Abstract
Objectives
To estimate a hybrid cost function of the relationship between total annual cost for outpatient methadone treatment and output (annual patient days and selected services), input prices (wages and building space costs), and selected program and patient case-mix characteristics.
Data Sources
Data are from a multistate study of 159 methadone treatment programs that participated in the Center for Substance Abuse Treatment's Evaluation of the Methadone/LAAM Treatment Program Accreditation Project between 1998 and 2000.
Study Design
Using least squares regression for weighted data, we estimate the relationship between total annual costs and selected output measures, wages, building space costs, and selected program and patient case-mix characteristics.
Principal Findings
Findings indicate that total annual cost is positively associated with program's annual patient days, with a 10 percent increase in patient days associated with an 8.2 percent increase in total cost. Total annual cost also increases with counselor wages (p<.01), but no significant association is found for nurse wages or monthly building costs. Surprisingly, program characteristics and patient case mix variables do not appear to explain variations in methadone treatment costs. Similar results are found for a model with services as outputs.
Conclusions
This study provides important new insights into the determinants of methadone treatment costs. Our findings concur with economic theory in that total annual cost is positively related to counselor wages. However, among our factor inputs, counselor wages are the only significant driver of these costs. Furthermore, our findings suggest that methadone programs may realize economies of scale; however, other important factors, such as patient access, should be considered.
Keywords: Drug treatment costs, cost function, methadone, SASCAP
Although a substantial literature provides estimates of the total and per-patient costs for substance abuse treatment, relatively little is known about what drives these costs or why large variation in treatment costs is often observed across programs. In this paper, we use data from a multistate sample of methadone treatment programs to examine the factors that drive the costs of providing outpatient methadone treatment. Understanding these factors has become particularly important given the limited funding for treatment and the demand for greater fiscal accountability for the services delivered. Moreover, this information is a crucial piece in understanding the delivery of treatment services as providers and policy makers continue to strive toward cost-effective treatment.
Numerous studies have examined costs for hospitals, physician practices, and other medical services (Reinhardt 1972; Grannemann, Brown, and Pauly 1986; Breyer 1987; Nyman and Dowd 1991; Goodman et al. 1992; McAvinchey and Yannopoulos 1994; Wholey et al. 1996; Carey 1997; Goodman, Nishiura, and Hankin 1998; McNamee et al. 1998; Andersen, Andersen, and Kragh-Sorensen 2000; Bilodeau, Crèmieux, and Oullette 2000). Perhaps the most relevant lesson from this literature is that, in addition to examining the influence of output and input prices on cost, the empirical specification should control for other variables that may affect costs. These variables include program characteristics such as ownership structure, urbanicity of the facility's geographic location, and severity of the program's patients. A specification that includes output, input prices, and these other program characteristics is known as a hybrid cost function (Rosko and Broyles 1988).
Using data from the 1996 Alcohol and Drug Services Study (ADSS), Duffy et al. (2004) estimated a hybrid cost function for 222 outpatient nonmethadone substance abuse treatment programs. In addition to measures of annual admissions (as a measure of output) and staff wages and rent (as measures of input prices), Duffy et al. include in their model several variables capturing facility characteristics (e.g., age, ownership, urbanicity) and patient case mix (e.g., patient race/ethnicity, percentage of criminal justice referrals). The authors found that a 10 percent increase in admissions yielded a 6.7 percent increase in total annual costs. In addition, the percentage of clients who received Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI) was positively associated with total annual costs. No other explanatory variables were statistically significant.
Harwood, Kallinius, and Liu (2001) estimated the relationship between total cost per patient day and average daily client census for 60 residential treatment programs. Average daily census was the only explanatory variable in the regression model. Harwood and colleagues found that larger programs had lower costs per day and that a 10 percent increase in average daily census is associated with decreases in the cost per patient day ranging from 3.5 to 10.7 percent.
Studies of methadone treatment over the past 25 years have rarely provided information on how a treatment program's costs vary with its output and input prices. But, as new funding mechanisms are being adopted and patients and providers face increasing pressures to reduce services and control costs, meaningful information on the relationship between program costs, program output, and treatment inputs is needed. Understanding this relationship may help methadone treatment providers in their decisions on staffing, setting reimbursement rates, and strategic business planning.
In this study, we estimate a hybrid long-run cost function of outpatient methadone treatment programs. This study is significant because it examines the effect of key inputs and program characteristics on the costs of providing methadone treatment—the most common treatment modality for opioid abuse in the United States. To date, there are no published studies that examine how a methadone treatment program's costs vary with its output, input prices, and other relevant covariates.
DATA AND METHODS
Data
Data in this study were collected as part of a larger study of methadone treatment programs that participated in CSAT's Evaluation of Opioid Treatment Program Accreditation Project (RTI International 2003). The evaluation study was primarily designed to study the effect on the national methadone treatment system of new opioid treatment regulations requiring accreditation from a Substance Abuse and Mental Health Services Administration (SAMHSA)-approved accreditation body. Treatment programs were chosen for the main evaluation study using a multistage, stratified-randomized control sampling design. The first stratum was states. Fifteen states were chosen to satisfy one or more of several criteria: being geographically dispersed throughout the four U.S. Census regions, having a large number of methadone programs that represent different models of treatment and/or regulation, being representative of states that participated in the National Institute on Drug Abuse's (NIDA's) Methadone Treatment Quality Assurance System (MTQAS) study, and states currently mandating accreditation. States outside the contiguous U.S. and states having fewer than four methadone treatment programs were excluded from sampling. The 15 states selected comprised almost 70 percent of all methadone programs in the United States in 1998 and almost 75 percent of all methadone patients.
