Abstract
Improving the health of urban residents, particularly those living in slum areas, requires an integrated approach. Appropriate interventions must be based on a well-grounded understanding of health determinants. Social factors are as important as physical factors in determining health status and suggest alternative interventions. Employment, stress, social exclusion, social support, substance use, nutrition, transport, and conditions during childhood are among the most important social determinants of health status identified by the International Center for Health and Society. This paper uses social determinants of health approach to understand morbidity outcomes for people residing in the slums of Surat City, India. To quantify suboptimal health behavior and identify the determinants of health status for this population survey data on household characteristics, health-seeking behavior, socioeconomic status, food and personal habits, social life, and physical activity has been used. After controlling for socioeconomic and demographic factors, logistic regression analysis reveals that social exclusion, stress, and lack of social support are significantly associated with morbidity. Thus, understanding of social determinants of health by policy makers is important as the health sector has a crucial role in addressing disparities in social determinants.
Keywords: Social determinants, Suboptimal behavior, Morbidity, Urban slums of India
Introduction
Surat, an industrial hub of Gujarat state, India, has experienced population growth due to its world famous textile and diamond industries and slums, slum-like areas, and squatter settlements have been developed to accomodate the growth. Poor sanitation and dense population, coupled with suboptimal health behaviors, pose a high risk of infections for the urban slum inhabitants, but not for their wealthier urban neighbors and rural residents.1 Furthermore, heterogeneity of slum dwellers, lack of common meeting areas, fewer extended family connections, and women engaged in work outside homes, affects flow of information about health services and facilities.2 It is only recently that the National Urban Renewal Mission has talked about the plight of this community, and improving their health status requires a frontal, focused, and integrated strategy.
International Centre for Health and Society, London has developed ten types of the social determinants of health (SDOH): social gradient, employment, stress, early life, social exclusion, work, social support, substance use, food, and transport. These directly impact health, are excellent predictors of individual and population health, structure lifestyle choices, and interact with each other to affect health.3 The World Health Organization established the Commission on Social Determinants of Health (CSDH), on the premise that action on SDH is the fairest and most effective way to improve health for all people and reduce inequalities. Central to the Commission’s remit is the promotion of health equity, defined as “the absence of disparities in health (and in its key social determinants) that are systematically associated with social advantage/disadvantage.”4
Research on the impact of social environment on health, as represented by social inequalities in health, is inadequate. Also, social environment is not inchoate and amorphous, but are characterizable and their separate effects on health observable.5 For instance, recent epidemiological surveys in urban slum populations in India in the cities of Delhi,6,7 Pune,8 Chennai,6 Lucknow,9 and Mumbai (Parikh et al. 1996, unpublished data) reported high general and reproductive morbidities, mainly among school-going children and those less than 3 years of age. There is a paucity of studies among the urban slum inhabitants which examine the entire ambit of social determinants and morbidity status. Understanding the importance of social determinants of health by policy makers and bureaucrats in local self-governments is vital as the health sector has a crucial role in addressing disparities in social determinants.
Surat has witnessed one of the largest labor immigration in recent years in India due to rapid industrialization and therefore we felt that a study on the level of social determinants and the suboptimal health behavior of urban slum dwellers with their relative contributions on self reported morbidity would be appropriate at this location.
Materials and Methods
Study Setting and Design
Sample Size (n) from Precision of Cross-Sectional Morbidity Prevalence Rates in Proportion (P)
Without replacement simple random sampling (SRS), the respondent sample size (n) needed to achieve precision as measured by a 95% margin of error (MOE) in estimating a morbidity prevalence rate (expressible as a proportion, P) for a population of size N is,
 |
1 |
where
 |
2 |
For a cluster sample with design effect (Deff), the SRS sample size from Eq. 1 must be multiplied by a factor of Deff. Based on earlier research, we assumed that Deff = 2.00 was a reasonable upper bound for the study.
The study is designed to produce estimates for the slum population in Surat city that are computed at the aggregate level and should have a 95% margin of error of 6 percentage points or less for morbidity prevalence rates of 40%.
To achieve the above outlined requirements, a study needs at least 512 households. This sample is further subject to nonresponse rates, which are assumed to be 5% in the study area. Therefore, we arrived at an estimated target sample size of around 540 households with completed interviews of one respondent per household.
