Abstract
Clinical decision support systems (CDSS) integrated within Electronic Medical Records (EMR) hold the promise of improving healthcare quality. To date the effectiveness of CDSS has been less than expected, especially concerning the ambulatory management of chronic diseases. This is due, in part, to the fact that clinicians do not use CDSS fully. Barriers to clinicians' use of CDSS have included lack of integration into workflow, software usability issues, and relevance of the content to the patient at hand. At Partners HealthCare, we are developing “Smart Forms” to facilitate documentation-based clinical decision support. Rather than being interruptive in nature, the Smart Form enables writing a multi-problem visit note while capturing coded information and providing sophisticated decision support in the form of tailored recommendations for care. The current version of the Smart Form is designed around two chronic diseases: coronary artery disease and diabetes mellitus. The Smart Form has potential to improve the care of patients with both acute and chronic conditions.
Introduction
In 2003–2004, electronic medical records (EMRs) were used in 18% of ambulatory care visits in the United States, 1 and use is increasing each year. Benefits of EMRs include easy retrieval of medical information, organization and improved readability of that information, and electronic prescribing to reduce medication errors. 2 Another theoretical benefit of EMRs is their ability to facilitate clinical decision support, defined as software designed to directly aid clinical decision making about individual patients. 3 Ideally, capture of coded clinical information can be linked to knowledge of evidence-based medicine to provide tailored recommendations at the point of care. Such integrated clinical decision support should then be able to help close the large and well-documented gap between best evidence and actual practice. 4,5
The Benefits and Limits of Current Clinical Decision Support Systems
Many studies have shown beneficial effects of clinical decision support systems (CDSS) on clinical decision-making. 6–15 A recent review found that CDSS improved practitioner performance in 40% of diagnostic systems, 76% of reminder systems, 62% of disease management systems, and 66% of prescribing systems. 9 However, improvement in patient outcomes has been less than anticipated, especially in the area of chronic diseases. For example, in the review by Garg et al., none of the three studies of diabetes management and only one of 12 studies of cardiovascular disease management showed improvement in patient outcomes. 16 Rates of recommended screening tests may increase, 17–20 but clinical inertia (i.e. recognition of a problem but failure to act) may remain. 21 Nationally, use of electronic health records has not been associated with improved ambulatory care quality. 1 One recent example of an unsuccessful CDSS to improve the care of patients with asthma or angina found three main problem areas: timing of the guideline trigger, ease of use of the system, and helpfulness of the proffered content. 22 Most likely, these same concerns would apply to decision support regarding the management of acute medical conditions. 23
These problems likely stem from five principal shortcomings of CDSS. First, decision support systems are often stand-alone applications poorly integrated into the clinician's workflow. Second, reminders generated by many decision support systems are often interruptive in nature (e.g., pop-ups and alerts). Third, decision support interventions may not be tightly coupled to actions (e.g., the ability to immediately order the medication triggered by the reminder), again decreasing workflow integration. Fourth, the end user may not believe the decision support is relevant to their decision making at hand. Lastly, although EMRs have improved in their ability to capture coded clinical information, 24,25 there may not always be sufficient coded data to drive decision support. 26,27
Physicians are increasingly willing to consider information technology (IT) to support clinical practice but require that it fit into their workflow, be at least time and revenue neutral, be applicable to their patients, and provide intrinsic clinical value. 28–31 The challenge, then, is to build a decision support system with sophisticated content that blends seamlessly into a clinician's workflow and is easy to use. Such a system may not only improve patient care in those practices that use the system, but also drive the increased adoption of EMRs as their inherent value to clinicians is demonstrated.
Linking Decision Support to Clinical Documentation
EMRs and decision support systems could provide self-evident value to clinicians by simplifying documentation, a principle goal of most medical records. Capabilities to create notes are a mainstay of modern EMRs, and some systems are sophisticated in their ability to facilitate coded data entry, auto-import patient data, and create notes in the inpatient and outpatient settings. 24,32–34 However, documentation is not often integrated with decision support. For example, CDSS rules may not always take advantage of detailed, coded, clinical data, and a recommended action from CDSS that is carried out may still have to be documented separately in a visit note. Documentation-based decision-support tools provide a unique opportunity to improve on the current paradigm of decision support. If designed correctly, such systems could seamlessly integrate into the current workflow of busy clinicians by suggesting actions at a time when a clinician is still in the process of clinical documentation. The Smart Form is designed to fit into a clinician's workflow before, after, and especially during the clinical visit where CDSS should have the biggest impact on provider behavior.
As the designers and developers of the documentation-based clinical decision support system, known as the Smart Form, we describe in this article the theoretical framework for the Smart Form's design, usability testing and iterative refinement of the tool, functional characteristics of the product in contrast to other CDSS, and future directions. The architecture and design of the Smart Form is described in an online appendix (available at www.jamia.org).
Smart Form Overview
The Smart Form is an EMR-based, clinical workflow tool designed for organized data review for specific conditions, effective and efficient facilitated data capture, documentation of a clinical visit, and integrated, dynamic, actionable decision support in a single environment. All the tasks typically performed before, during, and after a patient visit are included on one screen to improve efficiency and the user's ability to synthesize data and make clinical decisions.
To address the barriers to the effective use of CDSS, the goals of the Smart Form were several:
1 Create a documentation tool with a judicious mix of free form, structured, and coded data entry modalities to facilitate data entry with minimum burden.
2 Provide decision support that is sophisticated, dynamic, context-driven, actionable, and integrated into the process of documenting a visit note.
3 Enhance workflow by facilitating common actions and reducing the redundancy of data entry.
4 Create one Smart Form per patient, providing decision and workflow support for any number of acute and chronic conditions that the patient may have.
The purpose of the Smart Form was to increase the documentation of coded information necessary for CDSS, increase the proportion of deficiencies in disease management that are addressed at a primary care visit in which the Smart Form is used, and increase compliance with known evidence-based care management goals. Ideally, the Smart Form would replace the users' usual note-writing tools, including the standard free text or template-based note-writing function within the EMR for all patients with the conditions supported by it.
