Abstract
In this randomized controlled trial, the authors evaluated brief motivational interventions (BMIs) for at-risk college drinkers. Heavy drinking students (N = 509; 65% women, 35% men) were randomized into 1 of 6 intervention conditions formed by crossing baseline timeline followback (TLFB) interview (present versus absent) and intervention type (basic BMI, BMI enhanced with a decisional balance module, or none). Assessments completed at baseline, 1, 6, and 12 months measured typical and risky drinking as well as drinking-related problems. Relative to controls, the TLFB interview reduced consumption but not problems at 1 month. The basic BMI improved all drinking outcomes beyond the effects of the TLFB at 1 month, whereas the enhanced BMI did not. Risk reduction achieved by brief interventions maintained throughout the follow-up year.
Keywords: brief intervention, college drinking, alcohol abuse prevention, decisional balance, timeline assessment
Many college students engage in dangerous patterns of alcohol use. Although most have not yet achieved the legal drinking age, about 70% of college students report drinking alcohol in the last month (O’Malley & Johnston, 2002). Their drinking patterns are often characterized by episodic but heavy drinking; as many as 44% of college students report recent heavy drinking (5 or more drinks an occasion for men, 4 or more drinks for women), and 42% of women and 55% of men report that “getting drunk” is an important reason for drinking (Wechsler et al., 2002).
Heavy drinking among college students can result in an array of negative consequences. College drinkers frequently reported doing something they regretted (35%), missing a class (30%), driving after drinking (29%), and forgetting where they were or what they did (27%) after drinking (Wechsler et al., 2002). Some also report more severe consequences, such as getting hurt or injured (13%), damaging property (11%), or engaging in unprotected sex because of alcohol use (10%). Tragically, 1,400 college students die each year from injuries related to alcohol use (Hingson, Heeren, Zakocs, Kopstein, & Wechsler, 2002). Other students are also affected by having their sleep or studies disrupted, being insulted or humiliated, and receiving unwanted sexual advances from intoxicated students (Wechsler et al., 2002). Consequences of excessive drinking interfere with the academic and social missions of colleges and universities.
Numerous interventions have been developed to reduce heavy college drinking (Larimer & Cronce, 2002). Purely educational programs often increase students’ knowledge about the effects of alcohol but tend not to affect drinking attitudes and behaviors (e.g., Robinson, Roth, Gloria, Keim, & Sattler, 1993). These findings suggest that risky drinking is not associated with a lack of knowledge. Alternative models of drinking behavior suggest that motivational factors may be more important for behavior change, and brief motivational interventions (BMIs) have emerged as a method of reducing alcohol use in college students (Larimer & Cronce, 2002).
BMIs often involve two components: (a) an assessment of the quantity, frequency, and consequences of drinking, and (b) tailored motivational strategies, most commonly the use of personalized feedback and normative comparisons (Dimeff, Baer, Kivlahan, & Marlatt, 1999). It is hypothesized that both the assessment of drinking patterns and the use of one (or more) tailored motivational strategies lead to behavior change. However, because effects resulting from feedback-based interventions have ranged from small to medium (Walters & Neighbors, 2005), efforts to enhance the impact of BMIs have explored supplementing the “basic” BMI components with more detailed assessments and/or additional motivational strategies.
The notion that a thorough assessment can, by itself, produce changes in alcohol use has been confirmed in both clinical (Clifford & Maisto, 2000) and prevention (Murphy et al., 2001) contexts. Such change has been interpreted as the result of increased awareness of the self-defeating consequences of risk behavior. Indeed, evidence suggests that one assessment method, the Timeline Followback (TLFB) Interview (Sobell & Sobell, 1996), may be particularly effective at raising awareness of the consequences of engaging in risk behaviors. In one study, participation in a sexual behavior TLFB interview raised sexual risk reduction motivation more than did completion of standard survey questions (Weinhardt, 2002). In a second study, greater risk sensitization occurred for participants reporting riskier sexual practices (e.g., having multiple partners, engaging in vaginal versus oral sex; Weinhardt, Carey, & Carey, 2000). These findings suggest that the TLFB approach to assessment may serve as an active intervention. It is also possible that using a TLFB assessment as part of a BMI might enhance the BMI’s efficacy.
The second critical component of BMIs involves the use of one or more motivational enhancement strategies. The use of personalized feedback and normative comparisons is common to the “basic” BMI, but these components are sometimes supplemented with decisional balance exercises (Monti et al., 1999; Murphy et al., 2001). Decisional balance emerges from the notion of motivation as a balance between opposing forces (Janis & Mann, 1977). According to theory, costs of a problem behavior must outweigh benefits, and pros of a new behavior must outweigh cons before a person is motivated to change. Providing a structured method of organizing the information elicited during the BMI, the DB exercise may increase the salience of the costs of continuing to drink heavily and the benefits of reducing heavy drinking.
Whether more detailed assessment (i.e., a TLFB) and additional motivational strategies (i.e., a DB exercise) add value to a “basic” BMI has not been evaluated. We chose to investigate the incremental value of these BMI components for both theoretical and practical reasons. Theoretically, (a) increasing awareness of personal vulnerability through a more detailed assessment, and/or (b) increasing discrepancy between current behavior and an internal standard thorough a structured discussion of the pros and cons of change may, separately or jointly, enhance motivation to reduce risky drinking (Miller & Rollnick, 2002). Thus, use of a TLFB assessment and a DB exercise may enhance the motivation-enhancing impact of the “basic” BMI content. Practically, because of the exigencies of clinical practice, knowing whether these components improve outcomes can guide interventionists who need to know the most efficient way to provide prevention services with limited resources. For these reasons, we sought to determine whether the TLFB and DB components provide useful additions or whether a more streamlined (and perhaps more cost-effective) basic BMI is sufficient.
This study had three a priori goals. First, we evaluated the sensitizing effect of a baseline TLFB assessment with heavy drinking students. We predicted that students who received a TLFB would reduce risky drinking more than those who did not receive a TLFB. Second, we evaluated the efficacy of two forms of BMI relative to no BMI. We expected that students who received either the BMI (basic) and a BMI enhanced with a DB module (enhanced) would reduce their alcohol use and consequences more than students in conditions without a BMI. Third, we also predicted that the enhanced BMI would reduce drinking and problems more than the basic BMI. In addition, with exploratory analyses, we evaluated whether the TLFB and BMI interacted to produce the greatest reductions in drinking.
Method
Design
In this randomized clinical trial (RCT), eligible students were assigned randomly within gender to one of six conditions. The design included two between-subjects factors, baseline TLFB interview (administered or not) and intervention condition (none, basic BMI, or enhanced BMI), and one within-subjects factor, time of assessment (baseline, 1, 6, and 12 months). Primary outcome variables were consistent with those reported in the college drinking literature: (a) typical drinking (average drinks per week, drinks per drinking day), (b) risky drinking (heavy drinking frequency, peak blood alcohol concentration [BAC]) and (c) drinking-related problems.
