Abstract
We assessed the feasibility of using organizational network analysis in a local public health organization. The research setting was an urban/suburban county health department with 156 employees. The goal of the research was to study communication and information flow in the department and to assess the technique for public health management. Network data were derived from survey questionnaires. Computational analysis was performed with the Organizational Risk Analyzer. Analysis revealed centralized communication, limited interdependencies, potential knowledge loss through retirement, and possible informational silos. The findings suggested opportunities for more cross program coordination but also suggested the presences of potentially efficient communication paths and potentially beneficial social connectedness. Managers found the findings useful to support decision making. Public health organizations must be effective in an increasingly complex environment. Network analysis can help build public health capacity for complex system management.
Keywords: Public health, Complex systems, Network analysis, Organizational theory, Information management.
Introduction
There is a national need to manage public health organizations efficiently and effectively and to augment public health managers’ abilities to build adaptive organizations in an increasingly complex environment.1 Organizations are complex information processing entities in which internal structures and processes evolve contingent upon environmental conditions.2–5 Within an individual public health organization performance is influenced by complex interactions among employees, tasks, specialized knowledge, and resources. Organizational charts and process maps fail to capture these interactions with the result that important aspects of public health work may not be fully managed. Incomplete information also leads to uncertainty, which reduces the organizational managers’ ability to plan and to make the decisions required to achieve a given level of performance.
Network analysis is a means for understanding the complex interactions that occur in organizations. It is a quantitative, descriptive research technique that focuses on relationships among entities such as people, groups, or resources. The technique can help public health managers understand how intraorganizational networks are linked to process and outcomes. These insights can guide the optimal application of limited public resources to improve agency performance. Network analysis is used extensively to understand dynamics within private sector organizations,6,7 but there has been limited application in public sector management.8,9
We conducted a study to assess the feasibility of using organizational network analysis in a local public health department. The goal of the research was to describe the flow of information in the department and assess the technique’s suitability for use in public health management. The network analysis was conducted using the Organizational Risk Analyzer.10 This software is uniquely appropriate for examining organizations because it allows organizational systems to be modeled as interlocking networks of people, knowledge, resources, and tasks.
Materials and Methods
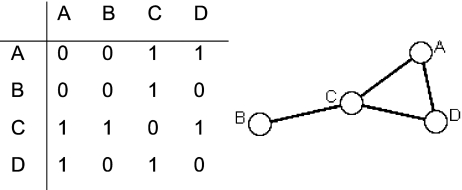
A network comprises a set of nodes connected by edges that represent some relationship between them. These nodes and edges are typically organized into adjacency matrices, where rows and columns represent people or things. Within each cell, numbers represent the presence or absence of an edge (i.e., a relation) or the frequency or strength of a relation. Figure 1 displays a matrix and the resulting graph in which node A (that may represent a person, a group, or some resource like a computer) has a relationship with C and D but no relationship with B. The results of a network analysis are reports containing network measurements and graphical displays depicting the relationships between nodes.
FIGURE 1.
Example of an adjacency matrix representing network relationships with the graph resulting from the data. 1 = relationship, 0 = no relationship.
Setting and Sample The study was conducted in a local health department serving a mixed urban/suburban county with a population of approximately 300,000. At the time of the study, the department consisted of 156 employees within five divisions and nine general program areas. The employees delivered a full range of public health services including environmental services. They represented a range of public health titles and programmatic specialization and adequately represented current public health workforce issues such as an aging workforce. The department was large enough to allow analysis at the program level as well as at the full organizational level.
Data Collection A survey based on conventional network questions to measure work-related relationships and communication11 was administered to every employee (N = 156). The response rate was 93%. Each respondent indicated his/her relationship with all other employees in response to four questions: (1) Do you receive work-related information from each person listed below? (2) To whom do you give work-related information? (3) Who is important in terms of helping you think about complex problems posed by your work? And finally, (4) I understand what knowledge and skills this person has.