The second stage of sampling involved selecting programs within states. Selection of these treatment programs was a multistage process, ensuring the inclusion of small programs (fewer than 50 patients) as well as for-profit programs. Correctional facilities, medication dispensing units, hospital-based detoxification facilities, and programs operated by the Veterans' Administration were excluded from sampling consideration.
Under the main study, the representativeness of the full sample (N=172) was analyzed based on key program characteristics (e.g., ownership, size, part of larger parent organization), and the sample was found to be very similar to the national distribution of outpatient methadone treatment programs in 1998 (RTI 2003). Statistical analysis weights were computed so that estimates could be derived for the population of outpatient methadone treatment programs in the United States (RTI 2003).
The data in this study were collected from 172 methadone treatment programs that participated in the evaluation study. Because we chose to limit our sample to outpatient facilities, we excluded two treatment programs that self-reported as residential facilities. Eleven additional programs were excluded from the analysis because they had missing program or patient characteristics data. Our final sample for this analysis included 159 outpatient methadone treatment programs.
As part of the evaluation study, methadone treatment programs were asked to complete the Substance Abuse Services Cost Analysis Program (SASCAP), a service-level cost estimation questionnaire that collects data on a treatment program's costs and the time allocation of staff across various treatment services. (See Zarkin, Dunlap, and Homsi 2004 for a detailed description of the SASCAP method.) We received strong support from the programs regarding the cost data collection yielding a 100 percent response rate for the baseline cost data.
The SASCAP questionnaire includes two components—a cost survey that collects standardized annual economic cost data that is comparable across treatment programs, and a labor allocation survey that collects data on staff time allocated across treatment services. We used data from the cost survey in our analysis. The cost survey was completed by each program's site director and/or financial officer (as appropriate) during the baseline data collection period that occurred between 1998 and 2000. Each program was asked to report their costs for the most recently completed fiscal year for personnel and salaries, supplies and materials, contracted services, buildings and facilities, equipment, miscellaneous resources (e.g., utilities) and costs associated with services at the level of a parent organization such as human resources, billing/finance, and marketing (if applicable). In addition, the questionnaire collected information on donated or subsidized labor or building resources so that the fair market value of these resources could be estimated. The information reported in the SASCAP was reviewed by RTI economists for accuracy, and treatment programs were contacted by telephone to gain additional information or clarification as needed. With these data, we calculated the total annual economic costs for each program and those are the costs analyzed here.
Program site directors were also asked to complete a Site Director survey, which collected information on the program's organizational structure, measures of average patient census, and patient characteristics. Similar to the SASCAP questionnaire, the site director's questionnaire was reviewed by RTI staff for accuracy, and additional information was collected if needed.
Variables
The dependent variable in our estimation model is the natural logarithm of total annual costs (in year 2000 dollars). Different measures of output for health care providers have been used in the literature, such as annual number of admissions or discharges, number of patient days, and number of specific health services provided. Methadone programs produce patient care by using a variety of intermediate inputs, such as counseling sessions, methadone doses, and case management. We chose to examine separately two different aspects of methadone treatment output. Our main output variable is annual patient days.1 We calculated annual patient days by multiplying the program's average daily census of methadone patients by 365 days. This patient-days measure represents an annualized volume of patient throughput based on average daily census. However, unlike hospital care in which a patient day means up to 24 hours of continuous care and monitoring including room and board, a patient day for methadone treatment typically does not mean that a patient receives a day's worth of treatment. Rather, it represents the annual number of days for each treatment slot for which the clinic operates and provides services to patients as needed. Patients typically receive <1 hour of services in a given day. Programs in our sample reported that staff, on average, spent about 2 hours per patient per week performing treatment services and administrative activities related to program operations. Although this number may seem low, in an average-sized clinic of 238 patients, this per-patient average translates into 476 total staff hours provided by the program each week, or equivalently a staff of 11.9 full-time equivalents (based on 40 hours per week).
We also examine primary services provided by methadone programs as output measures—annual hours of counseling, intake services, case management, and ongoing medical services. We chose to focus on the core direct patient services for methadone treatment; however, due to severe collinearity, we were not able to include methadone dosing in our model. We also did not include administrative activities because these are not services provided to patients, but rather are activities that support direct patient services and the ongoing operations of the clinic.
We calculated annual hours of counseling by multiplying the program's self-reported average weekly hours of individual and group counseling by 52 weeks. Annual hours of intake service, case management and ongoing medical service were calculated in the same way.
We included three measures for input prices because they represent the primary resources in producing days of patient care: the average hourly counselor wage, the average hourly nurse wage, and the program's monthly rental cost. For counselors, we used the appropriate average occupational wage reported by the Bureau of Labor Statistics (BLS) (2005) for the Metropolitan Statistical Area (MSA) in which the program is located. Specifically, for the counselor wage we used the mean wage for “Substance Abuse and Behavioral Disorder Counselor.” For nurses, we used the average of the mean wages for “Registered Nurse” and “Licensed Practical or Licensed Vocational Nurse” because both nurse types may be employed by methadone treatment programs. A small number of programs were not located in a defined MSA, and in these cases we used either the county-level wage data or data from the closest MSA as appropriate. For each program, we used BLS wages for the fiscal year in which costs were reported. If wage information was not available for the relevant fiscal year, we used the nearest fiscal year and adjusted wages using the Consumer Price Index (CPI). All wages were then adjusted to year 2000 dollars using the CPI.