Participants
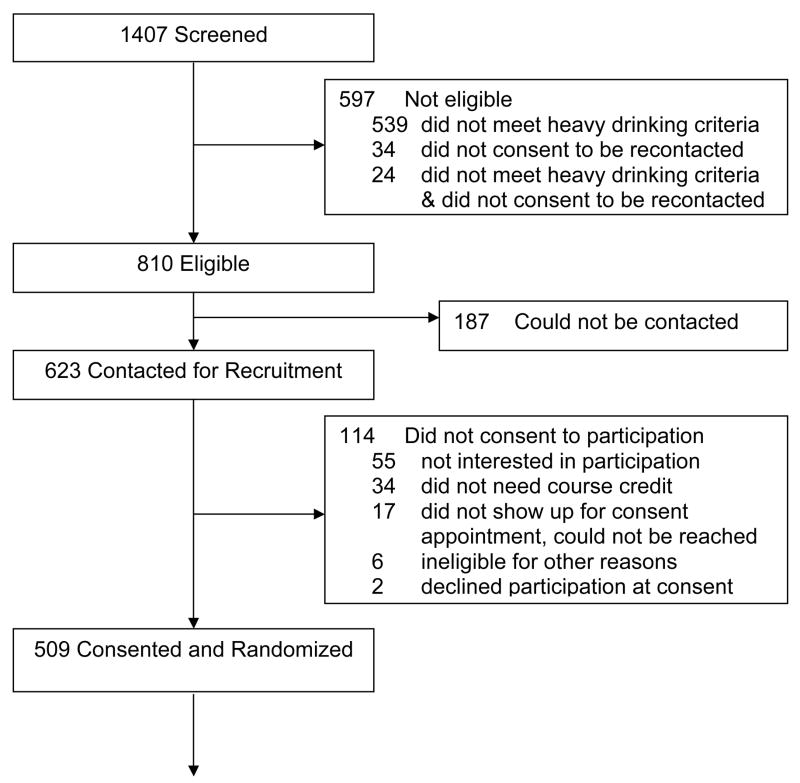
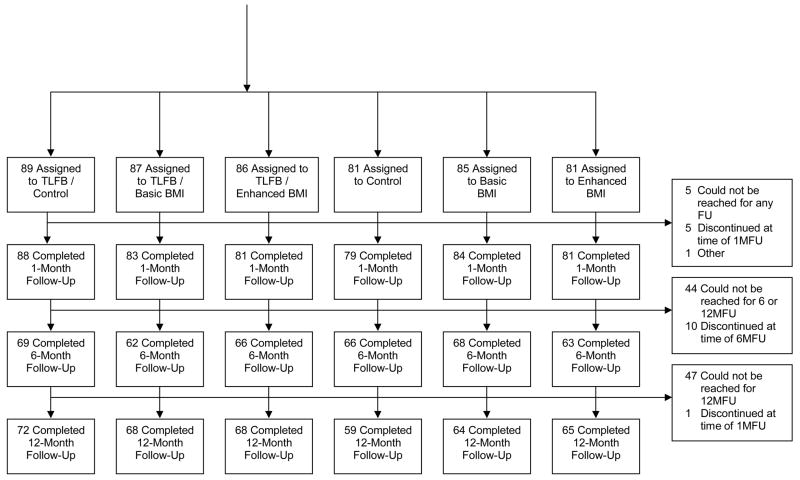
Student volunteers (N = 1407; 65% women) at a northeastern university were screened during five semesters: Fall, 2001—Fall, 2003. Most were freshmen (57%) or sophomores (31%) and living in campus housing (82%); only 17% were members of fraternities or sororities. The majority identified themselves as White (81%), whereas 6% identified themselves as Black, 8% as Asian, and 5% as other. Compared to the larger student body, this sample consisted of more underclassmen (88% vs. 64%) and more women (65% vs. 57%) but an equivalent proportion of minorities (19% vs. 21%). Students were eligible if they reported (a) ≥ 1 episode of heavy drinking in an average week, or four heavy drinking episodes in the last month, using gender-specific criteria (4/5 or more standard drinks for women/men); (b) age between 18 and 25; (c) freshman, sophomore, or junior status (to facilitate follow-ups); and (d) willingness to be recontacted. Of the 1407 students screened, 597 were ineligible (see Figure 1). Of the 810 eligible students, 187 could not be contacted, and 114 did not want to participate. Therefore, 509 eligible and consenting students were randomized.
Figure 1.
Participation Flow Diagram. TLFB = Timeline Followback interview; BMI = brief motivational intervention; FU = follow-up; 1M = 1-month; 6M = 6-month; 12M = 12-month.
Measures
Descriptive information
Participants provided demographic information regarding gender, age, race/ethnicity, residence, and Greek (fraternity or sorority) affiliation. They also provided height and weight for BAC calculations. Alcohol use. All drinking assessments used the previous month as a uniform time frame, and defined a drink as a 10–12 oz. can or bottle of 4–5% beer; 4 oz. glass of 12% table wine; 12 oz. bottle or can of wine cooler; 1.25 oz. shot of 80 proof liquor either straight or in a mixed drink. A modified version of the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985) allowed calculation of drinks per typical week and mean drinks per drinking day. Participants estimated the maximum number of drinks consumed in a single day and the number of hours spent drinking on that day (allowing calculation of peak BAC). BACs were estimated by BAC = [(consumption/2) * (GC/weight)] − (.016*hours), where (a) consumption = number of drinks consumed, (b) hours = number of hours over which the drinks were consumed, (c) weight = weight in pounds, and (d) GC = gender constant (9.0 for females and 7.5 for males) (Matthews & Miller, 1979). Participants also reported frequency of heavy drinking, defined as 5 or more drinks for men and 4 or more drinks for women (Wechsler, Davenport, Dowdall, Moeykens, & Rimm, 1995). This assessment yielded all four of the consumption-related outcome variables.
Alcohol problems
The Rutgers Alcohol Problems Index (RAPI; (White & Labouvie, 1989) assessed alcohol-related problems in the last month (alpha = .82). The RAPI total score served as the fifth outcome variable.
Collateral interviews
To corroborate self-reported drinking, participants identified friends who could provide estimates of the drinks consumed on each day in a typical week in the last month, maximum drinks consumed in the last month, frequency of heavy drinking, and participation in drinking games. Collaterals also reported how often they observed the participant use alcohol in the last month, and their confidence in the accuracy of their reports.
Post-intervention feedback
A modified Session Evaluation Questionnaire (Stiles & Snow, 1984) consisted of two sets of seven items, describing the session (e.g., difficult-easy; valuable-worthless) and the interventionist (e.g., likeable-not likeable, caring-uncaring) on 7-point semantic differentials. Mean scale scores were calculated for each (alphas = .80 and .86, respectively). Participants also provided General Feedback on four 4-point scales: the student’s impression of the session, the accuracy of the feedback, and whether s/he would recommend the intervention to others, and/or to a friend in need of help with drinking.
Screening and Recruitment Procedures
Students enrolled in Introductory Psychology were recruited to a “College Health Study,” and convened in small groups; all provided written consent prior to completing the screening survey, which was administered using a scannable booklet labeled with a unique code number. A Certificate of Confidentiality allowed research staff to provide confidentiality assurances.
Staff telephoned students who met inclusion criteria. The students were told about the procedures, that they would receive course credit for participation through the 1-month follow-up, and $20 and $25 for the 6- and 12-month follow-ups, respectively. If interested, students met with a Research Assistant (RA) in a private office, provided consent and contact information, received their condition assignment, and completed the TLFB interview (if required for their condition). Participants randomized to a BMI condition received an appointment within the next week; control participants were scheduled for the 1-month follow-up. RAs conducting assessments were always different from those conducting interventions, but were not blind to condition.
