thoroughly is the natural weight-loss that happens as individuals get older because of the aging process (e.g., loss of bone density) and/or the development of consuming chronic diseases and the associated treatments. This makes it difficult to trace the medical events in older age to extra body weight in younger age (Willett et al. 2005). For example, a 65-year-old overweight diabetic elderly individual will likely experience episodes of acute comorbidities, such as acute myocardial infarction (AMI) or stroke, and survive into her 70s with functional disabilities. Her weight in her 70s could drop into normal weight, or even underweight, because of natural aging, consuming diseases, medical treatment, and possibly some behavioral adjustment to control her weight. If we examine the cross-sectional relationship between her body weight and health care expenditures in her seventies, we cannot associate the medical treatments, such as rehabilitation, long-term care, or prescription drugs for her AMI or stroke, to her overweight condition in her 60s. Therefore, investigating the cross-sectional relationship between current body weight and health care expenditures could also lead to underestimates of the financial burden of overweight or obesity among the elderly.
In this study, using a nationally representative longitudinal sample of Medicare beneficiaries age 65 or older, we extend the literature on the economic consequences of the epidemic of obesity by developing a dynamic model to estimate both the direct relationship between body weight and four major types of health care expenditures (inpatient, outpatient, nursing homes, and outpatient prescription drugs) at the cross-sectional level, as well as the indirect relationships between body weight and subsequent health care expenditures which are induced by comorbidities associated with weight-related health problems longitudinally. Then, based on our estimation, we conducted a simulation of one age cohort with different baseline weights from age 65 to death or up to age 100 to gauge the lifetime health care expenditures attributed to extra body weight since age 65.
METHOD
Data
The data used in this study are the longitudinal Cost and Use files of the Medicare Current Beneficiary Survey (MCBS). The MCBS is a longitudinal survey conducted by the Centers for Medicare and Medicaid Services to examine medical care use and health status of a representative sample of Medicare beneficiaries in the United States. The Cost and Use files of MCBS provide two types of data: individual survey data and medical care claims. Demographic characteristics, height, weight, and health status (including mortality, functional status, and existing chronic diseases) are collected in the survey. The Medical claims files include the charges and payment information of each inpatient, outpatient, and nursing home event of all respondents during the survey time frame. The charge and payment of each outpatient prescription drug refill is also recorded in the claims file. The claims data include not only the services covered by Medicare, but also services not covered by Medicare, such as long-term care and outpatient prescription drugs. In addition to the total charge of each medical event, the amount of payment by each payer besides Medicare is provided in the claim data, including Medicaid, supplemental private insurances, health maintenance organizations, and out-of-pocket payment. As part of the longitudinal survey, the respondents were followed between 1 and 5 years. However, not all of the respondents in the MCBS were followed for the same number of years as some of them died or dropped out randomly. Additionally, new individuals were added to the survey each year, allowing the sample size to be relatively similar across time. A more thorough description of the MCBS is provided elsewhere (Adler 1994).
Cost and Use files of MCBS from 1992 to 2001 were used in this analysis. The respondents who were under age 65 or with missing height or weight information were excluded. Because this study aims at investigating both the direct influence of weight on current health care expenditures as well as the indirect influence of weight on subsequent health care expenditures, at least 2 years of observation for each individual is needed for the empirical estimation, and respondents with only 1 year of observation are excluded.1 From an initial 45,966 individuals, this resulted in an analytical sample of 85,038 person-year level observations representing 28,906 unique individuals. The summary statistics of the study sample are shown in Table 1.
Table 1.