We built the Smart Form around one acute condition—acute respiratory infections (ARIs), and two chronic conditions—coronary artery disease (CAD) and diabetes mellitus (DM). In the process of development, the ARI Smart Form was developed first, and we have previously reported our experience with usability and pilot testing for the ARI Smart Form. 35,36 The CAD/DM Smart Form was developed taking into account lessons learned from developing and testing the ARI Smart Form and implemented taking advantage of new informatics infrastructure at Partners HealthCare. Below, we discuss the conceptual design for the CAD/DM Smart Form as it is in use today.
Requirements Assessment and Design Process
The design of the Smart Form took place in several stages. First, we conducted focus groups involving approximately 25 PCPs in groups of 6–8 to better understand how clinicians currently use the EMR, the variety of workflows employed, methods for acute and chronic disease management, clinicians' attitudes towards decision support, and clinicians' wants and needs regarding Smart Form design. 37 An MD content expert and PhD focus group expert together conducted these sessions, reviewed recordings of the proceedings, and summarized themes.
Based on the findings from focus groups, we developed paper-based and eventually computer-based prototypes of the Smart Form. The prototypes were targeted primarily to project team members (including PCPs, clinical content experts, software usability experts, computer analysts, and clinician investigators) as tools to vet various design decisions and formed the basis for an iterative process of refining and testing ideas. 38 The prototypes were also used as proof-of-concept demonstrations to project stakeholders, health system leaders, and potential users, which allowed us to cultivate clinical champions in various clinics throughout our integrated delivery network.
Once the prototype was fully integrated into the Partners EMR and sufficiently mature, we conducted a pilot study with 31 clinicians drawn from throughout the Partners Healthcare System. We obtained feedback on the usability of the Smart Form in the field in several complementary ways: a feedback button on the Smart Form to allow for real-time, context-specific comments; surveys of users before and after the pilot; and interviews conducted by an outside consulting firm. In this way, we discovered and addressed many usability issues, including errors in decision support logic, desired features, appearance of the final visit note, and workflow enhancements. Feedback on usability also helped us customize our training for the widespread implementation required for the subsequent randomized controlled trial.
Detailed Description of Features and Functions
The Smart Form is primarily a documentation tool, and as such, has many features in common with other latest-generation EMRs, including the ability to add, edit, and delete coded and/or structured clinical information, such as medical problems, medications, allergies, vital signs, laboratory values, and health maintenance information, and to easily import that information into a visit note. Like some systems that use disease-specific templates, 39 the Smart Form organizes clinical data in a disease-focused manner to facilitate decision-making, and also highlights and “requests” coded information related to that disease, such as blood pressure, height, weight, and smoking status.
The Smart Form is also a clinical decision support system, and as such generates output that integrates patient demographic and clinical data with rule-based logic based on the latest guidelines for the management of CAD and DM. The output consists of assessments of the current state of clinical care (e.g., LDL cholesterol above goal of 100 mg/dL), requests for missing or out of date information (e.g., weight more than 1 year old), and suggested orders for medication additions or changes, laboratory studies, appointments and referrals, and printing of patient educational materials. If a suggested order is selected by the user, the action is carried out (i.e., it is linked to provider order entry, such as prescription writing) and the EMR is updated (i.e., the medication list reflects the change). In addition, the selected action can be easily added to the note with a few keystrokes or mouseclicks (explained in more detail below).
The Smart Form differs from most CDSS in the following ways:
1 Decision support is not interruptive in nature but rather is in the form of suggested orders and presented at a place and time in a user's work-flow, i.e., while they are gathering information and writing their note, which may make the decision support more acceptable.
2 The documentation function allows the user to document a typical outpatient visit note in a patient with multiple medical problems, some of which may be supported by decision support and some may not be. This obviates the need for a separate CDSS application.
3 The Smart Form is designed to provide decision support for multiple problems simultaneously and to allow for future expansion to additional acute and chronic conditions.
Use of the Smart Form in a Typical Workflow
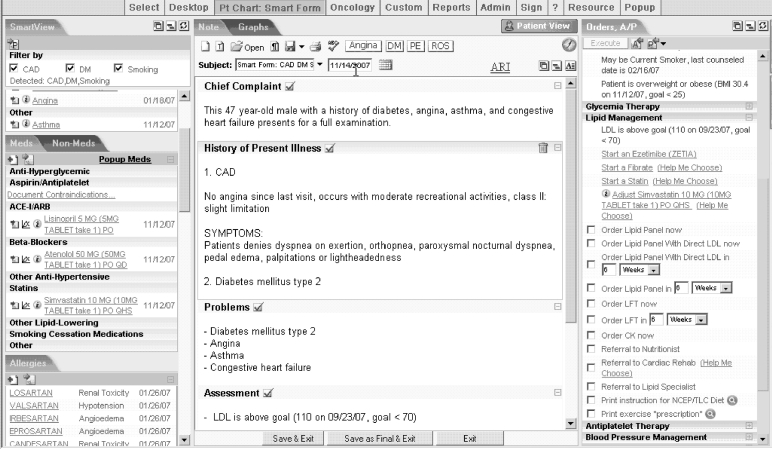
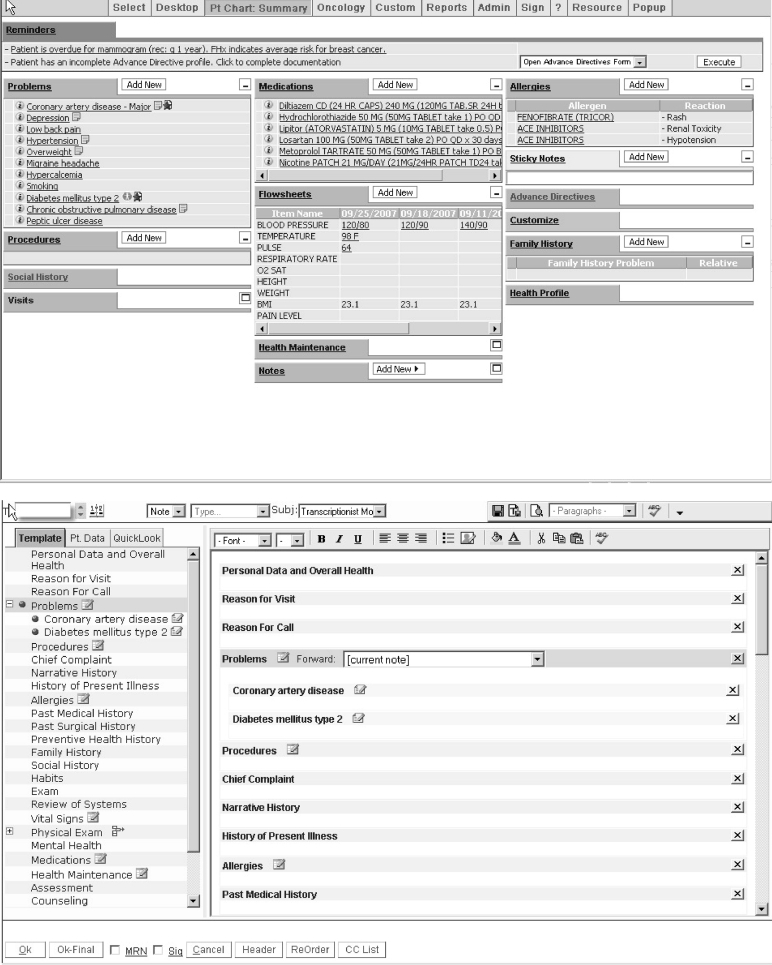
A typical use case will illustrate how the Smart Form works and its potential advantages to the user. ▶ shows the Smart Form. We purposely chose high information density when designing the application in order to minimize “screen flips” and present enough clinical information at once to allow for sophisticated decision-making by the user. The disadvantages of this approach are a “busy”-looking screen and the occasional need for scrolling (for example, if the patient has a lengthy medical problem list). ▶a shows the conventional summary page in the Partners EMR (known as the Longitudinal Medical Record, or LMR), including non-actionable decision support reminders, and ▶b a conventional note-writing screen in the LMR.