TLFB Procedure
The TLFB interview was administered in a private room by a trained RA, following standard procedures (Sobell & Sobell, 1996). Participants were oriented to calendars for the previous 90 days, on which holidays and campus events were marked to prompt recall. The RA provided definitions of standard drinks and helped the participant reconstruct daily drinking, starting with the current week and working backwards. The TLFB involved sequential assessment of alcohol use, drug use, and sexual behavior (Carey, Carey, Maisto, Gordon, & Weinhardt, 2001). After daily alcohol use had been documented, the process was repeated for drug use and then for sexual behavior, on the same calendar. A discrete coding scheme allowed the RA to summarize this information on the blocks representing days on the calendar.
Intervention Procedures
The development of the BMIs was based on these assumptions: (a) at-risk student drinkers are ambivalent about the need to change, (b) risk reduction is more acceptable than abstinence, (c) motivation to reduce risks will come from the student’s unique concerns about his/her drinking, and (d) students have the skills to use drinking reduction strategies. Manuals were created for both BMIs, and interventionists were trained to administer them using a motivational interviewing style (Miller & Rollnick, 2002). The interventionists were seven graduate students in clinical or counseling psychology. Using a non-confrontational approach, interventionists created opportunities for students to explore and resolve ambivalence about current drinking patterns, and to find intrinsic reasons for change in the direction of risk reduction. To encourage active participation, interventionists used open-ended questions, invited reactions to information presented, listened carefully and used reflections, emphasized the students’ choice and autonomy, and reinforced change talk. Consistent with motivational interviewing principles, interventionists responded to resistance with reflections, reframes, or shifting focus.
Basic BMI
The basic BMI combined personalized feedback and alcohol education to increase awareness of current drinking and its consequences, facilitate comparisons to peer norms, provide information that increases understanding of the effects of alcohol and the role it plays in the student’s life, and provide tips for reducing risks related to alcohol use. A personalized feedback sheet structured the session, providing information on drinking patterns, local and national gender-specific drinking norms, tolerance, typical and peak BAC, positive and negative alcohol expectancies, alcohol-related negative consequences and risk behaviors (unprotected sex, driving), and discussion of harm reduction, individual goal setting, and tips for safer drinking. Both interventions covered this content.
Enhanced BMI
For this intervention, the basic BMI was enhanced with a decisional balance exercise; this exercise occurred after the discussion of consequences and risk behaviors. This exercise used a worksheet, consisting of a 2 × 2 grid described as “a way to organize your thoughts about your current drinking and any potential changes you might want to make.” The top half of the grid was labeled with “Continuing to drink as I do now”: good things/not-so-good things. The bottom half of the grid was labeled with “Cutting down on my drinking”: What I might lose/What I might gain. The interventionist elicited information for each of the four boxes, summarized the information, ending on the potential advantages of reducing alcohol use, and solicited the student’s reactions. Students received the completed grid to take home.
Common procedure
Participants meet with interventionists in private rooms. The sessions were videotaped for supervision and quality assurance. If a student did not wish to be videotaped, s/he had the options of audiotaping or no taping. After the session, students completed post-intervention ratings, and received an appointment for a one-month follow-up.
Intervention Integrity
Interventionist training, led by Kate B. Carey involved (a) reading about BMIs and college drinking, (b) study of the manuals, (c) practice role-plays with feedback, and (d) reviews of videotaped sessions conducted with confederates. Weekly supervision of videotaped sessions (by Kate B. Carey and Stephen A. Maisto) ensured competence of the interventionists in the motivational style. Adherence to the manual was documented by rating a random set (48%; n = 162) of videotapes, sampling all semesters and interventionists. Raters used a checklist to rate whether all session content was covered; to establish interrater reliability, they rated 20% (n = 33) of the videotapes twice.
Follow-up Procedures
RAs contacted all participants assigned to conditions for follow-up assessments at 1, 6, and 12 months. Four to ten attempts were made to reach participants who were initially non-responsive to reminders. Most students completed the questionnaire in the research offices but some completed them by mail (13% at 6 months, 22% at 12 months) because they were studying abroad or were otherwise not in residence. They received course credit as compensation for the one-month assessment, $20 for the six-month assessment, and $25 for the 12-month assessment.
Students were randomly assigned to have collaterals contacted at one of the four assessment points, a procedure designed to enhance participants’ self-report accuracy. To maximize the credibility of this procedure, we attempted to contact collaterals for 25% of the participants at each assessment time.
Analysis Plan
Hierarchical linear modeling (HLM) was used to test hypotheses regarding intervention efficacy and change over time. Assumptions about the expected effects of the intervention influenced our choice of statistical models. First, we expected no baseline group differences. Second, in the absence of an intervention, we expected controls to gradually decrease their drinking over time, consistent with findings in other intervention trials (Borsari & Carey, 2005; Marlatt et al., 1998; Murphy et al., 2001). Third, we expected the greatest differences between conditions to occur at the one-month follow-up, consistent with previous studies (Borsari & Carey, 2005; Collins, Carey, & Sliwinski, 2002). Standard HLM growth models are unable to model the hypothesized non-linear intervention effect, so we used discontinuous HLM models (Singer & Willett, 2003). We expected that a discontinuity would result from the interventions received by a subset of the sample, such that an intervention should cause an immediate, sharp decrease in behavior that diminishes over time. Analyses were conducted in a forward stepwise fashion for each dependent variable (DV). Predictors were retained if the likelihood ratio test indicated a significant improvement in the model. Models were constructed as follows.
Level-1 (within-persons) model
The initial discontinuous HLM model included four level-1 predictors. First, the Baseline Intercept represents the average level of a DV at baseline. Second, the Control Slope represents the average monthly change in the DV for the control group (time points were coded 0, 1, 6, and 12). Third, the discontinuous aspect of the model originates with the Intervention Intercept, interpreted as the expected difference in the DV for the intervention condition from the controls at the 1-month follow-up. Intervention Intercept estimates are obtained by including a predictor that is coded 0 for all participants at baseline, 0 across the follow-ups for the control group, and 1 across the follow-ups for participants who received an intervention. The final predictor, Intervention Slope, reflects the slope of the intervention groups as an average deviation from the Control Slope, and is obtained by including the time variable recoded to account for the new intercept (coded 0 for all participants at baseline and at the one-month follow-up to reflect the location of the new intercept at 1 month). With four time points, only three level-1 predictors could be modeled as random. Because of their theoretical importance, Baseline and Intervention Intercepts were allowed to vary across individuals, and the slope parameter with the higher variability was allowed to vary.
Level-2 (between-persons) model
The level-2 aspect of the discontinuous HLM model incorporates predictors to differentiate individual growth functions. Level-2 predictors included gender, and a series of dummy-coded variables used to predict the Intervention Intercept and Intervention Slope that distinguishes among the TLFB, basic BMI, and enhanced BMI effects. Incorporating these predictors alters the interpretation of the Intervention Intercept, such that it becomes the difference in the DV at the one-month follow-up between the control condition and the TLFB/control condition. The dummy-codes then determine if receiving any type of BMI (regardless of TLFB) results in significant differences from the TLFB/control condition. Next, additional dummy-coded predictors were added to determine if the effect of a TLFB assessment interacted with the basic or enhanced BMI conditions, first combined and then separated.
