Abstract
The cytokines controlling the development of human interleukin (IL) 17–producing T helper cells in vitro have been difficult to identify. We addressed the question of the development of human IL-17–producing T helper cells in vivo by quantifying the production and secretion of IL-17 by fresh T cells ex vivo, and by T cell blasts expanded in vitro from patients with particular genetic traits affecting transforming growth factor (TGF) β, IL-1, IL-6, or IL-23 responses. Activating mutations in TGFB1, TGFBR1, and TGFBR2 (Camurati-Engelmann disease and Marfan-like syndromes) and loss-of-function mutations in IRAK4 and MYD88 (Mendelian predisposition to pyogenic bacterial infections) had no detectable impact. In contrast, dominant-negative mutations in STAT3 (autosomal-dominant hyperimmunoglobulin E syndrome) and, to a lesser extent, null mutations in IL12B and IL12RB1 (Mendelian susceptibility to mycobacterial diseases) impaired the development of IL-17–producing T cells. These data suggest that IL-12Rβ1– and STAT-3–dependent signals play a key role in the differentiation and/or expansion of human IL-17–producing T cell populations in vivo.
IL-17A (IL-17) is the first of a six-member family of cytokines (IL-17A–F). IL-17 is produced by NK and T cell subsets, including helper α/β T cells, γ/δ T cells, and NKT cells, and it binds to a widely expressed receptor (1). This cytokine was first described 10 yr ago, but interest in this molecule was recently revived by the identification of a specific IL-17–producing T helper cell subset in the mouse (1). The specific development and phenotype of IL-17–producing helper T cells have been characterized in the mouse model, in which these cells have clearly been identified as a Th17 subset. The hallmarks of mouse Th17 cells include (a) a pattern of cytokine production different from those of the Th1 and Th2 subsets, with high levels of IL-17 production, often accompanied by IL-17F and IL-22; (b) dependence on TGF-β and IL-6 for early differentiation from naive CD4 T cells, followed by dependence on IL-21 and IL-23 for further expansion; and (c) dependence on at least four transcription factors for differentiation: the Th17-specific retinoic acid receptor–related orphan receptor γt (RORγt) and RORα, and the more promiscuous STAT-3 and IFN regulatory factor 4 (for review see reference 1).
Increasingly detailed descriptions of the in vitro and in vivo differentiation of the Th17 subset in mice are becoming available. In contrast, the tremendous, uncontrolled genetic and epigenetic variability of human samples has made it difficult to characterize human IL-17–producing T cells (2–13). It has proved very difficult to identify the cytokines governing the differentiation of these cells in vitro. The first four groups that have investigated this issue all suggested that TGF-β was not required for the differentiation of human IL-17–producing T helper cells from purified naive CD4 T cells in vitro (5–8). TGF-β was even found to inhibit differentiation in three studies (5, 6, 8). IL-6 was inhibitory in one study (6) and redundant in three others (5, 7, 8). In contrast, IL-23 was found to enhance the development of IL-17 T cells in all four studies (5–8) and IL-1β was identified as a positive regulator in two studies (5, 6), whereas IL-21, which was tested in one study, was found to be redundant (8). In contrast, three recent studies showed that TGF-β is essential in this process, whereas there was more redundancy between the four ILs (11–13). In vitro studies using recombinant cytokines and blocking antibodies have therefore yielded apparently conflicting results, particularly if the results for human cells are compared with those for mice.
We used a novel approach to address this issue, making use of patients with various inborn errors of immunity impairing most of these cytokine signaling pathways separately to investigate the development of IL-17 T cells in vivo. We studied the following groups: (a) patients with autosomal-dominant developmental disorders associated with various mutations in the TGF-β pathway associated with enhanced TGF-β signaling, such as Camurati-Engelmann disease, with mutations in TGFB1 (14), or Marfan-like syndromes, with mutations in TGFBR1 or TGFBR2 (15); (b) patients with autosomal-recessive susceptibility to pyogenic bacteria and loss-of-function mutations in IRAK4 (16) or MYD88 (unpublished data), whose cells do not respond to IL-1β and related cytokines or to Toll-like receptors (TLRs) other than TLR3; (c) patients with autosomal-dominant hyper-IgE syndrome (AD-HIES) associated with dominant-negative mutations in STAT3 (17, 18), whose cells respond poorly to several cytokines, including IL-6; and (d) patients with autosomal-recessive susceptibility to mycobacterial diseases and loss-of-function mutations in IL12B or IL12RB1 (19), whose cells do not express or do not respond to IL-12 and IL-23 (Table S1, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1). The role of IL-21 cannot be studied in this way, as the only known defects in this pathway (i.e., JAK3 and common γ chain deficiencies) are typically associated with a total absence of T cells (20).
