Abstract
INTRODUCTION
The management of an efficient acute surgical service with conflicting pressures of managing elective and emergency work, compounded by waiting list targets and the maximum 4-h wait for patients in accident and emergency poses a significant challenge. We assess the impact of appointing a dedicated emergency surgeon on the delivery of our emergency surgery service.
PATIENTS AND METHODS
A comparative retrospective review was undertaken of all surgical admissions (n = 1622) over a 9-month period (between February and November) in the year before and after (2004 and 2005) the appointment of a dedicated emergency surgeon. The impact on service, training and possible financial consequences of this appointment was assessed.
RESULTS
A total of 798 surgical admissions in 2004 were compared with 824 admissions in 2005 for the 9-month periods of this study. In 2004, 258 patients were operated on compared with 286 in 2005 (NS). There was a significant increase in day-time operating from 57% in 2004 to 74% in 2005 (P < 0.001) and a significant increase in consultant-supervised operations from 14% to 52% (P < 0.001), with a consequent fall in out-of-hours operating (43% to 26%; P < 0.001). In addition, there was a significant increase in early (within 48 h) discharges from 41% to 53% (P < 0.001). The salary of the new appointment is more than offset by the quantifiable savings of approximately £90,000 per annum based on the increased proportion of earlier discharges alone as well as the improved quality of care provided.
CONCLUSIONS
The appointment of a dedicated emergency surgery consultant has resulted in an increase in day-time consultant-supervised operating, shorter hospital stay for emergency admissions, improved training for surgical trainees, as well as providing potential financial savings for the trust.
Keywords: Audit, Emergency surgery, Resources
The conflicting pressures of managing elective and emergency work with waiting list targets and the maximum of 4-h wait for patients in accident and emergency (4-h breaches) makes the management of an efficient acute surgical service a difficult challenge. The problem is compounded in trusts providing a tertiary referral service across more than one site. Individual trusts identify their own solutions depending on the number of surgeons, their specialist interests and the emergency work-load. However, there are significant opportunities to improve the delivery of emergency surgical care.
In the current NHS climate, the efficient use of surgical resources is essential. A number of studies have highlighted the increase in the number of emergency admissions over the past decades.1–3 This increases the strain on resources and is compounded by the pressures to meet UK Government targets for elective work.4 The volume of emergency surgical admissions has an impact on waiting times in accident and emergency, 4-h breaches, and patient satisfaction. A falling threshold for hospital admission and increasingly inexperienced junior trainees reluctant to refuse admissions leaves a potential for an increase in inappropriate admissions.5 Delays in senior surgical review and decision-making result in longer hospital stay and inefficient use of resources.
Continuity of care by the admitting team is essential to reassure the patient, avoid repetitive history taking, examination and investigations. Shift patterns of working led by the European Working Time Directive (EWTD) and the decreasing experience of surgeons in training have the potential for interrupting continuity of care, delaying the treatment of the patient and introducing errors of communication.
Historically, the emergency service has been provided by an on-call team (consultant, registrar [SpR] and/or senior house officer [SHO]), who in addition to elective commitments also accommodate the emergency work.
We present an approach to these issues by the appointment of a dedicated consultant surgeon to provide a weekday emergency surgery service between 8 am and 5 pm. The aim was to ensure a fast track for referrals, diagnosis, early discharge or prompt day-time emergency surgery.
This study has evaluated the impact of this new post on the availability of service provision to the patient, the training implications for trainees, and the possible financial impact of the new service.
Patients and Methods
A consultant surgeon (NEM) was appointed in February 2005 with responsibility for the emergency surgical service between 8 am and 5 pm Monday to Friday with no fixed elective commitments. A 15-bed Surgical Assessment Unit (SAU) similar in structure to those established in other hospitals6–8 was created to accommodate all emergency surgical admissions from all surgical specialities. The consultant rota is divided between eight (max part-time and part-time) surgical consultants (6.5 whole time equivalents) who cover between 5 pm and 8 am. Day-time registrar cover is available either from a registrar (PS) solely committed to emergency work or the registrar of the admitting team if they are free from fixed commitments.
Patient pathway
Referrals from the accident and emergency department are made to the surgical registrar carrying the general surgery on-call bleep. If unavailable to see the patient within 30 min, the dedicated consultant surgeon is called. All patients are assessed by a consultant/SpR within 30 min of referral, and a decision to admit to the SAU or discharge from accident and emergency back to GP care is made. Investigations are instigated and reviewed promptly. There is a dedicated theatre available for surgical emergencies. We aimed to ensure that all minor emergency operations were performed within 12 h of admission to allow discharge on the same day.
