Abstract
Recidivism is a pervasive problem facing the incarcerated. Incarcerated persons who are human immunodeficiency virus (HIV)-infected often have multiple risk factors associated with initial incarceration and recidivism, in particular, injection drug use. Yet, some jails provide case management for HIV-infected inmates to provide continuity of health care, which might have positive effects on reentry into the community. We sought to measure recidivism and factors related to recidivism in an HIV-infected cohort in an urban county jail with an active case management program. Fifty-two inmates surveyed in 1999 at the San Francisco County Jail were followed for rearrests through 2006. In follow-up, 73% were re-incarcerated on an average of 6.8 times for 552 days. Risk factors included nonwhite ethnicity, history of homelessness and crack use, common risk factors for incarceration. Less than high school education was associated with recidivism, shorter time to reincarceration, and more incarcerations. HIV-infected inmates spend a high proportion of time in multiple incarcerations, a reflection of the cyclical nature of incarceration despite comprehensive case management. Well-known risk factors for incarceration were associated with recidivism; in addition, lack of high school education played a prominent role. Education should be explored as a way to make further progress on breaking the cycle of incarceration.
Keywords: Recidivism, Education, Jail.
Introduction
Recidivism, defined as returning to a correctional facility after release, is common in the U.S.: among those released in 1994, 44% were rearrested within 1 year of release from prison and 67% rearrested within 3 years.1 Nearly half of all jail inmates in 2002 had served one or more prior incarcerations.2 The cyclical nature of arrest, conviction, release, and recidivism affects all former prisoners’ capacity to achieve long-term stability in their communities.
Successful reintegration to their home communities may be especially difficult for human immunodeficiency virus (HIV)-infected prisoners. HIV is often tied to the reason for incarceration, and HIV-infected jail inmates experience a multitude of problems both during their incarceration and upon return to their home communities. The stability and health of HIV-infected incarcerated and formerly incarcerated persons are bound to their social environment and the social conditions in which they live. Low socioeconomic status (SES), marginalized housing, and limited income can decrease access to critical community resources thereby increasing the risk of rearrest and poor health outcomes3–8 including mortality.9
While these individuals frequently lead chaotic lives, they are also intensively case managed in some U.S. jails and have access to social and medical resources both in and out of the institution.10–16 Health-related efforts in correctional facilities have mainly focused on short-term (<3 years) risk reduction and interventions to improve continuity of care after release, and even effective programs to improve HIV outcomes on the inside have shown reversal of gains made after release to the community.17 Risk reduction interventions have demonstrated positive outcomes related to behaviors,18 but the effect of such interventions on decreasing recidivism has often been inconclusive or not measured.10,11 Interventions to improve continuity of care and links to outside programs have demonstrated that high-risk individuals will access, utilize, and benefit from medical and social services provided by a regular network of providers,12–16,19 but these have not been evaluated for their long-term effect on recidivism.
Short-term case management and continuity of care interventions provide suggestions that health care services may have an effect on reducing recidivism. However, understanding of the factors associated with successful reintegration into the community, as opposed to the time in the free world being punctuated by frequent reincarcerations, is limited. Awareness of the role incarceration plays in the health of vulnerable groups has increased among clinicians, public health workers, and policymakers; knowledge of factors associated with the cycle of incarceration will assist in determining ways to intervene. The purpose of this study was to describe the natural history of incarceration in an HIV-infected cohort in an urban county jail that has a well-established case management program. Our research questions were: what are the characteristics of those who are rearrested; and what factors are related to time to first reincarceration, the number of times incarcerated, and the total number of days incarcerated over time?
Data and Methodology
Design, Participants and Setting
Baseline data for this historical cohort study came from secondary data analysis of interviews conducted in 1999 with 53 HIV-infected inmates at the San Francisco City and County Jail. Participants were under the care of the Forensic AIDS Project (FAP), an integrated medical case management program for persons diagnosed in jail or who self-identify as having HIV, including post-release case management services. Between May 1 and September 2, 1999, FAP medical providers identified English- or Spanish-speaking inmates who would be able to provide consent, and asked if they would be willing to be interviewed. Over the 4-month period of recruitment, 121 persons were identified; a small percent (5%) refused to consent to the study, and the remaining persons were not approached because of limited resources or were released or unavailable for consent and interview. This analysis includes jail record review of persons who were released to the community at some time during the follow-up period from the initial interview through December 2006. As one person was sent directly from jail to prison and died before ever being released, the sample for this study, which was approved by the Institutional Review Board of the University of California, San Francisco, included 52 subjects.
