Abstract
The authors develop a typology of clinicians' workarounds when using barcoded medication administration (BCMA) systems. Authors then identify the causes and possible consequences of each workaround. The BCMAs usually consist of handheld devices for scanning machine-readable barcodes on patients and medications. They also interface with electronic medication administration records. Ideally, BCMAs help confirm the five “rights” of medication administration: right patient, drug, dose, route, and time. While BCMAs are reported to reduce medication administration errors—the least likely medication error to be intercepted— these claims have not been clearly demonstrated. The authors studied BCMA use at five hospitals by: (1) observing and shadowing nurses using BCMAs at two hospitals, (2) interviewing staff and hospital leaders at five hospitals, (3) participating in BCMA staff meetings, (4) participating in one hospital's failure-mode-and-effects analyses, (5) analyzing BCMA override log data. The authors identified 15 types of workarounds, including, for example, affixing patient identification barcodes to computer carts, scanners, doorjambs, or nurses' belt rings; carrying several patients' prescanned medications on carts. The authors identified 31 types of causes of workarounds, such as unreadable medication barcodes (crinkled, smudged, torn, missing, covered by another label); malfunctioning scanners; unreadable or missing patient identification wristbands (chewed, soaked, missing); nonbarcoded medications; failing batteries; uncertain wireless connectivity; emergencies. The authors found nurses overrode BCMA alerts for 4.2% of patients charted and for 10.3% of medications charted. Possible consequences of the workarounds include wrong administration of medications, wrong doses, wrong times, and wrong formulations. Shortcomings in BCMAs' design, implementation, and workflow integration encourage workarounds. Integrating BCMAs within real-world clinical workflows requires attention to in situ use to ensure safety features' correct use.
Introduction
The authors herein identify and examine clinicians' workarounds when using barcoded medication administration (BCMA) systems. We then develop a typology of workarounds, their causes, and the implications of workarounds to BCMA processes. We also endeavor to document workflows, procedures, and system designs that likely engender workarounds and the medication errors potentially facilitated by them. We delineate the causes of these adaptations, and present staff's explanations for their actions. Finally, building on these findings, we suggest methods to systematically find, examine, and correct BCMA work and design processes that engender workarounds.
Background
The Institute of Medicine (IOM) estimates that, on average, a hospitalized patient is subject to one medication administration error per day, and deems medication administration error a priority for patient safety intervention. 1 In hospitals, the medication administration stage accounts for 26% to 32% of adult patient medication errors 2,3 and 4% to 60% of pediatric patient medication errors. 4 Errors in this latter stage of the medication process are far less likely to be intercepted and far more likely to reach patients than in any previous stage. 2,3,5 It is because medication administration errors are so prevalent, so seldom intercepted, and so final that BCMAs have been strongly recommended for all hospitals. 1,6,7
There is evidence that BCMA systems can reduce pharmacy dispensing errors, 8 and there are reports that BCMA systems can reduce administration errors, 9-11 although the latter claims have not been clearly demonstrated. 1 What has been demonstrated is that some users deviate from written BCMA-use protocols. 12-15 These deviations, called violations or workarounds, are staff actions that do not follow explicit or implicit rules, assumptions, workflow regulations, or intentions of system designers. 16 They are nonstandard procedures typically used because of deficiencies in system or workflow design. 17 Although several BCMA workarounds have been documented, no systematic evaluation of BCMA workarounds' causes and possible outcomes has been previously reported.
Design Objectives
The BCMAs are designed to enhance patient safety by: (1) integrating the patient's medication administration record (MAR) with the medication administration process; (2) confirming the five “rights” of medication administration: right patient, drug, dose, route, and time; and (3) helping to ensure that users, most often nurses, follow medication use and equipment use protocols.
Evaluation Research Strategy
The authors could not identify any preexisting comprehensive lists of BCMA workarounds, perhaps because so much of the literature has focused on BCMA's many and important advantages, and perhaps because of the complexity of studying the entwined processes of workarounds' causes and often sub-rosa characteristics, BCMA's evolving status (with evolving work rules), and BCMA's intricate linkages with other information technologies (ITs) (e.g., computerized physician order entry, MARs, and pharmacy IT systems and databases). As a result, this research required a multidisciplinary approach with on-the-floor observations; careful interviews conducted in situ or through detailed discussion to interpret actions taken; and analysis of BCMA-related failures. Last, because all of these elements are related to the sensitive issues of medication errors and personal actions, they are difficult to uncover via a single research approach.
Methods of Evaluation
We conducted a mixed-method study of BCMA use at a 470-bed Midwestern academic tertiary-care hospital and a four-hospital, 929-bed East Coast health care system during 2003 to 2006.
Study Genesis and Research Synthesis
Individually, we were studying BCMA use at our respective institutions or study sites (TW and B-TK: Midwest hospital; JLT: four suburban East Coast hospitals.) Upon discussing our analyses, we discovered we had been witnessing aspects of the same phenomenon: BCMA workarounds. Building on our separate research work, we combined five methods into a triangulated research effort to generate the initial workaround categories and the list of probable causes of workarounds: (1) observation of BCMA use and shadowing of staff administering medication, (2) interviews with staff and with hospital leaders involved in medication administration, (3) researcher participation in staff meetings about BCMA use, (4) a failure modes and effects analysis (FMEA) of BCMA use, and (5) analysis of BCMA override log data reflecting over 300,000 medication administrations and indicating each drug, dose, patient, and reason for overrides. (e.g., medication barcode is torn and thus unreadable by the scanner, or pharmacy sent two 20-mg tablets but the scanner will accept only one 40-mg tablet barcode).
The integration of the five methods proceeded as follows. First, observations were used to watch the BCMA work sequence leading to each workaround. Staff comments sometimes cued observers to workaround causes. Second, because the BCMA system requires the user to explain each override in a text box or pull-down menu on the BCMA's computer, the user records the perceived causes and his or her actions. These entries provided explanations that were not verbalized or seen in the observations. The other three methods—committee meetings to discuss BCMA use and override data, interviews with users to capture information not necessarily evident from the observations and BCMA data logs, and data from the FMEA about BCMA use—provided discussions and insights about workarounds by persons knowledgeable about the technology and work processes. Each of the five methods alone would provide only a subset of workarounds and causes. By using all methods and a grounded theory approach, each possible category was iteratively expanded, reduced, or eliminated. The methods and strategies are discussed in detail herein, and are reflected in ▶. ▶ ▶
Table 1.
