Abstract
Objective
To examine the effect of nonprice competition among managed care plans on the quality of care in the New York SCHIP market.
Data Sources
U.S. Census 2000; 2002 New York State Managed Care Plan Performance Report; and 2001 New York State Managed Care Annual Enrollment Report.
Study Design
Each market is defined as a county, and competition is measured as the number of plans in a market. Quality of care is measured in percentages using three Consumer Assessment of Health Plans Survey and three Health Plan Employer Data and Information Set scores. Two-stage least squares is applied to address the endogeneity between competition and the quality of care, using population as an instrument.
Principle Findings
We find a negative association between competition and quality of care. An additional managed care plan is significantly associated with a decrease of 0.40–2.31 percentage points in four out of six quality measures. After adjusting for production cost, a positive correlation is observed between price and quality measures across different pricing regions.
Conclusions
It seems likely that pricing policy is a constraint on quality production, although it may not be interpreted as a causal relationship and further study is needed.
Keywords: Nonprice competition, managed care, quality of care, SCHIP
The U.S. government is deeply involved in the health care market, and in the price control settings, one of the government's concerns is quality of care. Since managed care started expanding throughout the country in the 1980s, government and private organizations have been trying to develop quality measurement tools and monitor the quality of care. For example, the Consumer Assessment of Health Plans Survey (CAHPS®) and the Health Plan Employer Data and Information Set (HEDIS®) were developed to assess the quality of managed care plans in the 1990s. Starting in 1999, Congress has required the Agency of Healthcare Research and Quality (AHRQ) to produce an annual National Health Quality Report (AHRQ 2003).
In recent years, an increasing number of states have switched their Medicaid or State Children's Health Insurance Program (SCHIP) from fee-for-service to managed care (Kaiser Family Foundation 2001). For example, New York State and the State of Florida rely on managed care plans to provide health care for SCHIP enrollees. In New York State, mandatory Medicaid managed care has been implemented in about 30 counties (NYSDOH 2005). The New York State government sets the monthly capitation rate for participating managed care plans and releases an annual quality report of all the managed care plans operating in the state.
The relationship between quality of care and competition has been one of the focuses of researchers for the last several decades. Most prior studies are about hospital competition, which is subject to price control under the Medicare Prospective Payment System (PPS). Based on the data before 1983 when the PPS was implemented, many studies show a positive association between competition and quality or cost (e.g., Joskow 1980; Robinson and Luft 1985, 1987; Noether 1988). Those studies analyzing the data after 1983, however, provide mixed evidence on the relationship between competition and quality or cost because there are two forces at play: the PPS and the penetration of managed care. The PPS actually acts as a price control mechanism, and higher price is associated with higher quality if assuming the same market competition level, as shown in the study by Cutler (1995). Alternatively, if the price is held constant, increasing market competition would result in higher quality and higher cost. Theoretically, managed care penetration would lower the cost of care, but the PPS would lead to higher costs in more competitive markets. Not surprisingly, the evidence about cost or quality is mixed (e.g., Shortell and Hughes 1988; Zwanziger and Melnick 1988; Dranove, Shanley, and Simon 1992; Manheim, Bazzoli, and Sohn 1994; Kessler and McClellan 2000; Mukamel, Zwanziger, and Tomaszewski 2001; Gowrisankaran and Town 2003).
Because managed care plans have financial incentives to reduce cost at the expense of quality of care, the effect of managed care competition on quality is worthy of investigation. However, only a few studies have been conducted in this area. Using a national representative sample from the Community Tracking Study, Sommers and Wholey (2003) regress evaluation of physician thoroughness on health maintenance organization (HMO) competition and other control variables, and conclude that HMO competition increases the evaluation of physician thoroughness among HMO enrollees. Scanlon et al. (2005) assess the association between HMO competition and plan performance as measured by CAHPS and HEDIS, and find that competition is negatively correlated with three out of six quality domains. Another study using longitudinal data by Scanlon et al. (2006), however, shows that more HMO competition is associated with better overall ratings of health plans, but is not consistently correlated with HEDIS measures.
Despite the states' increasing dependence on managed care to provide comprehensive coverage for the low-income population, few studies have been conducted to examine the effect of nonprice competition on the quality of care. Nonprice competition means a situation where price does not play a role in market competition. Using the 2002 New York State Managed Care Plan Performance Report and 2001 Annual Managed Care Enrollment Report, we are able to assess the effect of nonprice competition on quality of care within the New York SCHIP market,1 which is subject to the price control from the state government.