Procedures
The interviews and interview methods, conducted as preliminary work with this population, have been described esewhere.20 All interviews were conducted face-to-face in a private setting in the jail by trained interviewers. The remaining study procedures included record review for dates of incarceration either in the San Francisco Jail or in the California State prison system.
Data and Measures
Dependent variables Data were obtained from the jail electronic medical record and Sheriff’s Department personnel and included dates of release and reentry, and date of death if that occurred, for the time period from interview through December 2006. As subjects were interviewed over a 4-month period, the final subject had a follow-up of 2,677 days; therefore, we limited follow-up for all other subjects to 2,677 days (7 years, 4 months) after interview. Our research questions examined four dependent variables. Recidivism was defined as a dichotomous variable, whether a subject reentered the San Francisco Jail at least once during the follow-up period. Time to re-incarceration was the number of days from the first release to the first re-incarceration, death, or end of the follow-up period. The number of re-incarcerations was counted for each subsequent entry into the San Francisco Jail. Only those re-entering jail from the community were counted as having another incarceration; movement among correctional facilities without release to the community was counted as part of a single incarceration. The number of days of incarceration included the days in jail or prison, in one or more incarcerations, from the date of the interview through the follow-up period.
Independent variables Data from the 1999 interview included a number of variables that describe the sample as well as factors often associated with incarceration: gender, age, ethnicity, education, marital status, employment before entering jail, ever homeless, previous incarceration, living situation in the month before entering jail and total number of days homeless. Questions were taken from the Quality of Life Interview (QOLI) on living situation,21 and dichotomized into stable housing (own apartment or home, living with friends or relatives, and living at a board and care facility or alcohol/drug treatment program) or unstable housing (homeless shelter or hotel or living in a car, a park or on the street).
Health-related variables included mental health, which has been associated with both the risk and length of incarceration.22–24 The mental health summary scale of the Medical Outcomes Health Survey Short Form 36 (SF-36) has been validated extensively with community and clinical samples,25,26 and is identical to MOS-HIV, the version used and extensively tested with HIV-infected persons.27 Subjects were asked a number of questions related to alcohol and drug use, which is strongly associated with the risk of incarceration.22,28 Questions adapted from the Addiction Severity Index, found to be effective in identifying substance abuse and dependence disorders,29 were explored including ever had a problem with alcohol, ever had a problem with drugs, ever had use of illegal drugs, ever had injection of illegal substances, and ever had use of a number of substances (crack, amphetamine, cocaine, marijuana). As heroin use was not separated from other injection drugs in the interview, heroin use was ascertained using medical records from the clinical evaluation and care during the 1999 jail term. Having some form of health insurance (Medicaid, Medicare, VA benefits, Kaiser or other private health insurance, dichotomized to self-report of any health insurance) was used as a surrogate measure of access to health care services, as it has been correlated with receipt of public assistance, health care, and access to substance abuse treatment.30 Likewise, a question about whether subjects had received HIV care outside jail was used as a measure of linkage to services.
Statistical Analysis
All analyses used SPSS, version 15, with alpha = 0.05 for determination of statistical significance. As the sample was very small, the focus of this paper is descriptive, to suggest future work. Bivariate analyses with dependent variables and correlations between variables at baseline were conducted, and a modest number of covariates were selected for multiple regression analyses. For the first research question (whether subjects were re-incarcerated), bivariate analyses (chi square and t tests) were done, as well as a logistic regression to generate adjusted odds ratios (OR) and 95% confidence intervals (CI) as estimates of relative risk.
For the second research question (time to re-incarceration), we employed Cox regression procedures to model time from release to the first re-incarceration. Censored cases included those not re-incarcerated who were right-censored at the end of follow-up, as were those who died during follow-up, right-censored at the date of death. We also used Kaplan–Meier procedures to examine the survival rate (defined as not re-incarcerated) at each point in time using estimated conditional probabilities, with plots of the survival function for groups by variables demonstrated in descriptive analyses of the sample.
