Abstract
Early-childhood obesity has reached epidemic proportions, particularly among low-income, minority, urban children. Understanding the progression of obesity prevalence rates from infancy through early childhood can inform public health efforts to combat this epidemic and create developmentally appropriate strategies. In this study, we assessed the prevalence of overweight and obesity among urban 1- to 5-year olds and estimated risk by age and gender. We surveyed the medical records of a random sample of 1,713 children seen at a New York City primary-care network. Outcome measures were weight-for-length for <2-year olds and body mass index for 2- to 5-year olds. Overweight was defined as percentiles ≥85% to <95%, obesity ≥95%. Analysis utilized chi-square, logistic regression, and z tests. Between 1 and 5 years of age, overweight increased 3.7% to 20.8% and obesity 7.5% to 29.8% (p < 0.01). Risk increased with age: compared with 1-year olds, 5-year olds were 8.2 times as likely (95% confidence interval (CI) = 5.5–12.21) to be overweight or obese. Boys were more likely to be obese than girls (adjusted odds ratio = 1.3; 95% CI = 1–1.64). Significant increases in overweight and obesity occurred between ages 1 and 3 years (overweight, 3.7% to 16%, p < 0.01; obesity, 7.5% to 30.2%, p < 0.01). Among urban children, more than half were overweight or obese by age 5. Overweight and obesity rates increased dramatically between the ages of 1 and 3 years. Interventions aimed at this age period may have the greatest impact at preventing childhood obesity.
Keywords: Body mass index, BMI; Childhood obesity; Community health; Ethnic minorities; Prevalence
Introduction
Nationwide, early-childhood obesity has reached epidemic proportions, particularly among low-income, minority, urban children.1–10 Although not all obese children become obese adults, research reveals obesity in early childhood is predictive of obesity later in life.6,11,14 In a national sample, children who were overweight at ages 24, 36, or 54 months were five times more likely to be overweight at age 12 years compared to those not overweight.13 Children who are obese are more likely to have high blood pressure, abnormal lipids, asthma, type 2 diabetes, nonalcoholic fatty liver disease, and sleep apnea.15 Moreover, adults who were overweight as children have higher morbidity and mortality than those who were never overweight, even if they lose the extra weight during adulthood.14,16 The children at greatest risk for overweight at an early age are low-income and minority children. Case studies also suggest that children living in large metropolitan areas are also at risk.6
Overweight and obesity start early in life, but how early? In 2000, using data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System (PedNSS 2000), the prevalence of obesity among low-income 2-year olds nationwide was 12.5%, 14.2% among 3-year olds, and 16% among 4-year olds, with a slight male-to-female preponderance.7 In 2001, among children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in New York City, 14% of 2-year olds were obese, and 17.1% were overweight. The rate of obesity nearly doubled to 26.5% among 4-year olds, while the rate of overweight slightly increased to 18.7%.17 Boys and girls were equally at risk. These findings suggest that, at least in certain low-income, minority, urban populations, early childhood may be a critical time period in the development of obesity, and therefore, provide an important window for introducing programs aimed at reducing risk of overweight.
Yet data are lacking on the prevalence of obesity and overweight for children under 2 years of age. This may be due to several factors, including body mass index (BMI) reference value standards not having been established for this age group; the weak association of obesity in early childhood and later life; the concern of labeling young children as obese; and lastly, the fear of making major nutritional changes to the diet of toddlers at a time when myelination of the central nervous system is very active.18 Additional research is needed on the progression of obesity prevalence rates from infancy through early childhood—ages 1 through 5 years—to inform public health efforts to combat this epidemic and create developmentally appropriate strategies.
The objectives of our study were to estimate the prevalence of overweight and obesity among 1- to 5-year-old low-income, minority boys and girls seen at a large, primary-care network in New York City; to quantify their risk of overweight and obesity based on age and gender; and to identify a critical age period in early childhood when the highest prevalence of overweight and obesity are documented.
