Abstract
Background
The relationship between population trends in delaying childbirth and rising rates of primary cesarean delivery is unclear. The aims of the present study were (1) to characterize the association between maternal age and the outcome of labor, (2) to determine the proportion of the increase in primary cesarean rates that could be attributed to changes in maternal age distribution, and (3) to determine whether the contractility of uterine smooth muscle (myometrium) varied with maternal age.
Methods and Findings
We utilized nationally collected data from Scotland, from 1980 to 2005, and modeled the risk of emergency cesarean section among women delivering a liveborn infant in a cephalic presentation at term. We also studied isolated myometrial strips obtained from 62 women attending for planned cesarean delivery in Cambridge, England, from 2005 to 2007. Among 583,843 eligible nulliparous women, there was a linear increase in the log odds of cesarean delivery with advancing maternal age from 16 y upwards, and this increase was unaffected by adjustment for a range of maternal characteristics (adjusted odds ratio for a 5-y increase 1.49, 95% confidence interval [CI] 1.48–1.51). Increasing maternal age was also associated with a longer duration of labor (0.49 h longer for a 5-y increase in age, 95% CI 0.46–0.51) and an increased risk of operative vaginal birth (adjusted odds ratio for a 5-y increase 1.49, 95% CI 1.48–1.50). Over the period from 1980 to 2005, the cesarean delivery rate among nulliparous women more than doubled and the proportion of women aged 30–34 y increased 3-fold, the proportion aged 35–39 y increased 7-fold, and the proportion aged ≥40 y increased 10-fold. Modeling indicated that if the age distribution had stayed the same over the period of study, 38% of the additional cesarean deliveries would have been avoided. Similar associations were observed in multiparous women. When studied in vitro, increasing maternal age was associated with reduced spontaneous activity and increased likelihood of multiphasic spontaneous myometrial contractions.
Conclusions
Delaying childbirth has significantly contributed to rising rates of intrapartum primary cesarean delivery. The association between increasing maternal age and the risk of intrapartum cesarean delivery is likely to have a biological basis.
Gordon Smith and colleagues find a linear increase in the log odds of cesarean delivery with advancing maternal age from 16 years upwards, and that increasing maternal age is associated with reduced spontaneous uterine activity but increased multiphasic spontaneous myometrial contractions.
Editors' Summary
Background.
The rising rates of cesarean sections have been a concern for over two decades. An acceptable rate of cesarean sections is between 10% and 15% for countries in the developed world, according to the World Health Organization (WHO). However, the estimated rate in the United Kingdom was 20% in 2004. In Canada, it was estimated at 22.5% in 2001–2002. And in the United States, the rate was 30.2% in 2005 (rising 46% since 1996).
This increase may have implications for the mother, baby, healthcare providers, and policy makers. Though it is difficult to directly compare risks between vaginal and cesarean deliveries, higher mortality and morbidity rates are associated with the latter. Risks encountered during the operation may include anesthetic complications and difficulty in stopping bleeding. Later risks include infections, wound healing problems, and increased risk of problems in subsequent pregnancies including malpresentation, placenta previa, and uterine rupture.
Why Was This Study Done?
The trend of increased rates of cesarean sections with maternal age appears to be consistent in different countries and has previously been reported by several epidemiological studies. However, it remains unclear why the risk of having cesarean section is associated with advancing maternal age. Could the association reflect a biological effect of advanced age, or is it a consequence of physician and maternal preference?
The researchers aimed to (1) characterize the association between maternal age and the outcome of labor, (2) determine the proportion of the increase in primary cesarean rates that could be attributed to changes in maternal age distribution, and (3) determine whether the contractility of uterine smooth muscle (myometrium) varied with maternal age.
What Did the Researchers Do and Find?
To address aims (1) and (2), the researchers analyzed data collected over the period 1980 to 2005 by the Scottish Morbidity Record (SMR2), which has been demonstrated to be 99% complete since the late 1970s and free from substantial errors in more than 98% of the records in most of the specific fields used for their analysis.
Their analysis showed a linear association between the risk of having a cesarean section and advancing maternal age in first pregnancies. The cesarean rate also more than doubled over the study period. They estimated that 38% of the additional procedures would have been avoided if maternal age distribution had remained the same as in 1980. Therefore they conclude that a substantial part of the increase may be associated with the trend of delaying of first childbirth.
They then hypothesized that this trend is a result of a biological effect of aging on the contractility of the uterus. This hypothesis was further evaluated with aim (3) of the study, where they biopsied the uteri of 62 women (of mixed parity) undergoing routine elective cesarean delivery to test their contractility. They found that advancing age was associated with impaired uterine function as evidenced by a reduced degree of spontaneous contraction and the type of spontaneous contraction.
What Do These Findings Mean?
This study adds to the evidence that advancing maternal age is associated with higher rates of cesarean sections. It also suggests a possible mechanism for this association, i.e., impaired uterine function. Though it was not studied here, the researchers hypothesize that impaired uterine contractility may be a consequence of prolonged stimulation of the uterus by estrogen and progesterone, resulting from a prolonged interval between menarche and first birth. Further research is needed to understand the determinants and management of dysfunctional labor in older women to help design strategies for reducing population cesarean delivery rates without adversely affecting maternal and infant outcomes.
Additional Information.
Please access these Web sites via the online version of this summary at http://dx.doi.org/10.1371/journal.pmed.0050144.