CONCEPTUAL MODEL
In the price control settings, managed care plans have two incentives: to attract consumers and save cost. Everything else being equal, in the long run, an increase in competition would drive plans to use more resources to improve the quality of care without exceeding the fixed price. It is possible, in reality, that plans will employ other methods, such as risk selection and product differentiation. Owing to the pressure of competition, if some plans engage in risk selection, others will follow. At equilibrium, the risk distribution should be similar across plans in a market. Because the SCHIP coverage is the same across competitors, product differentiation should not be an issue here.
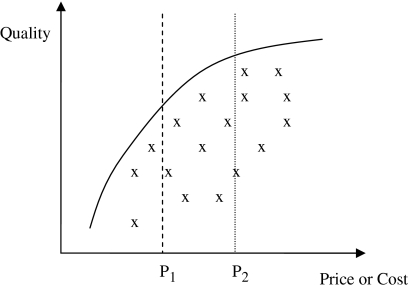
As shown in Figure 1, in a market where excess capacity exists, plans are distributed as the Xs in the figure. The curve represents the quality production frontier at each price (or cost) level.2 Consumers can choose a combination of price and quality that would maximize their utilities. If the regulation agency imposes a price control, say P1, then all the plans to the right of P1 will disappear because their production cost is greater than the fixed price as demonstrated in the case of nonprofit hospitals in Thorpe and Phelps (1990). Under the price control (P1), if consumers can perceive quality and are willing to respond to quality, all the plans in the market would try to move to the intersection of P1 and the quality production frontier.3 If the fixed price moves to P2, plans would try to move close to the new intersection of P2 and the quality production frontier. The average quality would increase if competition is held constant. When the fixed price is higher than the equilibrium price without regulation, excessive quality would be provided, which is exactly what happened before the deregulation in the airline industry when pub lounges and flight attendants were available (Pauly 2004).
Figure 1.
Price Control and Quality of Care.
When plans can choose their prices, competition might not necessarily lead to quality improvement. The average quality in a market depends on the consumer's preferences. Compared with the quality level under price regulation, competition could lead to higher quality with lower price, higher quality with higher price, or lower quality with lower price. The only impossible outcome from more competition is higher price with lower quality.
In New York State, however, price is not fixed across plans or markets. Each managed care plan requests a capitation rate for SCHIP enrollees for a certain contract period, and the state government sets price according to the plan's previous cost experience.4 The state is divided into nine regions for this purpose: New York City, Long Island, Mid-Hudson Region, Northern Metro Region, North East Region, Utica-Adirondack Region, Central Region, Finger Lakes Region, and Western Region. Some plans do request different rates for their branches in different pricing regions, while others do not. Within each region, the price is not the same across plans, and the range is about ±30 percent from the mean (NYSID 2006).
In this competition environment, if price does not vary across different markets or regions, then a positive correlation between competition and quality should be observed. But if price is different across markets or regions, then the association between competition and quality is unclear. It might be negative when competition is more intense in the markets with lower prices. In this study, we hypothesize that nonprice competition is positively correlated with quality of care.
METHODS
Data Sources
The following data are used for this analysis, which characterize the markets in 2001: the 2002 New York State Managed Care Plan Performance Report (NYSDOH 2002), the 2001 New York State Managed Care Annual Enrollment Report, and the U.S. Census 2000 data from FedStats (2005). The managed care plan performance measures come from the performance report, the plan enrollment information from the enrollment report, and the market characteristics from the U.S. Census data.
Market Definition
Each market is defined as a county within New York State, because the state government mandates that eligible children must enroll in a managed care plan operating within the county where they live. However, defining the competitors in a market is challenging since some plans had very small numbers of enrollees, e.g., <50. One approach is to include all the plans with at least one enrollee. A small number of enrollees in any plan might be due to chance or reporting errors, which would lead to an overestimation of the number of competitors in a market. Therefore, we adopt a more reasonable method by including only those plans with at least 1 percent of the SCHIP market share. In order to avoid excluding plans that did operate in a market, we also include plans with <1 percent of the SCHIP market share but with at least 10 percent of the overall managed care market share. A sensitivity analysis is conducted by including every plan with nonzero SCHIP enrollment, and it fails to change the main conclusions.
Statistical Model
The association between market structure (market concentration or the number of competitors) and market performance (cost, price, or quality) is endogenous, because they affect each other. In order to avoid the endogeneity problem, we apply two-stage least squares (2SLS) method. We use market population as an instrument, because population is one of the primary factors that determine the demand for health insurance, and does not affect quality directly.