Data analysis We used the quadratic assignment procedure (QAP) to determine if the networks produced by the four questions above were correlated. QAP is a method for calculating standard errors in network data.12,13 The analysis yielded fairly high pairwise correlation coefficients between 0.61 and 0.89 (see Table 1). These results raised a concern that the culture of public health, which values inclusiveness, collaboration, and cooperation, is a source of expansiveness bias or has a tendency for individuals to overstate their ties to others.14,15 To mitigate the effect of this bias, the research team elected to examine only the strongest ties between employees. Questions 1, 2, and 3 addressed information exchange, and question 4 addressed transitive knowledge (who knows whom) in the network. Social network research has found transitive knowledge to be a basis for strong ties.16,17 For this reason, we elected to merge the networks produced by all four questions, thus capturing strongest ties across domains as one composite variable. Although merging networks does mean that subtle differences in common links between employees are ignored, we felt these differences addressed issues beyond the goals of this feasibility study.
Table 1.
Pairwise correlations generated from a QAP analysis, which compared the networks generated by four network questions: (1) Do you receive work-related information from each person listed below? (give info); (2) To whom do you give work-related information? (get info); (3) Who is important in terms of helping you think about complex problems posed by your work? (discuss work); (4) I understand what knowledge and skills this person has (know skills)
| Dependent graph | Independent graph | |||
|---|---|---|---|---|
| Give info | Get info | Discuss work | Know skills | |
| Give info | 1.00 | |||
| Get info | 0.89 | 1.00 | ||
| Discuss work | 0.78 | 0.77 | 1.00 | |
| Know skills | 0.66 | 0.65 | 0.61 | 1.00 |
Secondary Analysis To develop networks representing employees’ links to public health tasks, knowledge, and resources, we performed a secondary analysis on data obtained from colleagues conducting an independent but complementary project on workforce competency in which employees reported information about their work.18 These categorical data were binarized to create three matrices: employee × tasks (187 items), employee × knowledge (29 items), and employee × resources (74 items).
Collaborative Formulation of an Analysis Plan A meaningful and accurate network analysis must be a joint effort between the organization’s representatives and those conducting the analysis.19,20 The researchers presented preliminary network measurements and visualizations to the health department’s leaders, and together they established goals for the analysis. For the managers, the goals were to identify patterns of information flow and resource distribution in the programs and divisions and to gain insight into the potential impact of a planned merger of two divisions. The research team requested meetings with the management team to present the completed analysis and to gather feedback to meet the overall study goal to assess the technique’s suitability for use in public health management.
Results
Table 2 describes the set of network measures used to identify patterns of information flow and resource distribution and presents the results. The overall cohesiveness of the network was assessed with network measures of total degree centralization, characteristic path length, density, and complexity. Resource distribution was examined through the measurement of task and resource redundancy and through a simulation to explore the effect of losing staff to retirement. The planned merger was examined by comparing the two divisions before and after a simulated merger.
Table 2.