For monthly rent, we used as a proxy for commercial rents—the four-bedroom Section 8 Fair Market Rent (FMR) as defined by the U.S. Department of Housing and Urban Development's (HUD) Office of Policy Development and Research (2001). The FMR used was for the MSA in which the program was located for the year 2001. Historical data on four-bedroom rates were not available before 2001. These rents were then adjusted to year 2000 dollars using the CPI. To our knowledge, no national database exists on commercial real estate rental rates. The HUD four-bedroom FMR is the same rental measure used by Duffy et al. (2004) in their estimation of a cost function for outpatient nonmethadone treatment facilities. Furthermore, as noted by them, this is the measure that is used in SAMHSA's Substance Abuse Prevention and Treatment (SAPT) block grant formula to assess the rental component of the cost of doing business in each State (U.S. Department of Health and Human Services [DHHS] 1996).
Although counselor wages, nurse wages, and rental costs are available from the SASCAP data, we did not use these data because they are endogenous and may reflect unobserved characteristics that may affect both total costs and wages or rental costs. Our use of exogenous measures for the average wages and rental rates reflects the importance of wages and building costs as a determinant of total costs but avoids potential endogeneity bias.
We also included several measures of program characteristics that may explain variation in costs across programs. These include the program's ownership status (for-profit versus not-for-profit/public), the degree of urbanicity of the program's location, whether the program is part of a larger parent organization (organizational structure), and the program's accreditation status at the time of the baseline data collection. The ownership status variable equaled 1 if the program was a private, for-profit facility and 0 otherwise. The degree of urbanicity of a program's location was represented using dichotomous variables to represent three categories—whether the program was in a large urban area (population greater than 1 million; the omitted reference category), a medium-sized urban area (population between 250,000 and 1 million), or a small-sized urban area (population between 20,000 and 250,000). Urbanicity classifications are based on the Beale urbanicity codes, which were assigned based on the facility's zip code (Butler and Beale 1994). The organizational structure variable equaled 1 if the program was not part of a larger parent organization and 0 otherwise. Programs that are part of a larger organization may be able to share administrative overheard, obtain inputs at lower prices, or take part in other efficiencies that may result in having lower operating costs (Duffy et al. 2004). On the other hand, programs that are part of a larger organization may offer a greater variety or scope of services or may have greater costs associated with administrative overhead due to a more complex management structure. Finally, the accreditation status variable equaled 1 if the facility reported being accredited before the onset of the evaluation study and 0 otherwise. Accredited programs may have greater costs because they provide a higher level of care.
We also included several program-level variables that describe the program's patient population. These case-mix variables were designed to help control for differences in programs' patient case mix that may help explain variation in treatment costs. Because programs with a more diverse racial/ethnic patient population may incur higher costs in providing services (Duffy et al. 2004), we included a continuous measure of the program's percentage of nonwhite patients. Programs with higher levels of dually diagnosed patients (i.e., individuals with both substance use and mental health disorders) may have greater costs because they may also provide mental health services. Therefore, we created a set of indicator variables measuring the program's percentage of patients who are dually diagnosed.
Because patients who are uninsured or on Medicaid may have greater unmet needs and thus require more intensive treatment services than patients with private health insurance, we include continuous measures of both the program's percentage of uninsured patients and the percentage of patients on Medicaid. We hypothesize that programs with patients in need of more intensive services may have higher costs. However, it is also possible that programs in States with Medicaid coverage for substance abuse treatment services may have more incentive to control costs. Furthermore, programs with uninsured patients may, in fact, have some patients who are insured but who prefer to pay out-of-pocket rather than report their substance abuse treatment needs to their insurance provider.
Empirical Model
We estimated a modified translog cost function of total annual cost using the following equation:
 |
(1) |
where Ln(Cj) is the natural logarithm of total annual cost for program j; Ln(PDAYj) is the natural logarithm of number of annual patient days; Ln(IPRICEj) is a vector of the natural logarithm of input prices (counselor wage, nurse wage, and monthly space cost); PROGj is a vector of program characteristics (for-profit status, urbanicity of program location, whether the program is part of a larger organization, and the accreditation status of the program); CASEMIXj is a vector of program-level patient case-mix variables (e.g., the percentage of nonwhite patients, the percentage of dually diagnosed patients, and the insurance status of patients); the βs are coefficients to be estimated; and ɛ is an error term.