NHS Choices is a patient information Web site developed to help patients take control of their health care
Wikipedia has a section on cesarean section (Note that Wikipedia is an internet encyclopedia that anyone can edit)
MedlinePlus also has information on cesarean section
Introduction
Rising rates of cesarean delivery are a major public health concern. In recent years, the proportion of women attempting vaginal birth after cesarean (VBAC) has declined [1]. Hence, rates of primary cesarean delivery will become an increasingly important determinant of overall cesarean rates. Many studies have demonstrated that rates of primary cesarean delivery have risen throughout the developed world in recent years [2–4], and the reasons for this are unclear. Some of the increase can be explained by changes in obstetric practice, such as the trend toward elective cesarean delivery when the infant presents by the breech [5]. However, the rise in primary cesarean rates has coincided with a trend of increasing average maternal age at the time of first birth. Previous studies have demonstrated that the risk of cesarean delivery increases with advancing maternal age. However, it is currently unclear whether the association reflects a biological effect of advanced age [6,7] or is a consequence of physician and maternal preference [8,9]. The contribution of delaying childbirth to recent rises in cesarean delivery rates is also unclear [3,10–12]. The aims of the present study were (1) to characterize the association between maternal age and the outcome of labor, (2) to determine the proportion of the increase in primary cesarean rates that could be attributed to changes in maternal age distribution, and (3) to determine whether the contractility of uterine smooth muscle (myometrium) varied with maternal age.
Methods
Population
The Scottish Morbidity Record (SMR2) collects information on clinical and demographic characteristics and outcomes for all patients discharged from Scottish maternity hospitals. The register has been greater than 99% complete since the late 1970s [13]. A quality assurance analysis in 1996–1997 compared 1,414 records with the clinical notes. This analysis demonstrated that the register was free from significant errors in greater than 98% of records in all the specific fields used in the present analysis, with the exception of postcode (94.0%), height (96.2%), estimated gestation (94.4%), and method of induction of labor (93.6%). The mode of delivery field was 99.2% accurate. The main focus of the present study was nulliparous women having a singleton birth in Scotland between 1980 and 2005, inclusive. The exclusion criteria were preterm birth, stillbirth, delivery by prelabor cesarean, noncephalic presentation of the infant, and records with missing data on key variables. We repeated the analyses in women who had one or two previous vaginal births.
Definitions
Emergency intrapartum cesarean delivery was defined as any nonplanned cesarean delivery with a documented duration of labor. Operative vaginal delivery was defined as birth using the assistance of obstetric forceps or vacuum (ventouse). Maternal age was defined as the age of the mother at the time of birth. Maternal height was measured in centimeters, and the value used was that documented in each woman's clinical record. Gestational age at birth was defined as completed weeks of gestation on the basis of the estimated date of delivery in each woman's clinical record. Gestational age has been confirmed by ultrasound in the first half of pregnancy in more than 95% of women in the United Kingdom since the early 1990s. Preterm birth was defined as delivery before 37 completed wk of gestation. Birth weight was converted into percentiles for week of gestation and these were calculated separately for males and females.
Myometrial Contractility Studies
Biopsies of the uterus were obtained from nonlaboring patients, undergoing routine elective cesarean delivery at the Rosie Hospital, Cambridge, UK at 38–40 wk pregnancy. Most of the cesarean deliveries were performed for breech presentation or previous cesarean delivery. The procedure was approved by the Cambridge Local Research Ethics Committee 2, and all patients gave written informed consent to participate. Following delivery of the infant, placenta, and membranes, specimens were taken from the upper edge of the lower segment uterine incision and placed into ice-cold Krebs solution. Samples were stored in Krebs solution at 4 °C (with EDTA-free protease inhibitors) overnight and then cleared of serosa, fibrous or damaged tissue, and any visible blood vessels. The muscle tissue was dissected into longitudinal strips (following the plane of the muscle fibers) of approximately 1–3 mm × 8–12 mm. Tissue strips were mounted in an organ bath (Radnoti) filled with Krebs solution at 37 °C and gassed with 95% O2 and 5% CO2. The Krebs solution was changed at 15-min intervals. Myometrial strips were secured by thread to an isometric tension transducer (MLT0201/RAD, ADInstruments), and the signal amplified and stored in a commercial data acquisition system (Octal ML228 Bridge Amplifier; Chart, version 5.2.2, both ADInstruments). Strips were stretched to 2 g tension, which was re-set 30 min later. After a total period of 90 min of equilibration following initial set up, a standardized contraction in response to 50 mM KCl was obtained.
Statistics
Continuous variables were summarized by the median and interquartile range, and groups were compared using the Mann-Whitney U test. Dichotomous data were compared between groups using the χ2 test or χ2 test for trend, as appropriate. All p-values were two sided, and statistical significance was assumed at p < 0.05. In the analysis of cesarean section risk, the numerator was all intrapartum cesarean deliveries and the denominator was all births. In the analysis of the risk of operative vaginal delivery, the numerator was all forceps or vacuum deliveries and the denominator was all vaginal births. Adjusted odds ratios were obtained using logistic regression using age as a continuous variable and with all other variables categorized [14]. Women with missing data on covariates were excluded from the multivariate analysis. The association between maternal age and cesarean section risk was compared between the whole population and those with complete data on covariates. Linearity of age in logistic models was tested using fractional polynomials, and interactions were tested using the likelihood ratio test.