Organizational level network measures used in the study with definitions, results, and interpretations
| Measure | Definition | Measurement | Interpretation |
|---|---|---|---|
| Centralization | Centralization of the employee communication network based on the total degree centrality of each employee. Reflects the extent that communication is centralized around a single individual or small group | F 0.46, P 0.28–0.50 | Measurements closer to 1 indicate more centralized information flow and hierarchical decision making. Measurements closer to 0 suggest decentralized information flow and decisions made closer to point of service |
| Density | Ratio of the number of links present versus the maximum number of possible links between employees. The measurement is normalized to account for network size | F 0.15, P 0.31–0.65 | Density reflects communication between employees. Density within the programs is much higher than in the full organization, which could mean reduced communication between programs and possible informational “silos” |
| Complexity | A composite measure to approximate interdependencies and integration. It represents the ratio of links present versus the maximum number of possible links in all four matrices (i.e., employee × employee, employee × knowledge, employee × task, and employee × resource) | F 0.21, P 0.26–0.39 | Interdependencies between people tasks, knowledge, and resources in the full organization are 21% of what is possible, and between 26% and 39% in the programs. If interdependencies are too low, there can be a duplication of effort and inefficiency, if too high errors are more likely |
| Characteristic path length | A measure of the typical separation between any two employees in the network. The value is equal to the number of links in the shortest path connecting any two employees, averaged over all pairs of employees | F 2.06, P 1.00–1.76 | An employee can connect with any other employee by going through two people on average. This measure reflects how quickly information can diffuse throughout the network. Networks with short path lengths transmit information efficiently. Long path lengths mean information spreads less evenly |
| Redundancy of resources | Average number of redundant employees per resource. An employee is redundant if there is already an employee with access to the resource | F 51, P 3–10 | Redundancy reflects the degree of system backup and capacity for reliable service under changing conditions. It also can suggest a duplication of effort |
| Redundancy of tasks | Average number of employees assigned to the same tasks. An employee is redundant if there is already an employee with the task | F 24, P 2–6 | There are at least three people in every program with access to the same resource and at least two performing the same tasks |
All measurements are normalized between 0.0 and 1.0, except characteristic path length and redundancy measures.
F Measurement at the full organization level, P range of measurements within the programs
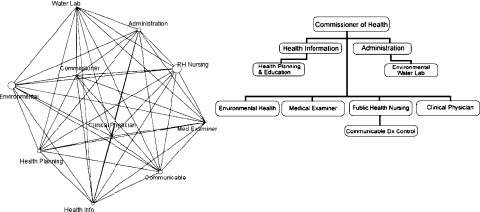
Patterns of Information Flow The network structure at the divisional level displayed in Figure 2 reflects how employees exchange information to do their work. The nonlinear structure of the associations between divisions presents a striking contrast to the directed hierarchy of the traditional organizational chart.
FIGURE 2.
The health department network at the divisional level on the left is compared to the traditional organizational chart. Node size in the network diagram is related to the number of staff in the division. The nonlinear pattern of links between divisions in the network presents a striking contrast to the directed hierarchy of the organizational chart.
Total degree centralization indicates the extent that communication in the agency follows a “command and control” structure. For example, if every employee in the network was only linked to a single “leader” at the center of the network, the centralization would be 1.0. Centralization at 0.46 in the agency network and between 0.28–0.50 in the programs suggest that in some areas communication and decisions tend to be controlled by a central group.21 The characteristic path length is the average number of links required for information to pass from one person to another. An average path length of 2 (i.e., two people) for the organization suggests there is potential for rapid information diffusion throughout the organization.22
Density and complexity characterize cohesiveness of the network on two levels. Density compares existing links to all possible links in the employee information network and reflects organizational cohesion at the social or interpersonal level.21 Density of the agency overall at 15% is lower than at the program level (31–64%), reflecting less communication between programs than within programs. Complexity compares existing links to all possible links in all four networks (employees, task, knowledge, resource) and reflects interdependencies among the organization’s components that allow economies of scale and more cohesive structure.20,23 The overall complexity score for the agency (0.21) and scores for individual programs (0.28–0.39) are below 40%. While we do not know the optimum level of complexity for a public health organization, several of the programs demonstrate a pattern of social density exceeding complexity. This may indicate information silos causing duplication of effort, particularly if employees are unaware of activities elsewhere in the department that are related to their work.24
