Abstract
We present a case of massive pneumoperitoneum in association with pneumatosis intestinalis that was successfully managed without surgery despite a clinical picture of an acute abdomen and biochemical evidence of inflammation and systemic upset. Recognition of non-surgical pneumoperitoneum is important to avoid unnecessary laparotomy, and clinical examination for the presence of peritonitis is the most important determinant of the need for emergency surgery.
Keywords: Pneumoperitoneum, Pneumatosis intestinalis, Conservative management
Pneumoperitoneum requires emergency laparotomy in 90% of cases1 although there are many causes of free intraperitoneal air which can be managed conservatively. An important non-surgical cause of benign pneumoperitoneum is pneumatosis intestinalis; these cases are usually only mildly symptomatic.
Pneumatosis intestinalis was first characterised in 1730, and is the term used for pockets of gas within the bowel wall; it is a radiological finding rather than a specific diagnosis.2 Around 15% of cases are idiopathic or primary (usually termed pneumatosis cystoides intestinalis), and the remainder are due to a variety of conditions including bowel ischaemia or obstruction, connective tissue diseases, necrotising enterocolitis, medications (immuno-suppressants, chemotherapy, steroids) and obstructive pulmonary disease; over 58 causative factors have been identified.2 Regardless of underlying cause, the condition can be associated with free intraperitoneal, retroperitoneal or portal venous air, even in the absence of bowel perforation. In these cases, the air is either due to rupture of the intramural air cysts into the peritoneal space or due to air tracking from elsewhere (such as the lungs, if seen in association with pulmonary disease).
This creates a diagnostic dilemma for the surgeon, who must decide whether emergency surgery to repair a bowel perforation is indicated. Pneumoperitoneum in the absence of bowel perforation is usually asymptomatic or presents with minor abdominal symptoms without severe pain. We present a case of non-surgical pneumoperitoneum in association with pneumatosis intestinalis which manifested as an acute abdomen with severe systemic upset and biochemical evidence of inflammation.
Case report
A 35-year-old man presented with a 1-day history of frequent vomiting, abdominal distension and severe generalised abdominal pain. He had had a previous laparotomy, apparently for bowel obstruction, and also gave a history of weight loss over the preceding weeks. On examination, he was clinically dehydrated with a pulse rate of 146 beats/min, blood pressure of 124/80 and a temperature of 36.4°C. Abdominal examination revealed a distended abdomen with generalised palpation tenderness; rebound tenderness and guarding were absent. Bowel sounds were present and digital rectal examination was normal with stool in the rectum.
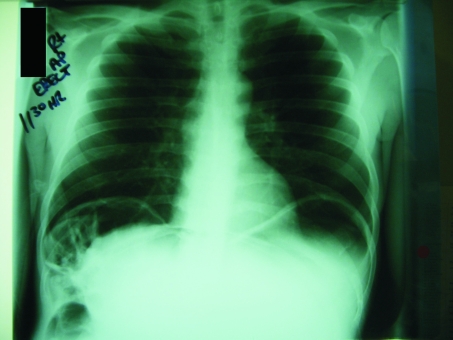
Blood tests revealed markedly raised inflammatory markers (white cell count 33.2 × 109 per litre, C-reactive protein 33 mg/l), haemoconcentration with acute renal impairment (haemoglobin 20.1 g/dl, platelets 617 × 109 per litre, urea 14.1 μmol/l, creatinine 352 μmol/l), deranged liver function tests (bilirubin 48 μmol/, aspartate transaminase 168 U/l, alkaline phosphatase 92 U/l) and normal amylase (34 U/l). Arterial blood sampling revealed alkalosis (pH 7.656), with low PaCO (4.31 kPa), normal PaO2 (12.5 kPa), lactate 9.6 mmol/l and bicarbonate 38.9 mmol/l. Erect chest radiograph revealed large amounts of air under the diaphragm bilaterally (Fig. 1); abdominal radiography was unremarkable. After discussion with the consultant on call, preparations were made for laparotomy.
Figure 1.
Erect chest radiograph showing large amounts of air under the diaphragm bilaterally.
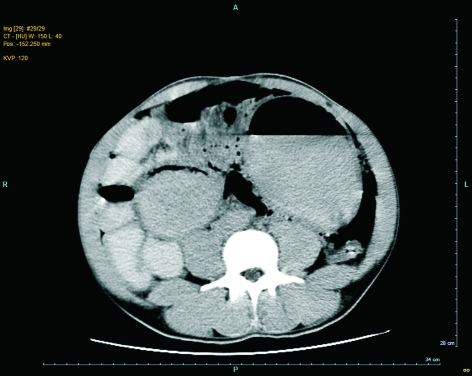
Subsequent further discussion revealed a previous diagnosis of pneumatosis cystoides intestinalis, discovered at laparotomy for bowel obstruction; he had undergone a gastrojejunostomy for benign pyloric stenosis 5 years previously. In view of this information, a computed tomography (CT) scan of the abdomen was performed (Fig. 2), which showed free intraperitonal air and intramural gas pockets in the small intestine, with no focal perforation seen.