In order to estimate the effect of changes in the age distribution on cesarean rates, we performed an analysis where we estimated what the annual cesarean section rate would have been had the age distribution of mothers remained unchanged over the period from 1980 to 2005. We did this by calculating a new age variable to represent the age of each mother had the age distribution remained constant over the period from 1980 to 2005. For example, a woman having a first birth in 2003 who was on the 76th percentile of age for 2003 would have a new age variable equivalent to the 76th percentile of age in 1980. The logistic regression equations fitted for the observed values of age were then used to derive an estimated probability of cesarean delivery using the new age variable. The mean probability for all women in a given year was then taken as the estimated rate of cesarean delivery had the maternal age distribution stayed the same as in 1980.
All recording of spontaneous contractile activity was performed blind to the mother's age. Contractile activity was quantified by integrating the area under the tension curve. Spontaneous activity was quantified as the ratio of the area under the curve for the 15 min prior to addition of potassium to the area under the curve for the 7 min in the presence of 50 mM potassium. The ratio was log transformed to normalize its distribution and the log10 of the ratio was called the “contraction unit.” A multiphasic contraction was defined as having two or more distinct peaks prior to the return to baseline. In order to maximize the statistical power of the analysis, we studied multiple strips from the same women. However, most regression methods assume that observations are independent and our approach necessitated that we use regression methods that could account for the nonindependence of different strips from the same woman. Hence, analysis of the association between maternal age and spontaneous contractile activity was performed using a linear mixed model with a random effect at the maternal level, to account for the nonindependence of different strips obtained from the same woman. The probability of multiphasic contractions was assessed using logistic regression, and the frequency of spontaneous contractions prior to potassium was assessed using Poisson regression. Both regression methods employed generalized estimating equations and were clustered on the maternal identifier to account for nonindependence. All analyses were performed using Stata, version 10 (Stata Corporation).
Results
Study Cohort
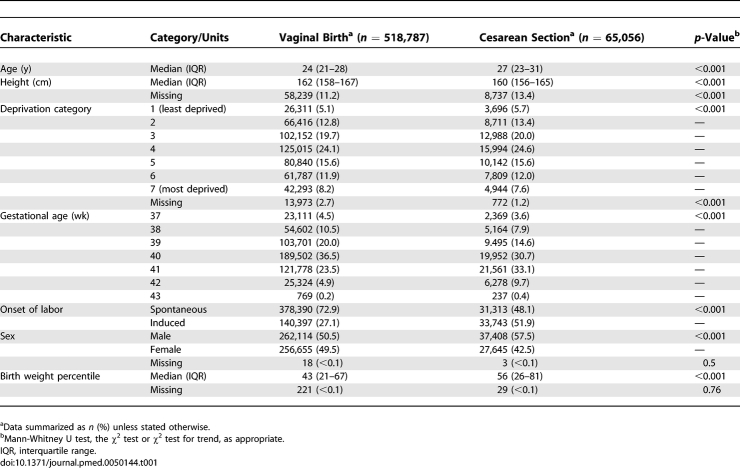
There were 1,531,261 available records from the Scottish Morbidity Record over the period from 1980 to 2005. Among these, there were 8,111 stillbirths (0.5%), 72,119 noncephalic births (4.7%), 851,486 multiparous women (55.6%), 89,964 preterm births (5.9%), 91,904 elective cesarean deliveries (6.0%), 40,224 prelabor emergency cesarean deliveries (2.6%), 510 with missing data on mode of delivery (<0.1%), and 478 with missing data on method of induction of labor (<0.1%). A total of 947,414 women had one or more of these exclusions leaving a main study group of 583,847 nulliparous women delivering a liveborn infant at term in a cephalic presentation, which was 86% of all nulliparous women in the database. The characteristics of the study group are described in relation to whether the women were delivered by emergency cesarean section (Table 1). This latter group was older, shorter, and likely to live in an area of low socioeconomic deprivation. They delivered at later weeks of gestation, were more likely to have an induced labor, more likely to deliver a male infant, and the birth weight percentile of their infants was higher. A total of 81,407 (13.9%) records had missing data for one or more of height, birth weight percentile, or deprivation category.
Table 1.
Demographic and Outcome Characteristics of Eligible Nulliparous in Relation to Mode of Delivery
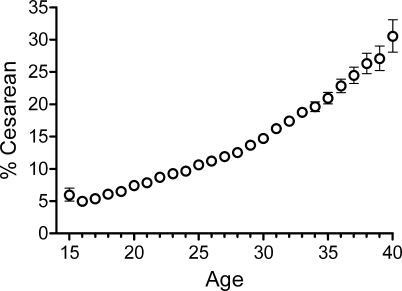
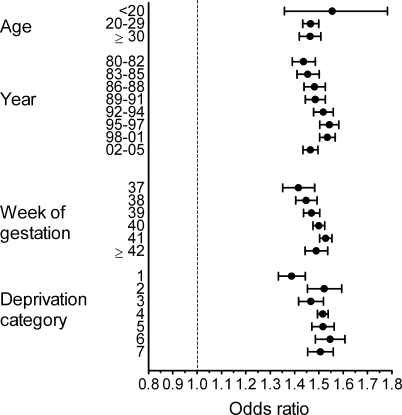
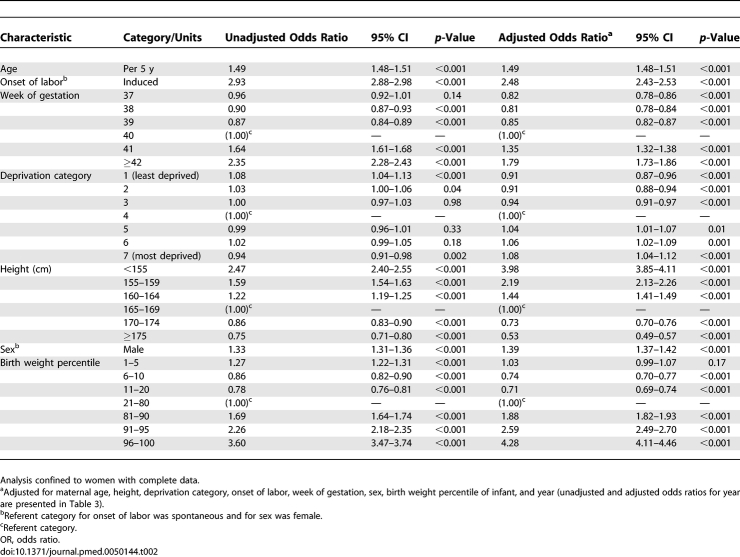
Age and Cesarean Risk