Summary Statistics of MCBS 1992–2001
| Variable | Mean | SD |
|---|---|---|
| Body weight | ||
| BMI | 25.47 | (4.80) |
| Under weight (BMI <18.5) | 0.05 | |
| Normal weight (BMI between 18.5 and 25) | 0.45 | |
| Overweight (BMI between 25 and 30) | 0.35 | |
| Obese (BMI>30) | 0.15 | |
| Health care expenditures | ||
| Any inpatient care | 0.22 | |
| Inpatient care expenditures, conditional on any | $4,715 | (6,139) |
| Any outpatient care | 0.88 | |
| Outpatient care expenditures, conditional on any | $3,364 | (5,462) |
| Any prescription drugs use | 0.84 | |
| Prescription drugs expenditures, conditional on any | $940 | (1,059) |
| Any nursing home care | 0.10 | |
| Nursing home care expenditures, conditional on any | $24,067 | (22,904) |
| Health status | ||
| Mortality | 0.05 | |
| No disability | 0.49 | |
| Moderately disabled (IADL or up to three ADLs) | 0.33 | |
| Severely disabled (four or more ADLs) | 0.14 | |
| Self-reported chronic conditions | ||
| Cardio/cerebrovascular diseases | 0.42 | |
| Respiratory diseases | 0.14 | |
| Cancer | 0.18 | |
| Diabetes | 0.17 | |
| Major medical care events | ||
| Cardio/cerebrovascular diseases | 0.22 | |
| Respiratory system diseases | 0.05 | |
| Cancer | 0.05 | |
| Demographics | ||
| Age | 76.45 | (7.52) |
| Male (omitted: female) | 0.41 | |
| Race (omitted: white) | ||
| Black | 0.09 | |
| Other nonwhite | 0.05 | |
| Marital Status (omitted: married) | ||
| Widowed | 0.40 | |
| Divorced, never married or separated | 0.10 | |
| Education (range: 0–18 years) | 10.06 | |
| Income (in 1,000 dollars) | 22.01 | (4.29) |
| Rural resident (omitted: urban) | 0.28 | (73.26) |
BMI, body mass index; MCBS, Medicare Current Beneficiary Survey; ADL, activities of daily living; IADL, instrumental activities of daily living; SD, standard deviation.
Body Mass Index (BMI)
Bodyweight in this study is measured by the BMI (an individual's weight in kilograms divided by the square of their height in meters) calculated by self-reported height and weight from the survey. The average BMI of our study sample was 25.47 (See Table 1), with a standard deviation (SD) of 4.80. About 5 percent of the sample were underweight (BMI <18.5), 45 percent were in normal weight range (BMI between 18.5 and 25), 35 percent were overweight (BMI between 25 and 30), and 15 percent were obese (BMI >30). The overweight or obese elderly account for about 50 percent of the study sample.
Health Care Expenditures
We estimated the total expenditures by all payers recorded in the claims (instead of total charges or spending) of four types of services: inpatient care, outpatient physician care, long-term nursing home care, and outpatient prescription drugs. All the expenditures are inflated to 2,001 dollars based on the Medical Care Component of Consumer Price Index published by Bureau of Labor Statistics. Approximately 22 percent of our sample had at least one hospital stay per year; conditional on that, the average hospital care expenditure was $4,715 (SD=6,139). About 88 percent of our study sample had at least one outpatient physician visit per year; conditional on that, the average physician care expenditure was $3,364 (SD=5,462). Roughly 84 percent of the sample had at least one prescription refill per year, the average prescription drug expenditure was about $940 (SD=1,059) conditional on at least one prescription or refill. Long-term care utilization was low, with only 10 percent of the sample using long-term nursing home care; the average nursing home care expenditure was $24,067 (SD=22,904), conditional on at least one nursing home stay.
Chronic Diseases and Acute Medicare Care Events
Survey respondents were asked about their existing chronic diseases. In our analysis, we included four types of chronic diseases that are the major threats to mortality or functional disability among the elderly population (Ferrucci and Guralnik 1997). These are cardio/cerebral vascular diseases (hypertension, heart diseases, stroke, etc.), respiratory system diseases (chronic obstructive pulmonary disease, bronchitis, etc.), cancer excluding skin cancer, and diabetes (both types I and II).
Major acute medical care events refer to the clinical diagnoses of acute medical conditions if the respondents seek inpatient or outpatient care for these conditions. These conditions are cardiovascular or cerebrovascular diseases (International Classification of Diseases 9th Revision [ICD-9] 390–490), respiratory system diseases (ICD-9 480–490), and cancer (ICD-9 140–209). The ICD-9 codes are obtained from the claims data. We included both the presence of existing chronic diseases and acute medical care events to measure the dynamic features of the development of chronic diseases. For example, an elderly individual without any previous history of chronic disease may experience an AMI and become a chronic cardiovascular patient. On the other hand, an elderly individual with diabetes may not necessarily have a major medical care event because of high-quality chronic care.
