Abstract
Objective
Assess patient knowledge of and response to drug cost sharing.
Study Setting
Adult members of a large prepaid, integrated delivery system.
Study Design/Data Collection
Telephone interviews with 932 participants (72 percent response rate) who reported knowledge of the structures and amounts of their prescription drug cost sharing. Participants reported cost-related changes in their drug adherence, any financial burden, and other cost-coping behaviors. Actual cost sharing amounts came from administrative databases.
Principal Findings
Overall, 27 percent of patients knew all of their drug cost sharing structures and amounts. After adjustment for individual characteristics, additional patient cost sharing structures (tiers and caps), and higher copayment amounts were associated with reporting decreased adherence, financial burden, or other cost-coping behaviors.
Conclusions
Patient knowledge of their drug benefits is limited, especially for more complex cost sharing structures. Patients also report a range of responses to greater cost sharing, including decreasing adherence.
Keywords: Drug cost sharing and benefits, financial incentives, knowledge, adherence, financial burden
In the face of rising prescription drug costs in the United States (Kaiser Family Foundation 2004), cost sharing has become more complex. For example, patients might face different copayment amounts for generic and brand name drugs (multitier benefits), and out-of-pocket costs for the same drug can vary at different points in time (such as with annual benefit caps). Despite the increasing complexity of cost sharing structures, few studies have examined how well patients know their actual drug costs, or have determined their specific responses to this mixture of incentives.
Moreover, higher cost sharing can have unintended consequences, especially in the case of prescription drugs that have documented effectiveness (Adams et al. 2001; Huskamp et al. 2003; Mojtabai and Olfson 2003; Briesacher et al. 2004; Goldman et al. 2004; Rice and Matsuoka 2004; Hsu et al. 2006). Cost-related reductions in medication use without physician consultation could lead to poor health. Even in the absence of drug use changes, higher patient out-of-pocket drug costs could create financial burdens.
Through telephone interviews with insured patients within a prepaid integrated delivery system, we assessed participants' knowledge of the structures and amounts of their drug cost sharing, and whether these costs had caused them to take less of their medications than prescribed. We also asked participants if their drug costs created a financial burden, and about other methods they used to help cope with these costs.
METHODS
Setting
Kaiser Permanente Northern California (KPNC) is an integrated delivery system (IDS) providing comprehensive medical care including prescription drugs. During the study period (2003), IDS members either had one copayment for all covered drugs (one-tier) or different copayments for brand name and generic drugs (two-tier); some also had an annual pharmacy benefit cap, a coverage threshold over which patients paid the full cost of prescription drugs. Members could also have copayments for other medical services.
Population
This population is a subset of a larger study on clinical and economic effects of cost sharing. The source population included approximately 2 million KPNC adult members in January 2000 who remained members at the time of the survey. The study sample was stratified by age, with 30 percent randomly selected from the overall adult population and the remaining 70 percent solely from members age 65 or older. We over-sampled from the 65+ group because of concerns that this group might be more vulnerable to the effects of cost sharing. In this paper, when we have found similar results in both age groups, we have given results for the overall population with proper weighting based on the stratified sampling proportions.
Additional details about the study sample selection and data collection methods are available in our previous publication (Reed et al. 2005). Overall, 72 percent of the eligible sample participated in the study. Participants were similar (p>.05) to nonparticipants with respect to age, gender, mean prescription copayment amounts, mean number of prescription drugs taken in the previous 12 months, and a comorbidity score (defined later).
Interview Data
We asked participants whether they had to pay any copayment for prescription drugs, whether they paid a different amount for brand name and generic drugs (tiered structure), and how much they paid. We also asked if they faced any annual prescription medication benefit cap, and how much their cap was. If participants were uncertain about the exact amount of their cost sharing, the interviewer encouraged them to give their best guess. We asked all participants who reported any drug cost sharing if, in the past 12 months, the amount they had to pay for drugs had caused them to change their behavior in 12 specific ways. Participants were able to report multiple types of behaviors within the previous 12 months.