The risk of cesarean delivery increased progressively from 16 y of age (Figure 1). The proportional increase in risk for a 5-y increase in age was similar comparing women <20 y, those aged 20–29 y, and those aged ≥30 y (Figure 2). The linearity of the relationship between age and risk of cesarean was further assessed using fractional polynomials. None of eight polynomial expressions tested provided a better fit than a simple linear model. The odds ratio for a 5-y increase in age was 1.51 (95% confidence interval [CI], 1.50–1.53) and was 1.49 (95% CI, 1.48–1.51) when confined to records with no missing data. Adjusting for a series of maternal and obstetric characteristics (Table 2) was without effect. When the covariate data were expressed continuously and nonlinear terms selected using multiple fractional polynomials, the odds ratio for a 5-y increase in age was 1.52 (95% CI, 1.51–1.54), which was very similar to the odds ratio obtained when the continuous variables were categorized. There were statistically significant interactions between age and week of gestation, socioeconomic deprivation, and year (all p < 0.01), and these are illustrated in a stratified analysis (Figure 2). This analysis demonstrates that the degree of variation between strata of these variables was relatively minor, and the statistical significance of the interaction terms reflects the large sample size.
Figure 1. Maternal Age and the Risk of Cesarean Delivery.
Proportion of women being delivered by emergency intrapartum cesarean section in relation to age of mother (n = 583,847). Bars are binomial 95% CIs.
Figure 2. Stratified Analysis of Maternal Age and Risk of Cesarean Section.
Adjusted odds ratio for a 5-y increase in maternal age (bars are 95% CIs) stratified by maternal age, year of delivery, week of gestation, and deprivation category. Interactions were statistically significant for year of delivery (p < 0.001), week of gestation (p = 0.002), and deprivation category (p = 0.002) using the likelihood ratio test. Odds ratios are adjusted for maternal age, height, deprivation category, onset of labor, week of gestation, sex, birth weight percentile of infant, and year. The vertical dashed line indicates unity.
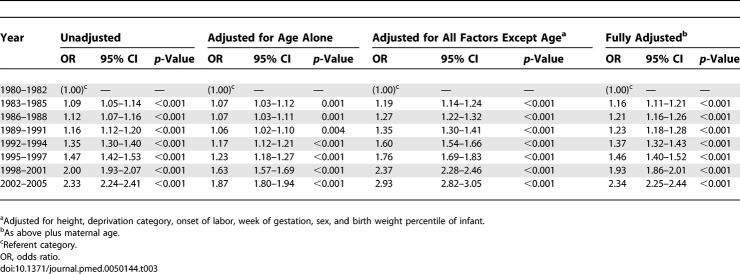
Table 2.
Unadjusted and Adjusted Odds Ratios for Intrapartum Cesarean Section among Nulliparous Women, Scotland 1980–2005
Information on body mass index was available for a previously described subset of the cohort [15]. Among the 72,137 of these women who fulfilled the inclusion criteria for the main cohort and who had complete data, the odds ratio for a 5-y increase in age was 1.52 (95% CI, 1.49–1.55) adjusted for the same characteristics as the present analysis and was 1.48 (95% CI, 1.44–1.51) when also adjusted for body mass index. The database employed lacked details on the indication for cesarean delivery. However, we performed a subgroup analysis where we compared the strength of association between maternal age and the risk of emergency intrapartum cesarean section in relation to whether the baby had a 5-min Apgar score of <7. The adjusted odds ratio for a 5-y increase in maternal age was 1.52 (95% CI, 1.50–1.54) for cesarean delivery with a normal Apgar score and 1.30 (95% CI, 1.22–1.38) for cesarean delivery with a low Apgar score.
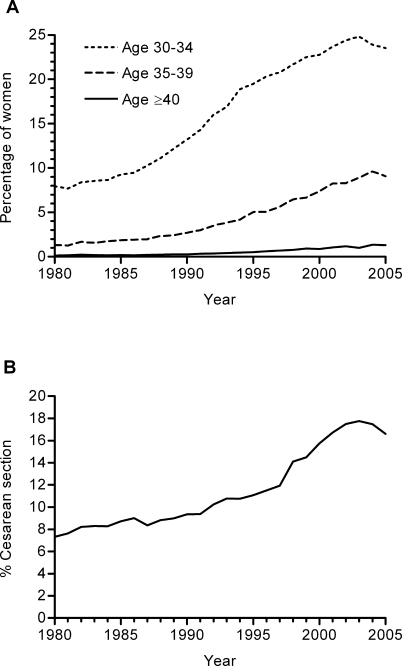
Population Trends, 1980–2005
Over the period from 1980 to 2005, the proportion of women having their first birth aged 30–34 y increased approximately 3-fold, the proportion aged 35–39 y increased approximately 7-fold, and the proportion aged ≥40 y increased approximately 10-fold (Figure 3A). Over the same period of time, the rate of cesarean delivery more than doubled (Figure 3B). Adjustment for age significantly reduced the strength of the association between year of delivery and the risk of cesarean delivery, both when analyzing year alone and when included with all other covariates (Table 3). Over the period 1981–2005, there were 16,548 more cesarean deliveries than would have occurred had the rate stayed the same as it was in 1980. Of these additional procedures, it was estimated that 37.6% would not have been performed had the maternal age distribution remained constant. The figure was very similar when adjusted for all other maternal characteristics (37.8%) and all other maternal characteristics plus statistically significant interactions (38.7%).