The literature suggests that both existing chronic conditions and acute medical care events relate to body weight (Flegal et al. 2002; Hedley et al. 2004; Lakdawalla, Goldman, and Shang 2005). However, the influences of chronic diseases and acute medical care events on health care expenditures are different. People with chronic diseases usually have higher demand for outpatient care or prescription drugs, but acute medical care events are more likely associated with higher inpatient or nursing-home expenditures. About 42 percent of our sample had chronic cardio/cerebral vascular diseases, 14 percent had chronic respiratory system diseases, 18 percent had cancer, and 17 percent had diabetes. Acute cardio/cerebrovascular diseases were the major acute medical events for this group; 22 percent of the sample sought medical treatment for these conditions. About 5 percent of the sample experienced acute medical events of cancer or respiratory system diseases separately. Each individual could have more than one acute medical event of the same type, or multiple acute medical events of different types within a calendar year.
Mortality and Functional Status
Data on deaths and functional disability are obtained from the survey. The mortality rate across all ages was approximately 5 percent. We grouped the functional status into three categories: (1) no functional limitations, (2) moderately disabled with at least one instrumental activities of daily living (IADL) limitation and/or up to three activities of daily living (ADL) limitations, and (3) severely disabled with four or more ADL limitations. Forty-nine percent of our study sample did not have any functional limitations, 33 percent were moderately disabled, and 14 percent were severely disabled.
Simultaneous Equations
We constructed a simultaneous equation system that includes four types of equations to model the dynamic relationship between body weight, prevalence of chronic diseases, development of functional disability, longevity, and health care expenditures. The unit of analysis is the person-year level. The four equations are outlined below:
Health Care Expenditure Equations
We estimated four two-part models to predict annual inpatient, outpatient, long-term care, and prescription drug expenditures conditional on BMI (Manning et al. 1987). Let i represent individual, t represent time period, and k represent the types of health care:
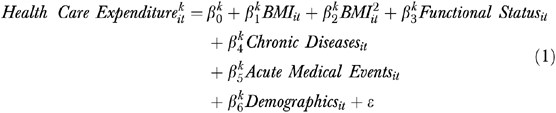 |
(1) |
In each two-part model, we first used a logit model to predict the probability of any health care utilization. Conditional on positive expenditures, we used a linear regression model to predict the natural log of the health care expenditures. The major independent variables are BMI and its quadratic form. The quadratic form helps capture the nonlinear relationship between BMI and health care expenditures, because the people in the lowest and highest BMI levels are generally in worse health and have higher health care expenditures (Fogel 1994). Functional status, existing chronic diseases, and acute medical care events were included as independent variables since these conditions closely relate to health care demand. In addition, demographic characteristics (age, gender, race, marital status, income, educational level, urban/rural residence, and smoking history) were included as independent variables.
Probability of Acute Medical Care Events
We estimated three logit models to predict the probability of each type of acute medical care events in a year. Let m represent the type of acute medical event
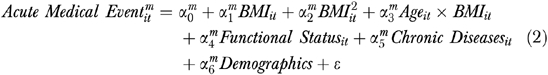 |
(2) |
The dependent variables are whether the elderly had any one type of the acute medical events in a year. The independent variables include BMI, its quadratic form, and the interaction of age and BMI to estimate the influence of body weight on the probability of major medical care events in different ages (Stevens et al. 1998). Functional status was included as an independent variable because the elderly with more functional disabilities are more likely to suffer acute medical care events. For example, people with ADLs are more likely to suffer pneumonia (El-Solh, Sikka, and Ramadan 2001). Because people with chronic diseases usually are in higher risk of acute medical care events, we controlled for the four chronic conditions. Demographic characteristics were included as independent variables.
Transition of Functional Status and Mortality
We modeled the transition of functional status and probability of mortality from year to year using a multinomial logit model.