Figure 2.
Abdominal CT scan showing free intraperitonal air and intramural gas pockets in the small intestine, with no focal perforation.
He was admitted and treated with intravenous fluids and antibiotics. Strict fluid balance monitoring was undertaken and a nasogastric tube passed, the patient being kept nil-by-mouth. He improved over the following 8–10 h and was treated conservatively.
After 3 days, his inflammatory markers had improved and his renal function normalised with fluid resuscitation; the renal dysfunction was, therefore, presumed due to dehydration. Oral intake was re-introduced, and he was discharged home to complete the course of oral antibiotics.
Discussion
Pneumoperitoneum, or air within the peritoneal cavity, is an important finding that in 90% of cases signifies perforation of the bowel.1 It can also result from thoracic causes (obstructive pulmonary diseases, pneumothorax, pneumomediastinum), abdominal causes (connective tissue diseases, subclinical or sealed perforated viscus, pneumatosis intestinalis), gynaecological causes (coitus, pelvic inflammatory diseases, recent vaginal examination), and iatrogenic causes (cardiopulmonary resuscitation, mechanical ventilation, oesophageal perforation, peritoneal dialysis, retained air from recent surgery, endoscopy, vaginal insufflation).3 It is primarily diagnosed radiologically, with air seen under the diaphragm on erect chest radiography, and outlining the bowel wall or forming air pockets on plain abdominal radiography. Computed tomography is only marginally more sensitive than plain radiography, which is able to detect 1–2 ml of free intraperitoneal air.3 Even CT scan, however, is often unable to determine the site of the perforation and, if this is suspected, emergency surgery should not be delayed.
Pneumoperitoneum is a common complication of pneumatosis intestinalis, and in primary pneumatosis may be massive and recurrent. This is usually asymptomatic but in less than 15% of cases can present with symptoms and signs ranging from mild abdominal pain to an acute abdomen, as here.3 However, many conditions leading to the development of pneumatosis intestinalis can also cause bowel perforation and so this must be excluded.
In recent years, there has been growing consideration given to the conservative management of pneumo-peritoneum,1,3 even following bowel perforation.5 Identification of cases in which laparotomy can be avoided is important to prevent unnecessary surgery with its associated morbidity and financial costs; in one literature review, 61 of 139 patients with benign pneumoperitoneum underwent unnecessary laparotomy.3 Despite efforts to formulate an objective algorithm to identify those cases of pneumoperitoneum that can be conservatively managed,1 the decision to proceed to emergency surgery remains subjective and is based on assessing symptomatology, clinical findings, laboratory results and imaging studies.
In the case described here, the presentation was with an acute abdomen. Clinically and biochemically there was evidence of inflammation and systemic upset, and there was radiological evidence of massive pneumoperitoneum. Had there been evidence of peritonitis on clinical examination, laparotomy to identify the site of perforation would have been the next step. An unnecessary operation was, therefore, prevented by careful clinical examination combined with recognition of a benign pneumoperitoneum.
Conclusions
Benign pneumoperitoneum usually presents with painless abdominal distension and normal laboratory findings,1 and most previous reports of conservatively managed pneumoperitoneum have been asymptomatic or complained only of minor abdominal pain. Here we present a case of symptomatic and painful pneumoperitoneum with evidence of severe dehydration and inflammation that was successfully managed conservatively. Thorough clinical examination remains the best way to assess the presence of peritonitis and is the most important determinant of the need for emergency surgery, in this case being the sole negative finding that prevented an unnecessary laparotomy.
References
- 1.Hoover EL, Cole GD, Mitchell LS, Adams CZ, Hassett J. Avoiding laparotomy in nonsurgical pneumoperitoneum. Am J Surg. 1992;164:99–103. doi: 10.1016/s0002-9610(05)80363-0. [DOI] [PubMed] [Google Scholar]
- 2.Pear B L. Pneumatosis intestinalis: a review. Radiology. 1998;207:13–9. doi: 10.1148/radiology.207.1.9530294. [DOI] [PubMed] [Google Scholar]
- 3.Mularski RA, Ciccolo ML, Rappaport WD. Nonsurgical causes of pneumoperitoneum. West J Med. 1999;170:41–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Baker SR. Unenhanced helical CT versus plain abdominal radiography: a dissenting opinion. Radiology. 1997;205:45–7. doi: 10.1148/radiology.205.1.9314960. [DOI] [PubMed] [Google Scholar]
- 5.Songne B, Jean F, Foulatier O, Khalil H, Scotte M. Non operative treatment for perforated peptic ulcer: results of a prospective study. Ann Chir. 2004;129:578–82. doi: 10.1016/j.anchir.2004.06.012. [DOI] [PubMed] [Google Scholar]