We asked about three Decreased Adherence behaviors, grouping behaviors that indicated if patients had not taken all of their prescribed medication:
Taking less of a drug than the prescribed amount to make it last longer (without their doctor's advice).
Not filling a prescription for a new medication.
Not refilling an existing prescription.
Next, we asked if the amount they paid for their prescription drugs had been a serious Financial Burden, causing them to:
Borrow money to pay for medications; or
Go without a necessity in order to pay for medications.
Finally, the third category of behaviors represented other ways that patients might adapt how they obtained medications in response to costs (without necessarily reducing their adherence or creating serious financial burdens). We asked participants to report any of the following other Cost-Coping behaviors:
Switching to a cheaper medication such as a generic.
Borrowing medications from a friend or family member.
Obtaining free samples from a doctor.
Purchasing drugs from an out-of-system pharmacy.
Using a pharmacy assistance program.
Purchasing drugs from an Internet pharmacy.
Splitting pills on the advice of their doctor.
The interview also collected demographic data including gender, race, marital status, self-reported health status, education, and household income.
Health System Data
Using the IDS's administrative data, we determined participant's actual prescription drug cost sharing structure and levels, and the number of prescription drugs filled in the previous 12 months. We also calculated each participant's comorbidity score using the prospective DxCG score, which is based on ambulatory and hospital diagnoses during the previous calendar year and has been adopted for Medicare payment risk adjustment (Ellis et al. 1996; Ash et al. 2000).
Data Analysis
To examine knowledge, we estimated the percentage of participants who correctly report each cost sharing structure and copayment level. To examine the behavioral responses, we estimated the percent of participants who reported any behavior change, any Decreased Adherence, Financial Burden, or Cost-Coping behavior, and each individual behavior. For analyses that pertain to the overall membership, estimates of proportions and logistic regression analyses were weighted by the reciprocal of the age-group sampling proportions using survey commands (svy) in Stata version 8.0.
To examine the association between knowledge or behavior and individual characteristics, we used multivariate logistic regression. The individual characteristics used in these analyses were age (65+), gender, race/ethnicity, education, marital status, annual household income, health status, comorbidity score (DxCG), and number of prescription drugs filled in the past 12 months. We also included variables for the generic drug copayment amount, the differential between brand name and generic copayment amounts, and having any drug benefit cap. Sampling weights were used so coefficients of other predictors would not be biased. Because participants were not always fully knowledgeable about their cost sharing, both self-reported and actual cost sharing were examined in association with reported Decreased Adherence, Financial Burden, and Cost-Coping behaviors. The findings in these analyses were comparable in direction and magnitude for self-report and actual cost sharing. In this paper, we show results that use self-reported cost sharing.
RESULTS
Overall, 932 participants completed the study interview: 91 percent had received at least one prescription drug in the previous 12 months. Table 1 displays the participants' individual characteristics.
Table 1.
Participant Characteristics
| Characteristic | Total (n = 932) (%) | Sample A: Overall Population (n = 254) (%) | Sample B: Age 65+ (n = 678) (%) |
|---|---|---|---|
| Age 65+ years | 77.7 | 14.2 | 100.0 |
| Female gender | 55.8 | 50.5 | 58.8 |
| Nonwhite race | 26.2 | 35.5 | 22.7 |
| Education: less than college graduate | 67.2 | 59.0 | 69.7 |
| Married | 63.9 | 71.6 | 61.6 |
| Household income: <$35,000 | 43.2 | 18.8 | 51.3 |
| Self reported health excellent or very good | 44.4 | 53.7 | 41.6 |
| Persons with any prescription meds within 12 months | 90.9 | 82.1 | 93.5 |
| Persons with any ED visits within 12 months | 23.8 | 21.7 | 24.7 |
Knowledge of Cost Sharing Structures
Among participants, 7.1 percent actually had no drug cost sharing, 29.0 percent had a one-tiered copayment with no cap, 56.1 percent had a two-tiered copayment with no cap, and 7.8 percent had a two-tiered copayment and a benefit cap. Table 2 shows participants' self-reported cost sharing among those with each of the four actual cost sharing structures. Overall, 56.3 percent of participants correctly reported their drug cost sharing structure (55.8 percent were correct among those under age 65 and 59.2 percent were correct among those age 65+, p = .39).