Figure 3. Time Trends in Maternal Age Distribution and Cesarean Section Rates in Scotland between 1980 and 2005.
(A) Proportion of women per year delivering within the age ranges 30–34, 35–39, and ≥40 y.
(B) Proportion of women per year delivered by emergency cesarean section.
Table 3.
Effect of Adjusting for Age on the Association between Year of Delivery and the Risk of Emergency Intrapartum Cesarean Section among Nulliparous Women, Scotland 1980–2005
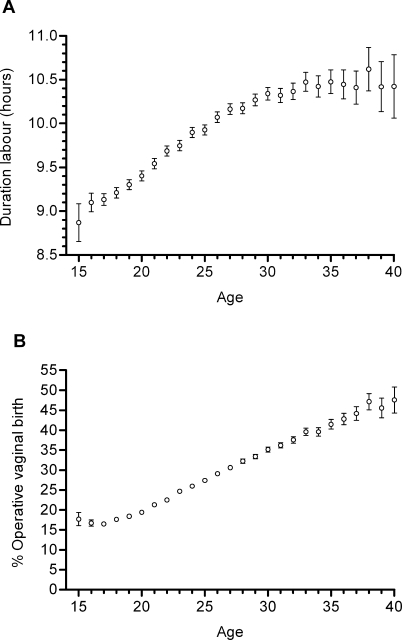
Duration of Labor and Operative Vaginal Birth
The average duration of spontaneous labor progressively increased from aged 16 y upwards (Figure 4A). The association appeared to plateau around 35 y of age and above. Between the ages of 16 and 30 y, a 5-y increase in age was associated with a 0.49 h longer duration of labor (95% CI, 0.46–0.51). The risk of operative vaginal birth also increased linearly with age (Figure 4B). The odds ratio for a 5-y increase in age, adjusted for the same factors as employed in the multivariate analysis described in Table 2, was 1.49 (95% CI, 1.48–1.50).
Figure 4. Maternal Age and the Duration of Labor and Risk of Operative Vaginal Birth.
(A) Mean duration of spontaneous labor in relation to maternal age (n = 409,703). Bars are 95% CIs of the mean.
(B) Proportion of nulliparous women who required operative vaginal delivery in relation to maternal age among the 518,787 women delivered by a means other than emergency cesarean section. Bars are binomial 95% CIs.
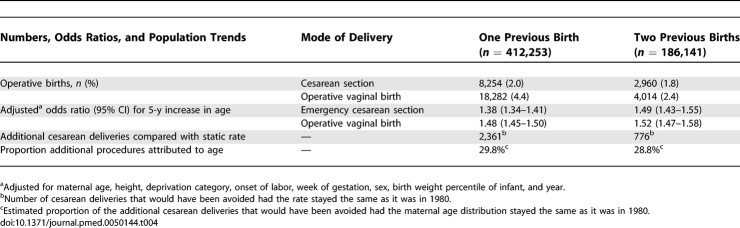
Multiparous Women
We then examined the relationship between maternal age and the risk of emergency cesarean section in multiparous women, analyzing women who had either one or two previous vaginal births but who otherwise fulfilled the inclusion criteria for the main study group (Table 4). All women who had a previous cesarean delivery were excluded. The odds ratio for intrapartum cesarean delivery associated with a 5-y increase in maternal age and adjusted for the same series of maternal characteristics as above was 1.38 (95% CI, 1.34–1.41) among women with one previous vaginal birth and 1.49 (95% CI, 1.43–1.55) among women with two previous vaginal births. The adjusted odds ratios for operative vaginal birth associated with a 5-y increase in maternal age were 1.48 (95% CI, 1.45–1.50) and 1.52 (95% CI, 1.47–1.58), respectively. Approximately 30% of the increase in cesarean section rate among multiparous women was related to increasing maternal age.
Table 4.
Outcome of Labor among Multiparous Women, Scotland 1980–2005
Age and Myometrial Contractility
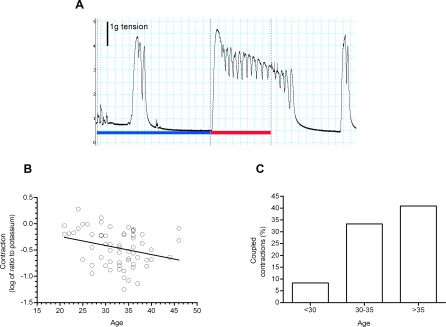
Myometrial biopsies were obtained from 62 women of varying parity, and a total of 181 strips were studied in vitro. The average number of strips studied per woman was 2.9 and the range 2–4. The characteristics of this group are summarized in Table 5. Figure 5A illustrates estimation of contraction units and shows an example of a multiphasic contraction in a biopsy from a 40-y-old woman. The mean peak response to potassium was 3.5 g tension, and there was no association between the age of the mother and the peak response to potassium (coefficient for a 5-y increase in age = 0.15 g tension, 95% CI, −0.12 to 0.43, p = 0.27).