Survey Design
The study target population was defined as all households living in Surat city who consider the household to be their primary place of residence.
The sample for the study is selected using a multistage geographically clustered design to ensure adequate coverage of the entire target population while simultaneously minimizing data collection costs. Costs are reduced because the geographic clustering of the sample design will minimize the travel needed for interviewers to visit each selected household. In summary, this sample selection process is as follows.
The first stage of the design involved allocating the number of households with probability propositional to size (PPS) within each geographic area. This selection process is highly dependent of the geography of Surat. The city is currently divided into seven administrative zones for which suitable data on slum households is available. This facilitated the allocation of number of households in each administrative zone of Surat city with PPS. In the next stage, households within each administrative zone were randomly selected with equal probability and without-replacement using a systematic sample selection so as to achieve a self weighting sample of households within each zone, giving every household in the zone the same chance of being included in the survey. After a listed address was selected and confirmed to be a resident household, the interviewer visited the household and created a roster of all survey-eligible individuals (males or females) who consider the household to be their primary place of residence. Finally, Kish’s Table was used by the interviewer to select one eligible individual from within the selected household. These individuals answered the study questionnaire. The geographic location of the slum dwellings was identified by means of a sketch map that was drawn including the streets, plots and other significant identifiers to identify the selected household. Each selected household was assigned a unique study number.
The survey succeeded in achieving a high overall response rate of 96%. Nonresponse at the household level was primarily due to respondents not being at home despite repeated household visits. Very few respondents refused to be interviewed. Data was collected successfully from 518 slum households. All the interviews were conducted in privacy after obtaining consent from the selected respondents.
All of the 13 investigators employed for the study were the graduate medical doctors who were posted in the Department of Community Medicine during their final year of compulsory rotatory housemanship program. They were trained in the administration of questionnaires consisting of questions related to social determinants of health and a household proforma in a 3-day training programme. A pilot study was also carried out among 25 respondents with cross sections of various subgroups such as age and gender to test the appropriateness of the questionnaire and make necessary modifications in the questionnaire. The results were utilized to know whether the scores were correlated with individual variables in order to test the appropriateness of the indices of social determinants developed by us.
Data Analysis
The analysis ran in two fold. First, analysis concerned with the association between demographic factors, socioeconomic factors, and social determinants. Significant predictors of social determinants were identified using multiple regression analyses. Then, we used conditional logistic regression analyses to evaluate the independent influences of social determinants, and suboptimal behavior on self-reported morbidity after controlling the socioeconomic and demographic factors. We evaluated the results by likelihood ratio tests and presented them as odds ratios with 95% confidence intervals. A backward stepwise method of elimination with the level of significance set at less than 0.10 is used for variable retention. Data was analyzed by using SPSS version 14.0 for Windows.
Scores of Social Determinants and Suboptimal Health Behavior
We have developed scores of various social determinants, suboptimal health behavior, and morbidity due to selected diseases. Social gradient score was derived by adding the standard of living index score to the socioeconomic class (Kuppuswami classification) score as standardized for use in India. Standard of living index is estimated by assigning weightage for the responses to the questions related to housing, environment, and durable goods possessed. A higher social gradient score implies favorable outcome on the part of the household. However, all the other scores, on higher side, are unfavorable for the households. Employment score is derived by asking various questions related to current work status, loss of employment in the past, reason(s) for the loss of employment, and stress due to the loss of employment. Work score deals with the issue of control over the work at home and workplace and the stress experienced by the respondents and the husband (in case respondent is a woman). Social exclusion score is derived by asking questions related to migration such as their native state of residence, years after migration, local language (Gujarati) proficiency, reasons for leaving their home state, and discrimination faced in the society due to their migrant status. Social support score deals with social network and the sort of help received by them while experiencing difficult situations. Stress score deals with their subjective feelings of stress in their domestic life, relations with neighbors and experience of domestic violence among women respondents. Early life score is based on financial and educational backgrounds of their parents during the childhood of the respondents and spouse; questions on major illness during childhood; and, experiences of physical/sexual abuse during childhood. Food score is derived by asking questions on their habits related to eating foodstuffs by the roadside vendors consumption of fruits, vegetables, sweets, fried food, and salty food. Tobacco and alcohol habits related history gives the estimate of the addiction score. Transport score includes questions on their modes of transportation, extent of physical activity required to reach workplace, and social contact.