For the third and fourth research questions, we evaluated the appropriateness of the negative binomial regression model for the number of incarcerations and the overall length of incarceration during follow-up. For both, outcomes were counts that we assumed would cluster around zero or one, with low frequencies at higher values, and neither would have an assumption of normal distribution of error terms. We evaluated each and found overdispersion in both, i.e., the variance was greater than the mean. Therefore, the negative binomial regression was the appropriate statistical model with no special corrections needed.31,32
Results
In 1999, subjects averaged 38.8 years of age (median 38) with an average of 6.8 years (range 37 days–15 years) since they found out they were HIV positive. Only one subject, the person whose time since HIV positive was 37 days, was diagnosed positive during this jail term. Nearly all reported that they had ever used illegal drugs (n = 51, 98%), 77% reported ever injecting drugs (n = 40), and most (n = 44, 85%) reported that they ever had a problem with drugs. A history of drug use was reported as follows: marijuana (90%), crack (79%), cocaine (65%), amphetamines (56%), and heroin (46%). Most (84%) had been homeless at some point in their lives, with days ranging from 2–6,205 (median 730 days) among those reporting homelessness.
Recidivism
At some point in the follow-up period, 73% of the subjects (n = 38) were re-incarcerated (Table 1), and of these, 19 (36%) went to prison. Nearly all had been in jail before (n = 36, 90%). Neither age nor time since being diagnosed with HIV influenced recidivism. Those who had ever used crack were more likely to be re-incarcerated (RR 1.8, 95% CI 0.9–3.4), and crack use was reported by all Blacks (29 of 29), compared to half of Whites (8 of 15) and Others (4 of 8). Nonwhites were 1.5 times as likely as Whites to be re-incarcerated (RR 1.5, 95% CI 0.9–2.5). Low education was significantly associated with recidivism, examined as a continuous variable or dichotomized (RR 1.5, 95% CI 1.1–2.0 for those with less than high school). Those reporting ever homeless were more likely to be re-incarcerated (RR 3.3, 95% CI 1.0–11.0). A logistic regression analysis conducted with nonwhite ethnicity, less than high school and ever homeless is presented on Table 2.
Table 1.
Characteristics of 52 HIV-infected inmates at baseline interview in 1999 by recidivism through 2006
| Characteristic at baseline interview | Rejailed | Not rejailed | Total | P |
|---|---|---|---|---|
| N = 38 | N = 14 | |||
| Number (%) | Number (%) | Number | ||
| Gender | 0.893 | |||
| Male | 32 (73) | 12 (27) | 44 | |
| Female | 6 (75) | 2 (25) | 8 | |
| Race/ethnicity | 0.041a | |||
| Black | 23 (79) | 6 (21) | 29 | |
| Latino | 2 (100) | 0 (0) | 2 | |
| Other, mixed ethnicity | 5 (83) | 1 (17) | 6 | |
| White | 8 (53) | 7 (47) | 15 | |
| Marital or partnered status | 0.632 | |||
| Never married | 17 (71) | 7 (29) | 24 | |
| Widowed, separated, divorced | 10 (67) | 5 (33) | 15 | |
| Married or partnered | 10 (83) | 2 (17) | 12 | |
| Education | 0.021 | |||
| <High school | 16 (94) | 1 (6) | 17 | |
| High school or more | 22 (63) | 13 (37) | 35 | |
| Not employed before jail | 0.688 | |||
| No | 32 (74) | 11 (26) | 43 | |
| Yes | 6 (67) | 3 (33) | 9 | |
| Ever homeless | 0.003 | |||
| Yes | 36 (82) | 8 (18) | 44 | |
| No | 2 (25) | 6 (75) | 8 | |
| In jail previously | 0.079 | |||
| Yes | 36 (77) | 11 (23) | 47 | |
| No | 2 (40) | 3 (60) | 5 | |
| Had no health insurance | 0.087 | |||
| Yes | 21 (84) | 4 (16) | 25 | |
| No | 17 (63) | 10 (37) | 27 | |
| Problem with drinking | 0.010 | |||
| Yes | 12 (54) | 10 (46) | 22 | |
| No | 26 (87) | 4 (13) | 30 | |
| Heroin use at jail entry | 0.736 | |||
| Yes | 17 (71) | 7 (29) | 24 | |
| No | 21 (75) | 7 (25) | 28 | |
| Ever use of crack | 0.050 | |||
| Yes | 33 (80) | 8 (20) | 41 | |
| No | 5 (46) | 6 (54) | 11 |
aIn the comparison between Whites and all others, p = 0.041.
Table 2.