Results
Preliminary Analyses
Sample characteristics
The inclusion criteria identified an at-risk sample. When compared to ineligible students (n = 597), eligible students (n = 810) consumed more alcohol across all outcomes (see Table 1). Moreover, eligible students were more likely to be male, White, not freshmen, housed on-campus or in a Greek house, a member of a Greek organization, and older.
Table 1.
Baseline demographic and drinking characteristics of participants
| Screening Sample N = 1407 | Eligible Sample N = 810 | Consented Sample N = 509 | ||||
|---|---|---|---|---|---|---|
| Variable | Ineligible n = 597 | Eligible n = 810 | Not Reached or Not Consented n = 301 | Consented n = 509 | Incomplete Follow-up Data n = 154 | Complete Follow-up Data n = 344 |
| Gender (% female) | 70% | 61%** | 55% | 65%** | 63% | 66% |
| Ethnicity (% White) | 72% | 88%** | 86% | 89% | 90% | 89% |
| Year (% freshmen) | 58% | 55%** | 54% | 55%** | 53% | 56% |
| Residence (% on campus) | 79% | 83%** | 78% | 86%** | 85% | 87% |
| Greek status (% non-Greek) | 91% | 78%** | 77% | 79% | 72% | 82%* |
| Age | 19.7 (3.1) | 19.3 (1.4)** | 19.5 (2.1) | 19.2 (0.8)* | 19.3 (0.9) | 19.2 (0.7) |
| Drinks/week | 3.5 (5.5) | 19.2 (13.6)** | 19.2 (15.2) | 19.2 (12.6) | 20.9 (13.4) | 18.5 (12.1) * |
| Drinks/drinking day | 1.5 (1.7) | 5.6 (3.2)** | 5.9 (3.8) | 5.7 (2.7) | 5.7 (2.9) | 5.6 (2.6) |
| Heavy drinking frequency | 1.0 (2.0) | 6.8 (4.4)** | 6.1 (4.5) | 7.2 (4.4)** | 7.9 (4.5) | 6.8 (4.3) * |
| Peak BAC | 0.09 (0.07) | 0.21 (0.09)** | 0.20 (0.10) | 0.21 (0.09) | 0.21 (0.08) | 0.21 (0.09) |
| RAPI total | 2.1 (3.7) | 7.0 (6.0)** | 6.4 (5.3) | 7.4 (6.3)* | 7.2 (5.9) | 7.5 (6.4) |
Note. Values indicate the means (and standard deviations) unless otherwise noted. All drinking variables sample the previous month. BAC = blood alcohol concentration. RAPI = Rutgers Alcohol Problems Index.
p< .05
p< .01
Comparisons of consenters (n = 509) and non-consenters (n = 301) on demographics and baseline drinking revealed that females were more likely to consent, as were students who lived on campus. Consenting students tended to be younger, but there were no differences in race/ethnicity, or in Greek status between consenters and non-consenters. With regard to drinking behaviors, consenting students had significantly more heavy drinking days, and experienced significantly more alcohol related problems than non-consenting students.
No significant differences emerged for any of the demographic or drinking variables across the six experimental conditions (see Table 2). Thus, randomization was effective in establishing equivalent groups.
Table 2.
Baseline demographics and primary drinking outcome variables for six study groups (n = 509)
| Timeline | No Timeline | |||||
|---|---|---|---|---|---|---|
| Variable | Assessment only | Basic BMI | Enhanced BMI | Assessment only | Basic BMI | Enhanced BMI |
| Sample Size | 89 | 87 | 86 | 81 | 85 | 81 |
| Gender (% female) | 67% | 64% | 64% | 67% | 65% | 64% |
| Ethnicity (% White) | 85% | 92% | 93% | 87% | 90% | 88% |
| Year (% freshmen) | 55% | 51% | 58% | 54% | 51% | 63% |
| Residence (% on campus) | 87% | 86% | 87% | 78% | 88% | 91% |
| Greek status (% non-Greek) | 80% | 80% | 83% | 75% | 74% | 79% |
| Age | 19.3 (0.7) | 19.3 (0.8) | 19.2 (0.7) | 19.2 (0.8) | 19.3 (0.9) | 19.0 (0.8) |
| Drinks/week | 18.1 (8.9) | 19.6 (12.4) | 18.7 (13.2) | 19.3 (11.2) | 20.7 (16.0) | 19.2 (13.0) |
| Drinks/drinking day | 5.5 (2.3) | 5.5 (2.2) | 5.7 (2.5) | 5.8 (2.6) | 5.7 (3.4) | 5.8 (3.3) |
| Heavy drinking frequency | 6.8 (3.8) | 7.4 (5.0) | 6.7 (3.7) | 7.7 (4.1) | 7.6 (5.2) | 7.0 (4.2) |
| Peak BAC | 0.22 (0.09) | 0.22 (0.09) | 0.21 (0.09) | 0.21 (0.09) | 0.21 (0.09) | 0.21 (0.09) |
| RAPI total | 7.8 (6.0) | 7.9 (7.9) | 6.6 (6.2) | 8.3 (5.7) | 6.6 (6.0) | 7.3 (5.5) |
Note. Values indicate the means (and standard deviations) unless otherwise noted. None of the between group differences were significant. BMI = brief motivational intervention; BAC = blood alcohol concentration; RAPI = Rutgers Alcohol Problems Index.
Follow-up rates
Figure 1 shows that 97% of the 509 students provided data at 1 month, 77% provided data at 6 months, and 78% provided data at 12 months. A total of 87% completed two or more follow-ups, and 68% completed all three follow-ups. Greek students were less likely to provide full follow-up data. Students who provided incomplete data drank more in a typical week and had more heavy drinking days at baseline. No other differences emerged among the remaining outcome variables (see last two columns in Table 1).
Collateral verification
A total of 311 participant-collateral pairs were obtained. No differences among conditions were observed in the proportions of collaterals contacted. Collaterals reported observing the participants drink an average of 6 times in the last month, and expressed confidence in most (44%) or some (52%) of their answers. Correlation coefficients and paired t-tests were calculated for (a) typical drinks per week, r = .53, with collateral M = 15.8 (SD = 12.1) and participant M = 15.7 (SD = 12), t (310) = 0.14, p = .89; (b) maximum drinks, r = .52, with collateral M = 8.3 (SD = 4.1) and participant M = 9.1 (SD = 4.6), t (307) = 3.2, p < .01; and (c) frequency of heavy drinking days, r = .58, with collateral M = 5.9 (SD = 4.9) and participant M = 6.4 (SD = 4.4), t (306) = 1.86, p = .06. Correlations were moderate, and when mean differences were found, collaterals underestimated friends’ drinking.
Client satisfaction
Scores for the Session Evaluation items could range from 0–6, with lower scores more favorable. The mean rating of the session was 1.1 (SD = .79). Participants tended to rate the session as easy, valuable, pleasant, comfortable, smooth, relaxed, and safe. The mean rating of the interventionist was .67 (SD = .69), reflecting ratings of friendly, likeable, warm, helpful, caring, understanding, and knowledgeable. On the General Feedback items, 89% of students reported a positive impression of the session, and 66% felt that the feedback information was accurate. Most would recommend such a session to other students (84%) or to a friend in need of help with drinking (82%). The four BMI conditions did not differ on the session or interventionist ratings, or on General Feedback items (all ps >.10).