Suboptimal health behavior includes questions on practices pertaining to safe water consumption, prevention of mosquito born diseases, contraception, place of delivery, breast feeding patterns, immunization status of children, and management of diarrhea. Morbidity score is designed by adding history of water-born diseases in the past 12 months, fever/malaria cases in past 12 months, attacks of pneumonia in five children in the past 12 months, presence of any major illness like tuberculosis, leprosy, hypertension, diabetes mellitus, coronary heart disease, congenital heart disease, and cancer among any of the family members. Apart from these major illnesses, history of any complications during pregnancy, delivery, and within 6 weeks of delivery, road traffic accidents, schizophrenia, and depression are also included while construing morbidity score. Logistic regression analysis was used to predict the relative influences of these indices on the morbidity status across various subgroups of slum population.
Working Hypotheses
The primary hypothesis is that the households with poor socioeconomic and demographic condition are more likely to experience higher levels of morbidity. The secondary hypothesis is that the social determinant scores and suboptimal health behavior will modify this relationship.
Results and Discussion
Morbidity Status vs. Socioeconomic and Demographic Factors
Morbidity status is a dichotomous variable defined as at least one self reported major illness or morbid condition such as tuberculosis, leprosy, hypertension, diabetes mellitus, coronary heart disease, congenital heart disease, cancer, history of any complication during pregnancy, complication during delivery, or complication within 6 weeks of delivery in the past 12 months from a household head or his or her spouse. To understand the influences of social determinants on morbidity status, first we analyzed the morbidity pattern among various socioeconomic and demographic subgroups and controlled their significant contributions on morbidity in the later stage of the analysis.
Social Determinants and Morbidity Status
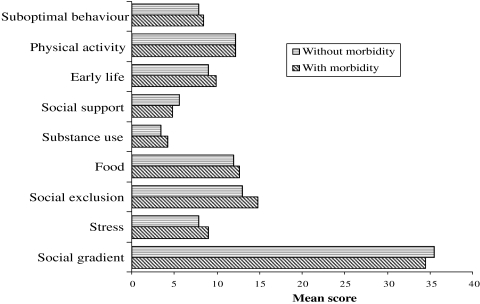
The levels of social determinants are considerably varied by self reported morbidity status of a household head or his or her spouse. Figure 1 explores the mean scores of various social determinants between the households with and without self reported morbidity. Mean score of stress, social exclusion, social support, and substance use are smaller among the households without any morbidity condition. Suboptimal behavior and social gradient mean scores are larger among the same group.
FIGURE 1.
Mean sources of social determinants by morbidity status.
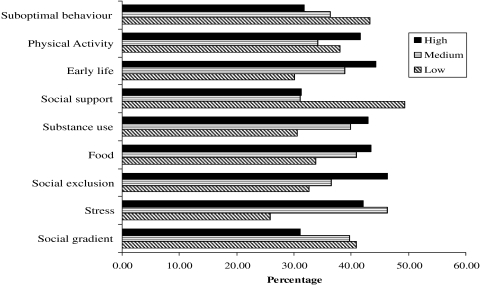
Figure 2 reports the prevalence of morbidity by social determinants. For this purpose, all the social determinants scores are categorized into low, medium, and high depending on the scores calculated below 33.3, 33.3–66.7, and above 66.7 percentile points. Social gradient score, a proxy for socio-economic status of the households, is found to have positive influence on health. The households with low social gradient score have reported significantly higher morbidity levels (40.84%) than medium (39.53%) or higher (30.97%) social gradient score. These findings are well supported by earlier studies.10 A wealth of evidence from Canada and other countries supports the notion that the socioeconomic circumstances of individuals and groups are equally or more important to health status than medical care and personal health behaviors, such as smoking and eating patterns.11–13 In terms of the health of populations, it is well known that disparities—the size of the gap or inequality in social and economic status between groups within a given population—greatly affect the health status of the whole. The larger the gap, the lower the health status of the overall population.14,15 Societies with larger gradients in socioeconomic status are more likely to encounter developmental problems in disadvantaged children.16
FIGURE 2.