Table 2.
Knowledge of Drug Cost Sharing Structures: Self-Reported Structure Compared to Actual Structure*
| Actual Cost Sharing Structure | |||||
|---|---|---|---|---|---|
| Self-Reported Cost Sharing Structure | None (No Cost) (%) | One-Tiered Copay/ No Cap (%) | Two-Tiered Copay/ No Cap (%) | Two-Tiered Copay/Cap (%) | Total (%) |
| None (no cost) | 85.9 | 4.5 | 2.3 | 2.9 | 8.6 |
| One-tiered copay/no cap | 7.1 | 68.1 | 36.5 | 16.2 | 42.1 |
| Two-tiered copay/no cap | 0.3 | 17.6 | 47.3 | 8.3 | 32.2 |
| One-tiered copay/cap | 6.7 | 3.7 | 5.5 | 17.4 | 6.0 |
| Two-tiered copay/cap | 0.0 | 0.2 | 4.0 | 47.4 | 6.1 |
| No response | 0.0 | 6.0 | 4.4 | 8.0 | 4.9 |
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Percentages who reported each type of behavioral response or category, weighted for sampling proportions.
One-tier refers to a single copayment amount for prescription drugs; two-tier refers to one copayment amount for generic drugs and another copayment amount for brand-name drugs. Cap refers to an annual drug benefit cap, above which patients pay for the full price of their drugs. There was no actual plan available with one-tiered copayand cap. No response refers to participants who reported that they did not know how much they had to pay and could not guess.
After adjusting for individual characteristics among those with a two-tiered plan, participants who were over age 65 (odds ratio [OR]: 2.70, 95 percent confidence interval [CI]: 1.14–6.22) and participants with greater drug use in the previous 12 months (OR for 2–4 versus 1 drug=2.73, 95 percent CI: 1.03–7.21; OR for 5+ versus 1 drug=10.04, 95 percent CI: 2.60–38.78) were significantly more likely to know that they had a tiered plan.
Knowledge of Cost Sharing Amounts
Actual single-tiered copayments ranged from $1 to $15; two-tiered plans had generic copayments of either $5 or $10, and brand-name drug copayments of $10–$35.
Table 3 shows the percentage of respondents who correctly reported their generic copayment and brand name copayment amounts, and the percentage that overestimated or underestimated their copayment by $5 or more. Overall, 27.2 percent of all participants correctly identified the structure and exact amounts of all of their prescription drug cost sharing.
Table 3.
Knowledge of Drug Cost Sharing Amounts: Self-Reported Copayment Compared to Actual Copayment*
| Generic Copayment | Brand-Name Copayment | |||||
|---|---|---|---|---|---|---|
| All Participants (%) | Age <65 (%) | Age 65+ (%) | All Participants (%) | Age <65 (%) | Age 65+ (%) | |
| Overestimated by >$5 | 10.7 | 10.7 | 10.7 | 7.6 | 7.1 | 9.8 |
| Overestimated by $1–5 | 14.0 | 14.7 | 10.3 | 9.1 | 10.1 | 3.9 |
| Exactly correct | 65.2 | 63.8 | 71.8 | 40.5 | 39.6 | 45.0 |
| Underestimated by $1–5 | 9.6 | 10.2 | 6.9 | 21.3 | 23.1 | 12.4 |
| Underestimated by >$5 | 0.5 | 0.6 | 0.3 | 21.6 | 20.1 | 28.9 |
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Percentages who reported each type of behavioral response or category, weighted for sampling proportions.