RESULTS AND DISCUSSION
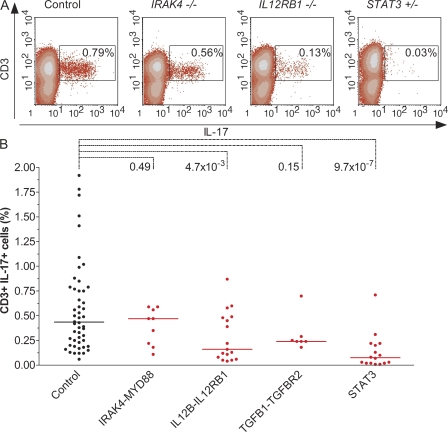
We used flow cytometry to investigate the percentage of IL-17–expressing blood T cells ex vivo in 49 healthy controls. Nonadherent PBMCs were stained for CD3, CD4, CD8, and IL-17. No IL-17–producing T cells were detected in the absence of activation (unpublished data). Upon activation with PMA-ionomycin, the percentage of CD3-positive cells producing IL-17 ranged from 0.06 to 2% (Fig. 1, A and B). The vast majority (>90%) of IL-17–positive cells were CD4-positive and CD8-negative (unpublished data). Thus, within the general population, there is considerable interindividual variability in the numbers of IL-17–producing cells present among freshly isolated T cells activated ex vivo. This makes it difficult to assess the impact of genetic lesions on the development of IL-17–producing T cells. We tested nine patients with null mutations in IRAK4 or MYD88, whose cells were unresponsive to IL-1β (and most TLRs and other IL-1 cytokine family members). The proportion of IL-17–producing T cells was not significantly different from that in healthy controls, as shown by Wilcoxon tests comparing the values for each individual between the two groups (Fig. 1, A and B). We then tested 17 patients with null mutations in IL12B or IL12RB1, whose cells did not produce (for IL12B mutations) or did not respond (for IL12RB1 mutations) to IL-23 (and IL-12). Interestingly, there were clearly fewer IL-17–producing T cells in these patients than in healthy controls (P = 4.7 × 10−3; Fig. 1, A and B). However, some patients had normal numbers of IL-17–producing T cells. In contrast, cells from patients with mildly enhanced TGF-β responses owing to mutations in TGFB1 or TGFBR2 did not differ significantly from controls (Fig. 1 B). These results suggest that IL-1R–associated kinase 4 (IRAK-4) and MyD88 are not required for the development of IL-17–producing T cells in vivo, that TGF-β probably does not markedly inhibit this process, and that both IL-12p40 and IL-12Rβ1 are required, at least in most individuals and in these experimental conditions of flow cytometry on T cells activated ex vivo.
Figure 1.
Identification of IL-17–producing T cells ex vivo. (A) Flow cytometry analysis of CD3 and IL-17 in nonadherent PBMCs activated with PMA-ionomycin as a representative control, an IRAK-4–deficient patient (P4), an IL-12Rβ1–deficient patient (P17), and a STAT-3–deficient patient (P36; Table S1, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1). The percentage indicated in the gate is that of IL-17– and CD3-positive cells. (B) Percentage of CD3-positive cells that were also IL-17–positive, as determined by flow cytometry of nonadherent PBMCs activated with PMA-ionomycin. Each symbol represents a value from an individual control (black circles) or patient (red circles). Horizontal bars represent medians. The p-values for Wilcoxon tests between controls (n = 49) and patients with mutations in IRAK4 or MYD88 (n = 9), IL12B or IL12RB1 (n = 17), TGFB1 or TGFBR2 (n = 7), and STAT3 (n = 16) are indicated.
We tested 16 patients with AD-HIES bearing mutations in STAT3. They displayed normal proportions of CCR6-positive CCR4-positive CD4 T cells but low proportions of CCR6-positive CCR4-negative CD4 T cells (Table S2, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1). These patients had significantly fewer IL-17–positive T cells than controls (P = 9.7 × 10−7; Fig. 1, A and B). However, as observed in patients with IL-12p40 or IL-12Rβ1 deficiency, some AD-HIES patients had normal proportions of IL-17–producing T cells, perhaps reflecting genetic or epigenetic heterogeneity between individuals, residual STAT-3 signaling, or both. In these experimental conditions, the huge variations in IL-17 secretion between healthy controls (from 50 to 5,000 pg/ml), as measured by ELISA, prevented rigorous comparison with the small number of patients studied (unpublished data). We did not assess other potential features of IL-17–producing T cells in the patients studied, such as the production of IL-22, a cytokine produced by Th17 cells in mice (1) and humans (5, 6), or expression of RORγt, a key transcription factor in mouse (1) and human Th17 cells (11), as too few blood samples were available. Our results nonetheless suggest that STAT-3 is required for the differentiation of human IL-17–producing T cells in vivo, as suggested by flow cytometry analysis on ex vivo–activated T cells. We also assessed the production of IFN-γ in some patients (Fig. S1). The proportion of IFN-γ–producing T cells was found to be lower in patients with mutations in IRAK4 and MYD88 (P = 1.2 × 10−4), IL12RB1 and IL12B (P = 1.8 × 10−3), or STAT3 (P = 8 × 10−4), but not in patients with mutations in TGFB1 or TGFBR2 (P = 0.11).