Prevalence of morbidity by social determinants and suboptimal behavior.
Apart from socioeconomic status, a list of potential causes of morbidity and mortality developed from epidemiological studies are attributable to substance use (alcohol, tobacco, and drug use)17 and food intake.18 There is also a great body of evidence that points to the inequalities in health having their origin early in life,19–22 in physical activity,23 social exclusion,24 social support,25 and psychosocial stress.26 The prevalence of morbidity in our study is found to be significantly higher among the households with high substance use (42.75%), food (43.24%), and early life (44.16%) scores. Socioeconomic status of parents during childhood and the way child is reared in the family has crucial impact on her/his physical, psychological, social, and emotional development.27
Social exclusion is a key factor influencing health and often exacerbated by gender, age, ability, sexual orientation, race, ethnicity, and religion. For example, women from racialized groups make up almost all of the workers in the garment industry that employs contingent workers in Canada’s low paying and often unsafe “sweat shops.”28 Research has found that those experiencing exclusion are more likely to experience higher rates of morbidity.29 Lack of social support, particularly from friends and family, is also considered a barrier to adherence and self-care, while high levels of support are related to better long-term management of health and health outcomes.30 In support of these findings, our study also demonstrates higher morbidity levels in high social exclusion (46.21%) and low social support (49.18%) categories.
Households engaged in low (37.85%) or high (41.41%) levels of physical activity have reported higher prevalence of morbidity than that of medium (34.09%) physical activity. Regular physical activity that is performed on most days of the week reduces the risk of developing or dying from some of the leading causes of illness and death.31 Research studies in India also show that a normal healthy individual with low or high level of physical activity is liable to encounter a risk of adult related diseases and maternal morbidity.32,33
It can be clearly observed that the households with high suboptimal behavior scores (43.07%) have higher prevalence of morbidity compared to medium (36.3%) or low (31.76%) suboptimal health behavior scores. It clearly explains the phenomena and supports the finding of many other studies6 on morbidity. Suboptimal health behavior can be seen as a disadvantage to one’s life, owing to its subsequent health risks on the part of individual. Most people in difficult living situations face more than one disadvantage. Shaw and colleagues argue that health inequalities are produced by the clustering of disadvantage—in opportunity, material circumstance, and behaviors related to health across people’s lives.34
Influences of Social Determinants and Suboptimal Health Behavior
To confirm the bivariate results obtained in Table 1 and Figures 1 and 2, two different conditional logistic regression models were fitted. The first model serves the first purpose of this research which is to examine the relative contributions of demographic determinants and socioeconomic factors to morbidity status. The second model predicts the significant social determinants and the role of suboptimal behavior after controlling the socioeconomic and demographic factors considered in the first model. In this study, full model (model II) explains more of morbidity than the first model (R2 0.247 versus 0.171).
TABLE 1.
Conditional logistic regression analysis predicting the influences on morbidity status
| Model I | Model II | |||||
|---|---|---|---|---|---|---|
| Exp(B) | 95% CI for exp (B) | Exp(B) | 95% CI for exp (B) | |||
| Lower | Upper | Lower | Upper | |||
| Intercept | 1.165 | 1.184 | ||||
| Age | 0.974** | 0.955 | 0.993 | 0.976* | 0.954 | 0.999 |
| Sex—female (male) | 1.343 | 0.834 | 2.165 | 1.363 | 0.813 | 2.283 |
| Religion—Hindu (non-Hindu) | 0.536* | 0.356 | 0.806 | 0.696 | 0.394 | 1.228 |