Next, we estimated a modified translog cost function of total annual cost with selected methadone treatment services as output variables using the following equation:
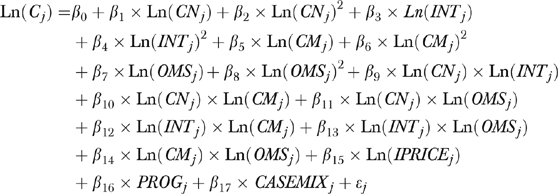 |
(2) |
where Ln(CNj), Ln(INTj), Ln(CMj), and Ln(OMSj) are the natural logarithms of annual hours of counseling, intake services, case management and ongoing medical services provided by program j.2 We included interaction terms for these output measures so that we could evaluate the potential for local economies of scope, or weak cost complementarities (WCC), generated by producing services with similar inputs. When the multiproduct cost function is in logarithmic form, a sufficient condition for the presence of economies of scope is that the cost function exhibits WCC; that is, ∂2C(ŷ)/∂yi∂yj≤0, i≠j for all ŷ with 0≤ŷ≤y (Baumol, Panzar, and Willig 1982). The remaining terms are defined as above in equation 1.
Because the dependent variable is continuous in each of the regression equations, we used ordinary least squares regression for weighted survey data to estimate the models (StataCorp 2003).
Using the estimated coefficients from the regression analyses, we estimated the marginal and average costs associated with different volumes of output. Marginal costs are derived by taking the derivative of the predicted total annual costs by the independent variable of interest (e.g., number of patients, hours of counseling). Average cost for each program for the single product specification of patient days is calculated by dividing the predicted annual total cost by the program's annual patient days, and then taking the average across all programs. For the multiproduct specification, we used the concept of average incremental costs (Grannemann, Brown, and Pauly 1986). For each program, incremental costs for a specified output are calculated by taking the difference between the predicted annual total cost of producing all outputs (at a determined level) and the predicted annual total cost of producing all outputs except the one being examined (i.e., setting the volume of the specified output to 0). We then divide this incremental cost by the specified output's volume to obtain its associated average incremental cost. Because the average incremental cost is a function of all the regressors in our specified equation and, therefore, differs across programs, we take the average across all programs.
In estimating marginal and average costs, we retransformed the predicted total annual costs to its original scale of dollars using a smearing estimate (Duan 1983). The retransformation of the predicted annual total cost is necessary because our model is log–linear with the Ln of annual total costs as the dependent variable, and to simply exponentiate the predicted logged total costs would result in a biased predictor. Rather, we multiplied the exponent of the predicted logged total cost by a common smearing factor equal to the mean of the residual (Duan 1983).3
We also evaluated ray economies of scale for our multiproduct cost function. Ray economies of scale is defined as the cost saving from an increase in the aggregate output when the output mix remains constant (Panzar and Willig 1977). This measure is calculated as the reciprocal of the sum of the cost elasticities for the individual service outputs, and this measure was evaluated at mean levels. If the ray economies of scale measure is greater than, equal to, or less than 1, then returns to scale are said to be increasing, constant, or decreasing (Baumol, Panzar, and Willig 1982).
RESULTS
Table 1 shows the weighted descriptive statistics of the dependent and explanatory variables. The mean annual total cost is $916,355 (year 2000 dollars), and the average cost per patient day is $11.53 which is similar to per-day methadone treatment cost estimates reported in the literature that typically range from about $10.50 to $13 per day (e.g., SAMHSA, 2003; Flynn, Kristiano, and Porto, 1999). Mean annual patient days is 86,734, which implies an average daily census of about 238 patients (86,734/365). The mean counseling, intake service, case management, and ongoing medical service hours provided per year is 5,813; 1,162; 1,949; and 1,286. The mean counselor wage is $14.89; the mean nurse wage is $19.96; and the mean monthly rent is $1,132.
Table 1.
Means of Analysis Variables (Weighted)
| n=159 | Mean | SE |
|---|---|---|
| Total costs (2000$) | $916,355 | $103,573 |
| Cost per patient day (2000$) | $11.53 | $0.74 |
| Output | ||
| Annual number of patient days | 86,734 | 5,889 |
| Average daily patient census | 238 | 16.13 |
| Annual hours of counseling (CN) | 5,813 | 493 |
| Annual hours of intake services (INT) | 1,162 | 79 |
| Annual hours of case management (CM) | 1,949 | 233 |
| Annual hours of ongoing medical services (OMS) | 1,286 | 147 |
| Input prices ($2000) | ||
| Counselor wage | $14.89 | $0.65 |
| Nurse wage | $19.96 | $0.46 |
| Monthly rent for space | $1,132 | $37.85 |
| Program characteristics (% of programs) | ||
| Private, for-profit | 46.8% | 7.1% |
| Located in large urban area | 66.3% | 5.6% |
| Located in medium-sized urban area | 25.9% | 4.9% |
| Located in small-sized urban area | 7.9% | 2.1% |
| Part of larger parent organization | 70.8% | 5.9% |
| JCAHO or CARF accredited | 22.0% | 4.6% |
| Patient case mix | ||
| Percentage nonwhite | 41.6% | 3.3% |
| Percentage uninsured | 44.9% | 4.4% |
| Percentage on Medicaid | 35.1% | 5.6% |
| Percentage dually diagnosed (percentage of programs within each category) | ||
| ≤10% | 19.6% | 4.4% |
| 11–40% | 43.5% | 5.1% |
| >40% | 14.0% | 2.4% |
| Unknown—not assessed | 22.5% | 4.2% |
SE, standard error.