Figure 1.
Smart Form application, displaying information in 3 vertical panels: Smart View (patient summary), Visit Note Editor, and Orders Assessment/Plan.
Figure 2.
a. Longitudinal Medical Record (LMR) conventional summary screen. b. LMR conventional note writing screen, demonstrating a structured template.
Before the Visit
The Smart Form is invoked by clicking on the Smart Form icon present next to any qualifying medical problem on the Problem List, from the main patient chart menu, or from the notes page. Prior to a visit, a user might review recent labs, studies, and previous notes by the user or other providers. This can easily be done via the Smart View, the left-most column in the Smart Form, which contains most patient data, problems, allergies, medications, vital signs, laboratory test results, and notes. Laboratory data, vital signs, and medications are presented in tabular format by default but can also be viewed graphically. For example, the user could display a graph of the patient's LDL values against the timing and doses of all lipid-lowering medications prescribed.
A new note can also be started in advance by clicking on the “new note” icons above the central note-writing section. Users can choose from any of the following: 1) a blank note, 2) pulling forward a previous note for updating, 3) starting with an “unstructured” note template (i.e., one block of text with auto-imported text specified by the user), or 4) starting with a structured note template (i.e., separate blocks of text for different data elements such as Medications and History of Present Illness). In this example, the user starts with a structured note, which automatically imports the current problem, medication, and allergy lists and health maintenance information (▶). He then “pulls forward” the “History of Present Illness” and “Assessment and Plan” sections from his last note and saves the preliminary note for later.
During the Visit
When the visit begins, the user reloads the saved Smart Form and begins by verifying the accuracy of the medication list from the Smart View. A medication on the list can be edited or deleted by clicking on its name, which pops up that medication's “prescription pad.” A new medication can be added by clicking on the “plus” icon under Medications. Similarly, the user adds an additional blood pressure reading to the Vital Signs section and updates the smoking status under Health Maintenance.
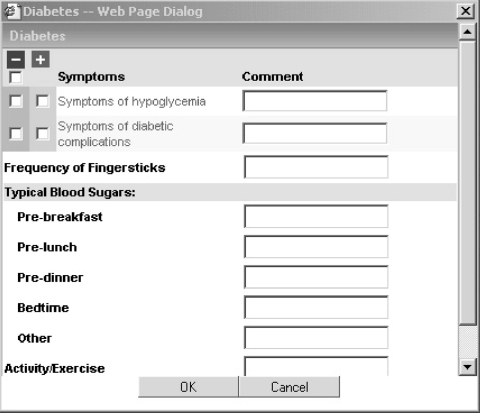
The user then starts interviewing the patient while typing into the History of Present Illness section of the structured template in the note writing section. Because the patient has diabetes, the user clicks on the Diabetes button in the note writing section. This invokes a “mini-template” for diabetes (▶), a pop-up window that allows users to record a specific set of observations by clicking checkboxes or radio buttons or choosing predefined statements from drop-down menus. In this case, the mini-template allows documentation of diabetes complications, symptoms of hypoglycemia, typical blood sugars at different times of the day, and compliance with diet and exercise recommendations. Once completed, a textual representation of the results is automatically inserted into the note. Other mini-templates are available for CAD, physical examination (PE), and review of systems (ROS). The CAD and diabetes mini-templates are only available if a qualifying problem is on the problem list. Where possible, a user may indicate a number of observations as normal with one click, and then select the ones that were found to be abnormal and which ones were not assessed. Free text comments can also be added to any data element.
Figure 3.
Mini-template for diabetes mellitus.
For the physical examination, the user has several options: using the PE mini-template (which because the patient has diabetes automatically includes a foot exam section), pulling forward the PE section from a previously written structured note, or importing a “canned paragraph” from a drop-down list of customized paragraphs or by typing a period followed by the first few letters of the name of the paragraph (i.e., using “dot-macro” technology).
The user might then use the Smart Form as he would any other EMR documentation tool: documenting information about the patient's other medical problems, renewing medication prescriptions, ordering laboratory tests unrelated to CAD and diabetes, etc.
Throughout the documentation exercise, clinical decision support related to diabetes and CAD is apparent to the user. The Smart View by default is organized around either or both problems, depending on which are present on the problem list (in this case, the patient has both). For example, medications are sorted by antiplatelets, beta-blockers, angiotensin converting enzyme inhibitors (ACE I)/angiotensin receptor blockers (ARB), other antihypertensive medications, HMG CoA reductase inhibitors (statins), other lipid agents, hypoglycemic agents, and other medications. Some of these classes are reserved for CAD patients (e.g., antiplatelets), others for diabetics (e.g., hypoglycemic agents), and others for both (ACE I/ARB). Decision support rules specify which classes will be shown and could theoretically accommodate any number of problems alone or in combination. Filtering by CAD and/or Diabetes can be turned on and off by the user by checking and unchecking boxes at the top of the Smart View.