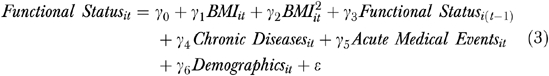 |
(3) |
The dependent variable is categorized into four categories: (1) no functional disability, (2) moderately disabled with IADL or up to three ADLs, (3) severely disabled with four or more ADLs, and (4) death.2 The purpose of the functional transition equation is to model the change of health status conditional on age and body weight over time. The functional status, along with mortality, measures the “health capital” of each individual, since people usually lose their functional abilities before death (Grossman 1972). The more functional disabilities a person has, the less “health capital” she has, and the closer she is to death. Death is the absolute worst health outcome with 0 “health capital” value. Based on our observation of the data, the changes in functional status from year to year do not follow one direction and become worse over time. For example, about 15 percent of the observations in our study sample experienced improvement in functional status because they recovered from severe diseases as a result of medical treatment. Therefore, instead of using an ordered logit or an ordered probit model, which assumes that functional status is deteriorating all the time, we used a multinomial logit model to estimate the functional transition equation. This allows for more flexibility in the estimation. The independent variables include functional status in the previous year, BMI, and its quadratic. Because of the well-documented correlation between the prevalence of chronic diseases and functional disability, the existing chronic diseases and acute medical care events were included as independent variables (Ferrucci and Guralnik 1997; Fried and Guralnik 1997; Costa 2002). Demographic characteristics were also controlled for.
Transition of BMI
We used linear regression to model the transition of BMI from year to year along with the other three models introduced above.
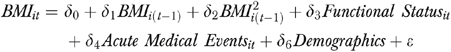 |
(4) |
The dependent variable is current BMI, the independent variables include previous BMI, and its quadratic. Functional status was included as an independent variable because functional ability closely relates to muscle mass, metabolism rate, and body weight. In addition, since major acute medical care events and associated treatments may cause weight change (e.g., chemotherapy could cause significant weight loss), we included the acute medical care events as independent variables. Demographic characteristics were also controlled for.
Maximum Likelihood Estimation (MLE) and Identification
The measures of BMI, chronic disease, acute medical events, and functional status affect one another in a dynamic pattern along the aging process. In addition, each individual adjusts their behaviors constantly depending on their weight and health conditions until death. Therefore, we estimated equations (1–4) simultaneously using the MLE. The simultaneous equation system serves as an approximation of the natural aging process in order to estimate the complex interrelationships between different aspects of the biological changes in human bodies, as well as the demand for health care.
The simultaneous system is identified by two mechanisms: first, we included several exogenous variables that help to explain the variations in body weight and general health status by geographic location, which include average food prices, density of fast food restaurants, and air quality at county level obtained from public used behavioral surveillance file in the body weight and health status transition equations. We also included health care provider information, such as density of hospitals, physicians, and nursing home beds at county level from area resource file in the health care demand equations. Second, we used discrete random effect to control for time-consistent and time-varying unobserved individual heterogeneity to help the identification (Heckman and Singer 1983; Mroz 1999; Yang, Gilleskie, and Norton 2004).
Simulation
The interpretation of the estimated parameters in every single equation in the simultaneous equation system is difficult because the effects of the coefficients in one single equation spill over to other equations (all the coefficients are presented in the Supplementary Materials appendix tables). In order to assess the health care expenditures associated with extra body weight, we have to account for both the direct effects of BMI on current health care expenditures, as well as the indirect effect of BMI on future health care expenditures through its influence on the probability of major medical events, transition of functional status, and mortality. The best way to illustrate the dynamic effect of BMI on health care expenditures over time is to apply all of the coefficients simultaneously to a virtual cohort of one population sample based on their baseline body weight by simulating all of the direct and indirect effects that emerge.
We performed 2,000 replications of the simulation for each individual using the parameters obtained from our simultaneous MLE model with a cohort starting at age 65 with observed demographic features, BMI, and existing chronic conditions. Each replication draws a random set of error terms for all the equations from age 65 until 100. In the years following age 65, we simulated the probabilities of major acute medical care events, and the probabilities and natural logs of the four types of medical care expenditures. Then, we simulated the transition of functional status and BMI and updated both the functional status and BMI in the next year. All existing chronic conditions at age 65 were treated as permanent in all simulations in all ages. In addition, if a person was simulated to have a new acute medical care event, the program updated her to have the associated chronic diseases throughout the remaining lifetime until death. Such procedures are repeated each year with updated functional status, chronic disease, and BMI. If any individuals were simulated dead, the program automatically stopped; otherwise the program continued until age 100. Then, we calculated the average BMI, average life expectancy, average healthy life expectancy (longevity without functional disability), and total health care expenditures from age 65 to death or age 100. We bootstrapped the standard errors of all the results. Because we estimated and simulated the natural log of all the health care expenditures, we retransformed all the log expenditures to real dollar values with the adjustment of smearing factor when calculating the health care expenditures after the simulation (Duan 1983).