The majority of programs are nonprofit/public (53 percent) and located in either large urban (66 percent) or medium-sized urban (26 percent) areas. Most programs reported being part of a larger parent organization (71 percent), and only 22 percent of the programs were accredited. Most programs have patients with limited financial resources as indicated by the finding that the average program had 35 percent of its patients on Medicaid and 45 percent of its patients reporting being uninsured. Most programs report racial/ethnic diversity in their programs with the average program reporting that 42 percent of their patient population was nonwhite. Patients with both substance abuse and mental health problems were also not uncommon. Fourteen percent of the programs reported that >40 percent of their patient population was dually diagnosed with a substance abuse and mental health problem. Another 44 percent of programs reported that between 11 and 40 percent of their patient population was dually diagnosed.
Multivariate Results
Table 2 presents results from the multivariate model that includes annual patient days as the output variable (column 1). We found that average cost per patient day is negatively associated with patient days (p<.05) and positively associated with patient days squared (p<.01). These estimates suggest that average costs are initially lower for larger programs up to a certain point, and beyond that point average costs increase (a U-shaped relationship). To help interpret these estimates, we evaluated the elasticity of total cost to a change in patient days and found that the elasticity evaluated at the mean is 0.82; that is, a 10 percent increase in mean annual patient days is associated with an 8.2 percent increase in total annual cost. The estimated elasticity varies with output as indicated by the statistically significant squared term for number of patients. We conducted a statistical test to determine whether the estimated elasticity is statistically different from 1 (i.e., no economies of scale), and we found that this difference is statistically significantly different from 1 (p<.01).
Table 2.
Cost Function Results
| Patient Days | Selected Services | |||
|---|---|---|---|---|
| Dependent Variable=Ln(Total Annual Cost) | Coefficients | SE | Coefficients | SE |
| Output | ||||
| Ln(annual number of patients) | −2.551** | 0.961 | — | — |
| Ln(annual patients) squared | 0.148*** | 0.043 | — | — |
| Ln(annual counseling hours) | — | — | 0.326*** | 0.038 |
| Ln(annual counseling hours) squared | — | — | 0.048 | 0.025 |
| Ln(annual case management hours) | — | — | 0.064*** | 0.011 |
| Ln(annual case management hours) squared | — | — | 0.017*** | 0.004 |
| Ln(annual intake hours) | — | — | 0.038 | 0.028 |
| Ln(annual intake hours) squared | — | — | 0.009 | 0.005 |
| Ln(annual ongoing medical hours) squared | — | — | 0.099*** | 0.020 |
| Ln(annual ongoing medical hours) squared | — | — | 0.039*** | 0.007 |
| Service interactions | ||||
| Ln(annual CN) × Ln(annual CM) | — | — | 0.002 | 0.016 |
| Ln(annual CN) × Ln(annual INT) | — | — | −0.035 | 0.024 |
| Ln(annual CN) × Ln(annual OMS) | — | — | −0.058 | 0.038 |
| Ln(annual CM) × Ln(annual INT) | — | — | 0.013 | 0.014 |
| Ln(annual CM) × Ln(annual OMS) | — | — | −0.009 | 0.009 |
| Ln(annual INT) × Ln(annual OMS) | — | — | 0.021 | 0.018 |
| Input prices | ||||
| Ln(counselor wage) | 0.612*** | 0.172 | 0.595*** | 0.167 |
| Ln(nurse wage) | −0.037 | 0.345 | 0.032 | 0.381 |
| Ln(monthly rent for space) | 0.145 | 0.183 | 0.310 | 0.195 |
| Program characteristics | ||||
| For-profit | −0.110 | 0.065 | −0.153** | 0.071 |
| Medium urbanicity | 0.042 | 0.086 | −0.019 | 0.086 |
| Small urbanicity | −0.302 | 0.165 | −0.292 | 0.218 |
| Not part of larger parent organization | −0.136** | 0.059 | −0.009 | 0.065 |
| JCAHO or CARF accredited | 0.072 | 0.062 | 0.101 | 0.063 |
| Patient case mix | ||||
| Percentage nonwhite | 0.001 | 0.001 | 0.001 | 0.001 |
| Percentage dually diagnosed | ||||
| 11–40% | 0.045 | 0.076 | −0.023 | 0.078 |
| >40% | 0.022 | 0.101 | −0.011 | 0.081 |
| Unknown—not assessed | −0.072 | 0.088 | 0.002 | 0.081 |
| Percentage uninsured | −0.0003 | 0.001 | −0.002 | 0.001 |
| Percentage on Medicaid | 0.002 | 0.001 | −0.0004 | 0.002 |
| Intercept | 3.218*** | 1.146 | 5.687*** | 1.213 |
n=159.
p<.05
p<.01.
We also find that total annual cost was positively associated with counselor wage (p<.01). A 10 percent increase in counselor's wage is associated with a 6 percent increase in total annual cost. The effect of monthly rent is positive but small in magnitude and statistically insignificant. Although nurse's wage is negatively associated with total annual cost (counter to our expectations), it is not statistically significant. Only one of the other covariates in the model is statistically significant. Total annual cost is less for programs that are not part of a larger parent organization (p<.05). Possibly, this variable is capturing more or better services being offered by programs that are part of a larger organization or reflects a more costly case mix for these programs.