Intervention fidelity
Adherence to the intervention manuals was evaluated by determining the proportion of prescribed items present (54 items for the Basic BMI, 60 for the Enhanced BMI). On average, interventionists addressed 90% of the content items. The two forms of the BMI did not differ in the percentage of content covered across the 13 common sections, t (160) = .94, p = .17. In the Enhanced condition, all of the specific items defining the decisional balance module were contained in 96% of the rated tapes. Exact agreement for the reliability sample ranged from 80%–100% on the presence or absence of individual items. Basic BMI sessions lasted an average of 65 minutes (SD =20.8), whereas Enhanced BMI sessions lasted an average of 70 minutes (SD= 18.8), a significant difference using a one-tailed test, t (232) = −1.88, p < .03.
Outcome Analyses
All of the alcohol outcomes except peak BAC exhibited positive skew. However, we did not transform the data because transformations obscure the interpretability of the estimated regression coefficients, and growth models fit to transformed data result in nonlinear growth functions across time. Therefore, robust solutions were used to address the nonnormality of the outcomes (Raudenbush & Bryk, 2002). Furthermore, residuals from the final models were examined for extreme departures from normality, and outliers in the outcome variables were recoded to the next highest value plus one. Raw means (and SDs) for all five outcome variables across assessment points appear in Table 3.
Table 3.
Raw Means (Standard Deviations) of Outcome Variables across Assessment Points
| Drinks per Week | ||||||
|---|---|---|---|---|---|---|
| Control | TLFB/Control | BMI Basic | TLFB/BMI Basic | BMI Enhanced | TLFB/BMI Enhanced | |
| Baseline | 19.4 (12.4) | 18.1 (8.9) | 20.7 (16.0) | 19.6 (12.4) | 19.2 (13.0) | 18.7 (13.2) |
| 1 month | 16.4 (9.1) | 16.0 (12.0) | 13.7 (9.5) | 13.3 (10.0) | 13.8 (10.5) | 13.1 (9.2) |
| 6 months | 17.4 (10.6) | 15.9 (10.6) | 14.0 (10.7) | 13.8 (10.2) | 17.6 (13.1) | 14.6 (11.7) |
| 12 months | 15.0 (10.5) | 16.2 (11.6) | 12.8 (9.9) | 14.5 (18.5) | 15.6 (10.8) | 16.5 (13.0) |
|
| ||||||
| Drinks per Drinking Day | ||||||
| Control | TLFB/Control | BMI Basic | TLFB/BMI Basic | BMI Enhanced | TLFB/BMI Enhanced | |
|
| ||||||
| Baseline | 5.8 (2.6) | 5.5 (2.3) | 5.7 (3.4) | 5.5 (2.3) | 5.8 (3.3) | 5.7 (2.5) |
| 1 month | 5.3 (2.3) | 4.9 (2.1) | 4.4 (2.1) | 4.4 (2.1) | 4.8 (3.0) | 4.8 (2.8) |
| 6 months | 5.4 (2.4) | 5.0 (2.2) | 4.3 (2.1) | 4.3 (2.4) | 4.8 (2.2) | 4.6 (2.6) |
| 12 months | 4.6 (2.5) | 5.0 (2.6) | 4.1 (2.5) | 4.1 (3.3) | 4.5 (2.2) | 4.9 (2.9) |
|
| ||||||
| Heavy Drinking Frequency | ||||||
| Control | TLFB/Control | BMI Basic | TLFB/BMI Basic | BMI Enhanced | TLFB/BMI Enhanced | |
|
| ||||||
| Baseline | 7.7 (4.1) | 6.8 (3.8) | 7.6 (5.2) | 7.4 (5.0) | 7.0 (4.2) | 6.7 (3.9) |
| 1 month | 6.2 (4.0) | 6.0 (4.5) | 5.1 (4.0) | 4.9 (4.1) | 5.1 (4.7) | 4.7 (3.9) |
| 6 months | 7.4 (5.4) | 7.1 (5.2) | 6.2 (5.0) | 5.3 (4.1) | 7.0 (5.3) | 5.8 (4.3) |
| 12 months | 5.1 (4.0) | 6.3 (4.3) | 4.9 (3.5) | 5.2 (4.4) | 5.7 (4.2) | 6.4 (5.3) |
|
| ||||||
| Peak BAC | ||||||
| Control | TLFB/Control | BMI Basic | TLFB/BMI Basic | BMI Enhanced | TLFB/BMI Enhanced | |
|
| ||||||
| Baseline | .21 (.09) | .22 (.09) | .21 (.09) | .22 (.09) | .21 (.09) | .21 (.09) |
| 1 month | .18 (.09) | .19 (.09) | .16 (.09) | .15 (.09) | .17 (.12) | .17 (.12) |
| 6 months | .20 (.11) | .19 (.11) | .17 (.10) | .16 (.10) | .18 (.11) | .18 (.10) |
| 12 months | .17 (.10) | .20 (.12) | .16 (.08) | .14 (.09) | .16 (.10) | .19 (.14) |
|
| ||||||
| RAPI | ||||||
| Control | TLFB/Control | BMI Basic | TLFB/BMI Basic | BMI Enhanced | TLFB/BMI Enhanced | |
|
| ||||||
| Baseline | 8.3 (5.7) | 7.8 (6.0) | 6.6 (6.0) | 8.0 (7.8) | 7.3 (5.5) | 6.6 (6.2) |
| 1 month | 8.5 (6.7) | 7.4 (5.6) | 5.9 (6.6) | 5.4 (5.2) | 6.2 (5.7) | 5.4 (5.0) |
| 6 months | 8.2 (8.0) | 7.2 (5.5) | 6.3 (7.1) | 5.3 (4.9) | 6.5 (6.1) | 4.7 (5.0) |
| 12 months | 5.3 (5.1) | 7.2 (7.3) | 4.7 (5.2) | 4.3 (3.9) | 5.5 (6.3) | 5.1 (5.7) |
Note: TLFB = Timeline Followback interview; BMI = brief motivational intervention; BAC = blood alcohol concentration; RAPI = Rutgers Alcohol Problems Index.
The discontinuous HLM models were fit using HLM software (Version 6.2, Raudenbush, Bryk, Cheong, Congdon, & du Tiot, 2004). Model comparisons were conducted using the full maximum likelihood estimation procedure, but final robust estimates were obtained using the restricted maximum likelihood algorithm. The variation in the estimated Intervention Slopes was not significant for any outcome, so the models held individual’s growth following the intervention constant across all intervention participants (i.e., as a level-1 fixed effect).