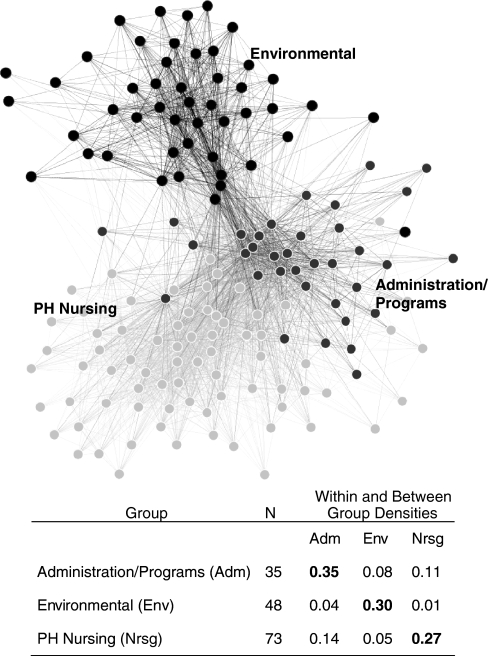
Visualizations showed the department’s network clustered around a central core, with no isolated employees or pendant groups of employees. Employees located toward the periphery of the network were largely frontline staff working in one of two branch offices. We used Newman’s modularity algorithm to explore subgroups in the network. This algorithm reflects the degree to which a network has found community structure by calculating the number of edges falling within groups minus the expected number in an equivalent network with edges placed at random.25 Modularity scores above 0.30 indicate there are cohesive subgroups. The analysis resulted in a modularity score of 0.31 and found three subgroups. The largest (n = 73) was composed of employees in public health nursing services and related programs such as communicable disease control; a second group (n = 48) was composed of employees in environmental health services; and a third group (n = 35) was composed of employees in administration and programs such as health education. The health department network showing subgroups and densities within and between groups are displayed in Figure 3. The proportion of links among employees within each subgroup was between 0.27 and 0.35 (i.0 27–35% of the number of possible links), much higher than the density of the full department (0.15). Between-group employees in the administration/programs group had 8% of possible links with the environmental group and 11% of possible links with the PH nursing group. Employees in the Environmental group had only 4% of possible links with administration/programs and only 1% of possible links to PH nursing. Employees in the PH nursing group had 14% of possible links with the administration/programs and only 5% of links to the environmental group. These findings reflect much lower information flow between subgroups, particularly between the environmental subgroup and the other parts of the organization.
FIGURE 3.
A graphical depiction of three cohesive subgroups located using Newman’s modularity algorithm with a table indicating the size of the groups and the density of links within (bolded) and between these groups.
Resource Distribution Redundancy measures the proportion of employees who perform the same task or have access to the same resources and reflects capacity for performing in the face of absences, personnel loss, or rapidly changing conditions. The preferred level of redundancy in public health organizations is unknown. More than 50 of 156 employees use the same resources to do their work, and 24 employees perform the same tasks. All programs have at least two employees with similar access to resources and similar task capacity or assignment.
Retirement is a significant issue for local public health due to an aging public health workforce.26 We simulated the effect of staff attrition by separately removing supervisory staff and senior employees with experience greater than 20 years from the network. There were marked decreases in network complexity and social density. Centralization of the network doubled with the removal of senior staff, suggesting that groups missing senior staff would be less capable of autonomous decision making. Centralization was halved with removal of supervisors, suggesting that some groups would be less likely to get information needed for work.
Analysis of the Planned Merger To assess the impact of the merger, measurements for the two unmerged divisions were compared to those for the merged divisions. Redundancies in access to resources and task assignment increased. Density in the two separate divisions of 0.35 and 0.57 was reduced to 0.32 when the divisions were merged. Moderate reductions in density such as this have been shown to aid network performance.27 Total degree of centrality of individual employees (a measure of their influence in the network) in the merger showed a potential loss of influence for key employees in the smaller of the two divisions.
Value for Public Health Management The health department scheduled a series of meetings for the researchers to present results and gather feedback on the value of the analysis from the health department’s management team. Feedback was recorded by taking notes during the meeting. The management team reported considerable value in the analysis. The findings afforded insights into organizational processes that suggested possible redeployment of resources. For example, through examining density and complexity measurement within and between programs, managers understood that more efficient processes might be achieved through increased integration of people, tasks, knowledge, and resources throughout the organization. The managers found that the findings could inform their efforts to support personnel in addressing priorities that were part of the health department’s strategic planning process. They determined that the organization needed to do more cross-training of new staff to address two strategic priorities: assure the capacity to provide essential services and provide opportunities to increase knowledge and skills necessary for employees to perform their jobs. To increase communication between programs, managers proposed workgroups with tasks that cut across program areas to address another strategic priority: enhance efficiency through effective information distribution. The initial target of this strategy was cross-programmatic emergency preparedness activities. The managers also indicated they would like to identify appropriate levels of redundancy for the department.