Table 2 also presents results for the second specification in which we replace the aggregate output measure of patient days with selected services (column 2). We find that counseling, case management, and ongoing medical services all have a positive and significant effect on total costs (p<.01). We estimated mean elasticities of 0.53 for counseling, 0.09 for intake services, 0.32 for case management, and 0.20 for ongoing medical service, although, our parameter estimates show that intake service does not have any significant effect on total costs. Thus, the effect of individual services is not great with a 10 percent increase in counseling, case management, and ongoing medical services resulting in a 5, 3, and 2 percent increase in total annual costs. Statistical tests revealed that these elasticities were statistically significantly different from 1 (p<.01). We also find that the included interaction terms for the services are not statistically significantly different from 0; thereby, yielding weak cost complementarities that are not different from 0 across services. These findings suggest that methadone programs may realize local economies of scope (weakly) in producing different types of services from similar inputs.
As with the patient days results, we also find that total annual cost was positively associated with counselor wage (p<.01), but, again, neither monthly rent nor nurse's wage is statistically significant. However, unlike the patient days results, we do not find a significant association between total cost and whether programs are part of a larger parent organization. But we do find a negative and statistically significant association between total cost and for-profit programs. Compared with nonprofit/public programs, for-profit programs are associated with lower total costs. Possibly, this variable is capturing differences in costs for other inputs that are not included in the specification or it may be capturing differences in patient case mix.
Table 3 shows that for patient days the marginal cost is increasing with output while average cost is decreasing. Furthermore, marginal cost is below average cost at each of our output levels. For example, the estimated average and marginal cost of an additional patient day for a medium-sized methadone treatment program is $10.20 and $7.82 compared with $12.73 and $7.24 for a small program. These findings suggest that larger methadone programs benefit from economies of scale as illustrated in the decreasing average costs.
Table 3.
Estimated Average Cost and Marginal Costs for Selected Output
| Volume of Output* | Average Cost per Patient-Day (SE†) | Marginal Cost per Patient-Day‡ (SE†) | Average Incremental Cost for Counseling Hour§ (SE†) | Marginal Cost Counseling Hour§ (SE†) | Average Incremental Cost for Case Management Hour¶ (SE†) | Marginal Cost Case Management Hour¶ (SE†) | Average Incremental Cost for Ongoing Medical Service Hour∥ (SE†) | Marginal Cost Ongoing Medical Service Hour∥ (SE†) |
|---|---|---|---|---|---|---|---|---|
| At mean | 9.80 (0.21) | 8.09 (0.18) | 150.54 (4.92) | 89.36 (2.92) | 170.61 (5.05) | 153.20 (4.54) | 312.82 (8.45) | 157.71 (4.26) |
| Low | 12.73 (0.28) | 7.24 (0.16) | 250.04 (8.18) | 129.39 (4.23) | 405.92 (12.02) | 487.98 (14.45) | 763.51 (20.62) | 298.51 (8.06) |
| Medium | 10.20 (0.22) | 7.82 (0.17) | 170.03 (5.56) | 97.14 (3.18) | 250.77 (7.43) | 245.23 (7.26) | 417.76 (11.28) | 197.25 (5.33) |
| High | 9.40 (0.20) | 8.67 (0.19) | 113.49 (3.71) | 70.58 (2.31) | 145.42 (4.31) | 125.93 (3.73) | 257.68 (6.77) | 133.01 (3.44) |
Volumes for low, medium, and high output are based on the unweighted variable distribution at 25, 50, and 75 percentiles.
SE estimated using Stata's bootstrap technique (StataCorp, 2003).
Low, medium, and high annual patient day volumes are 36,500, 71,175, and 1,20,450 representing average daily patient censuses of 100, 195, and 330 patients. Average patient-day volume is 86,870 representing an average daily census of 238 patients.
Low, medium, and high annual hours of counseling are 2,392, 4,368, and 7,540 annual hours. Average volume is 5,721.
Low, medium, and high annual hours of case management are 419, 1,040, and 2,496 annual hours. Average volume is 1,921 annual hours.
Low, medium, and high annual hours of ongoing medical services are 260, 832, and 1,872 annual hours. Average volume is 1,296 annual hours.
We also estimated the average incremental costs and marginal costs associated with different levels of service hours—average, low, medium, and high—for those services in which the estimated regression coefficients are statistically significant, with other services at mean values. These results (see Table 3) show that both the average and marginal costs are decreasing as output volume increases for counseling, case management, and ongoing medical service. However, the estimated measure of ray economies of scale associated with our multiproduct cost function is 0.89 indicating that returns to scale are decreasing for these selected services. We conducted a statistical test to determine whether this measure is statistically different from 1 (i.e., no economies of scale), and we found that this difference is statistically significantly different from 1 (p<.01).
DISCUSSION
Although a number of studies examine the total and per-person costs of substance abuse treatment, few have examined how treatment costs are associated with program output and the prices of program inputs. This study is the first to examine the determinants of the costs of providing methadone treatment.
Using a multistate sample of 159 methadone treatment programs, we find that greater patient days are associated with higher total annual cost for methadone treatment programs. For a program with mean annual patient days of 238 patients, our findings indicate that a 10 percent increase in average patient daily census is associated with an 8.2 percent increase in total annual cost. Our results also indicate that the average cost per patient day decreases with increases in patient days.
This finding parallels that of Duffy et al. (2004), who found a similar relationship between annual admissions and total annual cost in a study of outpatient nonmethadone treatment programs.4 In their study, Duffy et al. found that a 10 percent increase in output (as measured by admissions) was associated with a 6.7 percent increase in annual treatment costs.