Table 5.
Characteristics of Women Who Provided Myometrial Biopsies
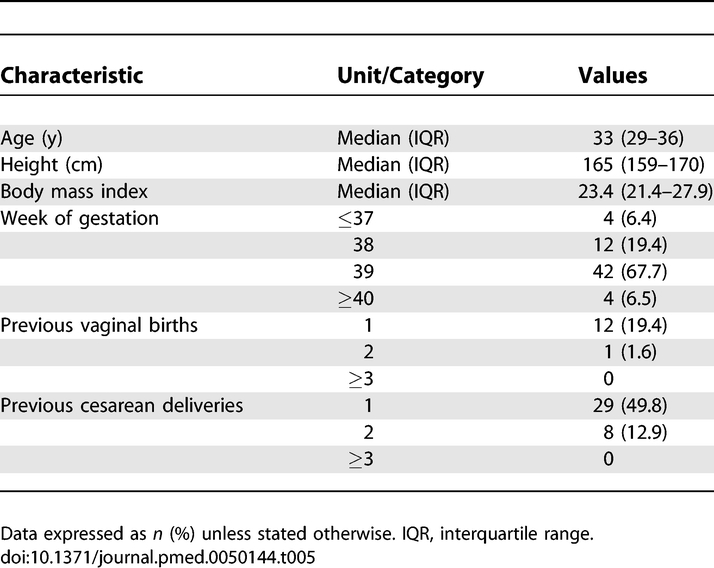
Figure 5. Myometrial Contractility in Relation to Maternal Age.
(A) Trace of isometric tension from myometrial strip obtained from a 40-y-old woman being delivered by planned cesarean section. The blue line represents the 15 min before addition of potassium, and the red line 7 min in the presence of 50 mM of potassium. The area under the curve is the space between the tension trace and the baseline, indicated by the blue and red lines. The log10 of the ratio of these two areas is the contraction unit. The spontaneous contraction before the addition of potassium and the contraction following potassium being washed out are both multiphasic.
(B) Mean spontaneous contractile activity (quantified as contraction units) of isolated strips of myometrium obtained from women (n = 62) at the time of planned cesarean section in relation to the age of the donor. Regression line: y = 0.1078 + (−0.0174 × age); 95% CI for slope, −0.0326 to −0.0022.
(C) Proportion of spontaneous contractions that were multiphasic in relation to maternal age (n = 62, 181 samples). See text for regression analysis of (B) and (C).
Of the 181 strips, 67 (37.0%) exhibited one or more spontaneous contractions prior to potassium stimulation. There was a nonsignificant trend towards a decreased frequency of spontaneous contraction with advancing age (change in contraction frequency for a 5-y increase in age = −26.4%, 95% CI, −50.9% to 10.2%, p = 0.14). When expressed as contraction units, the mean spontaneous activity was −0.49 contraction units and the standard deviation 0.44. The mean contraction unit value for each patient is plotted against maternal age (Figure 5B). Regression modeling demonstrated a significant negative association between spontaneous contractile activity and maternal age, with a coefficient of −0.086 contraction units for a 5-y increase in age (95% CI, −0.161 to −0.012, p = 0.02). Spontaneous activity increased with advancing gestational age (coefficient for one week increase = 0.10; 95% CI, 0.01–0.18, p = 0.04) and number of previous vaginal births (coefficient for each additional vaginal birth = 0.17; 95% CI, −0.01 to 0.34, p = 0.07). However, adjustment for these factors and other maternal characteristics (number of previous cesarean deliveries, height, and body mass index) had virtually no effect on the association between age and spontaneous activity (adjusted coefficient for 5-y increase in age = −0.084, 95% CI, −0.155 to −0.012, p = 0.02). When the analysis was confined to the 67 strips that exhibited at least one spontaneous contraction, there was still a statistically significant decrease in contractility with advancing age (coefficient of −0.080 contraction units for a 5-y increase in age, 95% CI, −0.149 to −0.009, p = 0.03). The risk of these spontaneous contractions being multiphasic also increased with advancing maternal age (Figure 5C). A 5-y increase in age was associated with an odds ratio for multiphasic contractions of 1.93 (95% CI, 1.41–2.63, p < 0.001). This odds ratio was also virtually unaltered by adjusting for maternal characteristics (adjusted odds ratio 1.95, 95% CI, 1.43–2.64, p < 0.001), and age was the only maternal characteristic associated with multiphasic contractions.
Discussion
We show that the risk of intrapartum cesarean delivery among women having their first birth at term increased with advancing maternal age from 16 y old upwards. The association was linear and was not explained by a range of other maternal characteristics. Over the period 1980 to 2005, the proportion of women in Scotland having their first birth aged 30–34 y increased approximately 3-fold, the proportion aged 35–39 y increased approximately 7-fold, and the proportion aged ≥40 y increased approximately 10-fold (Figure 3B). The cesarean rate more than doubled over the same period. This increase represented approximately 16,500 more procedures than would have occurred had the cesarean rate stayed at the level observed in 1980. Using these nationally collected data, we estimated that approximately 38% of these additional procedures would have been avoided had the maternal age distribution stayed the same as in 1980. Hence, we show that a substantial proportion of the increase in rate of emergency primary cesarean delivery in recent years may be attributed to the trend of delaying of first childbirth. The current observations cannot be explained by the offer of planned cesarean delivery to older women.