If a patient is not on one of the recommended classes of medications, the Smart Form presents a link to document contraindications. This allows for coded entry of preexisting conditions (filed in the LMR as problems) or reactions (filed as allergies), which would shut off decision support to order these medications. In this case, the user files a preexisting condition of peptic ulcer disease to explain why the patient is not on an antiplatelet medication.
Because the user has made several changes to the patient's clinical information (e.g., updated the medication list and smoking status, added a new blood pressure reading, documented a contraindication to antiplatelet medications), the user now dynamically regenerates the CDSS logic by clicking on a “regenerate” icon (the approximately 600 rules, codified using ILOG rules engine software (Sunnyvale, CA) and incorporating patient data from the EMR and other enterprise data repositories, are updated in about 1 second). The user now views the Orders/Assessment and Plan section in the right column of the Smart Form. This section begins with an assessment of how the patient is doing in each domain of CAD and/or diabetes management: glycemia control, lipid management, and blood pressure management; antiplatelet, beta-blocker, and ACE I/ARB medication use; weight/body mass index and smoking status; urine protein, eye exam, and foot exam status; immunizations, and follow-up appointments.
As with the Smart View, some domains are specific to CAD (e.g., antiplatelet use), some are specific to diabetes (e.g., annual screening for proteinuria), and some are included in both conditions (e.g., lipid management). The treatment goals are calculated based on the number and types of medical conditions the patient has. For example, a patient with CAD but without diabetes and with cardiac risk factors under good control has an LDL goal of 100 mg/dL, while a patient with both CAD and diabetes has an LDL goal of 70 mg/dL. 40 In this way, the Smart Form logic accommodates patients with one or both conditions, with or without other comborbidities, and can be expanded over time to support other medical conditions.
In this case, the patient's LDL goal is 70 mg/dL and the patient's LDL is above that goal (last LDL within the past 12 months is 110 mg/dL). Because the patient is not in compliance with the guideline, the assessment is in red text. The text of the assessment serves as link to the suggested actions below. Because the patient is already on a statin, the user sees the option to increase its dose: clicking on the option opens the prescription pad for the statin where its dose can be increased. The user can also click on a “help me choose” option, which takes the user to “passive decision support,” in this case a table that displays the dose and type of each statin predicted to achieve the desired LDL reduction. We chose such “passive” decision support rather than making a recommendation for a specific dose and type of statin for two reasons: 1) an acknowledgement that there are limits to how much CDSS can “know” about a patient compared with the patient's PCP, and 2) a desire not to alienate users by making recommendations that limit therapeutic choices unnecessarily. In this case, the user increases the dose of the statin on the prescription pad; the medication list in the EMR is automatically updated.
In addition to increasing the dose of statin, other possible actions are displayed, including starting a fibrate medication, ordering a lipid panel now or in the future (the number of weeks is specified by the user), printing patient instructions for a low cholesterol diet, and making a referral to a lipid specialist. When the option to order a fibrate is selected, the user sees a list of possible medications in that class, sorted by their out-of-pocket expense based on the patient's insurance coverage. Selecting a particular medication then opens up a prescription pad for that medication. Ordering labs and referrals and printing patient instructions only require checking a box next to each action.
In a similar manner, the user then orders other medication changes, laboratory tests, patient educational materials, and referrals related to the other domains of care. Finally, the user schedules a follow-up appointment with himself and with his nurse, selecting the time frame for each appointment.
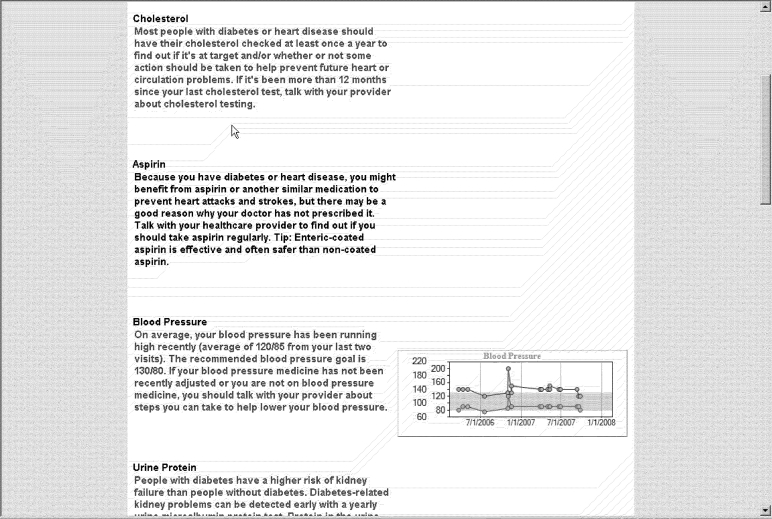
Once all desired actions have been selected, the user hits the “Execute” button. This sends all laboratory orders, referrals, and patient instructions to the printer. It also “tees up” all orders for easy entry into the visit note (see below). Before the patient leaves, the user prints the “Patient View,” (see ▶) a patient-friendly version of the assessment and a listing of those actions chosen by the Smart Form user. A time plot of values is presented for glycemic control (HbA1c), blood pressure, lipid management (LDL), and weight (body mass index). Also included in this view is a listing of patient's allergies and their medication list with all Latin abbreviations translated into English. The user reviews the findings with the patient and hands it to him.
Figure 4.
Patient View, displaying an individual's disease management status using patient-friendly language.
Finally, the user signs the note, which prints the new prescriptions or refills for the patient. The patient receives the prescriptions and educational material, while the office staff receives the laboratory and referral orders. As the patient leaves the office, the user quickly documents abnormal physical examination findings by clicking on the PE mini-template. The user saves a preliminary version of the note by hitting the save icon.
After the Visit
The job of completing the visit note often occurs after the patient has left, for example at the end of the day. In this case, the user re-loads his preliminary note, puts his cursor in the Assessment and Plan section, and types a macro, “.plan.” This imports documentation of all executed actions from the Smart Form into the note. He also imports orders placed through the LMR outpatient order entry system (known as End of Visit) outside of the Smart Form context by clicking on the import icon next to the End of Visit heading. He then places his cursor in the Chief Complaint section and types “.intro.” This imports a previously created “canned paragraph” that automatically incorporates the patient's current age and sex as well as the problem list in sentence format (e.g., “This 47 year-old male with a history of diabetes, angina, asthma, and congestive heart failure presents for a full examination.”) He also imports the last set of laboratory test results by placing the cursor in the Test Results section of his note and clicking on the import icon next to the date of the lab work. He makes final edits of the rest of the note, saves it as final, and signs the note.