Health plan quality is basically derived from physician quality, one might argue that physician competition could invalidate the instrument. It is true that physicians drive plan quality. The question is whether physician competition will uniformly affect quality of care in markets with different sizes. Little evidence exists in the literature on the relationship between physician competition and quality of care. Although the debate still exists, prior empirical studies about physician geographic distribution have shown that physicians are distributed according to demand (e.g., see Newhouse 1990 for a review). It is true that the physician/population ratio is higher in metropolitan areas, but in areas with a population >1 million, physicians' work time is about 10 percent less and their real income nearly 15 percent less, which reflects their preference of living in cities and does not necessarily mean physicians compete more intensely for patients (Newhouse et al. 1982). Based on the existing evidence, it is possible but not likely that the physician market competition would invalidate market population as the instrument.
Larger markets allow more firms to operate at efficient cost levels, but this effect on quality is also by affecting the number of competitors. We also perform Sargan's overidentification tests (Murray 2006) and they do not show significant results for six quality measures based on the 5 percent significance level except for “provider communication” with a p-value of .01.
In the first stage, the number of plans is regressed on the instrument and other market characteristics. The instrument consists of two variables: population and poverty rate, because both variables are key elements in determining the target population, which is a low-income population.
Conceptually, the number of plans in a market is determined by both demand and supply factors. Population, income, education, and average travel time have an effect on the demand, while housing cost, wages, capital cost, and production technology affect the supply. However, income, education, housing cost, and wages are highly correlated, with the correlation coefficients varying from 0.73 to 0.91. Accordingly, we only put income in the regression model. Travel time is a proxy for traveling cost, which can affect the demand for medical services and as a result the demand for health insurance. It is reasonable to assume that the capital cost and the production technology are the same in the state. The model is as follows, where βs are parameters and ɛ1 is the error term:
In the second stage, quality measures are modeled as a linear function of the predicted number of plans from the first stage regression, and other plan level characteristics, including having a commercial product line, the total number of enrollees, and a variable indicating whether a plan operates in at least two different regions in the state (New York City, Long Island, Hudson Valley, Northeast, Central, or Western regions [NYDOH 2002]). Since most plans operated in multiple markets and no market-specific measures are available, the plan is used as the analysis unit for the second stage regressions. For each plan, the variable of “predicted number of plans” is calculated as an average weighted by the plan's enrollment in different markets. Other market characteristics are computed similarly when applied. Profit status and market-level education are tested, and do not enter the final model based on the information criteria. The second stage model is as follows, where δs are parameters and ɛ2 is the error term:
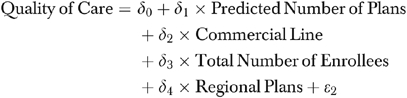 |
Each quality measure is regressed on the independent variables separately in the second stage analysis. Because the quality measures are correlated, we try two alternative methods: (1) using a seemingly unrelated regression; (2) aggregating the measures as one composite index and regressing this index on the independent variables. Neither analysis changes the main conclusions.
Variable Definitions
Since the purpose of using market population is to approximate the effective demand for health insurance, two variables are used to represent potential eligible enrollees: the population under 19 years of age and the poverty rate for individuals <18. The reason we do not multiply these two variables is that there is not an exact cutoff point in terms of eligibility. Every child below 19 years of age can join the program, but the premium varies depending on family income. The lower the family income is, the lower the premium. Therefore, multiplying two variables would result in a loss of information. Average travel time is measured as the average time to work in minutes for those 16 and older, and per capita income is used.
The Herfindahl–Hirschman index (HHI) has been frequently used in the previous literature. In this study, market competition is measured by the number of plans in a market because our data show a larger explanatory power for the number of plans than that for HHI, and a sensitivity analysis using HHI does not change the main conclusions. In the first stage regression, the R2 for the number of plans is 73.1 percent, while that for HHI is only 33.1 percent.
To measure the quality level for pediatric care, three CAHPS and three HEDIS measures are used, including “provider communication,”“problems with getting care needed,”“problems with services,”“preventive care visits” for children between 3 and 6 years of age, “use of appropriate medications for children with asthma” between 5 and 18 years, and “child immunization,” because these variables provide information on pediatric care quality and have fewer missing values. The first three measures are from CAHPS and the last three from HEDIS.
When these measurements are not available for SCHIP, those of Medicaid or commercial lines are used.5 In the 2002 plan performance report, only Medicaid and commercial CAHPS measurements are available. Medicaid CAHPS measures are used because they are also for the low-income population, and the missing values for four out of 29 plans are imputed from commercial CAHPS measurements. All HEDIS measures are SCHIP specific, with 3.4 percent imputed from commercial and 4.6 percent from Medicaid measurements.