The impact of potential retirements was a priority finding. Although the management team was aware of this potential prior to the network analysis, they were galvanized by observing the effect on cohesiveness in the network when experienced and senior employees were removed. To ensure that key expertise would be transferred, they decided to initiate mentoring relationships to pair junior staff with experienced staff. The simulation of a divisional merger demonstrated a shift in the network position of key employees, which alerted managers that they might need to head off possible “political” implications resulting from potential changes in influence.
Discussion
This study used organizational network analysis to describe empirically the intraorganizational networks in one local health department and demonstrated feasibility of the technique as a support for public health management. Health department managers who are expert in the science and practice of public health may have little formal background in organizational management. We documented that the management team engaged in this study uncovered significant insights to support their management decisions from visualizing, measuring, and interpreting the relational dynamics in the department. These insights led the managers to take formal steps to ensure that knowledge transfer occurred between senior and junior staff and to institute cross-training and cross-programmatic teams to address limited information exchange between programs. They gained insight into the dynamics of an upcoming merger of two divisions and have begun to consider the issue of appropriate redundancies for their organization.
The network analysis demonstrated the presence of three subgroups that correspond to broad programmatic areas in public health. Organizational theorists observe that organizations typically consist of dense, minimally overlapping subgroups that integrate with the larger organization through contacts outside the boundaries of the group.28–32 Of particular note was limited integration of environmental services, the implications of which cannot be determined in the absence of a comparative study of local health departments.
The department exhibited a centralized network structure; whether this is optimal for a local public health department is not known. Theories of collective action in network research suggest that centralized networks are more likely to be successful in achieving common good functions.33 Centralized organizations use a top-down model of decision making vs. decentralizing authority closer to the point of service. This is effective when the central core uses its tight connections to manage resources and integrate tasks, but centralized structures can risk overburdening those at the center with too much information while underutilizing the abilities of peripheral members.24,34,35 Programs with mobile field staff might perform best with a highly centralized structure, but too much centralization can prevent a unit from exercising discrete task resolution and forming interunit ties.20,36
In this health department, lower overall measurements of complexity (links between the organization’s components) were coupled with high social density (links between employees) in the programs. The interpretation of complexity and density measurement depends on the nature of the work. For example, multifaceted work in a dynamic environment typically requires a more cohesive organization than repetitive work in a very stable environment.37 Low complexity and high density is a marker for informational silos, which are tightly vertically integrated teams in which individuals tend to work closely together but have limited interactions with other parts of the organization (other silos).38 Silos are associated with poor communication and duplicative problem solving that can make organizations less efficient and adaptable. Based on this analysis, the department’s managers embraced strategies to increase complexity such as creating cross-functional teams and encouraging teamwork through tasks that require distributed decision making, both of which create an incentive for employees to collaborate and share information.39 These approaches can motivate individuals and groups away from the silo mentality and toward communicating horizontally.40
Relatively dense connections among employees are a possible strength for the department because dense connections can enhance coordination, increase productivity, and reduce errors. This density is mirrored in a short characteristic path length that suggests information can circulate quickly so employees are more likely to receive information close to the same time. This can contribute to satisfaction if, for example, employees feel they are getting the information they need in a timely way. Managers need to be aware that high density can also result in rumor propagation and a tendency for groups to evaluate their actions less critically.41,42 In some groups reduced network density results in more effective performance because there is more opportunity for information to come from outside the group.43