Table 1 BCMA-Related Workarounds
| Workaround | Possible Errors | Description or Example | Data Sources |
|---|---|---|---|
| Omission of process steps | |||
| 1. User scans medication from patient drawer without visual check of medication list, medication name, and dose. | Wrong medication, dose, route | Staff are required to check the medication label and compare this visually with the eMAR before scanning. They might, however, rely on the alarms from scanning as the sole confirmation of correctness. |
|
| 2. Physicians do not review eMAR to verify current medications. | Inappropriate monitoring of medication; wrong medication, dose, route | Physicians may not be trained on, or have log-ins for, the BCMA, and therefore eMAR access is difficult. Or eMAR data are not presented in manner usable for physicians. Therefore, eMAR not routinely reviewed and physicians not aware if medications administered, held or omitted, and do not stop unneeded medications. |
|
| 3. User administers medication without reviewing parameters for medication administration. | Wrong medication, dose, route, time | BCMA system cannot show all administration information for a particular medication on one screen, therefore, an icon appears to click to see additional information. However, the icon fails to reflect if information is present or when information has been updated, and is thus missed. |
|
| 4. Users bypass policy for “medication double check” by 2nd provider, or 2nd nurse confirms without reviewing medications. | Wrong medication, dose, route | Hospitals often require a second nurse to confirm medication name, dose, and patient for high-risk medications. BCMA may be set up to require the documentation of this confirmation. Documentation may be bypassed by overriding the medication in the BCMA system or by a pro forma confirmation by another nurse. |
|
| 5. User does not check/verify patient's new medication orders before administering medication. | Wrong medication dose, route | When a new medication order is processed, the BCMA system is updated after pharmacist entry and the order is available for nurse verification, but is not final until verified. Staff might not verify order for change in the medication (dose change, discontinue, etc.) before administering the next medication dose in the eMAR. |
|
| 6. User administers medication without scanning patient ID to confirm correct patient. | Wrong patient | Nurse scans medications but does not scan patient before administering. ID wristband may be missing, damaged (by body fluids or patient), or inaccessible because patient is sleeping (and RN wishes not to disturb patient). |
|
| 7. User administers medication without scanning medication barcode to confirm it is correct medication, time, dose. | Wrong medication, dose, route, time | Medication barcode is present but not scanned, so BCMA cannot verify medication and dose. Medication barcode may be damaged or torn, soaked, or crinkled. Scanner may not be available. |
|
| Steps performed out of sequence | |||
| 8. User documents medication administration before medication is administered and/or observed ingested by patient. | Medication omitted or not administered as documented | Users are prompted to document medication administration after scanning medications. It may take significant time for the nurse to prepare medication for administration (e.g., crush tablet, assemble infusion) or for patient to ingest medications, and therefore staff documents administration first. With computer carts that do not fit into patients' rooms (see below), medications are scanned and documented as administered before patients ingest them. Medications not ingested by patients. |
|
| Unauthorized BCMA process steps | |||
| 9. Patient ID barcode placed on another object (not on patient) and user scans it. | Wrong patient | Reproducing patients' wristband ID barcodes, and affixing them to nursing station, COW, supply room, patient's room doorjamb, medication dispensing machine, RN clipboard, scanner itself, in nurses' pockets or on belt rings, or worn as a group of bangles on nurse's sleeve. Wrong patient ID may be scanned. |
|
| 10. User prepares, scans, and transports medications for >1 patient at a time when administering medications. | Wrong patient | Staff takes medications due for multiple patients from medication room and places them in their pockets or prepares them together on the medication cart. At administration, staff scans patient ID wristband but administers another patient's medications. |
|
| 11. User scans medication barcode after barcode label has been removed from the medication itself. | Wrong medication, dose, route | The barcode on the medication packaging is scanned after the medication has been removed from the package. Example: staff remove all medications from their packages and place barcodes from the medication packages on their sleeves or carts to scan them in one motion. If patient is unable to ingest all medications, unlabeled medications are left on cart. As cart is wheeled from room to room, unlabeled medications accumulate. |
|
| 12. User has multiple medication packages for full dose and scans the same medication package multiple times. | Wrong medication, dose | A nurse has multiple medication packages to deliver a full dose of medication and scans one of the packages multiple times instead of scanning each package, e.g., nurses believe that they have four 50-mg medication tablets, but one or two of the packages is of a different dosage or a different medication that looks similar in size and shape. |
|
| 13. User takes the scanner separate from cart into the room where the cart alarm cannot be seen. | Wrong patient | The computers linked to the scanning device are mounted on carts (COW). The COW may be left outside of patient's room because COWs are too big or are tethered to electric outlets. Staff scan medication barcodes outside patient's room and take medications into the room and scan the patient. But because cart is in hallway, nurse cannot see alarm indicating medication is being given to wrong patient. |
|
| 14. User gives partial dose but electronically documents full dose. | Wrong dose administered or documented as administered | Nurses scan medication barcode(s) for full dose; however, patient may refuse full dose or clinical situation warrants partial dosing of dispensed medication (e.g., syringe of morphine 10 mg is dispensed, scanned, and documented given, but only 4 mg is ordered and administered). Also, half of medication dose may be available and nurse scans the medication twice to indicate a full dose being administered, and re-orders the remainder of the medication. Documentation of a partial dose administration requires extra steps to change the order, note reason, etc. |
|
| 15. User disables audio alarms on device. | Wrong patient, medication, dose, route, time | Staff who are concerned that audible alarms will disturb patients sometimes mute the alarms. The warnings of wrong medication or patient are thus not heard. |
|
BCMA = barcoded medication administration; COW = computer on wheels; eMAR = electronic medication administration records; FMEA = failure modes and effects analysis; ID = identification.
Table 2.