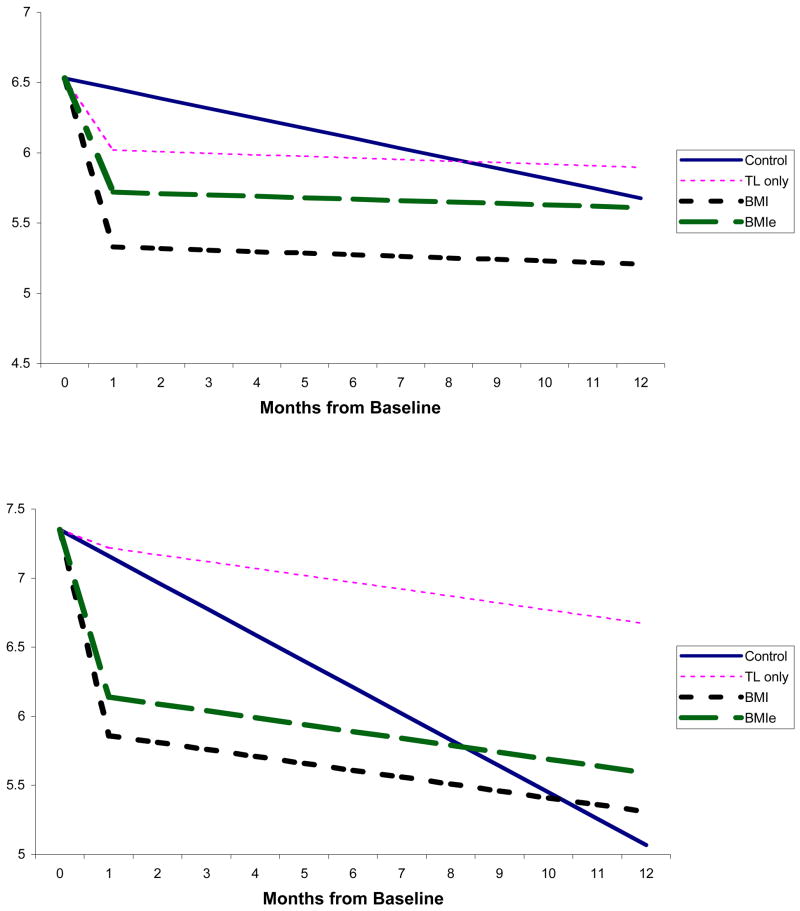
Level-1 model
For all of the outcomes, the discontinuous HLM model fit the data significantly better than a standard continuous model. Across all outcomes, the estimated discontinuous HLM models were as predicted: on average, the control group decreased gradually over 12 months, whereas the intervention groups exhibited a sharp drop at the 1-month follow-up, then remained relatively constant across the 12 months.
Baseline Intercept
Estimates for the final model are summarized in Table 4. Gender was a significant predictor of baseline drinking, so it was included as a covariate in the model. As a result, the Baseline Intercepts in row A represent baseline values for the males on the five outcome variables (columns a – e). The values for gender in row B reflect adjustments from the baseline intercept necessary to describe the baseline values for women. Women reported fewer drinks per week, drinks per drinking day, and fewer heavy drinking days than did men; women achieved higher peak BACs, but did not differ from men on RAPI scores.
Table 4.
Fixed effect estimates for the discontinuous hierarchical linear modeling models for typical drinks per week, drinks per drinking day, heavy drinking days, peak BAC, and RAPI score
| a | b | c | d | e | ||
|---|---|---|---|---|---|---|
| Drinks per week | Drinks per day | Heavy drinking days | Peak BAC | RAPI | ||
| A | Baseline Intercepts | 23.04 (7.99) | 6.53 (1.58) | 7.97 (3.23) | 0.200 (.064) | 7.35 (4.87) |
| B | Gender (0 = Male, 1= Female) | −6.64 | −1.51 | −1.31 | 0.015 | 0.03 |
|
| ||||||
| C | Control Slope | −0.24 (0.41) | −0.07 (0.13) | −0.12 (0.07) | −0.002 (.003) | −0.22 (0.19) |
|
| ||||||
| Intervention Intercepts | ||||||
| D | TLFB Intercept | −3.03 (3.21) | −0.44 (1.26) | −0.84 (0.78) | −0.021 (.039) | 0.09 (3.04) |
| Model A: | ||||||
| E | Combined BMI Intercept | −1.95 | −0.48 | −0.98 | −0.023 | −1.21 |
| Model B: | ||||||
| F | Basic BMI Intercept | −2.66 | −0.66 | −1.30 | −0.032 | −1.33 |
| G | Enhanced BMI Intercept | −1.22 | −0.30 | −0.64 | −0.014 | −1.08 |
|
| ||||||
| H | Intervention Slope | 0.35 | 0.06 | 0.18 | 0.002 | 0.17 |
Note. All estimates are significant at p < .05 except for underlined estimates, which are not significant. Values in parentheses are estimated standard deviations of random effects at Level–2. Model A refers to the model in which both brief motivational interventions (BMIs) are combined and entered as one factor; Model B refers to the model in which the Basic and Enhanced BMIs are entered as separate factors. BAC = blood alcohol concentration; RAPI = Rutgers Alcohol Problems Index; TLFB = Timeline Followback interview.
Control Slope
Across all outcomes, participants in the control group gradually but significantly decreased over the year (row C in Table 4). On average, for each month, participants in the control group drank .24 fewer drinks per week, drank .07 fewer standard drink per drinking day, had .12 fewer heavy drinking days, decreased their peak BACs by .002, and achieved a score of .22 less on the RAPI. Thus, over 12 months, we would expect college students in the control group to drink 2.9 fewer drinks per week (i.e., 12 × .24), .8 fewer drinks per drinking day, have 1.4 fewer heavy drinking days per month, decrease their peak BAC by .02, and score lower on the drinking consequences measure by 2.6 points.
Intervention Intercepts
The Intervention Intercepts represents the difference between the intervention and control groups at the 1-month follow-up. Initial statistical models compared individuals who received a TLFB/control to individuals who received either BMI (ignoring TLFB status). Next, the combined BMI effect was separated to examine individually the effects of the Basic BMI and the Enhanced BMI. Subsequent models tested interactive effects of a TLFB plus a BMI (first combined, then Basic vs. Enhanced); these revealed no synergistic effect of TLFB plus BMI on any outcome variable. To minimize complexity, we collapsed the BMI conditions across TLFB assessment status and compared them to the TLFB/control condition.
For the four consumption outcomes (Columns a–d in Table 4), the TLFB/control condition exhibited significant differences from the control condition; this is reflected in the row labeled TLFB Intercept (row D). The models indicated that, at the 1-month follow-up, students in the TLFB/control condition consumed 3 fewer drinks per typical week than controls, consumed .44 fewer drinks per drinking day, had .84 fewer heavy drinking days per month, and lowered their peak BACs by .021. However, TLFB/control participants did not differ from controls in reporting of negative consequences at the 1-month follow-up.
Participants who received either BMI (regardless of their TLFB status) demonstrated significant reductions beyond those achieved by the TLFB/control condition across all outcome variables (row E). For all five DVs, the model including the BMIs fit the data better than the model including TLFB/control. When the BMI conditions were entered separately (see rows F and G), the intercept for the Basic BMI differed from the TLFB/control intercept on all outcomes, whereas the intercept for the Enhanced BMI did not. Compared to the TLFB/control condition, participants who received a Basic BMI drank 2.66 fewer drinks per week, .66 fewer drinks per drinking day, had 1.3 fewer heavy drinking days, and decreased their peak BACs by .032. Furthermore, unlike the TLFB/control condition, participants who received a Basic BMI had lower consequences scores at the 1-month follow-up.
Although the consumption outcome averages were all lower for the Enhanced BMI condition than the TLFB/control condition, they were not significantly lower. Thus, counter to predictions, the Enhanced BMI did not produce outcomes that were better than those of the Basic BMI. The effects of the Enhanced BMI were all smaller than the Basic BMI, but overlapping 95% confidence intervals indicate that they were not significantly different from each other.
Intervention Slope
The Intervention Slope did not differ across intervention type but it differed significantly from the Control Slope. Predicted change over time for the intervention groups is derived by adding the effect estimate for the Intervention Slope (row H) to that obtained for the Control Slope (row C). Consequently, each month, intervention participants increased their typical drinks per week by .11, decreased their drinks per typical day by −.01, increased their heavy drinking days by .06, exhibited no change in their peak BAC, and decreased their RAPI score by −.05; however, none of these slopes differs from 0.