In analyses adjusting for individual characteristics, participants with larger actual generic copayment (OR per $5 increment: 0.40, 95 percent CI: 0.79–0.87) were significantly less likely to know the exact amount of their generic copayment, as were those under age 65 (OR: 0.47, 95 percent CI: 0.22–1.00). Similarly, among those with tiered copayments, those with larger brand copayment differential (OR per $5 increment: 0.59 [0.39–0.91] and those who took less medications (OR 1 versus 2–4 drugs: 0.23, 95 percent CI: 0.09–0.56; OR 1 versus 5+ drugs: 0.23, 95 percent CI: 0.07–0.70) were significantly less likely to know their brand copayment (detailed results available from authors upon request).
Decreased Adherence, Financial Burden, and Other Cost-Coping Behaviors
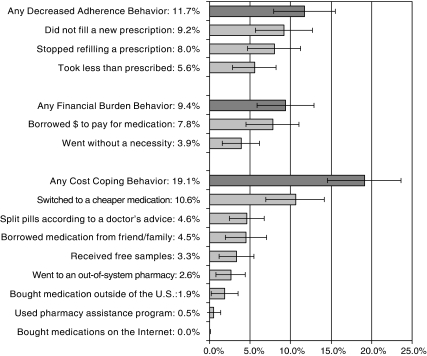
Figure 1 shows that 11.7 percent of participants reported that their drug costs caused them to be less adherent to prescription medications in the previous 12 months. Table 4 displays the patient characteristics associated with reports of decreased adherence because of costs. Report of having a benefit cap was strongly associated with reports of decreased adherence (OR: 3.79, 95 percent CI: 1.39, 10.34). In adjusted multivariate models, participants age 65 years or older, and those who took fewer drugs were significantly less likely to report decreased adherence.
Figure 1.
Self-Reported Behavioral Responses to Cost Sharing*
*Percentages who reported each type of behavioral response or category, weighted for sampling proportions, with 95 percent confidence intervals.
Table 4.
Self-Reported Behavioral Response to Drug Cost Sharing*
| Decreased Adherence Behavior | Financial Burden Behavior | Cost-Coping Behavior | ||||
|---|---|---|---|---|---|---|
| Characteristic | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Drug cost sharing: | ||||||
| Generic drug copayment ($5 increment) | 1.34 | 0.99, 1.81 | 1.50‡ | 1.11, 2.04 | 1.40† | 1.00, 1.94 |
| Brand – generic copayment difference ($5 increment) | 1.08 | 0.96, 1.23 | 1.03 | 0.89, 1.19 | 1.24† | 1.02, 1.51 |
| Any benefit cap | 3.79‡ | 1.39, 10.34 | 3.97† | 1.06, 14.87 | 1.65 | 0.65, 4.21 |
| Age 65+ years | 0.32† | 0.12, 0.83 | 0.19† | 0.05, 0.69 | 1.32 | 0.60, 2.89 |
| Female gender | 3.17 | 1.06, 9.44 | 3.23 | 0.68, 15.40 | 0.89 | 0.36, 2.20 |
| Nonwhite race | 1.65 | 0.56, 4.86 | 0.89 | 0.26, 3.02 | 1.17 | 0.53, 2.56 |
| Education: less than college graduate | 1.15 | 0.40, 3.34 | 2.90 | 0.77, 10.82 | 1.82 | 0.71, 4.63 |
| Married | 1.99 | 0.51, 7.72 | 3.45 | 0.86, 13.83 | 1.28 | 0.53, 3.07 |
| Household income <$35,000 | 1.78 | 0.45, 6.93 | 9.73‡ | 2.58, 36.75 | 1.09 | 0.40, 2.96 |
| Self-reported health excellent or very good | 0.78 | 0.26, 2.35 | 0.40 | 0.10, 1.55 | 0.44 | 0.18, 1.05 |
| Number of medications used in 12 months | ||||||
| 0 | 42.81 | 5.13, 357.00 | NA | NA | ||
| 1 | 1.00 | (Reference group) | 1.00 | (Reference group) | 1.00 | (Reference group) |
| 2–4 | 13.31 | 3.25, 54.46 | 2.05 | 0.39, 10.80 | 1.21 | 0.38, 3.85 |
| 5+ | 73.77 | 14.40, 377.91 | 4.68 | 0.55, 39.84 | 2.14 | 0.55, 8.39 |
Multivariate logistic regression, weighted for sampling proportions, adjusted for comorbidity score; because those who used zero medications in the previous 12 months did not report any financial burden or cost-coping behavioral responses, they are not included in these analyses. There were no statistically significant interactions between cost sharing structures and levels.