Table 2 Probable Causes of BCMA Workarounds
| Probable Cause | Definitions, Explanations, and Examples from Observations ∗ and Interviews | Data Sources† |
|---|---|---|
| Technology related | ||
| 1. User exceeds preset medication administration time | BCMA system times out a user after a preset number of minutes because user has not confirmed medication administration. |
|
| 2. Multiple screens to complete action | Finding medication information, orders on eMAR, or completing administration may necessitate clicking on multiple screens, especially if user needs to change medication order, etc. User may perceive time requirements onerous. One or more screens might not be allowed (e.g., required field grayed out). |
|
| 3. Multiple scans needed to read barcode | May be due to barcode, scanning technique, or technology capabilities. User uncertain whether there is barcode confirmation. |
|
| 4. Beeps for most functions | Scanners may emit beeps for each completed function. Beeps for acceptable vs. wrong scans may be confused or ignored. |
|
| 5. Information not readily available | Users do not know how to retrieve information, e.g., allergies, parameters for administration, or are unaware it is there because of the user interface/display. |
|
| 6. Computer cart or scanner is too large, heavy, or bulky | COW does not fit into patients' rooms. Computers remain plugged into hall outlets, and cannot be moved near patients' beds. Also, reluctance to carry scanning equipment back and forth from storage areas to patient rooms. |
|
| 7. Connectivity | Most BCMA systems are linked to the eMAR on hospital's server. Lost connection—wireless or corded—prevents scanning. |
|
| 8. Battery dies or is not charged and other BCMA equipment failure | Batteries fail on handheld devices or computer carts. Experience with some batteries failing leads to charging batteries continually, leading to batteries failing more quickly. This led to replacement of batteries in all machines in all hospitals of one system. |
|
| 9. User dissatisfied with BCMA | Users know how to use BCMA systems but find them slow or cumbersome. Often this response reflects negative views of the software design. |
|
| 10. Other reported scanning failures | Users report the barcode will not scan without specifying whether difficulty is with the barcode, scanner, or other BCMA function. |
|
| 11. BCMA engenders false sense of security | Users fail to perform required safety checks because they rely on technology, e.g., they do not perform a visual check of the patient's ID band or of medication name and dose. |
|
| Task related | ||
| 12. Not typical barcode use process | Unfamiliar with variation from common procedure, e.g., barcode inside different package, medication packaging has multiple barcodes, medications from patient's home without barcodes. |
|
| 13. Standard BCMA scanning procedure slower or more difficult than other methods | Conflict between workflow efficiency and proper/safe BCMA use, e.g., extra time to scan medications or to return to supply room for each patient's medications or to retrieve scanning equipment that works. Also, emergency medication administration may be viewed as superseding scanning protocol. |
|
| 14. Packaging discarded | Medication was administered without being scanned and the packaging was discarded, preventing confirmation scan. |
|
| Organizational | ||
| 15. Only partial dose, too large of a dose available, or different formulation | Less than a full dose is available when nurse administers medications, or syringe/medication tablet contains more than the ordered dose. Nurse must alter the automatic documented administration that is based on the dose on the scanned barcode. Examples: Partial dose: Pharmacy sends 10-mg tablet rather than 20-mg tablet. Nurse must document a partial dose being administered and why. Then create an order to administer the remainder when it arrives. Or nurse may scan medication twice to document a complete medication administration, deliver the partial dose, and remember to administer remainder later. Too large dose: If, for example, patient is to receive 4 mg and the syringe contains 10 mg, the nurse scans larger dose and must override overdose alarm and/or change the automatic documentation to document a smaller administered dose. Different formulation: Use of suppository rather than oral form. |
|
| 16. Nonformulary medication | Medications or medications' identifying numbers are not yet cataloged in the hospital computer formulary, or a unique barcode has not been created by the hospital as the medication is not expected to be prescribed. Therefore, medication does not have a readable barcode. |
|
| 17. Medication order not in system | The medication order is not in the eMAR (often orders that are stat, verbal, or not yet entered by pharmacy), and thus not in the eMAR. Nurse, however, desires to administer medication promptly. |
|
| 18. Medication does not have a (readable) bar code | Barcodes often crinkled, smudged, torn, missing, or covered by another label—the latter reminding staff to scan barcode. Some medications are patients' own from home without barcodes. |
|
| 19. Patient does not have a (readable) ID wristband barcode | Patients' wristbands are cut, smudged, chewed, deteriorated by fluids, never provided, or removed. Also, patient has nonvalid ID wristband barcode from prior admission or from another hospital within the same health care system. |
|
| 20. Preparation and dispensing practices | Size of tablet or syringe stocked by hospital is larger than needed for typical medication order (e.g., morphine 10-mg syringes stocked, and typical dose is 2 mg). Also, information on medications may not yet be programmed into system. (This differs from no. 13, above, because it reflects hospital buying/stocking policies and programming workflow, rather than difficulty with an individual order.) |
|
| 21. User not trained | User's BCMA training inadequate, e.g., users do not know: (1) which of several barcodes on medications to scan, (2) which screens have needed information, (3) computer confirmation procedures, or (4) how to respond to allergy notification. |
|
| 22. Inadequate staffing | Nurses rush to complete tasks or omit steps because of insufficient staffing for patient care needs. (Stated justification for not having time to scan patients or medications.) |
|
| 23. Viewed as another's job | Nurses believe pharmacy should create orders for medications in BCMA systems when needed order is not available, should prepare medications for scanning, and should provide the exact medication dose needed for the order to avoid multiple scans for same operation (e.g., several tablets for one dose). |
|
| 24. Unfamiliar with BCMA safety features or seen as noncritical | Unaware that scanning of patients and medication barcodes affords added safety benefits beyond human checks. |
|
| 25. Unaware of hospital policies |
|
|
| 26. Safety procedures incompatible with workflow | BCMA use may slow rapid medication administration in emergency situations, especially when equipment faulty (e.g., battery dies, screen out of alignment). Also, with patients in contact isolation for infection control, bringing scanning equipment into room without covering it would contaminate it and a plastic bag cover may interfere with scanning. |
|
| Patient related | ||
| 27. Patient barcode not usable or accessible | Patient ID band torn, wet, chewed, or not on patient. Patient's ID band is covered (e.g., covered with sterile dressing for procedure or by blankets) and cannot be easily accessed. |
|
| 28. Patient activity interferes with BCMA use | Patient does not accept scanning (e.g., combative, too agitated), or the patient is engaged in an activity that makes it difficult (e.g., central line being inserted, showering, breastfeeding). Scanning or administration would disturb patient (e.g., one who is asleep). Also, patient may vomit or refuse medication after administration documented. |
|
| Environmental | ||
| 29. Medication barcode remote from scanner | When using a COW for administration, medications requiring refrigeration are not on cart. Medication barcode scanning requires carrying medication package to scanner, scanning medication, returning remaining medication to refrigerator (e.g., insulin vial), and then back to patient to administer. |
|
| 30. Loud ambient noise | Noise in hallway or patient room (e.g., intensive care unit monitors, loud talking, patient distress noise) prevents nurse hearing scanner alarms. |
|
| 31. Location does not allow appropriate BCMA use | Patient in area that does not allow BCMA use. Examples: wireless connectivity loss, patient in operating room or radiology. |
|
∗ Includes all floor observations, shadowing, BCMA, morbidity and mortality conferences, and FMEA.
† For data on 1 month's BCMA overrides logged: (1) data document existence but not prevalence of a cause; (2) some of the causes listed occur in one BCMA system studied, but not in the system for which override reasons were counted; (3) similar data may illustrate multiple causes; (4) not all causes involve overrides.
Abbreviations as in ▶.