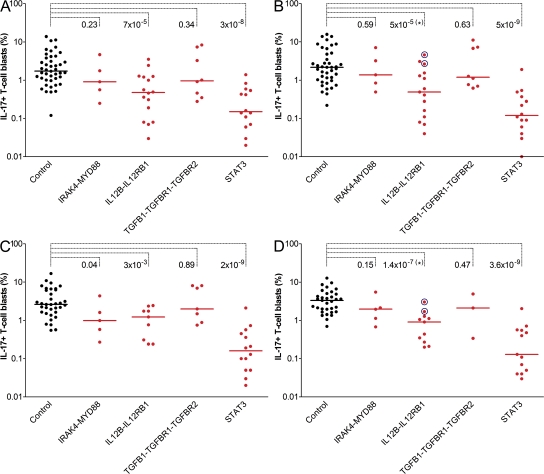
No consensus has yet been reached on how to best induce the differentiation of human IL-17 T cells from naive CD4 precursors in vitro (5–8, 11–13), and only small amounts of blood from a limited number of blood samples from our patients were available. We therefore tried to induce specific IL-17 memory T cell responses using the cytokines shown to be critical for this lineage in the mouse. We evaluated IL-17 production by populations of T cell blasts expanded in vitro from PBMCs. All patients studied, in particular STAT-3–deficient patients, displayed normal proportions of CD4 and CD8 T cells (Table S3, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1). We incubated nonadherent PBMCs from controls with OKT3 for 5 d, alone or in the presence of IL-23, IL-1β, TGF-β, or IL-6, or a combination of these four cytokines, and then activated them with PMA-ionomycin. We did not assess the development of antigen-specific IL-17–producing T cells. There were no IL-17–positive T cells in any control or in any set of experimental conditions in the absence of activation with PMA-ionomycin, as shown by flow cytometry (unpublished data). In the absence of cytokine stimulation, the percentage of IL-17–positive T cells found in healthy controls after stimulation with PMA-ionomycin was highly variable (from 0.12 to 10%; Fig. 2 A). A statistically significant increase in the number of IL-17–producing T cells was observed after stimulation with IL-23 (P = 7 × 10−3) and IL-1β (P = 0.04), but not after stimulation with TGF-β (P = 0.1) or IL-6 (P = 0.3), as shown by paired t tests (Fig. 2 and not depicted). This recall-response pattern is consistent with IL-1β and IL-23 playing an important role in maintaining and expanding IL-17 T cell populations in mice (1) and humans (11–13).
Figure 2.
Identification of IL-17–expressing T cell blasts expanded in vitro. Intracellular production of IL-17 in T cell blasts activated with PMA-ionomycin for controls (black circles) and patients (red circles), as assessed by flow cytometry. The cells were cultured in different stimulation conditions: OKT3 only (A), or OKT3 with IL-23 (B), IL-1β (C), or IL-23, IL-1β, TGF-β, and IL-6 (D). Each symbol represents a value for an individual control or patient. Horizontal bars represent medians. In controls, stimulation with IL-23 and IL-1β had a significant effect with respect to medium alone (P < 0.05). The p-values for Wilcoxon tests between each patient group and the control group are indicated. In B and D, the patients circled in blue carry IL12B mutations and cannot produce IL-12 and IL-23, but can respond to both cytokines. The p-value of the IL12B-IL12RB1 group was therefore calculated only with IL-12Rβ1–deficient patients (*).
We then investigated IL-17 production by T cell blasts from various patients in the same experimental conditions. For four patients with IRAK-4 or MyD88 deficiency and impaired responses to IL-1β, the proportion of IL-17–producing cells appeared to be normal in the various experimental conditions, except in response to IL-1β (Fig. 2). 16 patients with IL-12p40 (n = 2) or IL-12Rβ1 (n = 14) deficiency were found to have much smaller proportions of IL-17–producing T cells in the absence of cytokine stimulation (P = 7 × 10−5; Fig. 2 A). The two IL-12p40–deficient patients, unlike the IL-12Rβ1–deficient patients (P = 5 × 10−5), apparently responded to IL-23 in these conditions (Fig. 2 B). These data suggest that IL-23 makes a major contribution to the expansion of the IL-17 T cell population in this assay. However, patients bearing specific IL-23(R) mutations would be required to rigorously test this hypothesis. We then tested seven patients with mutations associated with mildly enhanced TGF-β responses and found no significant differences from controls in the four conditions tested (Fig. 2).
In contrast, 14 patients with mutations in STAT3 had almost no detectable IL-17–producing T cells in any of the four conditions tested (P = 3.2 × 10−8, 4.9 × 10−9, 1.9 × 10−9, and 3.6 × 10−9, respectively; Fig. 2). This phenotype was clearly more pronounced than that observed with cells from IL-12p40– and IL-12Rβ1–deficient patients, as the almost complete lack of IL-17–positive T cells was not complemented by IL-23, IL-1β, or a combination of the four cytokines. T cells from the 11 patients with STAT3 mutations studied proliferated normally in these conditions. Our results demonstrate that STAT-3 is required for the expansion of IL-17–producing T cell blasts, at least in these experimental conditions. In these conditions, all the groups of patients studied had fewer IFN-γ–producing cells than controls (Fig. S2, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1).