| Marital status—married (nonmarried) | 0.845 | 0.343 | 2.081 | 0.479 | 0.183 | 1.245 |
| Family type—nuclear (non-nuclear) | 2.800** | 1.609 | 4.873 | 2.505** | 1.538 | 4.078 |
| Caste—SCST (non-SCST) | 2.256** | 1.150 | 3.371 | 1.756* | 1.124 | 2.742 |
| Education (illiterate) | ||||||
| Primary school | 1.089 | 0.670 | 1.769 | NA | NA | NA |
| Middle school | 1.191 | 0.607 | 2.337 | NA | NA | NA |
| High school and above | 0.300** | 0.152 | 0.594 | NA | NA | NA |
| Employment (unemployed) | ||||||
| Employed by self | 0.993 | 0.405 | 2.436 | NA | NA | NA |
| Employed by someone | 0.770 | 0.331 | 1.793 | NA | NA | NA |
| Migration (nonmigrant) | ||||||
| Within state migrant | 2.234** | 1.253 | 3.984 | 1.872* | 1.070 | 3.276 |
| Interstate migrant | 2.447** | 1.497 | 3.998 | 2.369** | 1.486 | 3.776 |
| Standard of living (low) | ||||||
| Medium | 1.223 | 0.692 | 2.160 | NA | NA | NA |
| High | 0.444* | 0.235 | 0.838 | NA | NA | NA |
| Social determinants | ||||||
| Social gradient score | 0.969** | 0.942 | 0.997 | |||
| Stress score | 1.080* | 1.034 | 1.128 | |||
| Social exclusion score | 1.056* | 1.017 | 1.097 | |||
| Social support score | 0.879** | 0.820 | 0.943 | |||
| Early life score | 1.029 | 0.953 | 1.111 | |||
| Food score | 1.058 | 0.958 | 1.170 | |||
| Substance use score | 1.037 | 0.952 | 1.130 | |||
| Physical activity score | 1.092** | 1.020 | 1.169 | |||
| Suboptimal behavior score | 1.108** | 1.031 | 1.191 | |||
| R2 | 0.171 | 0.247 | ||||
| −2 Log likelihood | 615.505 | 579.132 | ||||
| N | 518 | 518 | ||||
Category within parenthesis represents the reference group. Dependent variable: currently with at least one major illness or morbid condition (0 no; 1 yes).
*p < 0.01
**p < 0.001
The most important determinants of morbidity in the first model are age, education, caste, family type, SLI, and migration status, as reported in many other studies. The relationship between morbidity and socioeconomic status is such that high school and above level of education (odds ratio = 0.30) and high SLI (odds ratio = 0.44) categories are associated with better health. The curve for age reveals the worst morbidity among young households. This can be explained in terms of smaller sample size in old age households. The shapes of the curves for family type, religion, as well as the categorical variable indicating migration status are coinciding with the previously reported findings from studies of health, morbidity, and mortality. The households belonging to non-nuclear families are 2.8 times more likely to report at least one major illness compared to nuclear families. Similarly, when compared to local residents, families migrated from within state (odds are 2.234) and the families from inter state migration (odds are 2.447) are more likely to report higher morbidity levels.
The total contribution of five significant variables in the first model is similar in the full morbidity model with social determinants, but the shapes of corresponding model terms differ considerably. It is the impact of social determinants that explains the model completely. Analysis reveals that after controlling the socioeconomic status and demographic variables along with all social determinant indices, suboptimal health behavior (odds = 1.108) of urban slum dwellers has a significant (p < 0.05) influence on the morbidity status. Morbidity status is also partially explained by the social determinants such as social gradient, stress, social exclusion, social support, and physical activity of the households. After controlling the other variables, multivariate model confirms the bivariate patterns seen in Figure 2. Every single unit increase in social gradient score decreases the odds of a household to be morbid by 0.97. After controlling for the socioeconomic and demographic factors, morbidity is significantly associated with increased social exclusion and social support and decreased physical activity. Stress is another important predictor explaining the morbidity condition. For every unit increase, stress is 1.08 times more likely to increase the self-reported morbidity of a household head or his/her spouse.