RESULTS
Descriptive Statistics
There are 62 markets (counties) in New York State, and the average number of plans is 3.79, varying from 1 to 13, as shown in Table 1. In terms of market size, there is an enormous variation in the number of SCHIP enrollees, which ranges from 199 to about 114,000 with an average of 8,615 enrollees. All five markets in New York City are among the largest, including Richmond (SI), Brooklyn, Queens, Bronx, and Manhattan, with about 11 plans operating in each county. Most small markets with only one or two SCHIP plans are in central or western New York, accounting for about one-third of the markets.
Table 1.
Summary Statistics at the Market Level and the Plan Level
| Market-Level Variables* | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|
| Number of plans | 3.79 | 2.85 | 1 | 13 |
| Number of SCHIP enrollees | 8,615 | 21,161 | 199 | 113,528 |
| Population under 19 years | 84,052 | 143,656 | 1,165 | 732,423 |
| Percentage of under 18 years | ||||
| Below federal poverty level | 15.49 | 6.11 | 4.5 | 41.5 |
| Per capita income (in 1999 U.S. dollars) | 19,984 | 5,114 | 13,959 | 42,922 |
| Average travel time of 16 years and older (in minutes) | 25.28 | 6.41 | 17.8 | 43.9 |
| Plan-level variables† | ||||
| Total number of enrollees | 120,274 | 182,082 | 4,810 | 733,783 |
| Number of SCHIP enrollees | 18,417 | 19,071 | 2,161 | 88,671 |
| Plan performance scores in percentages | ||||
| Provider communication | 86.79 | 3.64 | 79 | 95 |
| Problems with getting care needed‡ | 22.14 | 5.12 | 11 | 34 |
| Problems with services‡ | 36.52 | 6.00 | 26 | 52 |
| Preventive care visits | 70.66 | 5.92 | 59 | 83 |
| Use of appropriate medications for children with asthma | 58.14 | 10.72 | 21 | 72 |
| Child immunization | 79.04 | 10.48 | 51 | 95 |
All the variables come from U.S. Census 2000 representing market characteristics in year 1999, except “Number of Plans,” which is derived from the 2001 New York State Managed Care Annual Enrollment Report. There are 29 plans and 62 markets (counties) in total.
All the variables come from the 2002 New York State Managed Care Plan Quality Report.
A lower score is preferred.
SCHIP, State Children's Health Insurance Program.
There are 29 plans in the SCHIP program with tremendous variation in plan size. Some small plans only enroll about 5,000 individuals per year, while large plans have about 700,000 enrollees. The average number of SCHIP enrollees is about 18,000 (Table 1). Among these plans, 75.86 percent are nonprofit and 58.62 percent have business in at least two regions, with 44.8 percent having a commercial product line.
Plan performance scores are presented in Table 1. The variation in “provider communication” is relatively small with a standard deviation of 3.64 and an average of 86.79. The HEDIS scores have a larger variation, especially in “use of appropriate medications for children with asthma” and “child immunization,” with standard deviations being about 10.
Multiple Regression Analysis
In the first-stage regression, as shown in Table 2, both instruments have a significant positive effect because a larger population would create a greater demand for health insurance. Specifically, every additional plan requires about 200,000 children under age 19, while every 6.5-unit increase in percentage in the poverty level for individuals age <18 would lead to a new entry into the market. The higher the income is, the higher the demand for health insurance, which is consistent with the previous literature. Intuitively, more travel time means greater traveling cost and less demand for medical care and health insurance. However, travel time is positively correlated with the number of plans, which is possibly driven by New York City where travel time is longer and the number of plans is much greater than in other areas.
Table 2.
First Stage Regression: Predicting the Number of Plans†
| Variable | Coefficient | Standard Error |
|---|---|---|
| Population under 19 years (in 1,000s) | 0.0047** | 0.0021 |
| Percentage of under 18 years | ||
| Below federal poverty level | 0.1529*** | 0.0385 |
| Per capita income (in $1,000) | 0.1486*** | 0.0450 |
| Average travel time of 16 years and over (in minutes) | 0.1814*** | 0.0421 |
| Intercept | −6.5262*** | 1.4389 |
| N | 62 | |
| R2 (%) | 73.09 | |
Significant at the 5% level;
Significant at the 1% level.
An F-test for both instruments is highly significant (p<.001), and two instruments can explain 56.04% of the variation in the dependent variable.