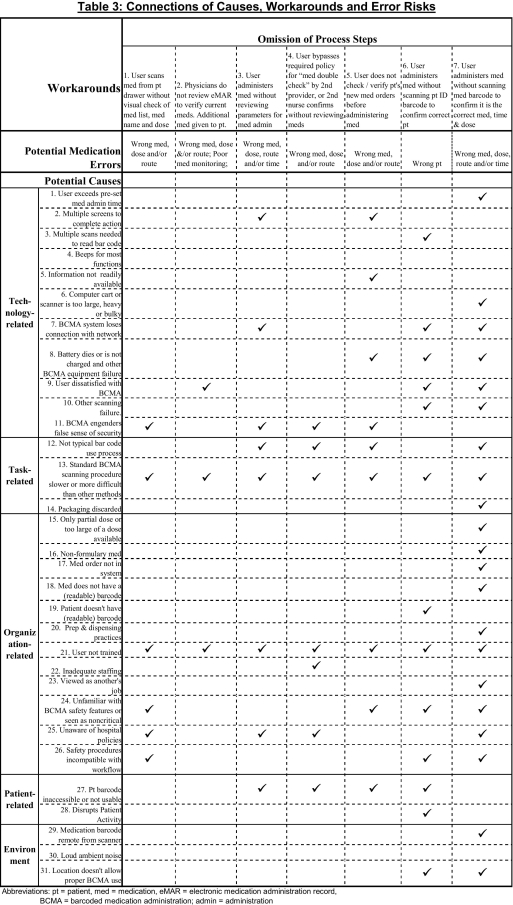
Table 3.
 |
 |
Data Sources
1 Structured observations12,18,19 (N = 62) and shadowing of nurses (N = 31) using BCMAs were conducted during medication administration at two hospitals (one Midwest, 2003–2004; one East Coast, 2005–2006). We observed both day and evening shifts in intensive care and medical surgical units. Researchers revealed that observations were conducted for a study of medication administration.
2 We conducted unstructured and semistructured interviews with three groups of participants. We interviewed 29 nurses using BCMA systems in conjunction with BCMA observations (TW,12,18,19 JLT: one Midwest, 2003–2004; and four East Coast hospitals, 2004–2006). Questions focused on the use of the BCMA and on its difficulties and advantages. At the four East Coast hospitals, we also interviewed one nursing informatics specialist, two pharmacists, and two nurse leaders (JLT). At one additional East Coast tertiary-care academic hospital, we also interviewed two IT directors, four pharmacists, and two clinical nursing directors (RK).
3 Two authors (JLT, TW; 2003–2006) participated in hospital staff meetings about BCMA use and medication administration procedures (e.g., multidisciplinary monthly operational review meetings of BCMA use, medication safety committee meetings, morbidity and mortality conferences). Through discussions beginning with detailed and aggregate computer data on alerts and overrides, the meetings with experts and frontline users explored staff practices, hospital policies, sources of and solutions to BCMA problems, and over time, the impact of efforts to improve BCMA operation and use. Meeting minutes and freehand notes were reviewed.
4 A FMEA of the medication use process and BCMA use processes was performed at the Midwest hospital from 2003–2004. The multidisciplinary team comprised four pharmacists, six nurse users, the pharmacist and nurse managers of BCMA (dedicated positions to the technology), one risk manager, two industrial engineers, two physicians (TW), one quality improvement facilitator, and the nurse patient safety officer. Team members mapped medication use processes and identified failure modes, causes of failure, and effects of failure on patient care. A total of 202 failure modes were identified, and 92 were related to BCMA use. Failures meeting definitions of workarounds, their causes, and their effects on patient safety were extracted from meeting documents.
5 We reviewed BCMA override log data for 1 month at 4 East Coast hospitals (December 2005). BCMAs record the number and types of alerts presented to users, the alert overrides, and the user's stated explanation for overriding the alert (from a standard list or free text). These explanations, both those mentioned frequently (such as medication label smudged or torn, patient wristband missing, dose differing in some way from that ordered) and those mentioned infrequently (such as patient combative, or too agitated to scan) were used to identify categories (types) and causes of workarounds. BCMA alert overrides occur when a user documents medication administration without a confirming barcode scan. This can be precipitated by an alert indicating that the scan does not match the medication order or the patient identification (ID), or when the user does not or cannot scan the barcode. Reasons for overrides are listed in ▶ and are discussed in the Results section. We then used the information from the override logs to guide additional observations and interviews at the four East Coast hospitals. In this way, the methods were iterative and reinforcing.
Data Analysis
After collecting and examining all available occurrences of apparent workarounds from each of the respective data sources, we reached an agreed-upon definition of each workaround. We examined hospital policies to ensure the occurrences were workarounds. Then we re-examined each workaround and its sources in an iterative fashion; combining the data into an overall final list of workaround types. The iterative and multiple methods helped validate each category. 20-22 When possible, subsequent interviews and our participation in meetings for FMEA, morbidity and mortality conferences, and BCMA implementation also helped validate the candidate workarounds and their causes. Only workarounds and their causes that were actually observed, reported, or documented are included in this analysis. Workaround causes were classified according to the work system model for Systems Engineering in Patient Safety (SEIPS). 23 Potential patient safety consequences of workarounds were determined by the researchers using the five rights of medication administration and associated FMEA findings.
Sample Sizes for BCMA Override Log Data
Calculation of Medication Administrations Override Percentage
We analyzed 307,698 medication administrations, of which 274,550 (89.2%) generated no alerts or alerts leading to cancellation or changing the medication. Of the remaining 33,148 alerts that were overridden, 1,376 were excluded from this analysis because the override reasons were ambiguous, or because of back-charting of medication administration, or documentation alerts. Thus there were 31,772 medication administration overrides that had listed reasons for being overridden that we could code as to cause of the override. Taking 31,772 as a percentage of the total administered and documented medication administrations equals 10.3%. In other words, 10.3% of all documented BCMA medication administrations were overridden.
Calculation of Patients' Medication Administration Override Percentage
We analyzed 142,203 instances of one or more medications administered to patients. Of those, there were no alerts or alerts leading to cancellation or changing the patient 135,328 times (95.2%). Of the remaining 3,785 alerts that were overridden, 837 were excluded from this analysis because the override reasons were ambiguous or for back-charting of medication administration. Thus there were 6,035 overrides that had reasons we could code as to the cause of the patient override. Taking 6,035 as a percentage of the total patient medication administrations equals overrides of 4.2% of administrations to patients.
This study was approved by each researcher's facility's internal review board. The BCMA vendors made hardware and software modifications in response to some of our reported findings, but no researcher was paid by them and no researcher has financial arrangements with BCMA companies.
System Description
The BCMAs usually consist of tethered or wireless handheld devices for scanning machine-readable barcodes on patients and medications, and are interfaced with electronic medication administration records (eMARs) displayed on handheld devices or computers on carts (computers-on-wheels, COWs).