Finally, we assessed the secretion of IL-17, IL-22, and IFN-γ by T cell blasts from controls and patients, with or without activation with PMA-ionomycin, as measured by ELISA (Fig. 3; and Figs. S3 and S4, available at http://www.jem.org/cgi/content/full/jem.20080321/DC1). Control T cell blasts cultured without recombinant cytokine produced detectable amounts of IL-17 in the absence of activation by PMA-ionomycin (mean = 137 ± 149 pg/ml; Fig. 3 A). The amounts of IL-17 secreted increased significantly (P = 3 × 10−4) upon activation with PMA-ionomycin (mean = 7,338 ± 11,134 pg/ml). However, considerable interindividual variability was observed in both sets of experimental conditions. The addition of IL-23, IL-1β, or a combination of IL-23, IL-1β, TGF-β, and IL-6 significantly increased the amounts of secreted IL-17 in the absence of activation with PMA-ionomycin (P = 10−4 and 8 × 10−4, and P < 10−4, respectively; Fig. 3, B–D). Upon PMA-ionomycin activation, only IL-1β significantly increased the amount of IL-17 secretion (P = 0.04). Four patients with IRAK-4 or MyD88 deficiency were tested. They displayed low levels of IL-17 secretion in the absence of activation with PMA-ionomycin in the four sets of conditions tested (P = 4 × 10−3, 10−5, 10−4, and 8 × 10−4, respectively; Fig. 3). Upon PMA-ionomycin activation, the level of IL-17 secretion is not significantly different from the controls, except in the presence of IL-1β (P = 0.04; Fig. 3). These results suggest that the Toll/IL-1R signaling pathway, and possibly the IL-1R pathway, may be involved in the secretion of IL-17 in T cell blasts. These patients produced amounts of IL-22 that were similar to the controls (Fig. S3).
Figure 3.
IL-17 secretion by T cell blasts expanded in vitro. Secretion of IL-17 by T cell blasts from controls (black circles) and patients (red circles), as measured by ELISA. Open circles represent values in the absence of stimulation, and closed circles correspond to values obtained after stimulation with PMA-ionomycin. Different stimulation conditions are shown: OKT3 only (A), or OKT3 with IL-23 (B), IL-1β (C), or IL-23, IL-1β, TGF-β, and IL-6 (D). Each symbol corresponds to a value obtained from an individual. Horizontal bars represent medians. The p-values for Wilcoxon tests between each patient group and the control group, either unstimulated or stimulated with PMA-ionomycin, are indicated. In B and D, patients circled in blue carry IL12B mutations and cannot produce IL-12 and IL-23, but can respond to both cytokines. The p-values of the IL12B-IL12RB1 group were therefore calculated only with IL-12Rβ1–deficient patients (*).
T cell blasts from the 13 IL-12p40– or IL-12Rβ1–deficient patients tested secreted normal amounts of IL-17 in the absence of cytokine stimulation (Fig. 3 A). The 10 patients tested produced normal amounts of IL-17 in the presence of IL-1β (Fig. 3 C). In the presence of the four cytokines, patients with IL-12Rβ1 deficiency did not secrete normal amounts of IL-17 without (P = 2 × 10−3) or with (P = 10−3) PMA-ionomycin stimulation (Fig. 3 D). In all culture conditions, cells from patients with IL12B and IL12RB1 mutations secreted less IL-22 than control cells (Fig. S3). T cell blasts from all patients with mutations in the TGF-β pathway secreted normal amounts of IL-17, whereas T cell blasts from all patients with STAT-3 deficiency secreted much smaller amounts of IL-17 (P = 8 × 10−6, 9 × 10−7, 9 × 10−11, 2 × 10−7, 10−8, 3 × 10−7, 4 × 10−9, and 3 × 10−6, respectively) and IL-22 in all experimental conditions (Fig. 3 and Fig. S3). These data indicate that STAT-3 is required for the maintenance and expansion of IL-17–secreting human T cell blasts and for the secretion of IL-22 by human T cell blasts, at least in these experimental conditions.
Patients with STAT-3 deficiency had the most severe IL-17 phenotype of all the patients tested, with a profound impairment of IL-17 production by T cells ex vivo and T cell blasts in vitro. This observation is consistent with findings for STAT-3–deficient mice (1, 21–24) and a recent report in humans (25). Impaired IL-6 signaling may be the key factor involved, as suggested by the results obtained for IL-6–deficient mice (1, 26, 27). However, STAT-3 is also involved in other relevant pathways, including the IL-21 and IL-23 pathways. Our data for IL-12p40– and IL-12Rβ1–deficient cells suggest that IL-23 is required for the optimal development of IL-17–producing T cells. IL-23 is probably the only cytokine involved, as the patients also lacked IL-12 responses, which might be expected to enhance the development of this subset (1). This is consistent with the mouse model, in which IL-23 is required for the maintenance and expansion of these cells (1, 28, 29), and with the results of previous human studies based on the use of recombinant cytokines (5–8, 11–13). In contrast, our findings for IRAK-4– and MyD88-deficient cells do not support the notion that IL-1β (or any of the IL-1Rs and TLRs other than, possibly, TLR3 and TLR4) is essential for the development of human IL-17–producing T cells (5, 6), consistent with the phenotype of IL-1–deficient mice (1). Finally, the paradoxical suggestion that TGF-β may have no effect or may even inhibit the development of human IL-17–producing T cells (5–8) was neither supported nor disproved by our data for patients with mildly enhanced TGF-β responses (1).