In the second-stage regressions (Table 3), it is shown that competition is negatively correlated with quality of care. This result is consistent across all quality measures: more competition (larger predicted number of plans) is associated with lower quality of care (lower scores in “provider communication,”“preventive care visits,”“use of appropriate medications for children with asthma,” and “child immunization”; higher scores in “problems with getting care needed” and “problems with services”). The coefficients of the predicted number of plans are statistically significant at the 10 percent level in all equations except for “preventive care visits” and “use of appropriate medications for children with asthma.” The negative effect of adding a new plan in a market varies from 0.34 to 2.31 percentage points. Being a regional plan is associated with higher quality in “provider communication.” Surprisingly, having a commercial product line is associated with lower quality in “problems with services,” which is also the case for larger plans.
Table 3.
Second Stage Regressions: Association between Competition and Quality of Care (Standard Errors in Parentheses)
| Provider Communication | Problems with Getting Care Needed† | Problems with Services† | Preventive Care Visits | Appropriate Medications for Asthma‡ | Child Immunization‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Equations/Variables | OLS | 2SLS | OLS | 2SLS | OLS | 2SLS | OLS | 2SLS | OLS | 2SLS | OLS | 2SLS |
| Predicted number of plans | −0.3215** (0.1390) | −0.4080**(0.1617) | 0.7434*** (0.2018) | 0.9406*** (0.2385) | 0.5447* (0.2886) | 0.6741* (0.3342) | −0.2706 (0.3318) | −0.3814 (0.3829) | −0.0045 (0.5901) | −0.3396 (0.6704) | −1.9738*** (0.4075) | −2.3099*** (0.4655) |
| Regional plan§ | 2.7818** (1.1080) | 2.8368** (1.1209) | −1.0667 (1.6084) | −1.1929 (1.6531) | 2.0352 (2.3008) | 1.9474 (2.3162) | 0.6004 (2.6448) | 0.6585 (2.6537) | −3.6325 (6.3520) | −3.4752 (6.3399) | 1.9054 (3.7518) | 2.1928 (3.6983) |
| Having a commercial product line | 2.9251** (1.4087) | 2.4272 (1.4835) | −0.4318 (2.0450) | 0.7085 (2.1878) | 6.8805** (2.9252) | 7.6558** (3.0654) | 1.6683 (3.3625) | 1.0978 (3.5122) | 9.4006 (6.3107) | 8.018 (6.3031) | −3.9873 (3.4660) | −6.2382 (3.8772) |
| Total number of enrollees (log transformed) | −0.559 (0.4834) | −0.4457 (0.4890) | −0.832 (0.7017) | −1.0936 (0.7212) | −2.7999** (1.0037) | −2.9890*** (1.0105) | 0.1093 (1.1538) | 0.211 (1.1577) | 1.0982 (2.1106) | 1.2033 (2.2067) | 1.2188 (1.5133) | 1.8755 (1.6350) |
| Intercept | 92.4893*** (5.0621) | 92.0291*** (5.0284) | 25.9637*** (7.3484) | 27.0485*** (7.4157) | 58.1333*** (10.5114) | 59.0426*** (10.3904) | 70.5544*** (12.0830) | 70.4547*** (11.9048) | 44.0534* (22.2422) | 46.0067** (22.2068) | 82.7824*** (15.4255) | 78.5441*** (16.0083) |
| N | 29 | 29 | 29 | 29 | 29 | 29 | 29 | 29 | 28 | 28¶ | 28 | 28¶ |
| R2 (%) | 58.20 | 60.21 | 55.47 | 60.72 | 33.65 | 35.19 | 9.95 | 11.19 | 23.72 | 24.63 | 53.06 | 54.41 |
| Sargan's test: χ2-value (p-value) | 6.4695 (.0110) | 1.3255 (.2496) | 0.4486 (.5030) | 0.3765 (.5395) | 0.9766 (.3230) | 0.4102 (.5219) | ||||||
Significant at the 10% level;
Significant at the 5% level;
Significant at the 1% level.
A lower score is preferred.
Robust standard errors are used due to heteroskedasticity.
Operating at least in two different regions in New York State (New York City, Long Island, Hudson Valley, Northeast, Central, or Western regions according to NYDOH 2002).
Owing to missing values, the number of observations is <29. We check the model assumptions and they seem to be fine except that heteroskedasticity exists in the equations of “use of appropriate medications for children asthma” and “child immunization,” for which robust standard errors are used.
OLS, ordinary least squares without using instruments; 2SLS, two stage least squares.
The naïve models using simple ordinary least squares (OLS) show similar patterns, with the same significances for the coefficients of the predicted number of plans (Table 3). Among the four quality measures with significant effects of competition, simple OLS models bias the effect toward zero by about 20 percent.