The determination of appropriate levels of redundancy in public health organizations is challenging. Public sector managers must document carefully how redundancy contributes to process improvement and more reliable service to avoid accusations of wastefulness.44 Yet, organizational performance can hinge on the reliability and efficiency created by adequate redundancy of tasks and resources.2 For example, parallel information pathways that overlap in functional areas and create ordered channels for information duplication are a way to build redundancy.45 This strategy could make sense for public health organizations, as fragmented information lodged in programmatic silos is an acknowledged cause of inefficiency.46–48 To determine the need for redundancy, program directors and managers could define the types of performance breakdowns that are likely to occur in their programs. By identifying gaps that are stressing cooperative working relationships, they can target where to develop channels for aggregating and accessing information and resources that overlap across programs.49
Conclusion and Further Study
The purpose of a network model is to organize theoretical beliefs by identifying important system aspects with empirical observations.50 The findings from this study document that a local health department’s network structure exhibits features common to other organizations. Local health department networks may also demonstrate common features that are shared across departments. If these features affect the functioning of each organization, this may have system-wide implications. The presence of a distinct environmental subgroup is an example; we found low integration of the environmental health services subgroup that may have a relationship to organizational effectiveness, efficiency, or performance. If this is a general feature of local health departments (which is consistent with informal observations by authors), then planning and resource management for the entire public health system could be affected. Evidence of information silos was an expected finding of a potential problem but may also reflect necessary aspects of public health work that can be ascertained through further network studies. The higher densities found within divisions may reflect redundant information pathways that positively influence organizational performance, as some network research suggests.27
The dynamics within organizations can obscure the determinants of performance because interactions among the multiple elements that comprise an organization are difficult to comprehend.51,52 For example, consider how difficult it has been for the public health practice community to measure performance across local health departments that vary in structure and composition due to local decisions.53 Yet, these departments have consistent missions and perform essentially similar work.54 Network analysis presents a means to see past administrative differences by capturing how public health workers actually interact to get their work done. The insights into organizational structure afforded by network analysis can provide decision support to build public health managers’ capacity for complex system management. For example, results can be applied locally to gauge performance, to assess organizational adaptability to changing conditions, to inform planning and resource allocation, to identify vulnerabilities and risk in organizational structures, and to contribute to root cause analysis of recognized problems or successes.
To make it easier to execute network analysis in support of public health managerial practice, we have developed a standard network survey with a minimum data set derived from practice documentation to capture employee relationships to public health tasks, knowledge, and resources. We are modifying the existing software program to produce reports specifically designed to meet the needs of public health managers to support management decisions in the workplace. A comparative study of several local agencies will establish baseline network measurements for public health organizations. We will correlate network measures with system performance to produce a broader exploration of how public health organizational networks are linked to process and outcomes.55
Acknowledgments
The study was funded by National Library of Medicine N01-LM-1-3521 and National Institute of Nursing Research P20 NR 007799. This work was supported in part by CASOS—the Center for Computational Analysis of Social and Organizational Systems at Carnegie Mellon University. Development of the ORA tool used for analysis was supported by Office of Naval Research N00014-06-0104. The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied of the Office of Naval Research or the US government.
References
- 1.Salinsky E, Gursky S. The case for transforming governmental public health. Health Aff. 2006;25(4):1017–1028. [DOI] [PubMed]
- 2.Galbraith J. Organization design: an information processing view. Interfaces. 1974;4:28–36.
- 3.Galbraith J. Organization Design. Reading, MA: Addison-Wesley; 1977.
- 4.March JG, Simon HA. Organizations. New York: Wiley; 1958.
- 5.Simon HA. Rational decision making in business organizations. Am Econ Rev. 1979;69:493–513.
- 6.Borgatti SP, Foster PC. The network paradigm in organizational research: a review and typology. J Manage. 2003;29(6):991. [DOI]
- 7.Brass DJ, Galaskiewicz J, Greve HR, Tsai W. Taking stock of networks and organizations: a multilevel perspective. Acad Manage J. 2004;47(8):795–817.