Discussion
The Smart Form is designed to integrate decision support into the normal tasks of seeing a patient and documenting a note. As such, we needed to completely redesign the current documentation experience. We learned several lessons during the design process. First, to provide clinicians with an incentive to use the Smart Form, it must be at least as good or better than current documentation tools while providing additional value: either time-saving features or tools that improve patient care while remaining time neutral. We attempted to do both. Second, improved usability was the result of many small changes made through iterative testing and refinement. We acknowledge that the Smart Form, due to its sophistication and power, is complicated to use at first and requires training and practice. However, because its value is soon self-evident, many users have found the up-front time invested to be worth the effort.
Comparison with Other Clinical Decision Support Systems
▶ provides a list of several features of the Smart Form and how it compares to other CDS systems. The vast majority of CDSS in the ambulatory care setting provide alerts, reminders, and/or suggested actions either on paper, in a stand-alone computer application, or within an EMR, often on a “summary page.” 7,17,18,41–48 In most systems, the output is not linked to electronic order entry or to electronic documentation. A few systems are documentation-based and help create visit notes but do not link directly to CPOE, 49,50 and a few others provide links to CPOE but not to electronic documentation. 51,52 The same is true of most inpatient and emergency department systems, although many of the inpatient systems link to order entry but not to electronic documentation. 53–56 The EDECS system at UCLA 57–59 is a documentation-based system that requires entry of coded data, creates documentation at the end of the encounter, and presents recommended actions that integrate with order entry. However, this system addresses one problem at a time in a setting (emergency department) where such a focus is appropriate. Our goal was to provide decision support as suggested actions in the note-writing section of an EMR and integrate that function with full-featured documentation support of an outpatient with multiple medical problems.
Table 1.
Table 1 Comparison of Smart Form Features with Other CDSS
| Feature | Examples of Systems ∗ |
|---|---|
| Provides decision support in the form of alerts, reminders and/or suggested actions based on patient data and clinical rule-based logic | Goldstein 2000, 41 Lobach 1997, 17 Ornstein 1995, 42 Mazzuca 1990, 43 Garr 1993, 44 Hetlevik 1999, 45 Filippi 2003, 46 Meigs 2003, 18 Ansari 2003, 47 Demakis 2000, 7 Rollman 2002, 48 Cannon 2000, 49 Murray 2004, 51 Tierney 2003, 52 Gorman 2000, 62 Safran 1995, 50 Larsen 1989, 63 Overhage 1997, 56 Kucher 2005, 55 Evans 1998, 53 Mullett 2001, 54 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Provides decision support on screen (as opposed to paper alone) | Goldstein 2000, 41 Ornstein 1995, 42 Filippi 2003, 46 Meigs 2003, 18 Ansari 2003, 47 Demakis 2000, 7 Rollman 2002, 48 Cannon 2000, 49 Murray 2004, 51 Tierney 2003, 52 Gorman 2000, 62 Safran 1995, 50 Overhage 1997, 56 Kucher 2005, 55 Evans 1998, 53 Mullett 2001, 54 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Provides decision support within the EMR (as opposed to a stand-alone system) | Ornstein 1995, 42 Filippi 2003, 46 Ansari 2003, 47 Safran 1995, 50 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Allows user to turn off specific recommendations | Goldstein 2000, 41 Lobach 1997, 17 Filippi 2003, 46 Cannon 2000, 49 Smart Form |
| Links suggested actions to CPOE | Murray 2004, 51 Tierney 2003, 52 Overhage 1997, 56 Kucher 2005, 55 Evans 1998, 53 Mullett 2001, 54 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Updates EMR coded data with actions taken | Smart Form |
| Facilitates entry of actions taken into electronic note documentation | Safran 1995, 50 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Facilitates entry of coded patient data into electronic note documentation | Cannon 2000, 49 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Requests entry of coded data that are missing | Meigs 2003, 18 Cannon 2000, 49 Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Presents decision support in the context of a note-writing screen (as opposed to an order entry or summary screen) | Schriger 1997, 57 Schriger 2000, 58 Mikulich 2001, 59 Smart Form |
| Provides decision support for more than one problem at a time | Ornstein 1995, 42 Garr 1993, 44 Smart Form |
| Provides patient view of adherence with treatment goals | Smart Form |
| Provides graphical views of patient data | Meigs 2003, 18 Smart Form |
| Provides problem-oriented data review | Lobach 1997, 17 Meigs 2003, 18 Smart Form |
| Provides clinical workflow support (patient care handouts, referrals) | Ornstein 1995, 42 Mazzuca 1990, 43 Meigs 2003, 18 Murray 2004, 51 Gorman 2000, 62 Safran 1995, 50 Smart Form |
∗ Absence of a reference from a specific feature does not necessary imply that the referenced CDSS is missing that feature, only that the feature's presence could not be confirmed by a review of the manuscript.
EMR = Electronic medical record; CPOE = computerized provider order entry.
Evaluation
We are currently conducting a randomized controlled trial to determine the effect of the CAD/DM Smart Form on care processes, patient outcomes, and user satisfaction. Within 10 primary care practices at Partners, physicians have been randomized to receive the Smart Form or usual care (i.e., the native EMR alone); subjects are all patients of these clinicians with CAD or DM. Outcomes will reflect each of the treatment domains, e.g., for lipid management, whether more patients have an LDL cholesterol level < 100 mg/dL at the end of the study period in the intervention group compared with the control group, adjusted for baseline performance, potential confounders, and clustering by physician.
Limitations
While the CAD DM Smart Form has many of the features originally designed for it, and has been greatly improved through the process of iterative testing and refinement, there are still limitations to the application, including the following:
1 Lack of full integration of both acute and chronic problems. As mentioned above, the goal is a “multi-problem Smart Form” tailored for each patient's unique combination of acute and chronic problems. One way to design this would be to allow for coded problem-based data entry into the History of Present Illness section that could trigger mini-templates for acute problems such as ARI.