BCMAs require that users: (1) scan their ID badges to access BCMAs, (2) obtain medications from supply areas, (3) check medication labels against the BCMA eMAR—a part of most BCMA systems, (4) scan medication barcodes, (5) scan the patient's ID wristband barcode, (6) administer medications, and (7) document (chart) medication administration. 12 If BCMAs detect mismatches between patient and medication or medication and medication order, audible and/or visual alerts are triggered. In response to alerts, users either change their actions (e.g., find correct patient or medications), or override alerts and document their reasons for overriding the alerts (e.g., “Gave 1/2 20-mg tab that was sent [by pharmacy] for a 10-mg order”). Similarly, if patients or medication barcodes cannot be scanned because of missing barcodes or scanning failures, users can override the scanning function to administer medications. Every BCMA alert, override, and medication administration is logged in a central computer database. In some hospitals, visual double-checks by another provider are documented for high-risk medications; in many hospitals physicians also use BCMAs to review eMARs.
Barcode Systems Studied
The BCMAs studied were Siemens Medication Administration Check using medication Admin Check version 23.4.1, InfoLogix SL series wheeled two- and four-drawer medication carts with UL2601 300-W 28-amp medical batteries, 17-inch computer monitors, and wireless HHP ImageTeam Linear scanners (implementation 6/2004–6/2005) and McKesson Corporation Horizon Admin-Rx version 4.8 point-of-care barcoding system using handheld devices to scan and display eMARs (implementation 12/2001–9/2004; upgraded to version 6.3.2 in 8/2004; upgraded to version 6.6.2 in 11/2006.) Siemens and McKesson comprise approximately 30% of the nongovernmental market of hospital BCMAs (Kelly J, Entropy Research, personal communication, February 14, 2007).
Evaluation Results
We identify 15 types of BCMA-related workarounds and 31 separate probable causes of the identified workarounds. We then present the relationships among workarounds, probable causes, and potential errors as a result of workaround occurrence.
Workarounds
We found 15 workaround types, which we placed into three broad categories (▶). We also indicated 6 types of linked potential errors with each workaround. The three workaround categories are as follows.
Omission of Process Steps (Rows 1–7)
This category reflects workarounds in which a typical process step is omitted, for example, failure to scan medication or patient ID barcodes, failure to review BCMA system computer screens or alerts, or failure to perform visual checks of medications and the eMAR.
The workaround may manifest itself in many different manners. To avoid scanning the patient's actual ID wristband, users were found to affix extra copies of patient ID barcodes on desks, scanner carts, doorjambs, supply closets, or clipboards, or to wear extra copies themselves on belt loops or their own arms. Other examples are scanning one medication barcode twice when administering two doses on the (possibly false) assumption that tablets or vials are identical, or scanning barcodes from discarded medication packaging. Medications also are not scanned when barcodes are missing or damaged (crinkled, blurred, covered by another label reminding them to scan the label, or torn).
Steps Performed Out of Sequence (Row 8)
This workaround group denotes documenting medications as administered before actually administering the medication or observing patient ingestion or administering medications and documenting it much later.
Unauthorized Process Steps (Rows 9–15)
This category describes workarounds that change how a process step is performed or that add new steps. Disabling audio alarms on BCMA devices that signal alerts or separating the scanning device from the COW are workarounds that preclude alerts from being heard or seen, thus disabling the technology's safety features.
Probable Causes of BCMA Workarounds
▶ lists the categories of workarounds' probable causes and defines and illustrates each cause. The last column lists data sources and any supportive data from the BCMA override logs. The probable cause categories are as follows.
Technology-Related Causes of Workarounds (Rows 1-11)
These include problems with BCMA software or hardware as they are used in practice, e.g., failing batteries of handheld scanners or linked computers, difficult-to-read or navigate screens, and alert beeps that sound like confirmation beeps. In addition to hardware and software limitations, these reasons include both negative and positive perceptions of the technology, i.e., resistance to BCMA use (negative), or overreliance on BCMA's ability to catch all errors (positive).
Task-Related Causes (Rows 12-14)
These include aspects of BCMA protocols with which users are unfamiliar or believed slow performance, e.g., nurses speed their work and circumvent BCMA protections by carrying several patients' medications on one tray or by not scanning medication IDs or patient IDs. Staff may also believe circumstances justify circumventing BCMAs, e.g., giving emergency medications. In other instances, they administer medications without scanning, discard the packaging, and retroactively chart (back-chart), precluding any mismatch alert.
Organizational Causes (Rows 15-26)
These are linked with most of our identified workarounds, and generally involve organizational policies incompatible with safety. Examples of these include patients or medications without barcodes (due to organizational or workflow flaws), medication barcodes covered by a label reminding users to scan barcodes, and pharmacies sending only partial doses. Hospital policy may not fit with BCMA procedures, e.g., barcodes should be placed on home-brought medications but are not. Workarounds are also enabled by inadequate technology-use training, inadequate staffing, and staff misunderstanding of BCMA's role in patient safety.
Patient-Related Causes (Rows 27-28)
These comprise staff decisions regarding patients' special circumstances, e.g., patients refusing medications, vomiting medications, sleeping, agitated, receiving central lines, or in contact isolation. Staff may therefore not scan patient IDs or document administrations before medications are ingested. For hospitals permitting home-brought medications, these medications are often not barcoded and scanned.
Environmental Causes (Rows 29-31)
These result from the hospital's physical structure and from locations of persons, medications, and related technologies, e.g., some hospital areas lack wireless BCMA connectivity (operating rooms, laboratories). Some doorways and patient room configurations hinder bedside access of the BCMA COWs. Also, medications stored remote from the scanner (e.g., those that require refrigeration) necessitate multiple trips to scan, dispense, and return. Loud ambient noise in rooms or hallways may prevent nurses from hearing scanner warning alarms.
Connecting Workarounds, Causes, and Potential Errors
In ▶, we show the relationships among workarounds, their probable causes, and the potential medication errors associated with each workaround. In the table, checked cells indicate which causes are associated with which workarounds; the row beneath the workarounds reflects the errors that may result from workarounds.
Although some causes might generate errors directly (e.g., loud ambient noise obscuring BCMA alarms, resulting in an administration error), our listed causes generally lead to workarounds, and those workarounds subsequently increase risks of errors.
Key to the impact and persistence of the workarounds is the multiplicity of relationships among causes and workarounds. In other words, workarounds may result from one or more causes and a cause may be associated with multiple workarounds. Organization-related and technology-related causes are associated with all 15 of the identified workarounds. Task-related causes, the smallest grouping, are nevertheless linked to 14 of the 15 workarounds, as most workarounds are a result of time-saving efforts. Patient issues and environmental causes each contribute to seven workarounds.
The structure and organization of clinical hospital work are factors for all 15 workarounds. For example, workarounds 6 and 7 are efforts to administer medications when confronting problematic patient or medication barcodes and/or when scanners fail. Workaround 9, affixing extra copies of patients' ID barcodes to other locations (e.g., nursing stations, clipboards, COWs, supply rooms, doorjambs, bangles around nurses' sleeves) is a time- and effort-saver allowing required computer documentation of medication and patient barcodes without the necessity (or protections) of bedside patient scanning. Not visually inspecting medication lists or medications before scanning (workaround 1) reflects confidence in the technology and saves time but increases wrong-medication and wrong-dose risks.