- 8.Agranoff R, McGuire M. Managing in network settings. Policy Stud Rev. 1999;16:18–41. [DOI]
- 9.Eisenberg M, Swanson N. Organizational network analysis as a tool for program evaluation. Eval Health Prof. 1996;19(4):488–506. [DOI] [PubMed]
- 10.Center for Analysis of Social and Organizational Systems. ORA: Organizational Risk Analyzer Version 1.9. Pittsburgh: Center for Analysis of Social and Organizational Systems, Carnegie Mellon University; 2008 [computer program].
- 11.Cross R. Organizational Network Analysis. http://www.robcross.org/sna.htm. Accessed February 1, 2005.
- 12.Hubert LJ, Schultz J. Quadratic assignment as a general data analysis strategy. Br J Math Stat Psychol. 1976;29:190–241.
- 13.Krackhardt D. QAP Partialling as a test of spuriousness. Soc Netw. 1987;9:171–186. [DOI]
- 14.Feld SL, Carter WC. Detecting measurement bias in respondent reports of personal networks. Soc Netw. 2002;24(4):365–383. [DOI]
- 15.Marsden PV. Recent developments in network measurement. In: Carrington PJ, Scott J, Wasserman S, eds. Models and Methods in Social Network Analysis. New York: Cambridge University Press; 2005.
- 16.Burt RM. The social capital of structural holes. In: Guillen MF, Collins R, England P, Meyer M, eds. New Directions in Economic Sociology. New York: Russell Sage Foundation; 2001.
- 17.Granovetter M. Economic action and social structure: the problem of embeddedness. Am J Soc. 1985;91(3):481–510. [DOI]
- 18.Cunningham DJ, Ascher MT, Viola D, Visintainer PF. Baseline assessment of public health informatics competencies in two Hudson Valley health departments. Public Health Rep. 2007;122(3):302–310. [DOI] [PMC free article] [PubMed]
- 19.Chang M, Harrington JE. Agent-based models of organizations. In: Handbook of Computational Economics II: Agent-based Computational Economics. http://www.econ.jhu.edu/People/Harrington/HCE9-04.pdf. Accessed December 12, 2006.
- 20.Scott J. Social Network Analysis: A Handbook. London: Sage; 2000.
- 21.Wasserman S, Faust K. Social Network Analysis: Methods and Applications. Cambridge: Cambridge University Press; 1994.
- 22.Milgram S. The small-world problem. Psychol Today. 1967;2:60–67.
- 23.March JG. Exploration and exploitation in organizational learning. Organ Sci. 1991;2(1):71–87.
- 24.Podolny JM, Page KL. Network forms of organization. Annu Rev Soc. 1998;24:56–76.
- 25.Newman MEJ. Fast algorithm for detecting community structure in networks. Phys Rev. 2004;69:066133. [DOI] [PubMed]
- 26.Association of State and Territorial Health Officials(ASTHO). State Public Health Employee Worker Shortage Report: A Civil Service Recruitment and Retention Crisis. http://www.astho.org/pubs/Workforce-Survey-Report-2.pdf. Accessed November 1, 2006.
- 27.Uzzi B, Spiro J. Collaboration and creativity: the small world problem. Am J Soc. 2005;111:447–504. [DOI]
- 28.Blau P. Inequality and Heterogeneity: A Primitive Theory of Social Structure. New York: Free; 1977.
- 29.Freeman LC. The sociological concept of group: an empirical test of two models. Am J Soc. 1992;98:152–166. [DOI]
- 30.Granovetter M. The strength of weak ties: a network theory revisited. Soc Theory. 1983;1:201–233. [DOI]
- 31.Simmel G. Conflict and the Web of Group Affiliations. Glencoe, IL: Free; 1955.
- 32.Simon HA. The Shape of Automation for Men and Management. New York: Harper & Row; 1965.
- 33.Kilduff M, Tsai W. Social Networks and Organizations. London: Sage; 2003.