2 Additional documentation features: there are currently a few areas where documentation within Smart Forms does not work as well as existing EMR documentation tools, e.g., problem-based editing within structured templates. Inclusion of these features will require additional development.
3 Lack of integration of reminders related to prevention: currently, reminders regarding prevention are presented on the patient summary page within the EMR. Ideally, these would be integrated into the Orders, Assessment and Plan section and would be actionable just like decision support for acute and chronic conditions.
Future Developments
In future versions of the Smart Form we hope to include the following:
1 Additional decision support for other acute and chronic conditions and health maintenance items. Likely near-term candidate conditions include urinary tract infections, low back pain, breast masses, congestive heart failure, and chronic obstructive pulmonary disease.
2 As the number of acute and chronic problems increases and health maintenance decision support is incorporated into the Smart Form, there will be a growing need to prioritize and limit the number of suggested actions in the Orders, Assessment, and Plan section in order not to overwhelm the user. The issue of knowledge creation, maintenance, and expansion is beyond the scope of this article and will be discussed in a separate manuscript.
3 Customization by the user of formatting (e.g., how to import lab values, appearance of each mini-template, etc.) and graphing functions (e.g., automatic stacking of blood pressure values with all anti-hypertensive medications).
4 Increased decision support for data obtained outside the Partners Healthcare System (e.g., outside laboratory test values).
5 Ability to turn decision support off for individual items and to explain why, other than for standard contraindications (e.g., patient refusal).
6 An option for problem-focused documentation (e.g., HPI, assessment, and plan grouped together for each problem).
7 Better integration of Smart Forms with billing functions (e.g., provide the diagnosis code for problems entered into the HPI section; provide an Evaluation & Management coding tool based on the content of a structured note).
8 Integration of the Smart Form with quality reporting tools,60 so that coded information from the Smart Form (e.g., vital signs, diabetic retinopathy screening, medication contraindications) can lead to better reporting of data and support pay-for-performance initiatives.
9 Integration with the Partners shared online patient portal,61 so patients can enter data in a template (e.g, family history, review of systems, medication usage, and condition-specific questionnaires) from home, workplace, or in the waiting room that could then be confirmed and quickly imported into the note by the treating clinician.
10 The medicolegal implications of the Smart Form, as with all CDSS, needs to be further explored (e.g., increased liability if decision support recommendations are not followed).
Conclusions
The Smart Form represents documentation-based clinical decision support that goes beyond standard interruptive methods by dynamically rendering an integrated data review, clinical documentation, and decision support environment for the end-user. Critical to the success of this application's development (and critical lessons for EMR developers and vendors) were strong participatory design principles, iterative development, and an understanding of clinician workflow and psychology. By integrating decision support into a clinician's workflow, the Smart Form has the potential to facilitate documentation of coded, actionable data, improve the quality of decision-making, and improve the management of patients with acute and chronic medical conditions. We hope Smart Forms will help to close the gap between best evidence and current medical practice.
Acknowledgments
The authors thank Lana Tsurikova, Andrea Melnikas, Svetlana Turovsky, Kerry McColgan, and Lynn Volk for their assistance with research project management, Frank Chang, Maya Olsha-Yehiav, Boris Rudelson, Sasha Fedtsov, and Nina Plaks for software development, David Taylor, Janak Joshi, and Lynn Klokman for analytical work, Alan Rose for usability testing, Judith Colecchi, Saverio Maviglia, Debora Goldman, and Tonya Hongsermeier for decision support knowledge management, and Alan Cole for content expertise in diabetes mellitus.
Footnotes
This study was supported by a grant from the Agency for Healthcare Research and Quality (1 R01 HS015169-01). Dr. Schnipper is supported by a mentored career development award from the National Heart Lung and Blood Institute (1 K08 HL072806-01). Dr. Linder is supported by a career development award (K08 HS014563) from the Agency for Healthcare Research and Quality.
There are no commercial or financial relationships that could pose a conflict of interest with the material presented in this paper.
References
- 1.Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States Arch Intern Med 2007;167(13):1400-1405Jul 9. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Gawande AA. Improving safety with information technology N Engl J Med 2003;348(25):2526-2534Jun 19. [DOI] [PubMed] [Google Scholar]
- 3.Randolph AG, Haynes RB, Wyatt JC, Cook DJ, Guyatt GH. Users' Guides to the Medical Literature: XVIII. How to use an article evaluating the clinical impact of a computer-based clinical decision support system. JAMA 1999;282(1):67-74Jul 7. [DOI] [PubMed] [Google Scholar]
- 4.Committee on Quality of Health Care in America IoM Crossing the quality chasm: a new health system for the 21st centuryWashinton, DC: National Academy Press; 2001.