CI, confidence interval; OR, odds ratio.
p<.05.
p<.01.
Among participants who had to pay any share of their prescription drug costs, 9.4 percent reported borrowing money to pay their drug costs or that drug costs caused them to go without a necessity (Figure 1). The amount of the generic copayment was significantly associated with reporting increased financial burden (OR per $5: 1.50, 95 percent CI: 1.11–2.04), as was report of a benefit cap (OR: 3.97, 95 percent CI: 1.06–14.87). Participants who were younger than age 65 and those with lower household income were more likely to report a financial burden behavior (Table 4).
Overall, 19.1 percent of participants with drug cost sharing reported that their costs caused them to do at least one of the eight other cost-coping behaviors (Figure 1). The amount of the participant's generic drug copayment (OR per $5: 1.40, 95 percent CI: 1.00–1.94) and the brand generic copayment difference (OR per 5 percent: 1.24, 95 percent CI: 1.02–1.51) were significantly associated with cost-coping behavior (Table 4).
DISCUSSION
Patients are facing prescription drug benefits that require increasing out-of-pocket costs and that are more complex in structure. We found that patients typically know whether they have any prescription drug cost sharing, but have limited knowledge of important details, such as whether they have tiered copayments or an annual benefit cap. While patients generally know their generic drug copayment, many underestimate their costs for brand name drugs. Few patients know both the structure and amounts of their cost sharing.
Despite limited knowledge, nearly one in four patients report changing their behavior in response to their perceived level of prescription drug cost sharing. Over one in 10 patients report decreasing their drug adherence because of costs, nearly one in 10 report borrowing money or going without some necessity because of drug costs, and nearly one in five report engaging in some other cost-coping behavior. These reports of increased financial burden are surprising given that all patients in this study had comprehensive health insurance, and none were on Medicaid. The strong association between lower household income and reports of financial burden points to the need to adapt cost sharing policies to lessen the burden for patients with lower income or wealth. Not surprisingly, patients who have greater levels of drug cost sharing (generic copayment) or additional cost sharing structures (which could represent higher drug costs such as tiered copayments or a benefit cap) are more likely to report these behaviors.
Our findings about cost-related decreased adherence are consistent with other findings of decreased drug utilization with increased cost sharing in multiple delivery settings and in several drug classes (Stuart and Zacker 1999; Mojtabai and Olfson 2003; Taira et al. 2003; Hsu et al. 2004; Piette and Heisler 2004; Piette et al. 2004; Reed et al. 2005). The decreased adherence raises concerns about whether these choices might put patients at increased risk of worse health outcomes. While our study focuses on patients' self-reported behavior in response to prescription drug cost sharing, it complements recent results from a study examining automated data for a large population over age 65 within the same IDS which show consistent negative clinical and economic consequences from decreased adherence observed in response to the drug benefit cap (Hsu et al. 2006).
This study has the unique ability to examine both self-reported and actual drug cost sharing. Patients' limited knowledge of their drug cost sharing increases the importance of examining both perceived cost sharing amounts and their impacts. More importantly, additional effort is needed to provide patients with adequate knowledge of their costs and of the range of alternatives if cost sharing is to create an effective incentive without concomitant undesired effects. Improving provider awareness of patient costs may also help them to actively assist patients in adapting to costs without making unsafe choices about avoiding prescription drugs.