▶ can be read from several perspectives. Focusing on the probable causes, each of the 31 causes facilitates multiple workarounds, without simple one-to-one cause-and-effect relationships. For example, slow or difficult BCMA procedures (row 13) are associated with 14 workarounds. Medications without readable barcodes (row 18) are associated with only two categories (workarounds 7 and 12), but link to almost all potential error categories—wrong patient, medication, dose, route, and/or time.
Focusing on workarounds, we see that each workaround can result from many causes, e.g., administering medications without scanning them (workaround 7) is linked to 19 of the 31 probable causes, including almost all organizational- and task-related causes, along with many technology-related causes (in addition to risks of wrong medication, dose, and time).
Discussion
We set out to examine BCMA workarounds and their causes. We found that many workarounds were engendered by difficulties with the technology and by interactions between BCMA technologies and other environmental, technical, work processes, workloads, training, and policies. In doing so, we have documented and categorized types of workarounds during BCMA use. We identified 15 BCMA-related workarounds in three categories: omitted steps, incorrect sequence, and unauthorized steps. We find these workarounds are associated with 31 probable causes, categorized as technology-related, organizational, task-related, patient-related, and environmental. These causes include obvious difficulties in using BCMAs (e.g., unreadable or missing barcodes, large/bulky COWs, medication packages not matching prescribed doses, battery failures) along with staff-perceived limitations of BCMAs and staff overestimation of BCMA's risk-elimination abilities. Many of these causes have never been examined in this context; some are new to the barcode literature, e.g., role of refrigerated medications and distance from patients, hallway-dwelling COWS with noise-obscuring alarms, special BCMA problems of contact isolation and patient refusals.
These data show that as with all health care technologies, 24-29 suboptimal design and implementation of BCMAs can facilitate new medication administration hazards, 13-15,30-32 lead clinicians to deviate from required safe-use protocols, reduce the technology's safety benefits, 12-15 and enhance the probability of medication errors. None of these identified workarounds were malicious, and many were engendered by system design deficiencies. Although individuals are often blamed for circumventing safety rules, these rules might be viewed as inappropriate in some circumstances, e.g., waking patients to scan their IDs to administer intravenous medications. Thus, workarounds perceived as necessary by the user for patient care, efficiency, 33 or safety, 34 may be beneficial, neutral, or dangerous for patients' safety 33,35-37 Some workarounds are clearly intentional tradeoffs, e.g., providing urgently needed medications without taking the time to scan the patient or medication. Therefore, reiterating existing rules or enacting more rules may not reduce workarounds. 38-44 BCMA patient safety is best served by improving system design, workflow integration, and implementation, 27,44-46 especially BCMA-specific impediments. 47-49
Despite these difficulties, our data also suggest that BCMAs offer many valuable benefits. We have presented the number and percent of overrides, but BCMAs have an important role in alerting users to drug–patient mismatches. Unpublished data for 1 year (June 2006–May 2007) from the four East Coast hospitals indicate there were 23,828 BCMA alerts of drug or patient mismatches that apparently led users to change their action instead of overriding an alert, e.g., change the medication or patient. That is nearly four for every 1,000 times a medication was administered or patient identified. Moreover, continuing modifications to BCMAs and to hospital policies reduced several workarounds and addressed some of the software screen issues in our study hospitals. Focused educational efforts based on interim findings helped providers use the equipment more efficiently (see Recommendations section)
Although staff frequently blame the technology, and many problems are indeed due to hardware or software design, a significant source of difficulties is not malfunctioning technology but rather barriers generated by how the technology is designed for and used in organizations, and how staff respond to its use. 29,50,51 Each organization must evaluate its social, technological, and physical contexts when selecting and implementing IT, 52-56 e.g., BCMAs.
These causes (and related workarounds) are neither rare nor secret. They are hiding in plain sight, 50 obscured by faith in technology, clinicians' need to focus on patients, the medical ethos of getting the job done, limited communication among hospitals with similar systems, and dispersed oversight of BCMAs used across many clinical services and units. Persistent workarounds and their causes are reported frequently by hospital staff. Vendors know of many. Workarounds are discussed routinely by committees overseeing BCMA use. They are the focus of educational campaigns and appear in the literature. 12-14
The evolving and encompassing nature of BCMA requires direct observation of technology use, user interviews, realistic review of override data, and proactive process change. All of this information should be applied to make protocol compliance user friendly and intuitive. With rare exceptions, it should be easier to follow policy than work around it. When it is not, stressing the patient safety reasons for the protocol becomes essential, as does continual coaching of staff on protocols (in contrast to punishing for not following).
There are several limitations to our data and to generalizability. Our data undoubtedly do not enumerate all possible workarounds or causes, even though we found similar workarounds and causes across multiple hospital sites. Nurses were aware that they were being observed administering medications using BCMA. This awareness may have affected their behavior. However, the expected change in behavior would have been in favor of their greater compliance with BCMA use protocols, not in the direction of the commission of additional workarounds. Some actions originally considered workarounds may have become institutionalized as “best practices.” Our observations and data would therefore not capture these.
We studied two widely used, state-of-the-art systems, thoroughly integrated into highly regarded hospitals with considerable IT implementation resources. It is therefore likely that other institutions will find additional types of causes, workarounds, and outcomes. Upgraded BCMA versions and differing patient-load profiles will inevitably engender new and potentially unforeseeable workarounds and causes (see Recommendations section). Additionally, there are functions in advanced BCMAs (e.g., daily and lifetime limits, look-alike–sound-alike warnings, drug reconciliation) that we have not examined. These functions might offer additional protections, although we predict they would probably also offer more workaround opportunities.
Some of our causes are unequivocally linked to specific workarounds (medications that are missing barcodes cannot be scanned), and some are less tightly coupled, e.g., confusion caused by multiple barcodes on medication packages does not automatically imply that nurses will seek workarounds (and one of those multiple barcodes is probably correct). We do not infer from our data which probable causes and/or workarounds generate the most or least medication errors, or the severity of errors that may occur. This is not a study of specific errors or patient harm, so we list only types of potential errors that are facilitated by each workaround. Similarly, the override data do not directly reflect workarounds' or causes' frequencies; they are staff explanations for BCMA overrides.
This combination of research methods and data sources does not offer the same level of certainty afforded by randomized clinical trials. But the complexity of the user–machine–patient–environment–policy interface necessitates use of our multimodal and qualitative methods for gaining a deeper understanding of BCMA use in situ.