- 5.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States N Engl J Med 2003;348(26):2635-2645Jun 26. [DOI] [PubMed] [Google Scholar]
- 6.Bonevski B, Sanson-Fisher RW, Campbell E, Carruthers A, Reid AL, Ireland M. Randomized controlled trial of a computer strategy to increase general practitioner preventive care Prev Med 1999;29(6 Pt 1):478-486Dec. [DOI] [PubMed] [Google Scholar]
- 7.Demakis JG, Beauchamp C, Cull WL, Denwood R, Eisen SA, Lofgren R, et al. Improving residents' compliance with standards of ambulatory care: results from the VA Cooperative Study on Computerized Reminders JAMA 2000;284(11):1411-1416Sep 20. [DOI] [PubMed] [Google Scholar]
- 8.Dexter PR, Wolinsky FD, Gramelspacher GP, Zhou XH, Eckert GJ, Waisburd M, et al. Effectiveness of computer-generated reminders for increasing discussions about advance directives and completion of advance directive forms. A randomized, controlled trial. Ann Intern Med 1998;128(2):102-110Jan 15. [DOI] [PubMed] [Google Scholar]
- 9.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review JAMA 2005;293(10):1223-1238Mar 9. [DOI] [PubMed] [Google Scholar]
- 10.Kuperman GJ, Teich JM, Tanasijevic MJ, Ma'Luf N, Rittenberg E, Jha A, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial J Am Med Inform Assoc 1999;6(6):512-522Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poller L, Shiach CR, MacCallum PK, Johansen AM, Munster AM, Magalhaes A, et al. Multicentre randomised study of computerised anticoagulant dosage. European Concerted Action on Anticoagulation. Lancet 1998;352(9139):1505-1509Nov 7. [DOI] [PubMed] [Google Scholar]
- 12.Pozen MW, D'Agostino RB, Selker HP, Sytkowski PA, Hood Jr WB. A predictive instrument to improve coronary-care-unit admission practices in acute ischemic heart disease. A prospective multicenter clinical trial. N Engl J Med 1984;310(20):1273-1278May 17. [DOI] [PubMed] [Google Scholar]
- 13.Rodman JH, Jelliffe RW, Kolb E, Tuey DB, de Guzman MF, Wagers PW, et al. Clinical studies with computer-assisted initial lidocaine therapy Arch Intern Med 1984;144(4):703-709Apr. [PubMed] [Google Scholar]
- 14.Selker HP, Beshansky JR, Griffith JL, Aufderheide TP, Ballin DS, Bernard SA, et al. Use of the acute cardiac ischemia time-insensitive predictive instrument (ACI-TIPI) to assist with triage of patients with chest pain or other symptoms suggestive of acute cardiac ischemia. A multicenter, controlled clinical trial. Ann Intern Med 1998;129(11):845-855Dec 1. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care Ann Intern Med 2006;144(10):742-752May 16. [DOI] [PubMed] [Google Scholar]
- 16.Barnett GO, Winickoff RN, Morgan MM, Zielstorff RD. A computer-based monitoring system for follow-up of elevated blood pressure Med Care 1983;21(4):400-409Apr. [DOI] [PubMed] [Google Scholar]
- 17.Lobach DF, Hammond WE. Computerized decision support based on a clinical practice guideline improves compliance with care standards Am J Med 1997;102(1):89-98Jan. [DOI] [PubMed] [Google Scholar]
- 18.Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, et al. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project Diabetes Care 2003;26(3):750-757Mar. [DOI] [PubMed] [Google Scholar]
- 19.Montori VM, Dinneen SF, Gorman CA, Zimmerman BR, Rizza RA, Bjornsen SS, et al. The impact of planned care and a diabetes electronic management system on community-based diabetes care: the Mayo Health System Diabetes Translation Project Diabetes Care 2002;25(11):1952-1957. [DOI] [PubMed] [Google Scholar]
- 20.Brownbridge G, Evans A, Fitter M, Platts M. An interactive computerized protocol for the management of hypertension: effects on the general practitioner's clinical behaviour J R Coll Gen Pract 1986;36(286):198-202May. [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia Ann Intern Med 2001;135(9):825-834Nov 6. [DOI] [PubMed] [Google Scholar]
- 22.Rousseau N, McColl E, Newton J, Grimshaw J, Eccles M. Practice based, longitudinal, qualitative interview study of computerised evidence based guidelines in primary care BMJ 2003;326(7384):314Feb 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linder JA. Health information technology as a tool to improve care for acute respiratory infections Am J Manag Care 2004;10(10):661-662Oct. [PubMed] [Google Scholar]
- 24.Rosenbloom ST, Grande J, Geissbuhler A, Miller RA. Experience in implementing inpatient clinical note capture via a provider order entry system J Am Med Inform Assoc 2004;11(4):310-315Jul-Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Welford CR. A comprehensive computerized patient record with automated linkage to QMR Proc Annu Symp Comput Appl Med Care 1994:814-818. [PMC free article] [PubMed]
- 26.Linder JA, Bates DW, Williams DH, Connolly MA, Middleton B. Acute infections in primary care: accuracy of electronic diagnoses and electronic antibiotic prescribing J Am Med Inform Assoc 2006;13(1):61-66Jan-Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onofrei M, Hunt J, Siemienczuk J, Touchette DR, Middleton B. A first step towards translating evidence into practice: heart failure in a community practice-based research network Inform Prim Care 2004;12(3):139-145. [DOI] [PubMed] [Google Scholar]
- 28.Apkon M, Singhaviranon P. Impact of an electronic information system on physician workflow and data collection in the intensive care unit Intensive Care Med 2001;27(1):122-130Jan. [DOI] [PubMed] [Google Scholar]
- 29.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality J Am Med Inform Assoc 2003;10(6):523-530Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teich JM, Spurr CD, Schmiz JL, O'Connell EM, Thomas D. Enhancement of clinician workflow with computer order entry Proc Annu Symp Comput Appl Med Care 1995:459-463. [PMC free article] [PubMed]
- 31.Webster C, Copenhaver J. Structured data entry in a workflow-enabled electronic patient record J Med Pract Manage 2001;17(3):157-161Nov-Dec. [PubMed] [Google Scholar]
- 32.Cimino JJ, Patel VL, Kushniruk AW. Studying the human-computer-terminology interface J Am Med Inform Assoc 2001;8(2):163-173Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hohnloser JH, Puerner F, Soltanian H. Improving coded data entry by an electronic patient record system Methods Inf Med 1996;35(2):108-111Jun. [PubMed] [Google Scholar]
- 34.Rosenbloom ST, Miller RA, Johnson KB, Elkin PL, Brown SH. Interface terminologies: facilitating direct entry of clinical data into electronic health record systems J Am Med Inform Assoc 2006;13(3):277-288May-Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Linder JA, Rose AF, Palchuk MB, Chang F, Schnipper JL, Chan JC, et al. Decision support for acute problems: The role of the standardized patient in usability testingDec J Biomed Inform 2006;39(6):648-655Epub 2006 Jan 6 2006 Jan 6. [DOI] [PubMed] [Google Scholar]
- 36.Linder JA, Schnipper JL, Volk LA, Tsurikova R, Palchuk MB, Olsha-Yehiav M, et al. Clinical decision support to improve antibiotic prescribing for acute respiratory infections: results of a pilot study AMIA Annu Symp Proc 2007:468-472. [PMC free article] [PubMed]
- 37.Rose AF, Schnipper JL, Park ER, Poon EG, Li Q, Middleton B. Using qualitative studies to improve the usability of an EMR J Biomed Inform 2005;38(1):51-60Feb. [DOI] [PubMed] [Google Scholar]
- 38.Virzi RA, Sokolov JL, Karis D. Usability problem identifaction using both low- and high-fidelity prototypesConference proceedings on human factors in computing systems; 1996; Vancouver, BC, Canada 1996.