In the broader health care costs literature, researchers have interpreted estimates of the relationship between treatment cost and size by referring to the concept of economies of scale (e.g., Grannemann, Brown, and Pauly 1986). Economies of scale are realized when long-run average costs fall as output increases, where the long-run is defined by the period of time over which programs can change all inputs (e.g., number of staff, size of facility) in providing care to patients. As noted above, in our single-product specification we find that average cost decreases with increasing output. This suggests that economies of scale may be present in the production of patient days for outpatient methadone treatment. Larger programs may be less costly on a per-person day basis than smaller ones. However, the decision for smaller programs to merge to achieve economies of scale should only be taken in light of other factors, such as the impact on patient access. For example, small programs located in rural or less densely populated areas may not be able to expand output because of their limited market size. Closing these programs or moving them to merge with larger programs may decrease patient access and increase patients' burden in getting to larger more distant-merged programs.
However, policy makers and providers may want to consider the possibility of consolidating small or medium-sized programs located in medium-sized and large urban markets to realize potential cost savings from economies of scale. Depending on the location of programs and the availability of transportation to program clinics, such mergers may be possible without harming access. Indeed, for publicly funded patients such mergers could increase access if the merger increases the number of available subsidized slots. A smaller program may be geographically more accessible, but it may lack subsidized slots, and therefore, be financially unavailable to such patients. Consolidating programs to generate economies of scale might allow a given program budget to support more funded slots making treatment financially available, although this benefit may come with the tradeoff that the patient may face greater travel time and transportation costs. Future research should consider the implications of this tradeoff and its impact on program and patient costs.
Our findings indicate that total annual cost is positively related to counselor wages. This finding concurs with economic theory. Surprisingly, neither nurse wages nor monthly building space costs had a significant association with total costs. Furthermore, only one of the measures capturing program characteristics had a statistically significant association with total costs. Total annual cost was negatively associated with a program not being part of a larger parent organization. As noted above, programs that are part of a larger parent organization may have higher administrative overhead or they may offer a greater variety or scope of services than programs that are not part of a larger parent organization. Neither urbanicity of the program location, accreditation status, nor ownership status were significantly associated with total annual cost. This finding mirrors that of Duffy et al. (2004) who found that case-mix measures were not statistically significant in their examination of costs of nonmethadone outpatient substance abuse programs.
In our multiproduct specification, we found that proportionate increases in service outputs did not lead to cost savings as indicated by our ray economies of scale measure. This finding suggests that the mix of services produced by a methadone program may affect their overall cost efficiency.
Finally, our examination of local economies of scope indicates that methadone programs do not gain much efficiency from producing different services from similar inputs. This finding is not surprising given the nature of methadone treatment. Unlike hospitals in which different services are distinct and target different patients (e.g., cardiac care versus obstetrics), counseling, intake service, case management, and ongoing medical service are parts of an overall package of care that methadone clinics offer.
The findings in this paper face two main limitations that indicate directions for future research. First, the data contained a limited number of variables for program and patient characteristics, and these variables may not capture important differences in programs (e.g., quality). Future research should attempt to include additional program and patient case-mix differences. Second, these data provide information only on the cost of supplying methadone treatment but not on the benefits of that treatment. To provide guidance on the optimal scale of operations for methadone treatment programs, we need to compare the benefits of treatment with its costs. Thus, like many other estimates of cost functions in the literature, our findings do not provide definitive policy conclusions on whether methadone programs should expand or merge. A natural extension of this work would be to combine treatment cost data with measures of patient outcomes to assess the cost effectiveness of alternative “doses” of treatment.
Despite these limitations, this study is important for several reasons. First, it advances our current knowledge of methadone treatment costs and associated cost factors. This information is a crucial step toward understanding what constitutes treatment costs and providing cost-effective treatment. Furthermore, these findings provide useful information to treatment providers and policy makers so that they may be better able to target limited funding resources to essential treatment areas. Finally, researchers and policy makers may find this study useful in examining the cost implications associated with changes in treatment output, inputs, and patient case mix.
Acknowledgments
This study was funded by a grant from the National Institute on Drug Abuse (R01–DA15655). This article does not necessarily represent the policies or the positions of the National Institute on Drug Abuse (NIDA) or RTI International and no official endorsement by NIDA or RTI is intended or should be inferred.
NOTES
We attempted to include annual admissions in addition to patient days in our patient days' model. However, admissions were found to be highly collinear with patient days, and we were unable to estimate this model.
The problem of multicollinearity was severe between linear and squared output variables and interaction terms in our service specification. To deal with this problem and disentangle the effects of the linear and squared terms on the dependent variable, we orthogonalized the squared term to make it statistically independent of its linear counterpart. To do this, we regressed the squared term on the linear term and used the estimated residual from this regression in our main equation in place of the original squared term. A similar procedure was followed to orthogonalize the interaction terms.
Manning (1998) has shown that in the presence of heteroskedasticity, use of a common smearing factor yields biased estimates of predicted costs. We tested for the presence of heteroskedasticity in our model, and the results of these tests indicated that we could not reject the null hypothesis of homoskedasticity. Therefore, our use of a common smearing factor to obtain our estimates for predicted total costs should not yield biased estimates.
We conducted a similar analysis for methadone treatment programs using log annual admissions instead of annual patient days. We found similar results pertaining to output, although the effect was smaller in magnitude. A 10 percent increase in annual admissions was associated with a 2.8 percent increase in total annual costs. These results are available from the corresponding author upon request.