Patients from our second site are transferred directly to SAU following senior surgical review for further surgical investigations and treatment.
All emergency general surgical admissions were studied retrospectively over a 9-month period between February and November 2004 and 2005. Information on all emergency admissions and operations were provided by hospital databases (Trisoft – Theatreman; ECIMS). This was substantiated with theatre diaries and clinical records. Comparison between the study periods in 2004 and 2005 was made concerning: (i) number of admissions; (ii) length of stay; (iii) timing of emergency operations; (iv) level of the operating surgeon; and (v) type of operation performed. The financial consequences derived by the new method of emergency surgery service provision were estimated on the basis of cost per 24-h patient episode and increase in discharges within 24–48 h. Statistical analysis on proportionate data was calculated using the chi-square test.
Results
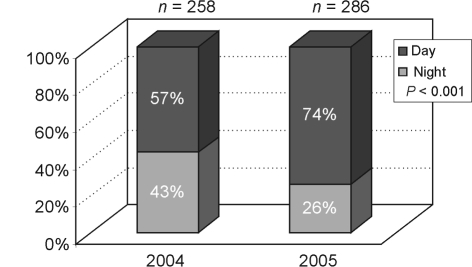
Emergency admissions represented 29% of the general surgical workload for 2005 over the 9-month period for this study. There was a small increase in emergency surgical admissions with a total of 798 admissions in 2004 compared to 824 in 2005 for the 9-month study periods (NS). Of these, 32% (258 patients) were operated on in 2004 compared to 35% (286 patients) in 2005 (NS: Fig. 1).
Figure 1.
Time of operation.
Day-time emergency surgery
There was a significant increase in emergency operations performed during the day (between 8 am and 5 pm) in the 9-month study period from 57% (146 operations) in 2004 to 74% (211 operations) in 2005 (P < 0.001; Fig. 1).
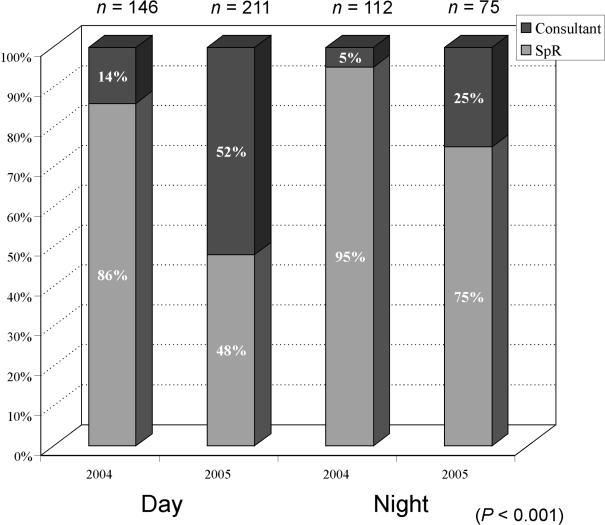
There was a significant increase in day-time consultant-supervised operations from 14% (20 operations) in 2004 to 52% (110 operations) in 2005 (P < 0.001; Fig. 2).
Figure 2.
Level of supervision day and night.
Of the 20 consultant-led operations in 2004 performed during the day, 70% were laparotomies. Of the 110 consultant-led operations during the day in 2005, 30% were laparotomies, 30% appendicectomies, 30% others (abscess drainage, examination under anaesthetic, etc.) and 10% hernia operations.
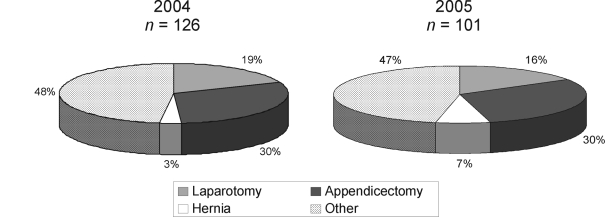
During the 9-month period in 2004, 86% (126 operations) of SpR-led operations were unsupervised during the day. In 2005, this decreased to 48% (101 operations)(Fig. 2). The breakdown of the operations performed by SpRs is shown in Figure 3.
Figure 3.
SpR operations: day.