Research Methods and Procedures
Study Setting
This study was conducted in a large, hospital-affiliated, primary-care network in Northern Manhattan, New York City, one of the most disadvantaged communities in New York City and the nation. The ethnic breakdown of this community of approximately 200,000 persons is two thirds Latino, the majority from the Dominican Republic, and one sixth African American. A third of residents live in poverty.19 The hospital is the primary birth center for the community20 and refers the majority of the newborns to the five-practice network. The practice network serves >20,000 children, with 60,000 pediatric visits per year. The patient population of this primary-care network mirrors the ethnic breakdown of the community: virtually all are minority and low income (85% of the children receive Medicaid). The relative high insurance rates found in this population is a tribute to Child Health Plus, New York’s state health insurance program, available to all children regardless of immigration status, and to the efforts of a coalition-led facilitated enrollment program which has actively enrolled over 7,000 children in this community.21,22
Study Design
We conducted a cross-sectional survey of a random sample of children ages 1–5 years who had made a visit to the practice network between September 2004 and January 2005. The sampling frame was generated from the hospital registration database. The database was stratified by age (single years) and gender. Five single-year age groups were constructed. Each group included children with ages spanning the 12 months of each respective age-group year (i.e., age-group 1 year = 12 months to 24 months minus 1 day; age-group 2 years = 24 months to 36 months minus 1 day; etc.) To be able to detect a 10% difference in BMI for each single year of age (1 to 5 years) and by gender, we estimated a sample size of 300 children per year for a total sample size of 1,500 children. Within each age group, we randomly selected the requisite number of children, alternating the selection between the two genders. This study was approved by the Institutional Review Board of Columbia University Medical Center.
Data Collection
Weight, height, age, and gender were collected from the children’s medical records. Insurance and ethnicity were extracted from the hospital database.
Outcome Measures
We calculated weight-for-length values for children 12–23 months of age and BMI values for children ages 2–5 years. The weight-for-length and BMI values were converted to weight-for-length or BMI percentiles for age and gender according to the Centers for Disease Control and Prevention growth charts.23 Children were classified into the following standardized weight categories: (1) underweight, ≤5th percentile; (2) normal weight, 5th to 85th percentiles; (3) overweight, ≥85th to <95th percentiles; and (4) obese, ≥95th percentile.
Data Analysis
Chi-square testing was used to detect significant differences in the distribution of weight categories among and within the different age groups when stratified by age, gender, and ethnicity. We defined the critical age period of overweight or obesity development as the interval between single-year age groups where we documented the highest increase in prevalence. The z test of two proportions was used to determine statistically significant differences in weight-category means among successive age groups. For the z-test analysis, we compared prevalence rates of overweight and of obesity between successive age-group pairs (1- to 2-year olds, 2- to 3-year olds, 3- to 4-year olds, and 4- to 5-year olds). Data analysis was performed using SPSS version 13.0.24 We performed multivariate analysis using logistic regression to further quantify any significant associations of weight category with age, ethnicity, and gender. The paired-sample t test was used to test for significant differences in BMI between our study population and the comparable distribution for the nation, from the PedNSS 2000.25
Results
Patient Characteristics
A total of 5,437 patients between the ages of 1 and 5 years made visits to the practice network during the study period (girls, n = 2652, 48.8%; boys, n = 2785, 51.2%). Seventy-four percent of the patients were Latino, 15% African American, and 11% other. The random sampling procedures generated a selection of 1,713 children between the ages of 1 and 5 years, split almost equally between the two genders (female, n = 813; male, n = 900). Seventy-eight percent of the children were Latino, 17% African American, and 4.5% other. Eighty-five percent of patients were Medicaid recipients. There were no statistically significant differences in gender or ethnicity of children among the five different age groups (chi-square = 0.037, p = 1 and chi-square = 2.319, p = 0.97, respectively).