Variables associated with recidivism, time to reincarceration, number of incarcerations, and total number of days incarcerated, in follow-up of 52 HIV-infected inmates from baseline interview in 1999 through 2006 by multiple regression analyses
| Parameter | Adjusted | 95% CI | P |
|---|---|---|---|
| Recidivism: were subjects rejailed?a (odds ratio) | |||
| Nonwhite ethnicity | 4.1 | 0.8–21.3 | 0.089 |
| Less than high school education | 19.8 | 1.3–307.3 | 0.033 |
| Ever homeless | 19.5 | 1.9–205.4 | 0.013 |
| Time to re-incarcerationb (relative hazard) | |||
| Nonwhite ethnicity | 1.8 | 0.8–4.3 | 0.159 |
| Less than High School education | 3.8 | 1.8–8.0 | 0.001 |
| Ever homeless | 7.9 | 1.7–36.7 | 0.008 |
| Ever use of crack | 2.3 | 0.8–6.2 | 0.113 |
| In jail previously | 0.7 | 0.2–3.5 | 0.698 |
| Number of incarcerationsc (odds ratio) | |||
| Educational grade completed | 0.8 | 0.7–0.9 | 0.041 |
| Total days homeless (per 100 days) | 7.4 | 1.2–44.7 | 0.029 |
| Ever use of crack | 2.8 | 1.1–7.0 | 0.032 |
| In jail previously | 5.3 | 1.1–25.7 | 0.037 |
| No health insurance | 1.9 | 0.9–3.8 | 0.083 |
| Number of days incarceratedc (odds ratio) | |||
| Male gender | 0.6 | 0.3–1.2 | 0.144 |
| Mental health summary score | 0.9 | 0.9–1.0 | 0.012 |
| Care for HIV outside jail | 1.7 | 0.7–4.3 | 0.233 |
CI Confidence interval
aLogistic regression analysis
bCox proportional hazards analysis
cNegative binomial regression analysis
Time to Reincarceration
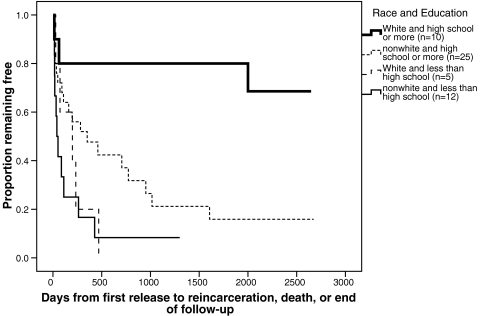
After the enrollment and interview in 1999, the 52 subjects in this sample remained in jail from 2–2,366 days (mean 193 days, median 86.5 days). After release, six subjects (11.5%) died during follow-up. After 1 month of follow-up, 21% had reentered jail, by 6 months 44%, and after 1 year of follow-up, 60% had been reincarcerated. Women were rejailed sooner than men (p = .092). Blacks and others were rejailed sooner than Whites (p = 0.011). Those who had been homeless versus not (p = .003) and those in jail before versus those who were not (p = .043) were rejailed sooner. Of all drug and alcohol use measures, only crack use was associated with shorter time to first rejailing (p = .004). Cox proportional hazard results are shown on Table 2. Our interest in education and ethnicity prompted display of Kaplan–Meier survival for Whites with high school or more, Whites with < high school, nonwhites with high school or more, and nonwhites with < high school (Figure 1), to illustrate the impact of high school education on remaining out of jail.
FIGURE 1.
Proportion of HIV-infected inmates remaining free by race and high school education.
Number of Reincarcerations
The total sample of 52 subjects experienced an average of 4.9 subsequent incarcerations (median 3), ranging from 0 to 22. The 38 (73%) who were reincarcerated averaged 6.8 times (median 5, range 1–22). In examining bivariate associations, those who had been previously incarcerated averaged 5.4 reincarcerations versus 0.8 for those who had not been in jail before (p = 0.069). Those reporting they had ever been homeless had 5.5 subsequent incarcerations (median 3.5, range 0–22) compared to those who had not (mean 1.9, median 0, range 0–11); total days homeless was correlated with the number of incarcerations (Pearson correlation 0.340, p = .015). Education was again negatively correlated (Pearson correlation −0.306, p = 0.027), with those having less than a high school education having 6.3 subsequent re-incarcerations versus 4.3 for those with at least high school, although the dichotomized variable was not statistically significant. Persons who reported having no insurance averaged 7.2 re-incarcerations versus 2.9 for those with insurance (p = 0.003). Negative binomial multiple regression analysis of these variables is shown on Table 2.