Conclusion
The research presented here provides an initial but critical step to understanding how BCMA systems are actually used in the challenging reality of hospital practice, why BCMA workarounds are so common, and what hospitals can do to find them and then to address their causes and unintended consequences. Although BCMA systems are intended to advance medication safety, our data reveal that integrating BCMAs within real-world clinical workflows requires critical attention to ensure that technology safety features are used as intended and that systems are designed to support this use. As with any technology in complex organizations, workarounds will occur.
Compliance with patient safety protocols is best achieved by configuring BCMAs for efficient as well as safe patient care. It is not enough to tell staff to “do it right.” Instead, repeated examinations and corrections of BCMAs' actual uses are needed to optimize their role in preventing medication errors. This research provides the groundwork and suggested methods to help health care organizations, clinicians, and BCMA vendors realize their patient safety and efficiency goals.
Recommendations
• Efforts to address workarounds should include investigation of technology, task, organization, patient-related, and environmental circumstances, in addition to increasing staff compliance.
• BCMA implementation requires meticulous attention to its actual use in situ. If possible, use multidisciplinary teams to review both qualitative (e.g., observational) as well as quantitative data.
• Evaluators and implementation teams should work with technology vendors to align hardware, software, user, policy, workflow, and patient safety needs. However, hospitals must maintain ultimate control.
• Ensure BCMA system design incorporates up-to-date standards for user interface design.
• Negotiate contracts that maximize vendor responsiveness to clinical, workflow, user, and safety needs, and especially oblige them to address technical problems that lead to invalid alerts and the need to override.
- • Preimplementation assessments to identify user, environment, policy, workflow, and patient issues are critical. Examples are:
- • Software interface characteristics, device size, nature and location of information in BCMA software, and methods for data acquisition should be assessed.
- • Environmental issues such as wireless coverage, interference from other machines, noise, space for COWs should be assessed.
- • Policy considerations to review might include new policies for medication administration of different medication forms, policies for what to do when scanning is not possible.
- • Patient concerns include placement of bar codes for neonates (body parts too small and sensitive for bands), children (choking hazard), and people in contact isolation.
These issues must all be considered together and not independently.
• Postimplementation assessments should drive hospital educational efforts, policy, workflow changes, and requests to vendors.
• New workarounds will emerge in response to changes in technology, workflow, and patient types. Evaluation of actual technology use must be ongoing.
Acknowledgments
The authors thank the following for their suggestions and comments on earlier drafts: Pascale Carayon, PhD, Thomas McCarter, MD, Gordon Schiff, MD, Christine Sinsky, MD, Scot Silverstein, MD, Frank Sites, RN, Sara Martin, RN, Edmund Weisberg, MS.
Footnotes
Supported in part by a grant from the Agency for Healthcare Research and Quality (AHRQ), P01 HS11530-01, Improving Patient Safety Through Reduction in Medication Errors (RK), AHRQ Grant 1-UC1 HS014253-01 (TW) and a Clinical Research Scholar Award from the National Institutes of Health (1 K12-RR01764-01) (TW).
References
- 1.Institute of Medicine Preventing Medication ErrorsWashington DC: The National Academies Press; 2007.
- 2.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: Implications for prevention JAMA 1995;274:29-34. [PubMed] [Google Scholar]
- 3.Kopp BJ, Erstad BL, Allen ME, Theodorou AA, Priestley G. Medication errors and adverse drug events in an intensive care unit: Direct observation approach for detection Crit Care Med 2006;34:415-425. [DOI] [PubMed] [Google Scholar]
- 4.Walsh KE, Kaushal R, Chessare JB. How to avoid paediatric medication errors: A user's guide to the literature Arch Dis Child 2005;90:698-702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events JAMA 1995;274:35-43. [PubMed] [Google Scholar]
- 6.Bates DW. Using information technology to reduce rates of medication errors in hospitals BMJ 2000;320:780-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wald H, Shojania KG. Prevention of misidentificationsIn: Shojania KG, Duncan BW, McDonald KM, Wachter RM, editors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Rockville, MD: Agency for Healthcare Research and Quality; 2001. [PMC free article] [PubMed]
- 8.Poon EG, Cina JL, Churchill W, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar code technology in the pharmacy Ann Intern Med 2006;145:426-434. [DOI] [PubMed] [Google Scholar]
- 9.Coyle GA, Heinen M. Scan your way to a comprehensive electronic medical record. Augment medication administration accuracy and increase documentation efficiency with bar coding technology. Nurs Manag 2002;33:5658–9. [DOI] [PubMed] [Google Scholar]
- 10.Johnson CL, Carlson RA, Tucker CL, Willette C. Using BCMA software to improve patient safety in Veterans Administration Medical Centers J Healthc Inform Manag 2002;16:46-51. [PubMed] [Google Scholar]
- 11.Puckett F. Medication-management component of a point-of-care information system Am J Health Syst Pharm 1995;52:1305-1309. [DOI] [PubMed] [Google Scholar]
- 12.Carayon P, Wetterneck TB, Schoofs Hundt A, et al. Evaluation of nurse interaction with bar code medication administration (BCMA) technology in the work environment J Patient Saf 2007;3:34-42. [Google Scholar]
- 13.Patterson ES, Cook RI, Render ML. Improving patient safety by identifying side effects from introducing bar coding in medication administration J Am Med Inform Assoc 2002;9:540-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patterson ES, Rogers ML, Chapman RJ, Render ML. Compliance with intended use of bar code medication administration in acute and long-term care: An observational study Human Factors 2006;48:15-22. [DOI] [PubMed] [Google Scholar]
- 15.Wideman MV, Whittler ME, Anderson TM. Barcode medication administration: Lessons learned from an intensive care unit implementationIn: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation. Vol 3. Rockville, MD: Agency for Healthcare Research and Quality; 2005. pp. 437-451. [PubMed]
- 16.Reason J, Manstead A, Stradling S, Baxter J, Campbell K. Errors and violations on the roads: A real distinction? Ergonomics 1990;33:1315-1332. [DOI] [PubMed] [Google Scholar]
- 17.Courtright JF, Acton WH, Frazier ML, Lane W. Effects of workarounds on perceptions of problem importance during operational testing 1988. Presented at: Human Factors Society 32nd Annual Meeting, October 24–28; Anaheim, California.
- 18.Carayon P, Wetterneck TB, Hundt AS, et al. Observing nurse interaction with medication administration technologiesIn: Henriksen K, Battles JB, Marks E, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation. Rockville, MD: Agency for Healthcare Research and Quality; 2005. pp. 349-364.
- 19.Carayon P, Wetterneck TB, Hundt AS, et al. Assessing nurse interaction with medication administration technologies: The development of observation methodologiesIn: Khalid HM, Helander MG, Yeo AW, editors. Work With Computing Systems 2004. Kuala Lumpur, Malaysia: Damai Sciences; 2004. pp. 319-324.