REFERENCES
- Andersen C K, Andersen K, Kragh-Sorensen P. Cost Function Estimation. The Choice of a Model to Apply to Dementia. Health Economics. 2000;9(5):397–409. doi: 10.1002/1099-1050(200007)9:5<397::aid-hec527>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Baumol W J, Panzar J C, Willig R D. Contestable Markets and the Theory of Industry Structure. Harcourt Brace Jovanovich: New York; 1982. pp. 50–7.pp. 71–9. [Google Scholar]
- Bilodeau D, Crèmieux P -Y, Oullette P. Hospital Cost Function in a Non-Market Health Care System. Review of Economics and Statistics. August 2000;28(3):489–98. [Google Scholar]
- Breyer F. The Specification of a Hospital Cost Function. A Comment on the Recent Literature. Journal of Health Economics. 1987;6(2):147–57. doi: 10.1016/0167-6296(87)90004-x. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (BLS) State Occupational Employment and Wage Estimates”. [December 15, 2005];2005 Available at http://www.bls.gov/bls/blswage.htm.
- Butler M A, Beale C L. Rural-Urban Continuum Codes for Metro and Non-Metro Counties, 1993. Washington, DC: U.S. Department of Agriculture, Economic Research Service; 1994. Staff Report No. AGES 9425. [Google Scholar]
- Carey K. A Panel Data Design for Estimation of Hospital Cost Functions. Review of Economics and Statistics. 1997;79(3):443–53. [Google Scholar]
- Duan N. Smearing Estimate. A Nonparametric Retransformation Method. Journal of the American Statistical Association. 1983;78:605–10. [Google Scholar]
- Duffy S Q, Dunlap L J, Feder M, Zarkin G A. Health Services Utilization by Individuals with Substance Abuse and Mental Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2004. A Hybrid Cost Function for Outpatient Nonmethadone Substance Abuse Treatment Facilities; pp. 133–53. [Google Scholar]
- Flynn P M, Kristiansen P L, Porto J V. Costs and Benefits of Methadone Treatment for Women and Men Who Left before or Were Still in Treatment at Follow-up.”. Presented at the Annual Meeting of the College on Problems of Drug Dependence; June 1999; Acapulco, Mexico. 1999. [Google Scholar]
- Goodman A C, Holder H D, Nishiura E, Hankin J R. An Analysis of Short-Term Alcoholism Treatment Cost Functions. Medical Care. 1992;30(9):795–810. doi: 10.1097/00005650-199209000-00004. [DOI] [PubMed] [Google Scholar]
- Goodman A C, Nishiura E, Hankin J R. Short Term Drug Abuse Treatment Costs and Utilization. A Multi-Employer Analysis. Medical Care. 1998;36(8):1214–27. doi: 10.1097/00005650-199808000-00009. [DOI] [PubMed] [Google Scholar]
- Grannemann T W, Brown R S, Pauly M V. Estimating Hospital Costs. A Multiple-Output Analysis. Journal of Health Economics. 1986;5(2):107–27. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Harwood H J, Kallinius S, Liu C. Do Larger Residential Service Delivery Units Have Lower Costs? Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. National Evaluation Data Service Technical Report. [Google Scholar]
- McAvinchey I D, Yannopoulos A. A Cost Function Approach to the Choice between Private and Public Acute Health Care Provision. Scottish Journal of Political Economy. May 1994;41(2):194–211. [Google Scholar]
- McNamee P, Gregson B A, Wright K, Buck D, Bamford C H, Bond J. Estimation of a Multiproduct Cost Function for Physically Frail Older People. Health Economics. 1998;7(8):701–10. doi: 10.1002/(sici)1099-1050(199812)7:8<701::aid-hec382>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Nyman J A, Dowd B E. Cost Function Analysis of Medicare Policy. Are Reimbursement Limits for Rural Home Health Agencies Sufficient? Journal of Health Economics. 1991;10(3):313–27. doi: 10.1016/0167-6296(91)90032-i. [DOI] [PubMed] [Google Scholar]
- Panzar J C, Willig R D. Economies of Scale in Multi-Output Production. Quarterly Journal of Economics. 1977;91(3):481–93. [Google Scholar]
- Reinhardt U. A Production Function for Physician Services. Review of Economics and Statistics. February 1972;54(1):55–66. [Google Scholar]
- Rosko M D, Broyles R W. The Economics of Health Care: A Reference Handbook. New York: Greenwood Press; 1988. [Google Scholar]
- RTI International. Evaluation of the Opioid Treatment Program Accreditation Study: Final Report (Contract No. 270-97-7022) Bethesda, MD: Center for Substance Abuse Treatment; 2003. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 8. College Station, TX: StataCorp LP; 2003. [Google Scholar]
- Wholey D, Feldman R, Christianson J B, Engberg J. Scale and Scope Economies among Health Maintenance Organizations. Journal of Health Economics. 1996;15(6):657–84. doi: 10.1016/s0167-6296(96)00499-7. [DOI] [PubMed] [Google Scholar]
- Zarkin G A, Dunlap L J, Homsi G. The Substance Abuse Services Cost Analysis Program (SASCAP). A New Method for Estimating Drug Treatment Services Costs. Evaluation and Program Planning. 2004;27(1):35–43. [Google Scholar]