Distribution of Weight Categories by Age and Gender
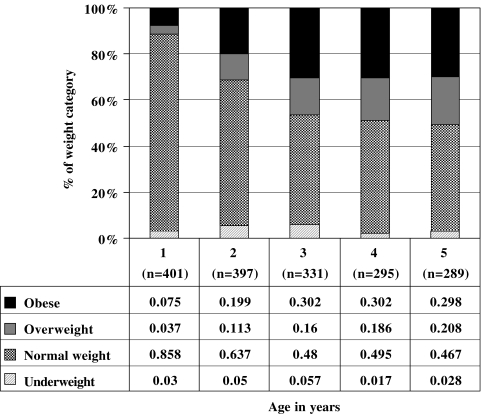
Overweight prevalence increased from a low of 3.7% among 1-year olds to 20.8% among 5-year olds. Obesity prevalence increased from a low of 7.5% among 1-year olds to 29.8% among 5-year olds (Figure 1). The prevalence of overweight and obesity increased with age (chi-square = 190.3, p < 0.001). By age five, half (50.6%) of the children were overweight or obese.
Figure 1.
Distribution of weight categories by age, children ages 1–5 years.
There was a significant, nonlinear association between gender and weight category, with more boys obese and more girls overweight. Among boys, 12.0% were overweight, and 24.2% were obese, while among girls, 14.8% of girls were overweight, and 20.4% were obese (chi-square = 5.1, p = 0.02). Within each age group, there were no statistically significant differences in the distribution of weight categories by ethnicity or gender.
Risk of Overweight and Obesity by Age
With each year of age, children were more likely to be overweight or obese. Older age was positively and significantly associated with an increased likelihood of being overweight or obese independent of ethnicity and gender (Table 1). Compared with 1-year olds, 2-year olds were 3.1 times, 3-year olds 4.7 times, 4-year olds 5.7 times, and 5-year olds 6.4 times as likely to be overweight. There was a similar increase in the risk of obesity with each additional year of life, but the progression was not as gradual as for overweight risk. The largest increase was for 3-year olds, and after that age the obesity risk remained stable. Compared with 1-year olds, 2-year olds were 3.4 times, 3-year olds 5.9 times, 4-year olds 5.8 times, and 5-year olds 5.6 times as likely to be obese. There was no significant association between overweight or obesity and gender or ethnicity. The prevalences of overweight and obesity in this study population were significantly higher than the national rates for 2-, 3-, and 4-year olds compared to those reported by the PedNSS25 (2-year olds, z = 4.458, p < 0.001; 3-year olds, z = 8.346, p < 0.001; and 4-year olds, z = 6.638, p < 0.001).
Table 1.
Risk of obesity or overweight by age, children ages 1–5 years
| Age (years) | Risk of overweight, OR (95% CI) | Risk of obesity, OR (95% CI) | Risk of overweight or obesity, OR (95% CI) |
|---|---|---|---|
| 1 | Ref 1 | 1 | 1 |
| 2 | 3.1 (1.7–5.7) | 3.4 (2.1–5.3) | 3.7 (2.5–5.5) |
| 3 | 4.7 (2.6–8.5) | 5.9 (3.8–9.4) | 7.2 (4.9–10.6) |
| 4 | 5.7 (3.1–10.3) | 5.8 (3.6–9.2) | 7.9 (5.2–11.7) |
| 5 | 6.4 (3.5–11.6) | 5.6 (3.5–8.9) | 8.2 (5.5–12.2) |
p values < 0.01 for all OR
OR Odds ratio
Ref 1 Reference value, age 1 year
The combined risk of being overweight or obese significantly increased with each successive year of age (Table 1). Compared with 1-year olds, 2-year olds were 3.7 times, 3-year olds 7.2 times, 4-year olds 7.9 times, and 5-year olds 8.2 times as likely to be overweight or obese.