RESULTS
The average lifetime health care expenditures from age 65 to death or up to age 100 for people with different baseline weights are presented in Table 2. Because of the well-documented gender disparities in longevity, health status, and demand for health care services, we present all the results by gender (Case and Paxson 2004). Among males, those who were overweight or obese at age 65 had higher average lifetime inpatient care expenditures ($61,099 and $64,702, respectively) than those whose baseline weight was normal weight or underweight ($57,337 and $47,537, respectively). For outpatient care and prescription drugs, the patterns are similar. The cohorts with higher baseline weights had higher lifetime expenditures. For long-term care, however, the pattern is different. The underweight and normal weight cohorts had higher lifetime expenditures ($36,651 and $37,439, respectively) than the overweight or obese cohorts ($34,817 and $35,014, respectively).
Table 2.
Total Healthcare Expenditures from Age 65 to Death or up to Age 100
| Health Care Expenditures (SD) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||
| Baseline Weight | Inpatient | Outpatient | Nursing Home | Prescription Drugs | Total | Inpatient | Outpatient | Nursing Home | Prescription Drugs | Total |
| Underweight | $47,537 (4,006) | $49,852 (4,034) | $36,651 (4,251) | $8,051 (944) | $142,092 (3,140) | $44,771 (3,958) | $53,952 (4,261) | $50,500 (4,012) | $12,305 (1,105) | $161,528 (3,341) |
| Normal weight | $57,337 (3,287) | $63,076 (3,865) | $37,439 (3,745) | $11,577 (1,113) | $169,430 (3,258) | $55,083 (3,326) | $68,014 (3,697) | $51,306 (3,943) | $17,000 (1,326) | $191,405 (3,649) |
| Overweight | $61,099 (3,364) | $69,875 (3,564) | $34,817 (3,236) | $13,902 (1,168) | $179,695 (3,054) | $60,146 (3,512) | $76,679 (3,457) | $54,352 (3,865) | $20,743 (1,598) | $211,922 (3,215) |
| Obese | $64,702 (4,487) | $74,923 (4,122) | $35,014 (3,725) | $16,016 (1,196) | $190,657 (3,169) | $64,280 (4,235) | $83,052 (4,021) | $52,442 (3,941) | $23,854 (1,476) | $223,629 (2,895) |
Among the female cohorts, the distributions of inpatient care, outpatient care and prescription drugs expenditures by baseline weight are similar to the male cohorts. The cohorts that were overweight or obese at age 65 had higher lifetime inpatient, outpatient, and prescription drugs expenditures than the cohorts who were within normal weight or underweight range. Interestingly, different from the males, the female cohorts who were overweight or obese at age 65 had higher lifetime long-term nursing home care expenditures ($54,352 and $52,442) than the normal weight or underweight cohort ($51,306 and $50,500). All female cohorts had higher health care expenditures for most types of services than the corresponding male cohorts in the same baseline weight category. The major explanation could be longer longevity and a more gradual aging process among women than among men.
Aggregating health care expenditures of all four types of medical care together, the average total health care expenditures of the male overweight cohort ($179,695) was 6 percent higher than the male normal weight cohort ($169,430). The male obese cohort spent 12.5 percent ($190,657) more than the male normal weight cohort. Among females, the overweight cohort spent 10.7 percent ($211,922) more than the normal weight cohort ($191,405), the obese cohort spent 16.8 percent ($223,629) more than the normal weight cohort. The magnitudes of increase in health care expenditures related to overweight or obesity were higher among women than among men. The total excess of medical care expenditures could be $15,000 of every overweight individual, and $26,000 of every obese individual on average. The total extra financial cost of health care of the overweight and obesity epidemic across the population could be up to 4 hundred billion dollars.