Does our report provide any clues to the possible function of IL-17 in host defense? The mouse Th17 subset plays a key role in mucosal defense (30). IL-23– and IL-17–deficient mice are vulnerable to Klebsiella (31, 32). This may account for the greater susceptibility of IL-12p40– and IL-12Rβ1–deficient patients than of IFN-γR–deficient patients to both Klebsiella (Levin, M., and S. Pedraza, personal communication; Table S1) and the related Salmonella (19). However, neither Klebsiella nor Salmonella is commonly found as a pathogen in STAT-3–deficient patients despite the apparently greater defect of these patients in terms of IL-17–producing T cell development (17, 18). Mice with impaired IL-17 immunity are also susceptible to Candida (33–35). This may account for the peripheral candidiasis commonly seen in STAT-3–deficient patients. Interestingly, although most IL-12p40– and IL-12Rβ1–deficient patients are not susceptible to Candida (19), some present with peripheral candidiasis (unpublished data). Mycobacterial disease is exceedingly rare in STAT-3–deficient patients, but not in IL-12p40– and IL-12Rβ1–deficient patients, in whom it results from impaired IFN-γ immunity, which is consistent with the redundancy of IL-17 in mouse primary immunity to mycobacteria (36, 37). Staphylococcal disease is the main infection seen in STAT-3–deficient patients. Mouse IL-17 seems to be involved in immunity to Staphylococcus (38). However, both IL-12p40– and IL-12Rβ1–deficient patients are normally resistant to Staphylococcus. The function of human IL-17 and related cytokines in host defense therefore remains unknown. The genetic dissection of human infectious diseases should help us to attribute a function to this important cytokine in natura (39, 40).
MATERIALS AND METHODS
Patients and controls.
55 healthy, unrelated individuals of various ages from 12 countries (Argentina, Canada, Cuba, France, Germany, Israel, Portugal, Spain, Switzerland, Turkey, UK, and USA) were tested as controls. We also investigated 50 patients with mutations in IRAK4, MYD88, IL12B, IL12RB1, TGFB1, TGFBR1, TGFBR2, or STAT3 (Table S1). Our study was conducted in accordance with the Helsinki Declaration, with informed consent obtained from each patient or the patient's family, as requested and approved by the institutional review board of the Necker Medical School.
Purification and activation of nonadherent PBMCs.
PBMCs were purified by centrifugation on a gradient (Ficoll-Paque PLUS; GE Healthcare) and resuspended in 10% FBS in RPMI (RPMI-10% FBS; Invitrogen). Adherent monocytes were removed by plating PBMCs in a 75-cm2 horizontal culture flask and incubating them for 2–3 h at 37°C in an atmosphere containing 5% CO2. The nonadherent cells were washed in RPMI and counted with a counter (Vi-Cell XR; Beckman Coulter). For flow cytometry, we distributed 5 × 106 cells in 5 ml RPMI-10% FBS in two 25-cm2 vertical culture flasks. One flask was stimulated with 40 ng/ml PMA (Sigma-Aldrich) and 10−5 M ionomycin (Sigma-Aldrich). All cells were treated with 1 μl/ml Golgiplug (BD Biosciences), a secretion inhibitor. The flasks were incubated for 12 h at 37°C under an atmosphere containing 5% CO2. For ELISA, a 200-μl aliquot of cells at a concentration of 2.5 × 106 cells/ml in RPMI-10% FBS was dispensed into each well of a 96-well plate. The cells were or were not activated with 40 ng/ml PMA and 10−5 M ionomycin. Supernatants were collected after 48 h of incubation at 37°C under an atmosphere containing 5% CO2.
Expansion and activation of T cell blasts.
Nonadherent PBMCs were dispensed into 24-well plates at a density of 2.5 × 106 cells/ml in RPMI-10% FBS. All cells were activated with 2 μg/ml of an antibody against CD3 (Orthoclone OKT3; Janssen-Cilag) alone, or together with 5 ng/ml TGF-β1 (240-B; R&D Systems), 20 ng/ml IL-23 (1290-IL; R&D Systems), 25 ng/ml IL-6 (206-IL; R&D Systems), 10 ng/ml IL-1β (201-LB; R&D Systems), or combinations of these four cytokines. Plates were incubated at 37°C under an atmosphere containing 5% CO2 for 3 d. The cells in each well were restimulated using the same activation conditions, except that the antibody against CD3 was replaced by 40 IU/ml IL-2 (Proleukin i.v.; Chiron). 1 ml of each appropriate medium was added, and we gently passed the culture up and down through a pipette to break up clumps. The culture in each well was split in two. Flow cytometry was performed on one of the duplicate wells 2 d later. The cells in this well were stimulated by incubation for 12 h with 40 ng/ml PMA and 10−5 M ionomycin plus 1 μl/ml Golgiplug at 37°C under an atmosphere containing 5% CO2. FACS analysis was performed as described in the following section, without extracellular labeling. For ELISA analysis, cultures were allowed to differentiate under various conditions for 6 d and were then diluted 1:2 in RPMI-10% FBS supplemented with 40 IU/ml IL-2. 200 μl of cells in a 96-well plate were activated with 40 ng/ml PMA and 10−5 M ionomycin, or left unactivated. Supernatants were collected after 48 h of incubation at 37°C under an atmosphere containing 5% CO2.
Flow cytometry.
Cells were washed in cold PBS and dispensed into a 96-well plate for labeling. Extracellular labeling (for the ex vivo study only) was achieved by incubating the cells with 3 μl CD3-PECy5 in 50 μl PBS-2% FBS (BD Biosciences) for 20 min on ice. The cells were washed twice with cold PBS-2% FBS. They were fixed by incubation with 100 μl BD Cytofix (BD Biosciences) for 30 min on ice and washed twice with BD Cytoperm (BD Biosciences), with a 10-min incubation period in BD Cytoperm on ice for the first wash. Cells were then incubated for 1 h on ice with IL-17–Alexa Fluor 488 (eBioscience) or IFN-γ–PE (BD Biosciences) at a dilution of 3 μl of antibody in 50 μl BD Cytoperm. Cells were washed twice with BD Cytoperm and analyzed with a FACScan machine and CellQuest software (both from Becton Dickinson).