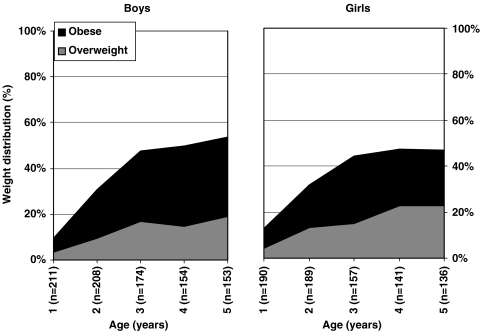
Risk of Overweight and Obesity by Gender
After adjusting for age and ethnicity, boys were slightly more likely to be obese than girls, [adjusted odds ratio = 1.3, 95% confidence interval (CI) = 1–1.635]. The strongest age trends in obesity and overweight were observed for boys, among whom rates of overweight and obesity increased from 16.7% and 31.0%, respectively, at age 3 to 19.0% and 34.6%, respectively, at age 5 (Figure 2). Although not statistically significant, for girls rates of overweight continued to increase with each year of age, from 15.3% at age 3 to 22.8% at age 5 years. Rates of obesity decreased between ages 3 (29.3%) and 5 years (24.3%; Figure 2).
Figure 2.
Percent of overweight vs. obesity among children ages 1 through 5 years.
Risk of Overweight and Obesity by Ethnicity
There were no significant differences in the rates of obesity in terms of ethnicity (Latino vs. African American).
Critical Age Period for Overweight and Obesity
We examined the overweight and obesity prevalence as it progressed with each single-year age group and found that the most significant increases in overweight and obesity occurred in two time intervals: 1–2 years and 2–3 years of age [z score (1–2 years) = −6.9, p < 0.01 and z score (2–3 years) = −4.2, p < 0.01). Between the ages of 1 and 3 years, overweight increased from 3.7% to 16%, and obesity increased from 7.5% to 30.2%. There were no significant differences in the prevalence of overweight or obesity for the 3- to 5-year age groups.
Discussion
This study of low-income minority urban children shows that overweight and obesity start very early in life, with prevalence rates increasing dramatically between the ages of 1 and 3 years. The study findings expand on those of a study of WIC participants in New York City that found a significant increase in prevalence of overweight and obesity between the ages 2 and 3.17 The ages from 1 to 3 may represent a critical age in the development of overweight and obesity, one that may be crucial to target for public health and population-based prevention interventions.
What is happening between the ages of 1 and 3 that could explain the dramatic jump in obesity prevalence at this time? The toddler years represent a major transition period for children with regard to diet and activity. From infancy to toddlerhood, children move from a milk-based diet to one consisting of a variety of solid foods. They also establish food preferences, start feeding themselves, and develop eating behaviors.26 Similarly, physical activity levels change dramatically in this period with the development of ambulation, increased socialization, and increased hours of television or DVD watching. In addition to the influence of the home environment, day-care centers may play a significant role in shaping dietary and activity patterns early in life.
Our study also documented the staggeringly high prevalence of overweight and obesity among this community’s youngest members. The risk of overweight or obesity increased with each successive year of age, and by age 5, more than half the children were overweight or obese. The rates of overweight and obesity in the study population were significantly higher than the national averages at these ages.1,2,17,27,28 This may be explained by the Latino predominance in our sample, the racial/ethnic group with the highest rates of obesity nationwide.1,2,9,10,17,27 However, health outcomes in Latino populations vary by national origin,29 and it is possible that higher rates are found among preschoolers of Dominican origin, the largest Latino group in this community. Dominicans often have mixed racial heritage, and this may also distinguish their obesity trajectories from other Latino groups.30
A major factor contributing to the rapid rise in overweight and obesity in this community may be its location, namely an inner-city, minority community. As in other inner-city communities, this community has areas where the most convenient grocery stores may not carry fresh vegetables, fruits, or even low-fat milk, all of which are recommended to reduce the risk of obesity. In addition, in this community, there is a paucity of playgrounds and parks, particularly ones that are both accessible and considered safe by the community. Families may not have the opportunities to ensure that their children are able to play as actively as is recommended.15,31 Our study findings suggest that living in an inner-city community adds to the risk of early-childhood obesity and that strategies aimed at reducing early-childhood obesity will need to take into consideration the effect of the neighborhood resources and barriers to healthy living.