Previous studies suggest that increased weight could be a protective factor against mortality among the elderly population (Grabowski and Ellis 2001; Taylor and Østbye 2001). Thus, we compared the simulated life expectancies and healthy life expectancies (longevity of life without IADLs or ADLs) of the cohorts with different baseline weights to investigate whether the higher health care expenditures among the overweight or obese cohorts were due to longer longevity (see Table 3). Among both men and women, the average life expectancy is the highest among the cohort with normal baseline weight, at 82.53 and 86.15 years, respectively. The cohorts who were overweight at age 65 had the second longest life expectancy at 82.32 and 85.41 years, respectively, but the results are not statistically significantly different from the normal weight cohorts. Those who were underweight or obese at age 65 had the shortest life expectancy among both men and women; their differences with the normal weight cohorts are statistically significant.
Table 3.
Simulated Life Expectancy Baseline Weight
| Life Expectancy (SD) | Health Life Expectancy (SD) | |||
|---|---|---|---|---|
| Baseline Weight | Male | Female | Male | Female |
| Underweight | 80.40 (1.54) | 81.76 (1.38) | 75.89 (1.87) | 74.13 (1.80) |
| Normal weight | 82.53 (1.57) | 86.15 (1.63) | 76.11 (1.49) | 73.97 (1.56) |
| Overweight | 82.32 (1.22) | 85.41 (1.30) | 74.95 (1.51) | 72.66 (1.48) |
| Obese | 80.93 (1.29) | 84.75 (1.29) | 74.22 (1.67) | 71.60 (1.71) |
Among males, the normal weight cohort had a healthy life expectancy of 76.11 years, followed by the underweight cohort at 75.89 years, the overweight cohort at 74.95 years, and the obese cohort at 74.22 years. Among females, the underweight cohort had slightly longer healthy life expectancy at 74.13 years than the normal weight cohort at 73.97 years, followed by the overweight cohort at 72.66 years. The female obese cohort had the shortest healthy life expectancy at 71.60 years. Therefore, the simulation results in our study do not support the conclusions from earlier studies that extra weight is a protective factor against mortality among the elderly population.
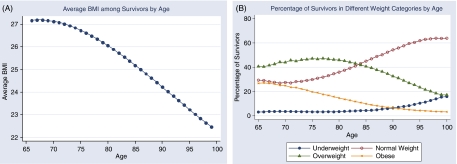
Concerning the dynamic changes of body weight along the aging process related to health conditions and survival, we plotted the average BMI among survivors and the distributions of survivors in different weight categories by age. The average BMI among survivors dropped from around 27 at age 65 to about 22 at age 100 (Figure 1A). Among survivors at age 65, about 40 percent were overweight, and 30 percent were obese. This distribution is close to the prevalence of obesity among adults. From age 65 to age 100, the percentages of overweight and obese survivors decrease from 40 and 25 percent to below 20 and <10 percent. Conversely, the percentages of normal weight and underweight survivors increase from about 30 and <10 percent to 60 percent and close to 20 percent (Figure 1B).
Figure 1.
Dynamics of BMI Transition along Aging Process. BMI, Body Mass Index.
CONCLUSIONS AND DISCUSSIONS
We investigated the financial burdens of overweight and obesity among elderly Americans by estimating a simultaneous dynamic model that unravels the complicated relationship between the biological changes of aging and health care expenditures. The results showed that the prevalence of obesity places significant financial burdens on the U.S. health care system. When the “baby boomers” start to turn 65, it is expected that growth in the size of the eligible Medicare population, the development of new medical technology, and the increases in average longevity will result in increases in Medicare and Medicaid spending. Our research indicates that the increasing prevalence of obesity will contribute toward additional financial burdens being placed on public health insurance.
Compared with early research, our approach in modeling health conditions, functional status, and health care expenditures is similar to the Future Elderly Model (FEM) developed by Rand. However, the major difference is that our model treats BMI as dynamic, and assumes changing relationships between body weight and other health outcomes among the elderly over time. In contrast, earlier studies treat body weight as a permanent chronic condition among the elderly (e.g., Grabowski and Ellis 2001; Taylor and Østbye 2001; Lakdawalla, Goldman, and Shang 2005). Therefore, our estimates of the increase in health care expenditures induced by higher body weight is lower than earlier studies, and we did not find higher body weight to be a protective factor against mortality. In addition, our study measured functional status by IADLs and ADLs directly. Comparatively, the Rand FEM model measured severe disability by transition into institutionalized state, which is a very close proxy to four or more ADLs. Such difference in measurement of disability could also lead to some differences in the expenditure estimates between these two studies, especially nursing home expenditures. Modeling the changes in body weight and the health dynamics of the elderly is challenging. Our research demonstrates a new estimation method to investigate the changes in population biological and behavioral characteristics on the demand for health care.