Conclusions
The prevalence of self reported morbidity in this study in urban slum settings is 37.5%. This prevalence is higher than previous estimates, although the conditions vary between studies conducted in various parts of India.35 Earlier studies had used recall periods of up to 5 years, and this feature may account for lower morbidity estimates than were found in this study. The main predictors of morbidity in the present study are demographic characteristics such as age, family type, caste, and education; social determinants scores such as social gradient, social exclusion, social support, stress, and physical activity; and suboptimal health behavior. Understanding of social determinants of health by policy makers and bureaucrats is important as the health sector has a crucial role in addressing disparities in social determinants. Countries as Finland and Sweden have incorporated equality-oriented action on the SDOH into their national policy agendas.3 In Canada, there are examples at the provincial and local level of successful policy and program changes that improve SDOH, the economy, and the labor market simultaneously.36
The Indian economy has witnessed excellent growth in recent years; however, the urban poor who have contributed the lion’s share in this success story have yet to benefit from its spoils. Surat Municipal Corporation (SMC) is committed to the welfare of the urban poor. The recent Indian National Urban Renewal Mission (NURM) aims to redress the hitherto neglected needs of the urban poor. Per se, no concrete policy or program exists to rebuild social cohesion in Surat city; efforts are ongoing from Gujaratis and the migrants alike to bring communal harmony and develop integrity. Diversity in culture, tradition, and customs is the hallmark of Indian society and traditionally people congregate to celebrate various festivals which help build up of social cohesion. There are social and caste specific groups, associations, and NGOs which promote social cohesion in Surat. Urban community halls have been constructed at various places in the city to provide a common platform for social festivities. Adopting a framework for social inclusion to guide the implementation of policies and practices that reduce inequities related to income, race, gender, ethnicity, geographic location, age, ability, and sexual orientation would be the key to tackle the issue of social exclusion.
The city of Surat has a unique primary health care infrastructure through a citywide network of 28 urban health centers and maternity centers, which could help modify suboptimal health behaviors among people, through a systematic health educational approaches; the theories of behavioral modifications, such as promoting increased physical activity and alleviating stress, two key determinants of morbidity in this study, need to be incorporated.
The health sector needs to champion policies that improve social conditions as areas of social and economic policy are largely beyond the purview of health departments. It has to “step on toes” and explore ways of intersectoral collaboration. The health sector has at least three key roles to play in addressing disparities in the social determinants: first, a direct leadership role to address health and long-term care needs of underprivileged groups; secondly, an influential catalyst, advocate, mediator, and collaborator in finding win–win situations that convinces other sectors to develop public policies and assign public resources to improving the SDOH; and finally, to communicate with the community and decision-makers on the impact of policies in labor, finance, housing, and other sectors which impact health, well-being, and productivity. The health sector can also serve as a knowledge broker in building and sharing understandings on the value of and mechanisms for reducing disparities in the SDOH and consequently in health status.
Limitations
Both morbidity and behavioral score variables are self-reported and thus subject to measurement errors from failure of memory or selective reporting.
Although the study identifies certain subgroups at higher risk of morbidity, we did not obtain qualitative data that might shed light on the reasons for this increased risk.
It is not possible in this study to establish whether the high rates of morbidity and ill health in urban areas as compared to other studies among urban slums in India are due to selective migration or to environmental factors.
Contributor Information
Ajay B. Pawar, Email: drabpawar@yahoo.com
Rajkumar K. Bansal, Email: kpalipudi@cdc.gov
References
- 1.Agarwal S. Urbanization and urban poverty. Paper presented at Ranbaxy Science Foundation’s 16th Roundtable Conference; November 11, 2005.
- 2.Atkinson S, Cheyne J. Immunization in urban areas: issues and strategies. Bull World Health Organ. 1994;72(2):183–194. [PMC free article] [PubMed]
- 3.Raphael D. Addressing the Social Determinants of Health in Canada: bridging the Gap between Research Findings and Public Policy Paper given at The Social Determinants of Health Across the Life-Span Conference, Toronto; November 2002; Policy Options. 2003;02:35–44.
- 4.Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health. 2003;57(4):254–258. [DOI] [PMC free article] [PubMed]
- 5.Marmot M, Wilkinson R. Social Determinants of Health. New York: Oxford University Press. 2001;2.
- 6.Sundar R, Mahal A, Sharma A. The Burden of ill health among the urban poor: the case of slums and resettlement colonies in Chennai and Delhi. NCAER. 2002;25:38–84.
- 7.Kapoor D, Agarwal KN, Sharma S, Kela K, Kaur I. Iron Status of children aged 9–36 months in an urban slum Integrated Child Development Services Project in Delhi. Indian Pediatr. 2002;39:136–144. [PubMed]
- 8.Rao S, Joshi SB, Kelkar RS. Changes in nutritional status and morbidity over time among pre school children from slums in Rune, India. Indian Pediatr. 2000;37:1060–1070. [PubMed]
- 9.Awasthi S, Pande VK. Prevalence of Malnutrition and intestinal parasites in Pre-school slum children in Lucknow. Indian Pediatr. 1997;34:599–605. [PubMed]
- 10.Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999;896:3–15. [DOI] [PubMed]
- 11.Evans RG, Barer ML, Marmor TR, eds. In: Why are Some People Healthy and Others Not? The Determinants of Health of Populations. New York: Aldine de Gruyter; 1994.