Figure 2 depicts the discontinuous models for two outcome variables. The difference in slopes between the control and intervention groups revealed different trajectories over time after the initial discontinuity at one-month. A series of one-way analyses of variance indicated that, by the 12-month follow-up, all groups were once again equivalent on all five outcome variables.
Figure 2.
Discontinuous Hierarchical Linear Models for Drinks per Drinking Day (top panel) and Alcohol Problems (bottom panel). Lines illustrate main effects of Control Condition, Timeline (TL) only, basic brief motivational intervention (BMI), and enhanced BMI (BMIe). RAPI = Rutgers Alcohol Problems Index.
Effect sizes
Within-group effects were calculated for the BMI conditions using data in Table 3. At one month, within-group effect sizes (d) averaged across the four BMI groups ranged from d = .21 (RAPI) to d = .53 (peak BAC) – small to medium effect sizes (Cohen, 1988). The TLFB/Basic BMI group produced the largest within-group effect sizes at one month for all 5 outcome variables: drinks/week d = .51, drinks/drinking day d = .50, heavy drinking frequency d = .50, peak BAC d = .73, and RAPI d = .33. At 12 months, within-group effect sizes averaged across the four BMI groups ranged from d = .33 (heavy drinking frequency) to d = .53 (peak BAC). The two Basic BMI groups produced the largest 12-month effects: drinks/week d = .49 (Basic BMI), drinks/drinking day d = .61 (TLFB/Basic BMI), heavy drinking frequency d = .51 (Basic BMI), peak BAC d = .89 (TLFB/Basic BMI) and RAPI d = .48 (TLFB/Basic BMI).
To characterize the between-groups effects, we focus on comparisons between the two conditions without any BMI (Control and TLFB/control) and the two conditions that included a Basic BMI, because primary outcome analyses revealed incremental effects of both TLFB and Basic BMI. We used Cohen’s d with pooled standard deviations as our effect size metric. As illustrated in the left side of Table 5, effect sizes comparing the Control condition to the Basic BMI at 1-month are small to moderate, ranging from .22 to .41. Comparing the Control to the TLFB/Basic BMI means enhances the effect sizes (.32 to .52), consistent with main effects of both TLFB and Basic BMI suggested by the HLM analyses. At one month, effect sizes comparing the “active” TLFB/control to the Basic BMI range from .21 to .33; they are slightly higher (.24 to .44) for the TLFB/control comparison with TLFB/Basic BMI. Overall, between groups effect sizes involving the Control condition are reduced at 12 months, due to gradual improvement of the Controls. Notably, small effect sizes are maintained at 12 months for three of the five outcomes in the combined TLFB/Basic BMI condition. Counterintuitively, effect sizes comparing the “active” TLFB/control to both Basic BMI conditions increase somewhat at 12 months. Inspection of the means in Table 3 reveals that the TLFB/control condition did not exhibit as strong a trend to maintain reductions over time as did the BMI or Control conditions.
Table 5.
Between groups effect sizes comparing Control and TLFB/control conditions to the Basic BMI and the TLFB/Basic BMI conditions
| 1-Month Assessment
|
12-Month Assessment
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Control versus
|
TLFB/Control versus
|
Control versus
|
TLFB/Control versus
|
|||||
| Basic BMI | TLFB/Basic BMI | Basic BMI | TLFB/Basic BMI | Basic BMI | TLFB/Basic BMI | Basic BMI | TLFB/Basic BMI | |
| Drinks per week | .29 | .32 | .21 | .26 | .22 | .03 | .31 | .11 |
| Drinks per drinking day | .41 | .41 | .24 | .24 | .20 | .17 | .35 | .30 |
| Heavy drinking frequency | .27 | .32 | .21 | .25 | .05 | −.02 | .36 | .25 |
| Peak BAC | .22 | .33 | .33 | .44 | .11 | .32 | .39 | .57 |
| RAPI | .39 | .52 | .24 | .37 | .12 | .22 | .39 | .50 |
Note. Values in the table represent Cohen’s d calculated with pooled standard deviations. Small effect sizes (.15–.39) are underlined; medium effect sizes (.40–.74) appear in bold. BMI = brief motivational intervention. TLFB = Timeline Followback interview; BAC = blood alcohol concentration; RAPI = Rutgers Alcohol Problems Index.
Discussion
Significant and lasting risk reduction can be achieved with brief individual interventions designed for heavy drinking college students. We tested three hypotheses regarding the efficacy of BMIs. First, we hypothesized and found that a pre-intervention TLFB assessment of daily drinking reduced both typical and risky alcohol consumption, relative to controls. However, the lack of an interaction between receiving a TLFB and participation in the BMIs indicated that a pre-intervention TLFB did not enhance students’ responses to the BMIs.
This is the first controlled demonstration indicating that participation in a TLFB can reduce alcohol use. One explanation for this effect is that it raised awareness of risky drinking patterns, and prior research has shown that a detailed TLFB can increase risk perception (Carey, Carey, Maisto, Gordon, & Weinhardt, 2001; Weinhardt, 2002). Awareness raising is a process linked with movement from precontemplation to contemplation stages of change, according to the Transtheoretical Model (Prochaska, DiClemente, & Norcross, 1992). According to self-regulation theory (Brown, 1998), problem recognition occurs when one becomes aware that current behavior deviates from a desired standard. It is possible that seeing drinking patterns on the TLFB activated an internal standard of comparison. The awareness-raising function of the TLFB may have provoked processes of self-correction for some participants.
Our second hypothesis was that a personalized BMI would reduce drinking. Indeed, we observed improvements across all four consumption indices as well as negative consequences within one month of receiving a BMI. These improvements exceeded the reductions associated with the TLFB/control condition. Our findings add to the growing literature documenting the efficacy of individually-administered BMIs for at-risk college drinkers (Baer, Kivlahan, Blume, McKnight, & Marlatt, 2001; Borsari & Carey, 2000; Murphy et al., 2004; Murphy et al., 2001). Importantly, this study demonstrated differential improvement compared to two comparison conditions, a standard assessment control and an active TLFB/control condition. Thus, a BMI provides active ingredients beyond the hypothesized awareness-raising of extended assessment.
Our findings also elucidate the pattern of outcomes over time, using an analytic technique that allowed us to model post-intervention slopes. Students in the control condition drank less over the follow-up year, consistent with other longitudinal (Schulenberg, O’Malley, Bachman, Wadsworth, & Johnston, 1996; Weingardt et al., 1998) and brief intervention (Marlatt et al., 1998) studies. In contrast, the BMI groups produced reductions much more quickly – within one month – with essentially flat slopes for the rest of the year. Although the groups were equivalent by 12 months, the intervention groups spent more of the follow-up period at lower consumption levels. Such a pattern of early effects from BMIs with dimishing between-group effects over time corroborates a meta-analysis of MI studies (Hettema, Steele, & Miller, 2005). From a public health perspective, the expedited reduction of risk behaviors confers immediate benefits to both the student and the campus community (Weitzman & Nelson, 2004).