- 34.Miller JH. Evolving information processing organizations. In: Lomi A, Larson ER, eds. Dynamics of Organizations: Computational Modeling and Organizational Theory. Menlo Park, CA: AAAI; 2001.
- 35.Mizruchi MS, Stearns LB. Getting deals done: the use of social networks in bank decision making. Am Soc Rev. 2001;66:647–671. [DOI]
- 36.Tsai W. Social structure of cooperation within a multi-unit organization. Organ Sci. 2002;13(2):179–190. [DOI]
- 37.Flap H, Bulder B, Beate V. Intra-organizational networks and performance: a review. Comput Math Organ Theory. 1998;4(2):109–147. [DOI]
- 38.Doerscher T. Teamwork Design for Success. http://www.chiefprojectofficer.com. Accessed November 1, 2005.
- 39.VonFoerster H. On self-organizing systems and their environments. In: Yovitts MC, Cameron S, eds. Self-organizing Systems. New York: Pergamon; 1960.
- 40.Goh S. Managing effective knowledge transfer: an integrative framework and some practice implications. J Knowledge Manage. 2002;6(1):23–30. [DOI]
- 41.Festinger L. A Theory of Social Comparison Processes. Hum Relat. 1954;7(2):117–140. [DOI]
- 42.Janis I. Victims of Groupthink: A Psychological Study of Foreign-Policy Decisions and Fiascoes. Boston: Houghton Mifflin; 1972.
- 43.Valente TW, Chou CP, Pentz MA. Community coalition networks as systems: effects of network change on adoption of evidence-based prevention. Am J Public Health. 2007;97(5):880–886. [DOI] [PMC free article] [PubMed]
- 44.Rainey HG. Comparing public and private organizations: empirical research and the power of the a priori. J Public Adm Res Theory. 2000;10:447–469.
- 45.Lerner AW. There is more than one way to be redundant: a comparison of alternatives the design and use of redundancy in organizations. Adm Soc. 1986;18(3):334–359. [DOI]
- 46.Koo D, Morgan M, Broome C. New means of data collection. In: O’Carroll PW, Yasnoff WA, Ward ME, Ripp LH, Martin EL, eds. Public Health Informatics and Information Systems. Indianapolis: Springer; 2002:379–407.
- 47.Lasker R, Humphreys B, Braithwaite W. Making a Powerful Connection: The Health of the Public and The National Information Infrastructure. Washington, DC: US Public Health Services, Public Health Data Policy Coordinating Committee; 1995.
- 48.Lee P, Giuse NB, Sathe NA. Benchmarking information needs and use in the Tennessee public health community. J Med Libr Assoc. 2003;91(3):322–336. [PMC free article] [PubMed]
- 49.Landau M. Redundancy rationality and the problem of duplication overlap. Public Adm Rev. 1969;39:346–358. [DOI]
- 50.Loerch A. Stochastic Models. http://mason.gmu.edu/~aloerch/Model_Intro.pdf. Accessed March 1, 2005.
- 51.Radzicki MJ. Introduction to System Dynamics: A Systems Approach to Understanding Complex Policy Issues. Washington, DC: US Department of Energy. http://www.albany.edu/cpr/sds/DL-IntroSysDyn/start.htm. Accessed December 1, 2005 [Internet Version 1.0].
- 52.Sterman JD. Business Dynamics: Systems Thinking and Modeling for a Complex World. Boston: Irwin McGraw Hill; 2000.
- 53.Turnock B, Handler A. Performance measurement and improvement. In: Novick LF, Mays GP, eds. Public Health Administration. Gaithersburg, MD: Aspen; 2001.
- 54.National Association of City and County Health Officials (NACCHO). Operational Definition of a Functional Local Public Health Agency. http://www.naccho.org/. Accessed December 1, 2006.
- 55.Robert Wood Johnson Foundation. RWJF Announces New Investments in the Field of Public Health Systems Research. http://www.rwjf.org/newsroom/newsreleasesdetail.jsp?productid=21928. Accessed January 12, 2007.