- 12.Frank J. Why population health? Can J Pub Health. May–June 1995;86:162–164. [PubMed]
- 13.Federal/Provincial/Territorial Advisory Committee on Population Health. Toward a Healthy Future. Second Report on the Health of Canadians. Ottawa: Health Canada; 1999.
- 14.Wilkinson R. Unhealthy Societies: The Afflictions of Inequality. New York: Routledge; 1996.
- 15.Wilkinson R, Marmot M. Social Determinants of Health: The Solid Facts. Copenhagen: World Health Organization; 1998.
- 16.Keating D. Developmental Health: Research, Policy and Practice. A presentation given at The Social Determinants of Health across the Life-Span Conference, Toronto; November 2002.
- 17.Single E, Robson L, Rehm J, Xie X, Xi X. Morbidity and mortality attributable to alcohol, tobacco, and illicit drug use in Canada. Am J Public Health. March 1999;89(3):385–390. [DOI] [PMC free article] [PubMed]
- 18.Hulshof KFAM, Brussaard JH, Kruizinga AG, et al. Socio-economic status, dietary intake and 10 y trends: the Dutch National Food Consumption Survey. Eur J Clin Nutr. 2003;57(1):128–137. [DOI] [PubMed]
- 19.Wadsworth MEJ. The Imprint of Time: Childhood, History And Adult Life. Oxford: Clarendon Press; 1991.
- 20.Power C, Manor O, Fox J. Health and Class: The Early Years. London: Chapman and Hall; 1991.
- 21.Davey Smith G, Hart C, Blane D, et al. Lifetime socioeconomic position and mortality: prospective observational study. BMJ. 1997;314:547–552. [DOI] [PMC free article] [PubMed]
- 22.Marmot M, Shipley M, Brunner E, Hemingway H. Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. J Epidemiol Community Health. 2001;55:301–307. [DOI] [PMC free article] [PubMed]
- 23.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:5. [DOI] [PubMed]
- 24.Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001;322(7294):1089–1094. [DOI] [PMC free article] [PubMed]
- 25.Glasgow RE, Toobert DJ, Gillette CD. Psychosocial barriers to diabetes self-management and quality of life. Diabetes Spectr. 2001;14(1):33–41. [DOI]
- 26.Aro S, Hasan J. Occupational class, psychosocial stress and morbidity. Ann Clin Res. 1987;19(2):62–68. [PubMed]
- 27.Friendly M. Early Childhood Education and Care. A presentation given at The Social Determinants of Health across the Life-Span Conference, Toronto; November 2002.
- 28.de Wolff A. Breaking the Myth of Flexible Work: Contingent Workers Project. Toronto; 2000.
- 29.Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001;322(7294):1089–1094. [DOI] [PMC free article] [PubMed]
- 30.Glasgow RE, Strycker LA, Toobert DJ, Eakin E. A social-ecologic approach to assessing support for disease self-management: the chronic illness resources survey. J Behav Med. 2000;23(6):559–583. [DOI] [PubMed]
- 31.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:5. [DOI] [PubMed]
- 32.Rao S. Nutritional status of the Indian population. J Biosci. 2001;26(4):481–489. [DOI] [PubMed]
- 33.Vijayalaxmi P, Lakshmi RN. Reproductive performance of expectant mothers. Indian J Nutr Diet. 1985;22:36–41.
- 34.Shaw M, Darling D, Gordon D, Davey Smith G. The Widening Gap: Health Inequalities and Policy in Britain. Bristol: The Policy Press; 1999.
- 35.Bhatia JC, Cleland J. Obstetric morbidity in South India: results from a community survey. Soc Sci Med. 1996;43(10):1507–1516. [DOI] [PubMed]
- 36.Vaillancourt Y, Aubry F, Tremblay L, Kearney M. Social Policy as a Determinant of Health and Well-Being: The Contribution of the Social Economy. A presentation given at The Social Determinants of Health across the Life-Span Conference; Toronto; November 2002.