This study demonstrated a gender difference, with girls having higher rates of overweight and boys having higher rates of obesity. These non-symmetric findings reflect the mixed pattern of weight-associated gender differences among preschoolers in other studies. While some studies have not found any gender-related differences,10,17 others have showed boys7,9 or girls with higher rates.1,2 Gender differences have also been noted in studies regarding parental perceptions of obesity. In a study based on National Health and Nutrition Examination Survey 1988–1994 data, mothers were more likely to misclassify their overweight daughters as “obese” than their sons.32 This finding may reflect greater parental acceptance for boys to be heavier than girls and could result in variable parental practices in managing weight issues in their children.
The findings from our study emphasize the need to start obesity prevention at the earliest stages. These efforts need to be comprehensive and reinforcing across the home, the medical home, day care, nutritional support programs, the community, and the media. In the home, parental modeling and feeding practices play a role in the development of satiety and food preferences,26 but studies are limited by small sample size and lack of cultural context. In addition, further research is needed on exploring what developmental-appropriate interventions are most effective in promoting self-regulation of energy intake in early childhood.33
Although primary-care providers are concerned with obesity, most feel ineffective at preventing obesity and poorly prepared to deal with the overweight or obese child and his/her family.15 Most successful obesity programs are multidisciplinary and have been conducted in academic settings. However, there has been little work adapting successful programs for the fast pace of the primary-care setting, nor has money been made available to cover for the cost of their implementation.34 An additional provider challenge is the clinical controversy of how to approach the management of toddlers under 2 years who are overweight or obese. In recently published guidelines, the Expert Committee recommended decreasing juice and milk intake, offering healthy food choices and, importantly, not restricting total energy intake.15 Therefore, resources are needed to create interventions applicable to the primary-care settings, train providers, and provide funding for the effort required.
The majority of low-income children benefit from the WIC program, and WIC efforts should complement those of primary-care providers. The WIC program, which serves half of US infants and a quarter of US children ages 1–4 years, has recently announced significant positive changes to its nutrition supplements, to be fully implemented in the next 18 months.35 In response to a commissioned Institute of Medicine report,36 WIC packages will eliminate juice through age 12 months, decrease juice and milk allowance after 12 months, allow only low-fat milk after age 2 years, and add a $6 allowance a month for fruit and vegetables—potatoes excluded. These changes may have an impact in preventing obesity, provided the neighborhood stores stock adequate fresh produce, an ongoing challenge for inner-city communities.34,37
Day care is another critical environment that helps shape nutritional and activity patterns in early childhood. Nationwide, a third of children under age 6 attend day care.38 Head Start has mandated nutritional and exercise standards, which can reduce the risk of overweight development, but these are effective only for children 3–5 years of age, after the age group where we have documented the rise in overweight. In addition, Head Start regulations pertain only to these federally regulated programs, and all other day-care facilities, including those serving children from infancy up, are regulated by a widely varying set of standards applied in each state.34 The expansion of federal regulations for healthy food and exercise at Head Start programs to all state-regulated day-care facilities would impact a large number of children, particularly those at younger ages. The integration of improved diet and exercise standards for all child-care settings would be very important for families living in inner-city communities, where there are not enough Head Start program slots and many children are in other forms of family or group day care.
This study has several limitations. Our study was conducted in an inner-city, minority community, and generalization to other communities, particularly non-metropolitan or to other ethnic groups, should be made with caution. BMI reference value standards have not been established for children under 2.15 Therefore, the assessment of overweight and obesity uses one set of measures (weight-for-length percentiles) for 1-year olds, while for 2- to 5-year olds, BMI percentiles were used. This measurement may have affected the calculation of change in overweight and obesity across these age groups. In addition, the cross-sectional design did not allow tracking of individual children.