With regard to our third hypothesis, we determined that the addition of a decisional balance module to the BMI did not enhance outcomes. In contrast to the Basic BMI, the Enhanced BMI did not improve outcomes beyond those produced by the TLFB/control condition. Although counter-intuitive, the Basic BMI produced stronger effects on both typical and risky drinking. These findings, together with those of an earlier study (Collins & Carey, 2005), challenge the value of decisional balance exercises for college drinkers.
We speculate that an unintended outcome of completing the DB was to remind students of the benefits gained from drinking. Although heavy drinking students acknowledge the costs of their drinking, they also identify many benefits. As a result, the DB may not be developing sufficient discrepancy to motivate behavior change. An alternative explanation is that the DB exercise prompts an introspective process, in which students were (implicitly) encouraged to compare their drinking to an internal standard. In contrast, the Basic BMI encourages students to compare their drinking to an external standard (i.e., normative drinking patterns). Thus, the Basic BMI may be better suited to young adults who look to peers for standards to guide their behavior. A final consideration is that therapeutic activities that are not matched to readiness-to-change can produce reactance and negative outcomes (Miller & Rollnick, 2002). Thus, unless students are ready to change their drinking behavior, the Basic BMI (which relies on the feedback method of discrepancy development) may be better suited.
On the Basis of the patterns of effect sizes, we offer the following recommendations for practice. Both the Basic BMI alone and supplemented with the TLFB produce significant risk reduction at one month; the Basic BMI/TLFB combined intervention produced the largest short-term changes, generalizing across measures of typical and heavy consumption and alcohol-related problems. Both interventions using the Basic BMI produced long-term risk reduction, with medium to large within-group effects. Thus, the Basic BMI is an effective intervention for both short- and long-term risk reduction, and supplementing it with the TLFB extended assessment is likely to enhance risk reduction in the short-term. Future research may reveal predictors of response to the Basic BMI and TLFB components.
One limitation of our study was the use of retrospective self-reports, which are subject to recall bias. However, we used methods to optimize data quality, including gathering multiple indicators of drinking, providing assurances of confidentiality, and obtaining collateral verification. A second limitation is that our sample lacked diversity. The inclusion criteria (i.e., heavy drinking) effectively excluded minority students who tend not to drink as heavily as White students (O’Malley & Johnston, 2002). Therefore, we suggest caution when generalizing these findings to communities containing larger proportions of racial and ethnic minorities. The efficacy of BMIs for young adult drinkers from diverse backgrounds deserves further study.
Several strengths of this study enhance confidence in the validity and generalizability of the findings. First, the large sample provided excellent statistical power. Second, we retained nearly all students through one month, and a large percentage through the entire year. Our follow-up rates compare favorably with those obtained by others conducting research with this population (Baer, Kivlahan, Blume, McKnight, & Marlatt, 2001; Fromme & Corbin, 2004; Larimer et al., 2001). Third, use of collateral verification enhances confidence in students’ self-reports. Fourth, interventionists were carefully trained and supervised, enhancing treatment integrity. Fifth, our statistical approach allowed us to better characterize the variability within our data (i.e., the discontinuous model). Finally, we observed a pattern of findings across multiple indicators of alcohol use, enhancing confidence in the generalizability of these effects.
Acknowledgments
K. B. Carey, M. P. Carey, S. A. Maisto, J. M. Henson, Center for Health and Behavior, Syracuse University. J. M. Henson is now at the Department of Psychology at Old Dominion University. This work was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01-AA12518 to Kate B. Carey. The authors thank Brian Borsari, Tanesha Cameron, John Hustad, Carrie Luteran, Stephanie Martino, Dan Neal, Kevin O’Shea, C. Teal Pedlow, Mary Spagnola, Kalyani Subbiah, Dawn Sugarman, and Andrea Weber for their assistance with this project.
References
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68:728–733. [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors. 2005;19:296–302. doi: 10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JM. Self-regulation and the addictive behaviors. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. 2. New York: Plenum Press; 1998. pp. 61–73. [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. International Journal of STDs and AIDS. 2001;12:365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA. Subject reactivity effects and alcohol treatment outcome research. Journal of Studies on Alcohol. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analyses for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Collins SE, Carey KB. Lack of effect for decisional balance as a brief motivational intervention for at-risk college drinkers. Addictive Behaviors. 2005;30:1425–1430. doi: 10.1016/j.addbeh.2005.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE, Carey KB, Sliwinski MJ. Mailed personalized normative feedback as a brief intervention for at-risk college drinkers. Journal of Studies on Alcohol. 2002;63:559–567. doi: 10.15288/jsa.2002.63.559. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students (BASICS) New York: Guilford; 1999. [Google Scholar]
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology. 2004;72:1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. A meta-analysis of research on motivational interviewing treatment effectiveness. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Zakocs RC, Kopstein A, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24. Journal of Studies on Alcohol. 2002;63:136–144. doi: 10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision making: A psychological analysis of conflict, choice and commitment. New York: Free Press; 1977. [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention and treatment: a review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol Suppl. 2002:148–163. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, et al. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62:370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, et al. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Matthews DB, Miller WR. Estimating blood alcohol concentration: two computer programs and their applications in therapy and research. Addictive Behaviors. 1979;4:55–60. doi: 10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford; 2002. [Google Scholar]
- Murphy JG, Duchnick JJ, Vuchinich RE, Davison JW, Karg RS, Olson AM, et al. Relative efficacy of a brief motivational intervention for college student drinkers. Psychology of Addictive Behaviors. 2001;15:373–379. doi: 10.1037//0893-164x.15.4.373. [DOI] [PubMed] [Google Scholar]
- O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol Suppl. 2002:23–39. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. American Psychologist. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. London: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YK, Congdon RT, du Tiot M. HLM 6: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software; 2004. [Google Scholar]
- Robinson SE, Roth SL, Gloria AM, Keim J, Sattler H. Influence of substance abuse education on undergraduates’ knowledge, attitudes and behaviors. Journal of Alcohol and Drug Education. 1993;39:123–130. [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Sobell LC, Sobell MB. Timeline FollowBack user’s guide: A calendar method for assessing alcohol and drug use. Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- Stiles WB, Snow JS. Counseling session impact as seen by novice counselors and their clients. Journal of Counseling Psychology. 1984;31:3–12. [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: what, why and for whom? Addictive Behaviors. 2005;30:1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Rimm EB. A gender-specific measure of binge drinking among college students. American Journal of Public Health. 1995;85:982–985. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Weingardt KR, Baer JS, Kivlahan DR, Roberts LJ, Miller ET, Marlatt GA. Episodic heavy drinking among college students: Methodological issues and longitudinal perspectives. Psychology of Addictive Behaviors. 1998;12:155–167. [Google Scholar]
- Weinhardt LS. Effects of a detailed sexual behavior interview on perceived risk of hiv infection: Preliminary experimental analysis in a high risk sample. Journal of Behavioral Medicine. 2002;25:195–203. doi: 10.1023/a:1014888905882. [DOI] [PubMed] [Google Scholar]
- Weinhardt LS, Carey KB, Carey MP. HIV risk sensitization following a detailed sexual behavior interview: a preliminary investigation. Journal of Behavioral Medicine. 2000;23:393–398. doi: 10.1023/a:1005505018784. [DOI] [PubMed] [Google Scholar]
- Weitzman ER, Nelson TF. College student binge drinking and the “prevention paradox”: Implications for prevention and harm reduction. Journal of Drug Education. 2004;34:247–266. doi: 10.2190/W6L6-G171-M4FT-TWAP. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]