Determination of cytokine levels by ELISA.
IL-17, IL-22, and IFN-γ levels were determined by ELISA. We used the capture antibodies, detection antibodies, and standards supplied in the kits for IL-17 and IL-22 (Duoset; R&D Systems) and in the kit for IFN-γ (Sanquin), diluted in HPE dilution buffer (Sanquin). Milk was used for blocking, and antibody binding was detected with streptavidin poly–horseradish peroxidase (Sanquin) and TMB microwell peroxidase substrate (KPL). The reaction was stopped by adding 1.8 M H2SO4. Optical density was determined with a microplate reader (MRX; Thermolab Systems).
Statistical analysis.
We first assessed differences between controls and patients (when there were more than two patients) for (a) the percentage of circulating IL-17–producing T cells, (b) the percentage of IL-17–positive T cells in vitro, and (c) the level of IL-17 production in various stimulation conditions, as assessed by ELISA. As the distribution of these three variables could not be assumed to be normal and some of the patient groups examined were very small, we used the nonparametric Wilcoxon exact test, as implemented in the NPAR1WAY module of SAS software (version 9.1; SAS Institute). A second set of tests was performed on controls only to assess the effects of different stimulation conditions on (a) the percentage of IL-17–positive T cells in vitro and (b) the level of IL-17 production, as assessed by ELISA. We used a strategy of matching, with paired t tests performed with the TTEST procedure of SAS software (version 9.1) to investigate the correlation between observations for different controls. For all analyses, P < 0.05 was considered statistically significant.
Online supplemental material.
Fig. S1 shows the percentage of CD3-positive IFN-γ–positive cells, as determined by flow cytometry of nonadherent PBMCs activated with PMA-ionomycin from controls and patients. Fig. S2 shows intracellular IFN-γ production in T cell blasts activated with PMA-ionomycin from controls and patients in the various culture conditions, as assessed by flow cytometry. Fig. S3 shows the secretion of IL-22 by T cell blasts from controls and patients in the various culture conditions, as measured by ELISA. Fig. S4 shows the secretion of IFN-γ by T cell blasts from controls and patients in the various culture conditions, as measured by ELISA. Table S1 shows the genetic and clinical features of the patients studied. Table S2 shows the proportions of CCR6-positive CD4 T cells in controls and STAT-3–deficient patients. Table S3 shows the proportions of CD4 and CD8 T cells in patients. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20080321/DC1.
Supplementary Material
Acknowledgments
We would particularly like to thank the patients and their families, whose trust, support, and cooperation were essential for the collection of the data used in this study. We thank N. Matamoros, F.M. Ruemmele, and F. Rieux-Laucat for their help with this study, and all members of the laboratory for helpful discussions. We thank M. Courat, C. Bidalled, M. N'Guyen, T. Leclerc, S. Fahy, and G. Brami for secretarial and technical assistance.
The Laboratory of Human Genetics of Infectious Diseases is supported by the Agence Nationale de la Recherche, the Programme Hospitalier de Recherche Clinique, the European Union (grant LHSP-CT-2005-018736), the BNP Paribas Foundation, the March of Dimes, the Dana Foundation, and the Candi'Oser Association. L. de Beaucoudrey is supported by the Fondation pour la Recherche Medicale as part of the PhD program of Pierre et Marie Curie University. J.L. Casanova is an International Scholar of the Howard Hughes Medical Institute.
The authors have no conflicting financial interests.
References
- 1.Dong, C. 2008. TH17 cells in development: an updated view of their molecular identity and genetic programming. Nat. Rev. Immunol. 8:337–348. [DOI] [PubMed] [Google Scholar]
- 2.Acosta-Rodriguez, E.V., L. Rivino, J. Geginat, D. Jarrossay, M. Gattorno, A. Lanzavecchia, F. Sallusto, and G. Napolitani. 2007. Surface phenotype and antigenic specificity of human interleukin 17-producing T helper memory cells. Nat. Immunol. 8:639–646. [DOI] [PubMed] [Google Scholar]
- 3.Sato, W., T. Aranami, and T. Yamamura. 2007. Cutting edge: Human Th17 cells are identified as bearing CCR2+CCR5− phenotype. J. Immunol. 178:7525–7529. [DOI] [PubMed] [Google Scholar]
- 4.Annunziato, F., L. Cosmi, V. Santarlasci, L. Maggi, F. Liotta, B. Mazzinghi, E. Parente, L. Fili, S. Ferri, F. Frosali, et al. 2007. Phenotypic and functional features of human Th17 cells. J. Exp. Med. 204:1849–1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acosta-Rodriguez, E.V., G. Napolitani, A. Lanzavecchia, and F. Sallusto. 2007. Interleukins 1beta and 6 but not transforming growth factor-beta are essential for the differentiation of interleukin 17-producing human T helper cells. Nat. Immunol. 8:942–949. [DOI] [PubMed] [Google Scholar]