Price Variation across Markets or Regions
As noted previously in the conceptual model, if a negative association between nonprice competition and quality is observed, it is quite possible that more competition exists in markets or regions with lower prices. It turns out that the average monthly premium does not vary much across different pricing regions, $123–$131 as of 2005 (NYSID 2006). However, if we use average median earnings as a measure for labor cost which is a major component of health care production cost, the variation in the price labor cost ratio (the average monthly premium divided by the average median earning) across pricing regions is more obvious, ranging from 2.81 to 4.81. More importantly, four out of six quality measures show a significant positive association with price labor cost ratio.6 The correlation coefficients are 0.82 (p=.01), −0.79 (p=.01), −0.05 (p=.89), 0.40 (p=.29), 0.77 (p=.02), and 0.67 (p=.05) for “provider communication,”“problems with getting care needed,”“problems with services,”“preventive care visits,”“use of appropriate medications for children with asthma,” and “child immunization,” respectively. More competition exists in the regions with lower price labor cost ratios, which is a precondition for observing a negative association between quality and competition.
DISCUSSION
We find a negative association between nonprice managed care competition and quality of care. Three previous studies of HMO price competition and quality of care provide mixed evidence, but the study by Scanlon et al. (2005) also shows a negative association between HMO competition and three out of six quality domains based on CAHPS and HEDIS measures. The state government sets prices based on a plan's previous cost experience, which is somewhat similar to the Medicare hospital pricing policy before the PPS. However, we do not observe a positive correlation between competition and quality of care as occurred in the hospital industry before 1983, which might be explained by several other potential factors that are worth examination.
Even if we use the 2SLS method with market population as an instrument to address the endogeneity problem, there still exists a concern that it is not sufficient. Simple OLS models show similar negative associations and result in a bias toward zero compared with 2SLS. For “provider communication” and “child immunization,” the coefficients are biased upward, while the coefficients for “problems with getting care needed” and “problems with services” are biased downward because lower scores are preferred for the later two measures. This is exactly what one would expect if competition, as measured by the number of plans, is positively correlated with the error term. We also try the instruments one at a time in the second stage regressions and the results are similar. Compared with 2SLS, the magnitudes of the coefficients of competition slightly increase when population is the only instrument, and slightly decrease when poverty level is the only instrument, but the significances are the same. Moreover, overidentification tests for different quality measures also support the validity of our instruments except for “provider communication.” Therefore, it is unlikely that the endogeneity problem has led to our findings.
Three HEDIS measures are SCHIP specific, while the CAHPS measures are not because the state does not conduct a member satisfaction survey for SCHIP separately. It is interesting that a negative association is observed both for HEDIS and CAHPS measures. There are three potential explanations. First, it is possible that the SCHIP product line quality might result from the spillover effect when health plans set the quality level for other product lines. It is not an easy task for plans to implement these separate decisions because different products often share the same group of providers, which is one of the reasons that the measures of other product lines are highly correlated with those of the SCHIP product line.
Second, SCHIP competition and prices are highly correlated with those of other product lines. Because population is one of the primary determinants of the demand for health insurance, it is highly possible that competition in different product lines is very similar. The state government uses plans' previous cost experience to set prices, and consequently, the prices could also be highly correlated to those of other product lines.
Third, the results could be affected by physician market competition. Health plans can affect physicians' quality of care through different management tools or contractual arrangements, but the extent to which a health plan can affect the physicians' quality at the market level remains largely unknown. In the physician market, competition generally takes the form of price competition, where more competition can lead to either higher or lower quality. Therefore, given the limited extent to which health plans can affect the providers' quality, the negative association between competition and quality in the health plan market might result from the same association in physician markets where more price competition could be associated with lower quality.
In addition to the possible explanations discussed above, there are limitations that would limit our ability to explain the findings. First, the quality measures used in this study are not risk adjusted. In other words, we are not able to tease out the consumers' effect on the quality of care. Second, the sample sizes are relatively small. Although the regressions have a fairly large explanatory power, there are only 62 markets in the first-stage regression and 29 in the second-stage regressions. New York State has been releasing managed care plan quality reports since 1994, and it is possible that we can conduct a longitudinal study. However, there are other issues with these data. For example, the quality measures change from year to year, and some plans have merged during a relatively long time frame.
Although further study is needed, it seems likely that pricing policy is a constraint on quality production, as suggested by the positive correlation between price labor cost ratio and quality of care across pricing regions and the absence of a positive association between nonprice competition and quality as was observed in the hospital industry before 1983. However, we should avoid a causal interpretation, and it is likely that before the state government started its policy, the quality distribution was similar to what we find here, and the policy itself has only been reinforcing this pattern.