Total Number of Days Incarcerated
On average, the group of 52 subjects were incarcerated 552 days (median 330.5, range 3–2,366), 21% of the time over the 7.3 years of follow-up. Women were incarcerated longer (mean 925 days, median 577) than men (mean 484 days, median 300; p = 0.051). Ethnic group differed but did not reach statistical significance: in detailed examination, Blacks were incarcerated 624 days (median 370) compared to Whites (mean 471, median 263) or others (mean 444, median 303). There was a negative correlation between the SF-36 mental health summary score and the number of days of total incarceration (Pearson correlation −0.432, p = 0.001)− that is, the poorer the mental health the more days of incarceration. None of the drug or alcohol variables was associated with time incarcerated. Those who reported they received HIV care outside jail were incarcerated 466 days on average (median 328) compared to 1,212 days (median 1,211) for those who did not receive HIV care outside jail (p = 0.003). Negative binomial regression analysis of these variables is shown on Table 2.
Discussion
Our study found that HIV-infected inmates spend a high proportion of time behind bars in multiple incarcerations, a reflection of the cyclical nature of incarceration and the barriers encountered in achieving long-term stability in their home communities. Characteristics reflect those who are likely to be incarcerated, including the impact of nonwhite ethnicity, history of homelessness, mental illness, and prior incarceration.2 Upon release, these individuals frequently experience homelessness and lack of employment.1,22,33,34 They have high rates of substance abuse and mental illness,1,23,35 and these illnesses coupled with marginalized social circumstances lead to high rates of recidivism.22,24,36 But this sample also came from a jail with a well-developed case management program, although the program focuses on continuity of health care and interventions to facilitate this linkage rather than any specific activities to reduce recidivism. Similar research is needed for HIV-infected inmates without such a program to help in the understanding of the potential by-product of case management for health care on recidivism. Our results may represent the best case; alternately, our findings may indicate that a health-related case management program has little effect on recidivism in a cohort with high rates of substance abuse.
By contrast, we found that reporting no health insurance predicted higher likelihood of any recidivism; this adds to the work by Lee et al. that health insurance may be a marker for successful interaction with public institutions to obtain care, benefits, and public assistance after jail.30 Likewise, having medical care outside of jail predicted fewer days of incarceration, suggesting a positive role for health care in reducing recidivism. In a prospective cohort study of 871 HIV-infected women and 439 high-risk HIV-negative women, Sheu et al. found that those with a continuous relationship with a single health care provider for more than 2 years were half as likely to be incarcerated as those without, during the 2-year study period.15 Other research has demonstrated that having Medicaid and receiving behavioral health services were related to reduced recidivism and longer time to rearrest among inmates with severe mental illness in two counties, although the effect was small.35 Consistent medical care may be an indication of involvement in a larger social and supportive network that may assist the individual in preventing high-risk behavior leading to rearrest and reincarceration. However, the relationship between continuity of medical care and decreased incarceration rates over a longer time period is not well understood and would benefit from further exploration.
Perhaps our most interesting findings relate to the association between education and recidivism. There is ample evidence on the importance of a high school diploma in improved health outcomes,3,4,37 including less mortality.4 Woolf et al. have suggested that more lives could be saved by improving the social determinants of health such as inadequate education, low SES, and homelessness than by medical intervention.4 A high school education has also been shown to play a role in reducing criminal activity and first-time incarceration rates.5,6 High school dropout status is related to a higher likelihood of injection drug use and limited economic opportunity that in turn have been associated with an increased risk of incarceration.3,5–7,38 Obot et al. found that African-American (AA) adults who had dropped out of high school were twice as likely to have injected drugs when compared with neighborhood-matched AA adults who had completed high school.7 Data from National Longitudinal Survey of Youth and the Uniform Crime Reports showed that high school dropouts were more likely to engage in property, drug, and violent crimes and more likely to be incarcerated over a 5-year period compared to high school graduates and persons attending college.5
Adding to the literature on the impact of a high school education on criminal activity and the risk of first-time incarceration, our study presents new evidence of the association between high school education and an individual’s ability to remain in his community after a period of incarceration. A cross-sectional survey of 1,405 injection drug users in Baltimore found that a previous arrest was twice as likely for persons with less than an 11th grade education as for those with an 11th grade education or more.3 Our longitudinal study of jail inmates, nearly all of whom were substance abusers and had multiple risk factors for rearrest, suggests that a high school education is related to successful transition to the community.