In conclusion, our study suggests that the ages between 1 and 3 represent a critical age period for the development of obesity among inner-city, minority children. Our study does not permit assessment of the factors contributing to this extraordinary risk of early-childhood obesity in this community, but we think that the limited opportunities for outdoor active play and access to healthy foods may contribute to this risk. Future research should include prospective studies looking at the development of overweight and obesity, along with associated neighborhood, physical, and dietary risk factors for children as they progress through early childhood. This could further define the concept of a critical age period for the development of overweight and obesity and help design culturally and developmentally appropriate population-based interventions to prevent childhood obesity.
References
- 1.Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the centers for disease control and prevention pediatric nutrition surveillance, 1983 to 1995.[see comment]. Pediatrics 1998;101(1):E12. [DOI] [PubMed]
- 2.Ogden CL, Troiano RP, Briefel RR, Kuczmarski RJ, Flegal KM, Johnson CL. Prevalence of overweight among preschool children in the United States, 1971 through 1994. Pediatrics 1997;99(4):E1. [DOI] [PubMed]
- 3.Stettler N, Elliott MR, Kallan MJ, Auerbach SB, Kumanyika SK. High prevalence of overweight among pediatric users of community health centers. Pediatrics 2005;116(3):e381–e388. [DOI] [PMC free article] [PubMed]
- 4.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity 2006;14(2):301–308. [DOI] [PubMed]
- 5.Rappaport EB, Robbins JM. Overweight in Southeastern Pennsylvania children: 2002 household health survey data. Public Health Rep 2005;120(5):525–531. [DOI] [PMC free article] [PubMed]
- 6.Robbins JM, Khan KS, Lisi LM, Robbins SW, Michel SH, Torcato BR. Overweight among young children in the Philadelphia health care centers: incidence and prevalence. Arch Pediatr Adolesc Med 2007;161(1):17–20. [DOI] [PubMed]
- 7.Sherry B, Mei Z, Scanlon KS, Mokdad AH, Grummer-Strawn LM. Trends in state-specific prevalence of overweight and underweight in 2- through 4-year-old children from low-income families from 1989 through 2000. Arch Pediatr Adolesc Med 2004;158(12):1116–1124. [DOI] [PubMed]
- 8.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA 2001;286(22):2845–2848. [DOI] [PubMed]
- 9.Thorpe LE, List DG, Marx T, May L, Helgerson SD, Frieden TR. Childhood obesity in New York City elementary school students. Am J Public Health 2004;94(9):1496–1500. [DOI] [PMC free article] [PubMed]
- 10.Whitaker RC, Orzol SM. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med 2006;160(6):578–584. [DOI] [PubMed]
- 11.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337(13):869–873. [DOI] [PubMed]
- 12.Guo SS, Roche AF, Chumlea WC, Gardner JD, Siervogel RM. The predictive value of childhood body mass index values for overweight at age 35 y. Am J Clin Nutr 1994;59(4):810–819. [DOI] [PubMed]
- 13.Nader PR, O’Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics 2006;118(3):e594–e601. [DOI] [PubMed]
- 14.Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Utility of childhood BMI in the prediction of adulthood disease: comparison of national and international references. Obes Res 2005;13(6):1106–1115. [DOI] [PubMed]
- 15.Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(Suppl 4):S164–S192. [DOI] [PubMed]
- 16.Deckelbaum RJ, Williams CL. Childhood obesity: the health issue. Obes Res 2001;9(Suppl 4):239S–243S. [DOI] [PubMed]
- 17.Nelson JA, Chiasson MA, Ford V. Childhood overweight in a New York City WIC population. Am J Public Health 2004;94(3):458–462. [DOI] [PMC free article] [PubMed]
- 18.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 2005;111(15):1999–2012. [DOI] [PubMed]
- 19.Olson EC, Van Wye G, Kerker B, Thorpe L, Frieden TR. Take Care Inwood and Washington Heights. NYC Community Health Profiles, 2nd ed. 2006;19(42):1–16.