- 6.Wilson, N.J., K. Boniface, J.R. Chan, B.S. McKenzie, W.M. Blumenschein, J.D. Mattson, B. Basham, K. Smith, T. Chen, F. Morel, et al. 2007. Development, cytokine profile and function of human interleukin 17-producing helper T cells. Nat. Immunol. 8:950–957. [DOI] [PubMed] [Google Scholar]
- 7.Chen, Z., C.M. Tato, L. Muul, A. Laurence, and J.J. O'Shea. 2007. Distinct regulation of interleukin-17 in human T helper lymphocytes. Arthritis Rheum. 56:2936–2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans, H.G., T. Suddason, I. Jackson, L.S. Taams, and G.M. Lord. 2007. Optimal induction of T helper 17 cells in humans requires T cell receptor ligation in the context of Toll-like receptor-activated monocytes. Proc. Natl. Acad. Sci. USA. 104:17034–17039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim, H.W., J. Lee, P. Hillsamer, and C.H. Kim. 2008. Human Th17 cells share major trafficking receptors with both polarized effector T cells and FOXP3+ regulatory T cells. J. Immunol. 180:122–129. [DOI] [PubMed] [Google Scholar]
- 10.Singh, S.P., H.H. Zhang, J.F. Foley, M.N. Hedrick, and J.M. Farber. 2008. Human T cells that are able to produce IL-17 express the chemokine receptor CCR6. J. Immunol. 180:214–221. [DOI] [PubMed] [Google Scholar]
- 11.Manel, N., D. Unutmaz, and D.R. Littman. 2008. The differentiation of human T(H)-17 cells requires transforming growth factor-beta and induction of the nuclear receptor RORgammat. Nat. Immunol. 9:641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volpe, E., N. Servant, R. Zollinger, S.I. Bogiatzi, P. Hupe, E. Barillot, and V. Soumelis. 2008. A critical function for transforming growth factor-beta, interleukin 23 and proinflammatory cytokines in driving and modulating human T(H)-17 responses. Nat. Immunol. 9:650–657. [DOI] [PubMed] [Google Scholar]
- 13.Yang, L., D.E. Anderson, C. Baecher-Allan, W.D. Hastings, E. Bettelli, M. Oukka, V.K. Kuchroo, and D.A. Hafler. 2008. IL-21 and TGF-beta are required for differentiation of human T(H)17 cells. Nature. DOI: 10.1038/nature07021. [DOI] [PMC free article] [PubMed]
- 14.Janssens, K., F. Vanhoenacker, M. Bonduelle, L. Verbruggen, L. Van Maldergem, S. Ralston, N. Guanabens, N. Migone, S. Wientroub, M.T. Divizia, et al. 2006. Camurati-Engelmann disease: review of the clinical, radiological, and molecular data of 24 families and implications for diagnosis and treatment. J. Med. Genet. 43:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramirez, F., and H.C. Dietz. 2007. Marfan syndrome: from molecular pathogenesis to clinical treatment. Curr. Opin. Genet. Dev. 17:252–258. [DOI] [PubMed] [Google Scholar]
- 16.Ku, C.L., H. von Bernuth, C. Picard, S.Y. Zhang, H.H. Chang, K. Yang, M. Chrabieh, A.C. Issekutz, C.K. Cunningham, J. Gallin, et al. 2007. Selective predisposition to bacterial infections in IRAK-4–deficient children: IRAK-4–dependent TLRs are otherwise redundant in protective immunity. J. Exp. Med. 204:2407–2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Minegishi, Y., M. Saito, S. Tsuchiya, I. Tsuge, H. Takada, T. Hara, N. Kawamura, T. Ariga, S. Pasic, O. Stojkovic, et al. 2007. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 448:1058–1062. [DOI] [PubMed] [Google Scholar]
- 18.Holland, S.M., F.R. Deleo, H.Z. Elloumi, A.P. Hsu, G. Uzel, N. Brodsky, A.F. Freeman, A. Demidowich, J. Davis, M.L. Turner, et al. 2007. STAT3 mutations in the hyper-IgE syndrome. N. Engl. J. Med. 357:1608–1619. [DOI] [PubMed] [Google Scholar]
- 19.Filipe-Santos, O., J. Bustamante, A. Chapgier, G. Vogt, L. de Beaucoudrey, J. Feinberg, E. Jouanguy, S. Boisson-Dupuis, C. Fieschi, C. Picard, and J.L. Casanova. 2006. Inborn errors of IL-12/23- and IFN-gamma-mediated immunity: molecular, cellular, and clinical features. Semin. Immunol. 18:347–361. [DOI] [PubMed] [Google Scholar]
- 20.Buckley, R.H. 2004. Molecular defects in human severe combined immunodeficiency and approaches to immune reconstitution. Annu. Rev. Immunol. 22:625–655. [DOI] [PubMed] [Google Scholar]
- 21.Harris, T.J., J.F. Grosso, H.R. Yen, H. Xin, M. Kortylewski, E. Albesiano, E.L. Hipkiss, D. Getnet, M.V. Goldberg, C.H. Maris, et al. 2007. Cutting edge: An in vivo requirement for STAT3 signaling in TH17 development and TH17-dependent autoimmunity. J. Immunol. 179:4313–4317. [DOI] [PubMed] [Google Scholar]