- 39.Henry SB, Douglas K, Galzagorry G, Lahey A, Holzemer WL. A template-based approach to support utilization of clinical practice guidelines within an electronic health record J Am Med Inform Assoc 1998;5(3):237-244May-Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grundy SM, Cleeman JI, Merz CN, Brewer Jr. HB, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines Circulation 2004;110(2):227-239Jul 13. [DOI] [PubMed] [Google Scholar]
- 41.Goldstein MK, Hoffman BB, Coleman RW, Musen MA, Tu SW, Advani A, et al. Implementing clinical practice guidelines while taking account of changing evidence: ATHENA DSS, an easily modifiable decision-support system for managing hypertension in primary care Proc AMIA Symp 2000:300-304. [PMC free article] [PubMed]
- 42.Ornstein SM, Garr DR, Jenkins RG, Musham C, Hamadeh G, Lancaster C. Implementation and evaluation of a computer-based preventive services system Fam Med 1995;27(4):260-266Apr. [PubMed] [Google Scholar]
- 43.Mazzuca SA, Vinicor F, Einterz RM, Tierney WM, Norton JA, Kalasinski LA. Effects of the clinical environment on physicians' response to postgraduate medical education Am Ed Res J 1990;27(3):473-488. [Google Scholar]
- 44.Garr DR, Ornstein SM, Jenkins RG, Zemp LD. The effect of routine use of computer-generated preventive reminders in a clinical practice Am J Prev Med 1993;9(1):55-61Jan-Feb. [PubMed] [Google Scholar]
- 45.Hetlevik I, Holmen J, Kruger O. Implementing clinical guidelines in the treatment of hypertension in general practice. Evaluation of patient outcome related to implementation of a computer-based clinical decision support system. Scand J Prim Health Care 1999;17(1):35-40Mar. [DOI] [PubMed] [Google Scholar]
- 46.Filippi A, Sabatini A, Badioli L, Samani F, Mazzaglia G, Catapano A, et al. Effects of an automated electronic reminder in changing the antiplatelet drug-prescribing behavior among Italian general practitioners in diabetic patients: an intervention trial Diabetes Care 2003;26(5):1497-1500. [DOI] [PubMed] [Google Scholar]
- 47.Ansari M, Shlipak MG, Heidenreich PA, Van Ostaeyen D, Pohl EC, Browner WS, et al. Improving guideline adherence: a randomized trial evaluating strategies to increase beta-blocker use in heart failure Circulation 2003;107(22):2799-2804Jun 10. [DOI] [PubMed] [Google Scholar]
- 48.Rollman BL, Hanusa BH, Lowe HJ, Gilbert T, Kapoor WN, Schulberg HC. A randomized trial using computerized decision support to improve treatment of major depression in primary care J Gen Intern Med 2002;17(7):493-503Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cannon DS, Allen SN. A comparison of the effects of computer and manual reminders on compliance with a mental health clinical practice guideline J Am Med Inform Assoc 2000;7(2):196-203Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Safran C, Rind DM, Davis RB, Ives D, Sands DZ, Currier J, et al. Guidelines for management of HIV infection with computer-based patient's record Lancet 1995;346(8971):341-346Aug 5. [DOI] [PubMed] [Google Scholar]
- 51.Murray MD, Harris LE, Overhage JM, Zhou XH, Eckert GJ, Smith FE, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial Pharmacotherapy 2004;24(3):324-337Mar. [DOI] [PubMed] [Google Scholar]
- 52.Tierney WM, Overhage JM, Murray, MD, Harris LE, Zhou XH, Eckert GJ, et al. Effects of computerized guidelines for managing heart disease in primary care J Gen Intern Med 2003;18(12):967-976Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme Jr. JF, et al. A computer-assisted management program for antibiotics and other antiinfective agents N Engl J Med 1998;338(4):232-238Jan 22. [DOI] [PubMed] [Google Scholar]
- 54.Mullett CJ, Evans RS, Christenson JC, Dean JM. Development and impact of a computerized pediatric antiinfective decision support program Pediatrics 2001;108(4):E75Oct. [DOI] [PubMed] [Google Scholar]
- 55.Kucher N, Koo S, Quiroz R, Cooper JM, Paterno, MD, Soukonnikov B, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients N Engl J Med 2005;352(10):969-977Mar 10. [DOI] [PubMed] [Google Scholar]
- 56.Overhage JM, Tierney WM, Zhou XH, McDonald CJ. A randomized trial of “corollary orders” to prevent errors of omission J Am Med Inform Assoc 1997;4(5):364-375Sep-Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schriger DL, Baraff LJ, Rogers WH, Cretin S. Implementation of clinical guidelines using a computer charting system. Effect on the initial care of health care workers exposed to body fluids. JAMA 1997;278(19):1585-1590Nov 19. [PubMed] [Google Scholar]
- 58.Schriger DL, Baraff LJ, Buller K, Shendrikar MA, Nagda S, Lin EJ, et al. Implementation of clinical guidelines via a computer charting system: effect on the care of febrile children less than three years of age J Am Med Inform Assoc 2000;7(2):186-195Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mikulich VJ, Liu YC, Steinfeldt J, Schriger DL. Implementation of clinical guidelines through an electronic medical record: physician usage, satisfaction and assessment Int J Med Inform 2001;63(3):169-178Oct. [DOI] [PubMed] [Google Scholar]
- 60.Olsha-Yehiav M, Einbinder JS, Jung E, Linder JA, Greim J, Li Q, et al. Quality dashboards: technical and architectural considerations of an actionable reporting tool for population management AMIA Annu Symp Proc 2006:1052. [PMC free article] [PubMed]
- 61.Wald JS, Middleton B, Bloom A, Walmsley D, Gleason M, Nelson E, et al. A patient-controlled journal for an electronic medical record: issues and challenges Medinfo 2004;11(Pt 2):1166-1170. [PubMed] [Google Scholar]
- 62.Gorman CA, Zimmerman BR, Smith SA, Dinneen SF, Knudsen JB, Holm D, et al. DEMS - a second generation diabetes electronic management system Comput Methods Programs Biomed 2000;62(2):127-140. [DOI] [PubMed] [Google Scholar]
- 63.Larsen RA, Evans RS, Burke JP, Pestotnik SL, Gardner RM, Classen DC. Improved perioperative antibiotic use and reduced surgical wound infections through use of computer decision analysis Infect Control Hosp Epidemiol 1989;10(7):316-320Jul. [DOI] [PubMed] [Google Scholar]