Previous studies addressing the effects of population trends in delaying childbirth on cesarean delivery rates had produced inconsistent findings. An analysis of US birth certificate data from 1991 to 2002 concluded that increasing rates of cesarean delivery were unrelated to maternal risk profiles [12]. A recent study of 432,327 singleton cephalic births at term in Western Australia reached the same conclusion [10]. However, an earlier study of 225,466 births in Washington State estimated that 18% of the increase in cesarean rates between 1970 and 1987–1990 might be explained by the combined effects of changes in maternal age, parity, and birth weight [11], and an analysis of 127,564 births between 1988 and 2000 in Nova Scotia suggested that virtually all of the increase in cesarean rates over that period could be attributed to changes in age, parity, and maternal weight [3]. The strengths of the present analysis are that we studied a large number of women, that we had quality assured data collected in a standardized fashion, that data were nationally collected covering a population with free access to health care, and that we could exclude prelabor cesarean deliveries. Moreover, the analytic method employed directly addressed the question of what would have been predicted had the age distribution remained constant. The analysis also indicates that part of the increase in cesarean rates was independent of changes in maternal age. Other possible determinants of increased rates of cesarean delivery may include changes in other maternal characteristics, such as body mass index, or changes in obstetric practice, such as generally more liberal use of cesarean section.
Some authors had interpreted higher rates of cesarean delivery among older women as reflecting physician and maternal preference. We interpret the current data as supporting a biological effect of aging on performance during labor. First, we adjusted for a range of maternal characteristics. The lack of effect of statistical adjustment for both body mass index and birth weight percentile suggest the findings are not explained by comorbidities, such as obesity or gestational diabetes. Secondly, previous analysis by indication for cesarean delivery demonstrated that 80% of procedures performed during term labor in nulliparous women include failure to progress in the indication [16]. This finding suggests that any factor that is strongly associated with primary intrapartum cesarean delivery among nulliparous women at term is likely to be associated with poor progress during labor. Thirdly, we found that other indicators of poor progress in labor were also associated with increasing age. The duration of labor increased linearly with advancing age, as did the risk of requiring operative vaginal delivery. The latter observation also indicates that the association between age and cesarean delivery is not merely a reflection of a tendency toward performing a cesarean delivery rather than an operative vaginal birth in older women. Finally, the associations were all strikingly linear across the maternal age range 20–29 y. This pattern cannot plausibly be explained either by bias on the part of the obstetrician or a tendency to vascular complications affecting older women. We also found that the association was stronger for procedures performed where the infant had a normal Apgar score than procedures where the infant was delivered with a depressed Apgar, indicating that the association is unlikely to be explained by effects of aging on the risk of fetal distress, other than as a consequence of prolonged labor.
Given these findings, we hypothesized that aging is associated with impairment of myometrial contractility. We tested this hypothesis by obtaining uterine biopsies at the time of planned cesarean section and assessing their contractility in vitro. We quantified spontaneous contractile activity blind to the age of the donor. We found that advancing age was associated with a reduced degree of spontaneous contraction compared with a standardized response to potassium. Moreover, the spontaneous contractions observed were more likely to be multiphasic. Our contractility studies included women of mixed parity. However, we demonstrated that the association between maternal age and the risk of both cesarean section and operative vaginal birth was similar in multiparous women as we observed in nulliparous women. Moreover, multivariate statistical methods demonstrated that the association between age and the contractility of isolated myometrial strips was independent of other maternal characteristics. The association between age and both spontaneous activity and the coordination of contractions may indicate adverse effects of aging on control of electrical activity in the myometrium, for example, membrane depolarization or conduction between cells, which could be mediated by effects of aging on the composition of the uterine wall, such as increasing connective tissue between muscle bundles. Alternatively, it could be mediated at the cellular level, such as effects of aging on gap junction or ion channel expression. Further studies will be required to define further the extent of this functional impairment and its molecular basis. Whatever the case, these observations suggest that the increased risk of operative delivery associated with advancing maternal age may be a manifestation of impaired uterine function, which is consistent with the overall importance of poor progress in labor as an indication for cesarean delivery [17]. There are also specific findings that are consistent with an association, for example the observation that the presence of multiphasic (also called “coupled”) contractions during labor among nulliparous women monitored with intra-uterine pressure catheters was associated with prolonged labor and an increased risk of emergency cesarean delivery [18].
We propose that an association between advancing age and impaired uterine function is biologically plausible. Women who delay childbirth using the combined oral contraceptive pill, barrier methods, nonhormonal intra-uterine devices, or sexual abstinence (which collectively constitute the majority of women), will have repetitive cyclical stimulation by estrogens and progestogens. Myometrium expresses both estrogen and progesterone receptors and these hormones have profound effects on myometrial growth, metabolism, and contractility (see review [19]). We hypothesize that the adverse effect of advancing maternal age on myometrial contractility may be a consequence of this prolonged cyclical stimulation of the myometrium by estrogen and progesterone. This hypothesis is falsifiable, as it predicts that early menarche would be independently predictive of the risk of dysfunctional labor. If this hypothesis is true, it may be that the effect of delaying childbirth on the outcome of labor varies according to the method of contraception used, which could be of clinical and public health relevance. Whatever the case, understanding the determinants and management of dysfunctional labor in older women is central to designing strategies for reducing population cesarean delivery rates without adversely affecting maternal and infant outcomes.