This study was limited by its small sample. The refusal rate was low, but limited resources precluded interviewing all who were eligible in the 4-month period of the interviews. Therefore, the sample may not represent HIV-infected persons in the San Francisco Jail or in FAP care; likewise, results may not be generalizable to other jails, with or without case management programs for HIV care. Data collected at baseline were by self-report, and may be biased. Associations seen should not be interpreted as causal but descriptive, with the intent to prompt further study.
While case management and continuity of health care are important components in assisting individuals to receive and maintain care in the short-term after release, our results suggest that there are larger social conditions and disadvantages, such as inadequate education that may be associated with recidivism. To be truly effective in helping formerly incarcerated people live successful lives in their home communities, public health policymakers, researchers, and clinicians should consider a deeper involvement in and commitment to changing the social conditions in which these individuals live.4 The relationships between education and risk of incarceration and recidivism are complex, not well understood, and deeply embedded within societal and environmental contexts. Additional information is needed to broaden the understanding and define more clearly the role that education, both early childhood education and adult education, may play in helping formerly incarcerated individuals achieve long-term stability in their communities. With more clarity on these questions, focused research to improve the social determinants and circumstances within the environments in which these individuals live can be tested,3,4 including educational programs in correctional facilities. Like other social circumstances—such as housing—which appears to play an important role in preventing recidivism, educational achievement may be an underappreciated, yet addressable factor in the life of HIV-infected adults who have been incarcerated. Access to and completion of education both by our youth and by adults who need a second chance in life may increase their capacity to achieve long-term stability in the community and may make further progress on breaking the cycle of incarceration.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s11524-008-9289-4
References
- 1.Langan PA, Levin DJ. Recidivism of prisoners released in 1994. Bureau of Justice Statistics Special Report. 2002; NCJ 193427.Washington, DC: US Dept of Justice, Office of Justice Programs.
- 2.James DJ. Profile of jail inmates, 2002. Bureau of Justice Statistics Bulletin. 2004; NCJ 201932.Washington, DC: US Dept of Justice, Office of Justice Programs.
- 3.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness and incarceration. Public Health Rep. 2002;117(Supplement 1):138–145. [PMC free article] [PubMed]
- 4.Woolf S, Johnson RE, Phillips RL, Philipsen M. Giving everyone the health of the educated: an examination of whether social change would save more lives than medical advances. Am J Public Health. 2007;97:679–683. [DOI] [PMC free article] [PubMed]
- 5.Lochner L. Education, work, and crime: a human capital approach. International Economic Review. 2004;45(3):811–843. [DOI]
- 6.Lochner L, Morretti E. The effect of education on crime: evidence from prison inmates, arrests, and self-reports. Am Economic Review. 2004;94:155–189. [DOI]
- 7.Obot IS, Hubbard S, Anthony JC. Level of education and injecting drug use among African Americans. Drug and Alcohol Dependence. 1999;55:177–182. [DOI] [PubMed]
- 8.Seaman SR, Gore SM, Brettle RP. Injecting drug users in Edinburgh have a high rate of recidivism. Addiction. 2000;95(5):791–792. [DOI] [PubMed]
- 9.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. [DOI] [PMC free article] [PubMed]
- 10.Grinstead O, Zack B, Faigeles B. Reducing postrelease risk behavior among HIV seropositive prison inmates: the health promotion program. AIDS Educ Prev. 2001;13(2):109–119. [DOI] [PubMed]
- 11.Myers J, Zack B, Kramer K, Gardner M, Rucobo G, Costa-Taylor S. Get Connected: an HIV prevention case management program for men and women leaving California prisons. Am J Public Health. 2005;95(10):1682–1684. [DOI] [PMC free article] [PubMed]