Acknowledgments
The authors wish to thank Satya Pabuwal and Gary Teitel from the New York State Insurance Department, Guy Warner and Jacqueline Maston from the New York State Department of Health for providing information on the SCHIP and Medicaid quality management and the pricing policies. Thanks also go to Hao Yu, Peter Veazie, and two anonymous reviewers for their great comments and constructive suggestions.
Disclosures: There is no conflict of interest related to the article.
Disclaimers: The views expressed here are those of the authors and do not necessarily represent those of the University of Rochester.
NOTES
As of 2001, the New York SCHIP program included an expansion of Medicaid (Child Health Plus A) and a separate program (Child Health Plus B). In this study, SCHIP means Child Health Plus B only.
It is assumed that there is a positive correlation between cost and quality, which has not been established in the literature. As long as the health care production follows a typical production function, then the assumption is reasonable.
Farley et al. (2002a, b) show that the Medicaid population do respond to plan quality information if they actually read the quality report and understand it, although there is more evidence among employees in universities or large companies (e.g., see Beaulieu 2002; Scanlon et al. 2002; Wedig and Tai-Seale 2002).
The SCHIP pricing policy was obtained through personal communications with Satya Pabuwal and Gary Teitel from the New York State Insurance Department in January 2006 and June 2007. The 2006 plan rate application package is available at http://www.ins.state.ny.us/ihealth.htm.
Only seven plans have both commercial and Medicaid CAHPS measures, and the correlation coefficients for three CAHPS measures are 0.43, 0.52, and 0.86, respectively. Nearly 20 plans have both SCHIP and Medicaid HEDIS measures, the correlation coefficients for three HEDIS measures are 0.30, 0.65, and 0.80, respectively.
We include median earning in the second stage regressions and find that it does not significantly predict quality after controlling for other variables or contribute to the models based on Akaike's information criteria, but the association between quality and competition still holds. One possible explanation is that median earning is only a proxy for labor cost or production cost and it affects both the demand and the supply of health insurance.
REFERENCES
- Agency of Healthcare Research and Quality (AHRQ) “National Health Quality Report”. [December 3, 2005];2003 Available at http://www.qualitytools.ahrq.gov/qualityreport/archive/2003/download/documents/Quality_Report.pdf.
- Beaulieu N D. Quality Information and Consumer Health Plan Choices. Journal of Health Economics. 2002;21(1):43–63. doi: 10.1016/s0167-6296(01)00126-6. [DOI] [PubMed] [Google Scholar]
- Cutler D M. The Incidence of Adverse Medical Outcomes under Prospective Payment. Econometrica. 1995;63(1):29–50. [Google Scholar]
- Dranove D, Shanley M, Simon C. Is Hospital Competition Wasteful? RAND Journal of Economics. 1992;23(2):247–62. [PubMed] [Google Scholar]
- Farley D O, Short P F, Elliott M N, Kanouse D E, Brown J A, Hays R D. Effects of CAHPS Health Plan Performance Information on Plan Choices by New Jersey Medicaid Beneficiaries. Health Services Research. 2002a;37(4):985–1007. doi: 10.1034/j.1600-0560.2002.62.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley D O, Elliott M N, Short P F, Damiano P, Kanouse D E, Hays R D. Effect of CAHPS Performance Information on Health Plan Choices by Iowa Medicaid Beneficiaries. Medical Care Research and Review. 2002b;59(3):319–36. doi: 10.1177/107755870205900305. [DOI] [PubMed] [Google Scholar]
- FedStats. “USA Mapstats”. [December 15, 2005];2005 Available at http://www.fedstats.gov/qf/maps/new_york_map.html.
- Gowrisankaran G, Town R J. Competition, Payers, and Hospital Quality. Health Services Research. 2003;38(6):1403–21. doi: 10.1111/j.1475-6773.2003.00185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joskow P L. The Effects of Competition and Regulation on Hospital Bed Supply and the Reservation Quality of the Hospital. Bell Journal of Economics. 1980;11(2):421–47. [Google Scholar]
- Kaiser Family Foundation. “Medicaid and Managed Care”. [December 13, 2005];2001 Available at http://www.kff.org/medicaid/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=13724.