Abbreviations
- CI
confidence interval
Footnotes
Author contributions. GCSS had full access to all of the data in the study, takes responsibility for the integrity of the data, the accuracy of the data analysis, and is the guarantor. GCSS formed the hypothesis. MF performed the linkage and extracted the population data. GCSS and IRW performed the statistical analysis. GCSS and YC designed the contractility studies. YC, DP, and HML recruited patients, conducted the contractility studies, and extracted data. GCSS drafted the paper. GCSS, YC, IRW, DP, HML, JPP, DSCJ, and MF critically reviewed the draft for content and approved the final version of the paper.
Funding: This work was funded by the Evelyn Trust and by the Cambridge National Institute for Health Research (NIHR) Biomedical Research Centre. DP was funded by an MRC Clinical Training Fellowship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist.
References
- Ecker JL, Frigoletto FD., Jr. Cesarean delivery and the risk-benefit calculus. N Engl J Med. 2007;356:885–888. doi: 10.1056/NEJMp068290. [DOI] [PubMed] [Google Scholar]
- Guihard P, Blondel B. Trends in risk factors for caesarean sections in France between 1981 and 1995: lessons for reducing the rates in the future. BJOG. 2001;108:48–55. doi: 10.1111/j.1471-0528.2001.00009.x. [DOI] [PubMed] [Google Scholar]
- Joseph KS, Young DC, Dodds L, O'Connell CM, Allen VM, et al. Changes in maternal characteristics and obstetric practice and recent increases in primary cesarean delivery. Obstet Gynecol. 2003;102:791–800. doi: 10.1016/s0029-7844(03)00620-3. [DOI] [PubMed] [Google Scholar]
- Lee SI, Khang YH, Yun S, Jo MW. Rising rates, changing relationships: caesarean section and its correlates in South Korea, 1988–2000. BJOG. 2005;112:810–819. doi: 10.1111/j.1471-0528.2004.00535.x. [DOI] [PubMed] [Google Scholar]
- Rietberg CC, Elferink-Stinkens PM, Visser GH. The effect of the Term Breech Trial on medical intervention behaviour and neonatal outcome in The Netherlands: an analysis of 35,453 term breech infants. BJOG. 2005;112:205–209. doi: 10.1111/j.1471-0528.2004.00317.x. [DOI] [PubMed] [Google Scholar]
- Main DM, Main EK, Moore DH. The relationship between maternal age and uterine dysfunction: a continuous effect throughout reproductive life. Am J Obstet Gynecol. 2000;182:1312–1320. doi: 10.1067/mob.2000.106249. [DOI] [PubMed] [Google Scholar]
- Adashek JA, Peaceman AM, Lopez-Zeno JA, Minogue JP, Socol ML. Factors contributing to the increased cesarean birth rate in older parturient women. Am J Obstet Gynecol. 1993;169:936–940. doi: 10.1016/0002-9378(93)90030-m. [DOI] [PubMed] [Google Scholar]
- Gareen IF, Morgenstern H, Greenland S, Gifford DS. Explaining the association of maternal age with Cesarean delivery for nulliparous and parous women. J Clin Epidemiol. 2003;56:1100–1110. doi: 10.1016/s0895-4356(03)00199-9. [DOI] [PubMed] [Google Scholar]
- Bell JS, Campbell DM, Graham WJ, Penney GC, Ryan M, et al. Do obstetric complications explain high caesarean section rates among women over 30? A retrospective analysis. BMJ. 2001;322:894–895. doi: 10.1136/bmj.322.7291.894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary CM, de Klerk N, Keogh J, Pennell C, de Groot J, et al. Trends in mode of delivery during 1984–2003: can they be explained by pregnancy and delivery complications. BJOG. 2007;114:855–864. doi: 10.1111/j.1471-0528.2007.01307.x. [DOI] [PubMed] [Google Scholar]
- Parrish KM, Holt VL, Easterling TR, Connell FA, LoGerfo JP. Effects of changes in maternal age, parity and birth weight distribution on primary Cesarean section rates. JAMA. 1994;271:443–447. [PubMed] [Google Scholar]
- Declercq E, Menacker F, Macdorman M. Maternal risk profiles and the primary cesarean rate in the United States, 1991–2002. Am J Public Health. 2006;96:867–872. doi: 10.2105/AJPH.2004.052381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole S. Scottish maternity and neonatal records. 8th Study Group of the Royal College of Obstetricians and Gynaecologists. 1980. pp. 39–52.
- Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley and Sons; 2000. [Google Scholar]
- Smith GCS, Wood AM, Pell JP, White IR, Crossley JA, et al. Second-trimester maternal serum levels of alpha-fetoprotein and the subsequent risk of sudden infant death syndrome. N Engl J Med. 2004;351:978–986. doi: 10.1056/NEJMoa040963. [DOI] [PubMed] [Google Scholar]
- Ecker JL, Chen KT, Cohen AP, Riley LE, Lieberman ES. Increased risk of cesarean delivery with advancing maternal age: indications and associated factors in nulliparous women. Am J Obstet Gynecol. 2001;185:883–887. doi: 10.1067/mob.2001.117364. [DOI] [PubMed] [Google Scholar]
- Macara LM, Murphy KW. The contribution of dystocia to the cesarean section rate. Am J Obstet Gynecol. 1994;171:71–77. doi: 10.1016/s0002-9378(94)70080-x. [DOI] [PubMed] [Google Scholar]
- Ferreira CJ, Odendaal HJ. Does coupling of uterine contractions reflect uterine dysfunction. S Afr Med J. 1994;84:20–23. [PubMed] [Google Scholar]
- Hertelendy F, Zakar T. Regulation of myometrial smooth muscle functions. Curr Pharm Des. 2004;10:2499–2517. doi: 10.2174/1381612043383926. [DOI] [PubMed] [Google Scholar]