- 20.Cooper H, Hedges LV. Handbook of Research SynthesisNew York, NY: Russell Sage Foundation; 2004.
- 21.Glaser B. The Grounded Theory Perspective3rd ed.. Mill Valley, CA: Sociology Press; 2006.
- 22.Miles MB, Huberman AM. Qualitative Data Analysis2nd ed.. Thousand Oaks, CA: Sage; 1994.
- 23.Carayon P, Hundt AS, Karsh B, et al. Work system design for patient safety: The SEIPS model Qual Saf Health Care 2006;15(Suppl I):i50-i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gosbee JW, Gosbee LL. Using Human Factors Engineering to Improve Patient SafetyChicago, IL: Joint Commission Resources; 2005.
- 25.Harrison M, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care—An interactive sociotechnical analysis J Am Med Inform Assoc 2007;14:542-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holden RJ, Karsh B. A theoretical model of health information technology behavior Behav Inf Technol 2007:1-17DOI: 10.1080/01449290601138245.
- 27.Karsh B, Alper SJ, Holden RJ, Or KL. A human factors engineering paradigm for patient safety—Designing to support the performance of the health care professional Qual Saf Health Care 2006;15(Suppl I):i59-i65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.In: Schiff G, editor. Getting Results: Reliably Communicating and Acting on Critical Test Results. Chicago, IL: Joint Commission Resources; 2006.
- 29.Wears RL, Berg M. Computer technology and clinical work: Still waiting for Godot JAMA 2005;293:1261-1263. [DOI] [PubMed] [Google Scholar]
- 30.Karsh B. A conceptual framework for understanding the safety implications of bar code enabled point of care (BPOC) systems 2005. Presented at: 11th International Conference on Human–Computer Interaction; Las Vegas.
- 31.Karsh B, Scanlon M. Using bar code technology for medication administration: Special human factors considerations for pediatric populations Proc Intern Conf Healthc Syst Ergon Patient Saf 2005:135-138.
- 32.McDonald CJ. Computerization can create safety hazards: A bar-coding near miss Ann Intern Med 2006;144:510-516. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi M, Fussell SR, Xiao Y, Seagull FJ. Work coordination, workflow, and workarounds in a medical context 2005. Presented at: CHI '05: Conference on Human Factors in Computing Systems; Portland, OR.
- 34.Reason J, Parker D, Lawton R. Organizational controls and safety: The varieties of rule-related behavior J Occup Organizational Psychol 1998;71:289-304. [Google Scholar]
- 35.Koppel R. Commentary: What do we know about medication errors made via A CPOE system versus those made via handwritten orders? J Crit Care 2005;9:427-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koppel R, Localio AR, Cohen A, Strom BL. Neither panacea nor black box: Responding to three Journal of Biomedical Informatics papers on computerized physician order entry systems J Biomed Inform 2005;38:267-269. [DOI] [PubMed] [Google Scholar]
- 37.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors JAMA 2005;293:1197-1203. [DOI] [PubMed] [Google Scholar]
- 38.Almaberti R. The paradoxes of almost totally safe transportation systems Saf Sci 2001;37:109-126. [Google Scholar]
- 39.Cook R, Rasmussen J. “Going solid”: A model of system dynamics and consequences for patient safety Qual Saf Health Care 2005;14:130-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Polet P, Vanderhaegen F, Amalberti R. Modelling border-line tolerated conditions of use (BTCU) and associated risks Saf Sci 2003;41:111-136. [Google Scholar]
- 41.Rasmussen J. Risk management in a dynamic society: A modelling problem Saf Sci 1997;27:183-213. [Google Scholar]
- 42.Reason J. A systems-approach to organizational error Ergonomics 1995;38:1708-1721. [Google Scholar]
- 43.Alper SJ, Karsh B, Holden RJ, Scanlon M, Patel N, Kaushal R. Protocol violations during medication administration in pediatrics 2006. Presented at: Human Factors and Ergonomics Society 50th Annual Meeting; San Francisco, CA.
- 44.Alper SJ, Scanlon M, Kaushal R, Shalaby TM, Karsh B. Using the technology acceptance model to predict violations in the medication administration process 2007. Paper presented at: Human Factors and Ergonomics Society 51st Annual Meeting; Baltimore, MA.
- 45.Karsh B. Beyond usability for patient safety: Designing effective technology implementation systems Qual Saf Healthc 2004;13:388-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wears RL. Beyond error Acad Emerg Med 2000;7:1175-1176. [DOI] [PubMed] [Google Scholar]
- 47.American Hospital AssociationHealth Research and Education TrustInstitute for Safe Medication Practice Assessing Bedside Bar-Coding Readinesshttp://www.medpathways.info/medpathways/tools/tools.html 2000. Accessed Aug 22, 2006.
- 48.Cummings J, Bush P, Smith D, Matuszewski K. Bar-coding medication administration overview and consensus recommendations Am J Health Syst Pharm 2005;62:2626-2629. [DOI] [PubMed] [Google Scholar]
- 49.Patterson ES, Rogers ML, Render M. Fifteen best practice recommendations for bar-code medication administration in the Veterans Health Administration Jt Comm J Qual Saf 2004;30:355-365. [DOI] [PubMed] [Google Scholar]
- 50.Nemeth C, Cook R. Hiding in plain sight: What Koppel et al. tell us about healthcare IT J Biomed Inform 2005;38:262-263. [DOI] [PubMed] [Google Scholar]
- 51.Nemeth C, Nunnally M, O'Connor M, Klock PA, Cook R. Getting to the point: Developing IT for the sharp end of healthcare J Biomed Inform 2005;38:18-25. [DOI] [PubMed] [Google Scholar]
- 52.Battles JB, Dixon NM, Borotkanics RJ, Rabin-Fastmen B, Kaplan HS. Sensemaking of patient safety risks and hazards Health Serv Res 2006;41:1555-1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamilton-Escoto K, Hallock M, Wagner J, Karsh B. Using variance analysis to detect hazards in a bar-code assisted medication preparation process Jt Comm J Qual Saf 2004;30:622-628. [DOI] [PubMed] [Google Scholar]
- 54.Wetterneck TB, Skibinski KA, Roberts TL, et al. Using failure mode and effects analysis to plan implementation of smart I.V. pump technology Am J Health Syst Pharm 2006;63:1528-1538. [DOI] [PubMed] [Google Scholar]
- 55.Marx DA, Slonim AD. Assessing patient safety risk before the injury occurs: An introduction to sociotechnical probabilistic risk modeling in health care Qual Saf Health Care 2003;12(Suppl II):ii33-ii38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McCarter TG, Centafont RD, Farrah N, Kokoricha T, Leander Po JZ. Reducing medication errors: A regional approach for hospitals drug safety Drug Saf 2003;26:937-950. [DOI] [PubMed] [Google Scholar]