- 12.Conklin TJ, Lincoln T, Flanigan TP. A public health model to connect correctional health care with communities. Am J Public Health. 1998;88:1249–1250. [PubMed]
- 13.Farley JL, Mitty JA, Lally MA, et al. Comprehensive medical care among HIV-positive incarcerated women: the Rhode Island experience. J Womens Health Gend Based Med. 2000;9(1):51–56. [DOI] [PubMed]
- 14.Rich JD, Holmes L, Salas C, et al. Successful linkages of medical care and community services for HIV-positive offenders being released from prison. J Urban Health. 2001;78:279–289. [DOI] [PMC free article] [PubMed]
- 15.Sheu M, Hogan J, Allsworth J, et al. Continuity of medical care and risk of incarceration in HIV-positive and high-risk HIV-negative women. J Womens Health. 2002;11(8):743–50. [DOI] [PubMed]
- 16.Vigilante KC, Flynn MM, Affleck PC, et al. Reduction in recidivism of incarcerated women through primary care, peer counseling, and discharge planning. J Women’s Health. 1999;8(3):409–415. [DOI] [PubMed]
- 17.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760 Jun 15. [DOI] [PubMed]
- 18.Arriola KR, Braithwaite RL, Holmes E, Fortenberry RM. Post-release case management services and health-seeking behavior among HIV-infected ex-offenders. J Health Care Poor Underserved. 2007;18(3):665–674. [DOI] [PubMed]
- 19.Needels K, James-Burdumy S, Burghardt J. Community case management for former jail inmates: its impacts on rearrest, drug use, and HIV risk. J Urban Health. 2005;82(3):420–433. [DOI] [PMC free article] [PubMed]
- 20.White MC, Tulsky JP, Estes M, Jamison R, Long HL. Health and health behaviors in HIV-infected jail inmates, 1999 and 2005. AIDS Patient Care and STDs. 2008; 219–229. [DOI] [PubMed]
- 21.Lehman AF. A quality of life interview for the chronically mentally ill. Eval Program Plann. 11:51–62.
- 22.McNeil DE, Binder RL, Robinson JC. Incarceration associated with homelessness, mental disorder, and co-occurring substance abuse. Psych Services. 2005;56(7):840–846. [DOI] [PubMed]
- 23.National Commission on Correctional Health Care, The health status of soon-to-be-released inmates; a report to congress. Vol 1 and 2. Chicago: March, 2002.
- 24.Lamberti JS. Understanding and preventing criminal recidivism among adults with psychotic disorders. Psych Services. 2007;58(6):773–781. [DOI] [PubMed]
- 25.Ware JE. SF-36 health survey update. Spine. 2000;25:3130–3139. [DOI] [PubMed]
- 26.Ware JE, Snow KK, Kosinski M. SF-36(R) Health Survey: manual and Interpretation Guide. Lincoln, RI: Quality Metric, 2000.
- 27.Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the Medical Outcomes Study of health-related quality of life measures in HIV/AIDS. Quality of Life Res. 1997;6:531–554. [DOI] [PubMed]
- 28.Karberg JC, James DJ. Substance dependence, abuse and treatment of jail inmates, 2002. Bureau of Justice Statistics Bulletin. 2005; NCJ 209588.Washington, DC: US Dept of Justice, Office of Justice Programs.
- 29.Peters RH, Greenbaum PE, Steinberg ML, et al. Effectiveness of screening instruments in detecting substance use disorders among prisoners. J Subst Abuse Treat. 2000;18(4):349–358. [DOI] [PubMed]
- 30.Lee J, Vlahov D, Freudenberg N. Primary care and health insurance among women released from New York City jails. J Health Care Poor Underserved. 2006;17(1):200–217. [DOI] [PubMed]
- 31.Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: poisson, overdispersed poisson, and negative binomial models. Psych Bull. 1995;118(3):392–404. [DOI] [PubMed]
- 32.Hutchinson MK, Holtman MC. Analysis of count data using poisson regression. Res Nurs Health. 2005;28:408–418. [DOI] [PubMed]
- 33.Robertson MJ, Clark RA, Charlebois ED, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. Am J Public Health. 2004;94(7):1207–1217. [DOI] [PMC free article] [PubMed]
- 34.Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005;95:1747–1752. [DOI] [PMC free article] [PubMed]
- 35.Morrissey JP, Cuddeback GS, Cuellar AE, Steadman HJ. The role of Medicaid enrollment and outpatient service use in jail recidivism among persons with severe mental illness. Psych Services. 2007;58(6):794–801. [DOI] [PubMed]
- 36.Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95:1725–1736. [DOI] [PMC free article] [PubMed]
- 37.Adler NE, Ostrove JM. Socioeconomic status and health: what we know what we don’t. Ann N Y Acad Sci. 1999;896:3–15. [DOI] [PubMed]
- 38.Arum R, Beattie IR. High school experience and the risk of adult incarceration. Criminology. 1999;37(3):515–540. [DOI]