- Kessler D P, McClellan M B. Is Hospital Competition Socially Wasteful? Quarterly Journal of Economics. 2000;115(2):577–615. [Google Scholar]
- Manheim L M, Bazzoli G J, Sohn M. Local Hospital Competition in Large Metropolitan Areas. Journal of Economics and Management Strategy. 1994;3(1):143–67. [Google Scholar]
- Mukamel D B, Zwanziger J, Tomaszewski K J. HMO Penetration, Competition, and Risk-Adjusted Hospital Mortality. Health Services Research. 2001;36(6):1019–35. [PMC free article] [PubMed] [Google Scholar]
- Murray M P. Avoiding Invalid Instruments and Coping with Weak Instruments. Journal of Economic Perspectives. 2006;20(4):111–32. [Google Scholar]
- New York State Department of Health. “New York State Managed Care Plan Performance Report”. [January 19, 2005];2002 Available at http://www.health.state.ny.us/health_care/managed_care/qarrfull/qarr_2002/qarr2002.pdf.
- New York State Department of Health. “New York State Medicaid Managed Care Enrollment Report”. [December 15, 2005];2005 Available at http://www.health.state.ny.us/health_care/managed_care/medicaid/2005/en5_05.pdf.
- New York State Insurance Department. “Child Health Plus Approved Rate as of April 1, 2005.”. 2006
- Newhouse J P. Geographic Access to Physician Services. Annual Review of Public Health. 1990;11:207–30. doi: 10.1146/annurev.pu.11.050190.001231. [DOI] [PubMed] [Google Scholar]
- Newhouse J P, Williams A P, Bennett B W, Schwartz W B. Does the Geographical-Distribution of Physicians Reflect Market Failure? Bell Journal of Economics. 1982;13(2):493–505. [Google Scholar]
- Noether M. Competition among Hospitals. Journal of Health Economics. 1988;7(3):259–84. doi: 10.1016/0167-6296(88)90028-8. [DOI] [PubMed] [Google Scholar]
- Pauly M V. Competition in Medical Services and the Quality of Care. Concepts and History. International Journal of Health Care Finance and Economics. 2004;4(2):113–30. doi: 10.1023/B:IHFE.0000032419.89581.04. [DOI] [PubMed] [Google Scholar]
- Robinson J C, Luft H S. The Impact of Hospital Market Structure on Patient Volume, Average Length of Stay, and the Cost of Care. Journal of Health Economics. 1985;4(4):333–56. doi: 10.1016/0167-6296(85)90012-8. [DOI] [PubMed] [Google Scholar]
- Robinson J C, Luft H S. Competition and the Cost of Hospital Care, 1972 to 1982. Journal of American Medical Association. 1987;257(23):3241–5. [PubMed] [Google Scholar]
- Scanlon D P, Chernew M, McLaughlin C, Solon G. The Impact of Health Plan Report Cards on Managed Care Enrollment. Journal of Health Economics. 2002;21:19–41. doi: 10.1016/s0167-6296(01)00111-4. [DOI] [PubMed] [Google Scholar]
- Scanlon D P, Swaminathan S, Chernew M, Bost J E, Shevock J. Competition and Health Plan Performance. Evidence from Health Maintenance Organization Insurance Markets. Medical Care. 2005;43(4):338–46. doi: 10.1097/01.mlr.0000156863.61808.cb. [DOI] [PubMed] [Google Scholar]
- Scanlon D P, Swaminathan S, Chernew M, Lee W. Market and Plan Characteristics Related to HMO Quality and Improvement. Medical Care Research and Review. 2006;63(6, suppl):56S–89S. doi: 10.1177/1077558706293835. [DOI] [PubMed] [Google Scholar]
- Shortell S M, Hughes E F. The Effects of Regulation, Competition, and Ownership on Mortality Rates among Hospital Inpatients. New England Journal of Medicine. 1988;318:1100–7. doi: 10.1056/NEJM198804283181705. [DOI] [PubMed] [Google Scholar]
- Sommers A R, Wholey D R. The Effect of HMO Competition on Gatekeeping, Usual Source of Care, and Evaluations of Physician Thoroughness. American Journal of Managed Care. 2003;9(9):618–27. [PubMed] [Google Scholar]
- Thorpe K E, Phelps C E. Regulatory Intensity and Hospital Cost Growth. Journal of Health Economics. 1990;9(2):143–66. doi: 10.1016/0167-6296(90)90015-u. [DOI] [PubMed] [Google Scholar]
- Wedig G J, Tai-Seale M. The Effect of Report Cards on Consumer Choice in the Health Insurance Market. Journal of Health Economics. 2002;21(6):1031–48. doi: 10.1016/s0167-6296(02)00075-9. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Melnick G A. The Effects of Hospital Competition and the Medicare PPS Program on Hospital Cost Behavior in California. Journal of Health Economics. 1988;7(4):301–20. doi: 10.1016/0167-6296(88)90018-5. [DOI] [PubMed] [Google Scholar]