Several other studies also found limited understanding about health coverage details (Cafferata 1984; McCormack 2002; Hsu et al. 2004; Reed et al. 2005), suggesting a need to educate patients if they are to be judicious consumers. Similar to an earlier study, higher complexity of the benefit structure results in a lower proportion of persons who correctly understood their benefits (Table 2) (Marquis 1983). More informed patients might be better able to plan for costs or explore alternatives such as asking their physician for more affordable options. The need for better information and education might become particularly pronounced as the complexity of drug benefits and the amount of cost sharing both increase. For example, Medicare beneficiaries face a range of cost sharing amounts and structures that change with the yearly cumulative amount of drug expenditure (Stuart et al. 2005). Early reports suggest some confusion among these beneficiaries about their plan options alone (Kaiser Family Foundation 2005).
It is important to note that our study focused on patients enrolled in a prepaid, integrated delivery system with a high level of care coordination, and with low levels of brand-name drug use. In other less coordinated care settings, the likelihood of poor drug adherence may even be higher. The drug cost sharing levels in this study also are arguably more modest and less complex than those in other plans available in the market (e.g., benefit caps and gaps, deductibles, larger numbers of tiers), including the cost sharing in many Medicare Part D drug plans. If faced with higher levels of cost sharing and more complex cost sharing structures, patients might reduce their drug adherence and use other coping behaviors more often than we observed.
Overall, our findings suggest that patients have limited knowledge of their drug benefits. Despite this limited knowledge, many patients report changing their drug use behavior in response to cost sharing, some taking less medication than prescribed, and some reporting that the drug costs create a substantial financial burden. The full economic and health implications of these behaviors are important to explore further, particularly for population groups that might be vulnerable to adverse effects.
REFERENCES
- Adams A S, Soumerai S B, Ross-Degnan D. The Case for a Medicare Drug Coverage Benefit: A Critical Review of the Empirical Evidence. Annual Review of Public Health. 2001;22:49–61. doi: 10.1146/annurev.publhealth.22.1.49. [DOI] [PubMed] [Google Scholar]
- Ash A, Ellis R, Pope G C, Ayanian J Z, Bates D W, Burstin H, Iezzoni L I, MacKay E, Yu W. Using Diagnoses to Describe Populations and Predict Costs. Health Care Finance Review. 2000;21:7–28. [PMC free article] [PubMed] [Google Scholar]
- Briesacher B, Kamal-Bahl S, Hochberg M, Orwig D, Kahler K H. Three-Tiered-Copayment Drug Coverage and Use of Nonsteroidal Anti-Inflammatory Drugs. Archives of Internal Medicine. 2004;164(15):1679–84. doi: 10.1001/archinte.164.15.1679. [DOI] [PubMed] [Google Scholar]
- Cafferata G. Knowledge of Their Health Insurance Coverage by the Elderly. Medical Care. 1984;22(9):835–47. doi: 10.1097/00005650-198409000-00008. [DOI] [PubMed] [Google Scholar]
- Ellis R, Pope G, Iezzoni L, Ayanian J Z, Bates D W, Burstin H, Ash A S. Diagnosis-Based Risk Adjustment for Medicare Capitation Payments. Health Care Finance Review. 1996;17:101–28. [PMC free article] [PubMed] [Google Scholar]
- Goldman D, Joyce G, Escarce J, Pace J, Solomon M, Laouri M, Landsman P, Teutsch S. Pharmacy Benefits and the Use of Drugs by the Chronically Ill. Journal of American Medical Association. 2004;291(19):1344–50. doi: 10.1001/jama.291.19.2344. [DOI] [PubMed] [Google Scholar]
- Hsu J, Price M, Huang J, Brand R, Fung V, Hui R, Fireman B, Newhouse J P, Selby J V. Medicare Drug Benefit Caps: Unintended Consequences. New England Journal of Medicine. 2006;354(22):2349–59. doi: 10.1056/NEJMsa054436. [DOI] [PubMed] [Google Scholar]
- Hsu J, Reed M, Brand R, Fireman B, Newhouse J P, Selby J V. Cost-Sharing: Patient Knowledge and Effects on Seeking Emergency Department Care. Medical Care. 2004;42(3):290–6. doi: 10.1097/01.mlr.0000114917.50457.52. [DOI] [PubMed] [Google Scholar]
- Huskamp H A, Deverka P A, Epstein A M, Epstein R S, McGuigan K A, Frank R G. The Effect of Incentive-Based Formularies on Prescription–Drug Utilization and Spending. New England Journal of Medicine. 2003;349(23):2224–32. doi: 10.1056/NEJMsa030954. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. 2004. Employer Health Benefits: 2003 Annual Survey, Kaiser Family Foundation.”.