- 22.Wei, L., A. Laurence, K.M. Elias, and J.J. O'Shea. 2007. IL-21 is produced by Th17 cells and drives IL-17 production in a STAT3-dependent manner. J. Biol. Chem. 282:34605–34610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang, X.O., A.D. Panopoulos, R. Nurieva, S.H. Chang, D. Wang, S.S. Watowich, and C. Dong. 2007. STAT3 regulates cytokine-mediated generation of inflammatory helper T cells. J. Biol. Chem. 282:9358–9363. [DOI] [PubMed] [Google Scholar]
- 24.Mathur, A.N., H.C. Chang, D.G. Zisoulis, G.L. Stritesky, Q. Yu, J.T. O'Malley, R. Kapur, D.E. Levy, G.S. Kansas, and M.H. Kaplan. 2007. Stat3 and Stat4 direct development of IL-17-secreting Th cells. J. Immunol. 178:4901–4907. [DOI] [PubMed] [Google Scholar]
- 25.Milner, J.D., J.M. Brenchley, A. Laurence, A.F. Freeman, B.J. Hill, K.M. Elias, Y. Kanno, C. Spalding, H.Z. Elloumi, M.L. Paulson, et al. 2008. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 452:773–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimura, A., T. Naka, and T. Kishimoto. 2007. IL-6-dependent and -independent pathways in the development of interleukin 17-producing T helper cells. Proc. Natl. Acad. Sci. USA. 104:12099–12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen, X., O.M. Howard, and J.J. Oppenheim. 2007. Pertussis toxin by inducing IL-6 promotes the generation of IL-17-producing CD4 cells. J. Immunol. 178:6123–6129. [DOI] [PubMed] [Google Scholar]
- 28.Langrish, C.L., Y. Chen, W.M. Blumenschein, J. Mattson, B. Basham, J.D. Sedgwick, T. McClanahan, R.A. Kastelein, and D.J. Cua. 2005. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201:233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thakker, P., M.W. Leach, W. Kuang, S.E. Benoit, J.P. Leonard, and S. Marusic. 2007. IL-23 is critical in the induction but not in the effector phase of experimental autoimmune encephalomyelitis. J. Immunol. 178:2589–2598. [DOI] [PubMed] [Google Scholar]
- 30.Matsuzaki, G., and M. Umemura. 2007. Interleukin-17 as an effector molecule of innate and acquired immunity against infections. Microbiol. Immunol. 51:1139–1147. [DOI] [PubMed] [Google Scholar]
- 31.Happel, K.I., P.J. Dubin, M. Zheng, N. Ghilardi, C. Lockhart, L.J. Quinton, A.R. Odden, J.E. Shellito, G.J. Bagby, S. Nelson, and J.K. Kolls. 2005. Divergent roles of IL-23 and IL-12 in host defense against Klebsiella pneumoniae. J. Exp. Med. 202:761–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ye, P., F.H. Rodriguez, S. Kanaly, K.L. Stocking, J. Schurr, P. Schwarzenberger, P. Oliver, W. Huang, P. Zhang, J. Zhang, et al. 2001. Requirement of interleukin 17 receptor signaling for lung CXC chemokine and granulocyte colony-stimulating factor expression, neutrophil recruitment, and host defense. J. Exp. Med. 194:519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang, W., L. Na, P.L. Fidel, and P. Schwarzenberger. 2004. Requirement of interleukin-17A for systemic anti-Candida albicans host defense in mice. J. Infect. Dis. 190:624–631. [DOI] [PubMed] [Google Scholar]
- 34.LeibundGut-Landmann, S., O. Gross, M.J. Robinson, F. Osorio, E.C. Slack, S.V. Tsoni, E. Schweighoffer, V. Tybulewicz, G.D. Brown, J. Ruland, and C. Reis e Sousa. 2007. Syk- and CARD9-dependent coupling of innate immunity to the induction of T helper cells that produce interleukin 17. Nat. Immunol. 8:630–638. [DOI] [PubMed] [Google Scholar]
- 35.Ouyang, W., J.K. Kolls, and Y. Zheng. 2008. The biological functions of T helper 17 cell effector cytokines in inflammation. Immunity. 28:454–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Umemura, M., A. Yahagi, S. Hamada, M.D. Begum, H. Watanabe, K. Kawakami, T. Suda, K. Sudo, S. Nakae, Y. Iwakura, and G. Matsuzaki. 2007. IL-17-mediated regulation of innate and acquired immune response against pulmonary Mycobacterium bovis bacille Calmette-Guerin infection. J. Immunol. 178:3786–3796. [DOI] [PubMed] [Google Scholar]
- 37.Khader, S.A., G.K. Bell, J.E. Pearl, J.J. Fountain, J. Rangel-Moreno, G.E. Cilley, F. Shen, S.M. Eaton, S.L. Gaffen, S.L. Swain, et al. 2007. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nat. Immunol. 8:369–377. [DOI] [PubMed] [Google Scholar]
- 38.Schwarzenberger, P., and J.K. Kolls. 2002. Interleukin 17: an example for gene therapy as a tool to study cytokine mediated regulation of hematopoiesis. J. Cell. Biochem. Suppl. 38:88–95. [DOI] [PubMed] [Google Scholar]
- 39.Casanova, J.L., and L. Abel. 2007. Primary immunodeficiencies: a field in its infancy. Science. 317:617–619. [DOI] [PubMed] [Google Scholar]
- 40.Quintana-Murci, L., A. Alcais, L. Abel, and J.L. Casanova. 2007. Immunology in natura: clinical, epidemiological and evolutionary genetics of infectious diseases. Nat. Immunol. 8:1165–1171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.