Acknowledgments
The authors would like to thank the Aldrich Award for Faculty Research from Michigan State University to purchase the MCBS data used in this study. We are also grateful for the valuable comments from the two anonymous referees, as well as numerous comments from the participants of the third Annual Southeastern Health Economics Study Group Conference and the Inaugural Meeting of American Society of Health Economists.
NOTES
We compared the summary statistics of BMI, demographic characteristics, functional status, prevalence of chronic diseases, and acute medical events, as well as mortality rate among those with only a 1-year observation and those in our study sample with at least 2 years of observation. We did not find statistically significant differences between these two samples. Therefore, we believe the attrition is random and does not influence the conclusion of this study.
We did not include the transition to the institutionalized state in the functional limitation equation for these reasons: (1) functional status is well recognized as a good objective measure of health status of the elderly; (2) functional status closely relates to institutionalization; most of the long-term care residents have functional disabilities, so that measuring both will be duplicative; and (3) the data we used contain no more than 5 years observation for one individual; for those respondents who are observed to enter a nursing home during the last 1 or 2 years of the MCBS survey period, we are not sure if their institutionalization is permanent. So, in order to avoid measurement error, we simply did not model such status.
Supplementary material
The following supplementary material for this article is available online:
Estimation Results from the Simultaneous Equation System.
This material is available as part of the online article from: http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2007.00801.x (this link will take you to the article abstract).
Please note: Blackwell Publishing is not responsible for the content or functionality of any supplementary materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Adler G. A Profile of the Medicare Current Beneficiary Survey. Health Care Financing Review. 1994;15(4):153–63. [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya J, Bundorf M K. The Incidence of Healthcare Costs of Obesity. 2005. NBER Working Paper #11303. [DOI] [PMC free article] [PubMed]
- Case A, Paxson C. Sex Differences in Morbidity and Mortality. 2004. University of Princeton Working Paper. [DOI] [PubMed]
- Cawley J. The Impact of Obesity on Wage. Journal of Human Resources. 2004;39(2):451–74. [Google Scholar]
- Costa D L. Changing Chronic Disease Rates and Long-Term Declines in Functional Limitation among Older Men. Demography. 2002;39(1):119–37. doi: 10.1353/dem.2002.0003. [DOI] [PubMed] [Google Scholar]
- Daviglus M L. Health Care Costs in Old Age Are Related to Overweight and Obesity Earlier in Life. Health Affairs. 2005;W5:98–100. doi: 10.1377/hlthaff.w5.r97. [DOI] [PubMed] [Google Scholar]
- Duan N. Smearing Estimate. A Nonparametric Retransformation Method. Journal of the American Statistical Association. 1983;78(383):605–10. [Google Scholar]
- El-Solh A A, Sikka P, Ramadan F. Outcomes of Older Patients with Severe Pneumonia Predicted by Recursive Partitioning. Journal of American Geriatric Society. 2001;49(12):1614–21. doi: 10.1046/j.1532-5415.2001.t01-1-49269.x. [DOI] [PubMed] [Google Scholar]
- Ferrucci L, Guralnik J. Hospital Diagnoses, Medicare Changes, and Nursing Home Admissions in the Year When Older Persons Become Severely Disabled. Journal of the American Medical Association. 1997;277(9):728–34. [PubMed] [Google Scholar]
- Finkelstein E A, Fiebelkorn I C, Wang G. National Medical Spending Attributable to Overweight and Obesity. How Much, and Who's Paying? Health Affairs. 2003;W3:219–26. doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- Flegal M K, Carroll M, Ogden C, Jonson C. Prevalence and Trends in Obesity among US Adults, 1999–2000. Journal of the American Medical Association. 2002;288(14):1723–8. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- Flegal M K, Graubard B, Williamson D, Gail M. Excess Deaths Associated with Underweight, Overweight and Obesity. Journal of the American Medical Association. 2004;293(15):1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Fogel R W. Economic Growth, Population Theory, and Physiology. The Bearing of Long-Term Processes of Making Economic Policy. American Economic Review. 1994;84(3):369–95. [Google Scholar]