- Kaiser Family Foundation. 2005. The Medicare Drug Benefit: Beneficiary Perspectives Just before Implementation, Kaiser Family Foundation/Harvard School of Public Health.”.
- Marquis M. Consumers' Knowledge about Their Health Insurance Coverage. Health Care Finance Review. 1983;5(1):65–80. [PMC free article] [PubMed] [Google Scholar]
- McCormack L. Health Insurance Knowledge among Medicare Beneficiaries. Health Services Research. 2002;37(1):43–63. [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. Medication Costs, Adherence, and Health Outcomes among Medicare Beneficiaries. Health Affairs (Millwood) 2003;22(4):220–9. doi: 10.1377/hlthaff.22.4.220. [DOI] [PubMed] [Google Scholar]
- Piette J D, Heisler M. Problems Due to Medication Costs among VA and Non-VA Patients with Chronic Illnesses. American Journal of Management Care. 2004;10(11 part 2):861–8. [PubMed] [Google Scholar]
- Piette J D, Heisler M, Wagner T H. Problems Paying Out-of-Pocket Medication Costs among Older Adults with Diabetes. Diabetes Care. 2004;27(2):384–91. doi: 10.2337/diacare.27.2.384. [DOI] [PubMed] [Google Scholar]
- Reed M, Fung V, Brand R, Fireman B, Newhouse J P, Selby J V, Hsu J. Care-Seeking Behavior in Response to Emergency Department Copayments. Medcial Care. 2005;43(8):810–6. doi: 10.1097/01.mlr.0000170416.68260.78. [DOI] [PubMed] [Google Scholar]
- Rice T, Matsuoka K Y. The Impact of Cost-Sharing on Appropriate Utilization and Health Status: A Review of the Literature on Seniors. Medical Care Research Review. 2004;61(4):415–52. doi: 10.1177/1077558704269498. [DOI] [PubMed] [Google Scholar]
- Stuart B, Briesacher B A, Shea D G, Cooper B, Baysac F S, Limcangco M R. Riding the Rollercoaster: The Ups and Downs in Out-of-Pocket Spending under the Standard Medicare Drug Benefit. Health Affair (Millwood) 2005;24(4):1022–31. doi: 10.1377/hlthaff.24.4.1022. [DOI] [PubMed] [Google Scholar]
- Stuart B, Zacker C. Who Bears the Burden of Medicaid Drug Copayment Policies? Health Affair (Millwood) 1999;18(2):201–12. doi: 10.1377/hlthaff.18.2.201. [DOI] [PubMed] [Google Scholar]
- Taira D A, Iwane K A, Chung R S. Prescription Drugs: Elderly Enrollee Reports of Financial Access, Receipt of Free Samples, and Discussion of Generic Equivalents Related to Type of Coverage. American Journal of Management Care. 2003;9(4):305–12. [PubMed] [Google Scholar]