- 20.Community District Profiles, Manhattan Community District 12. NYC Government Website. Available at: http://www.nyc.gov/html/dcp/pdf/lucds/mn12profile.pdf. Accessed on March 24, 2008.
- 21.Perez M, Findley SE, Mejia M, Martinez J. The impact of community health worker training and programs in NYC. J Health Care Poor Underserved 2006;17(1 Suppl):26–43. [DOI] [PubMed]
- 22.Fairbrother G, Stuber J, Dutton M, Scheinmann R, Cooper R. An examination of enrollment of children in public health insurance in New York City through facilitated enrollment. J Urban Health 2004;81:191–205. [DOI] [PMC free article] [PubMed]
- 23.Growthcharts. CDC Website. Available at: http://www.cdc.gov/growthcharts. Accessed on March 24, 2008.
- 24.SPSS 13.0 for Windows [computer program]. Version. Chicago, IL: SPSS Inc.; 2005.
- 25.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc 2004;104(2):215–221. [DOI] [PubMed]
- 26.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics 1998;101(3 Pt 2):539–549. [PubMed]
- 27.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–1555. [DOI] [PubMed]
- 28.Edmunds LS, Woelfel ML, Dennison BA, Stratton H, Pruzek RM, Abusabha R. Overweight trends among children enrolled in the New York State special supplemental nutrition program for women, infants, and children. J Am Diet Assoc 2006;106(1):113–117. [DOI] [PubMed]
- 29.Fuentes-Afflick E. Obesity among Latino preschoolers: do children outgrow the “epidemiologic paradox”?[comment]. Arch Pediatr Adolesc Med 2006;160(6):656–657. [DOI] [PubMed]
- 30.Getaneh A, Michelen W, Findley SE. The prevalence of cardiovascular risk conditions and awareness among a Latino subgroup: Dominicans in Northern Manhattan. Ethn Dis In press. [PubMed]
- 31.Rundle A, Roux AV, Free LM, Miller D, Neckerman KM, Weiss CC. The urban built environment and obesity in New York City: a multilevel analysis. Am J Health Promot 2007;21(4 Suppl):326–334. [DOI] [PubMed]
- 32.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics 2003;111(5 Part 2):1226–1231. [PubMed]
- 33.Johnson SL. Improving Preschoolers’ self-regulation of energy intake. Pediatrics 2000;106(6):1429–1435. [DOI] [PubMed]
- 34.Story M, Kaphingst KM, French S. The Role of Child Care Settings in Obesity Prevention. Available at: http://www.futureofchildren.org/usr_doc/07_5562_story-care.pdf. Accessed on March 6, 2008. [DOI] [PubMed]
- 35.Department of Agriculture, Food and Nutrition Service. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC Food Packages; Interim Rule. Available at: http://www.fns.usda.gov/wic/regspublished/wicfoodpkginterimrulepdf.pdf. Accessed on March 5, 2008.
- 36.United States Department of Agriculture, Food and Nutrition Service, Office of Research N, and Analysis,. WIC Food Packagese, Executive Summary. Available at: http://www.fns.usda.gov/oane/MENU/Published/WIC/FILES/Time4AChange(execsum).pdf. Accessed on March 5, 2008.
- 37.Sloane DC, Diamant AL, Lewis LBYA, et al. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med 2003;18(7):568–575. [DOI] [PMC free article] [PubMed]
- 38.Mulligan GM, Brimhall D, West J. Child Care and Early Education Arrangements of Infants, Toddlers, and Preschoolers: 2001 (NCES 2006-039). Available at: http://nces.ed.gov/pubs2006/2006039.pdf. Accessed on March 6, 2008.