- Fried L P, Guralnik J M. Disability in Older Adults. Evidence Regarding Significance, Etiology and Risk. Journal of American Geriatric Society. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Grabowski D C, Ellis J E. High Body Mass Index Does Not Predict Mortality in Older People. Analysis of Longitudinal Study of Aging. Journal of American Geriatrics Society. 2001;49(7):968–79. doi: 10.1046/j.1532-5415.2001.49189.x. [DOI] [PubMed] [Google Scholar]
- Grossman M. On the Concept of Health Capital and the Demand for Health. Journal of Political Economy. 1972;80(2):223–55. [Google Scholar]
- Heckman J, Singer B. A Method for Minimizing the Impact of Distributional Assumptions in Econometric Models for Duration Date. Econometrica. 1983;52:271–320. [Google Scholar]
- Hedley A A, Ogden C L, Johnson C L, Carroll M D, Curtin L R, Flegal K M. Prevalence of Overweight and Obesity among US Children, Adolescents, and Adults, 1999–2002. Journal of the American Medical Association. 2004;291(23):2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Lakdawalla D N, Goldman D P, Shang B. The Health and Cost Consequences of Obesity among the Future Elderly. Health Affairs. 2005;W5:30–41. doi: 10.1377/hlthaff.w5.r30. [DOI] [PubMed] [Google Scholar]
- Lubitz J, Cai L, Kramarow E, Lentzner H. Health, Life Expectancy, and Health Care Spending among the Elderly. New England Journal of Medicine. 2003;349:1048–55. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- Manning W, Newhouse J, Duan N, Keeler E, Leibowitz A, Marquis M. Health Insurance and the Demand for Medical Care. Evidence from a Randomized Experiment. American Economic Review. 1987;77(3):251–77. [PubMed] [Google Scholar]
- Mroz T A. Discrete Factor Approximation in Simultaneous Equation Models. Estimating the Impact of a Dummy Endogenous Variable on a Continuous Outcome. Journal of Econometrics. 1999;92:233–74. doi: 10.1016/s0304-4076(98)00091-8. [DOI] [PubMed] [Google Scholar]
- Must A, Spadano J, Coakley E H, Field A E, Colditz G, Dietz W H. The Disease Burden Associated with Overweight and Obesity. Journal of the American Medical Association. 1999;282(16):1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States with Chartbook on Trends in the Health of Americans. Hyattasville, MD: National Center for Health Statistics; 2006. [Google Scholar]
- Newman A, Yanez D, Harris T, Duxbury A. Weight Change in Old Age and Its Association with Mortality. Journal of American Geriatrics Society. 2001;49(10):1309–18. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- Ogden C L, Carroll M D, Curting L R, McDiwekk M A, Tabak C J, Flegal K M. Prevalence of Overweight and Obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Parikh N I, Pencina M J, Wang T J, Lanier K J, Fox C S, D'Agostino R B, Vasan R S. Increasing Trends in Incidence of Overweight and Obesity over 5 Decades. American Journal of Medicine. 2007;120:242–50. doi: 10.1016/j.amjmed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Stevens J, Cai J, Pamuk E, Williamson D, Thun M, Wood J. The Effect of Age on the Association between Body-Mass Index and Mortality. New England Journal of Medicine. 1998;338(1):1–7. doi: 10.1056/NEJM199801013380101. [DOI] [PubMed] [Google Scholar]
- Taylor D, Østbye T. The Effect of Middle- and Old-Age Body Mass Index on Short-Term Mortality in Older People. Journal American Geriatrics Society. 2001;49(10):1319–26. doi: 10.1046/j.1532-5415.2001.49259.x. [DOI] [PubMed] [Google Scholar]
- Willett W C, Hu F B, Colditz G A, Manson J E. Underweight, Overweight, Obesity and Excess Deaths. Journal of the American Medical Association. 2005;294(5):551. doi: 10.1001/jama.294.5.551-a. [DOI] [PubMed] [Google Scholar]
- Yang Z, Gilleskie D B, Norton E C. “Prescription Drugs, Medical Care, and Health Outcomes: A Model of Elderly Health Dynamics.”. 2004. NBER Working Paper #10964.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Estimation Results from the Simultaneous Equation System.