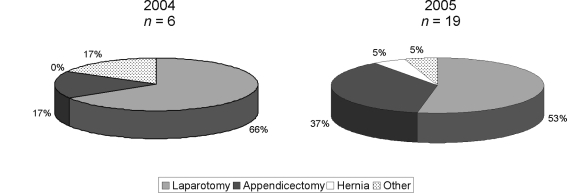
Out-of-hours emergency surgery
There was a consequent significant decrease in the total number of operations performed out-of-hours, with 43% (112 operations) performed between 5 pm and 8 am in 2004 compared to 26% (75 operations) in 2005 (P < 0.001; Fig. 1). Of these, 5% (6 operations) were consultant-led in 2004 and 25% (19 operations) in 2005. Similar proportions were laparotomies (66% in 2004 compared to 53% in 2005), but larger proportions were appendicectomies (17% in 2004 compared to 37% in 2005;: Fig. 4). SpR-led operations during the night fell from a total of 106 (95%) in 2004 to 56 (75%) in 2005 (P < 0.001)(Fig. 2).
Figure 4.
Consultant led operations: out-of-hours.
Discharges
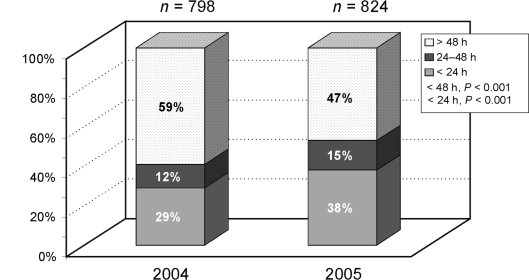
There was a significant increase in 24-h discharges from 29% in 2004 to 38% in 2005 (P < 0.001), as well as 48-h discharges from 41% to 53% (P < 0.001; Fig. 5).
Figure 5.
Time to discharge.
Financial implications
The cost of one patient-occupied-bed per day in London is approximately £495.8 If the discharge rate for our service is 38% compared to 29% in 2004, the resultant 9% increase in discharges within 24 h, and 3% increase in discharges between 24–48 h equates to an estimated saving of approximately £90,000 per annum.
There was a reduction in number of 4-h breaches from 74 in 2004 to 38 in 2005.
Discussion
The delivery of a high-quality emergency service that provides accurate diagnosis and prompt treatment of the acute surgical patient improves outcomes. We have invested in a consultant-led week-day emergency service in an effort to rationalise acute surgical admissions across two sites, thus providing early senior opinion and clinical decision-making without disrupting elective specialist work.
Traditional patterns of working have meant that many patients in accident and emergency often have had to wait for a senior surgical opinion when available and free from fixed elective commitments. When senior opinions are not immediately available, the target of a 4-h maximum wait in accident and emergency has led to inappropriate investigations or admissions. Hospitals with higher emergency work loads and numbers of surgical consultants can ameliorate this problem by commitment to an on-take week. However, in trusts providing a tertiary referral service with smaller emergency work-loads, this inefficient use of consultant time impacts on the delivery of elective care.
Impact on service
Our emergency work-load (29%) from two sites remains lower than trusts not providing specialist services which, from previous studies looking at district general hospital emergency surgical admissions, has been around 50%.9,10 The increase in number of admission between 2004 and 2005 in our study period has been small (3.3%). The major impact of the new appointment on the delivery of service has been on: (i) the increase of day-time operating (57% to 74%); (ii) shorter hospital stay; and (iii) ensured continuity of care. Involvement of a senior clinician minimises delays in access to imaging, endoscopy and the operating theatre, and early daily review of all surgical emergencies has facilitated prompt diagnosis and early management decisions. Early completion of minor or intermediate operations has meant that the proportion of patients discharged within 48 h has risen from 41% to 53%. Prompt discharge has allowed this service to be managed despite a 17% reduction11 in the total number of beds.
Consultant availability has resulted in a significant reduction in operations performed by surgical trainees unsupervised. The reduction in out-of-hours operating is in line with National Confidential Enquiry into Patient Outcome and Death (NCEPOD) guidelines and the European Working Time Directive (EWTD); it has increased the availability of SpRs for a prompt opinion in accident and emergency. This has resulted in almost halving (74 to 38) the number of 4-h breaches.
Impact on training
Our concerns that this appointment might detract from the experience of surgical trainees were unfounded. Indeed, we have shown that the level of supervision has increased and opportunities for training junior surgeons have been enhanced by this appointment.
With the increased need for teaching and exposure to surgical emergencies, the concentration of acute surgical admissions to the SAU provides excellent educational opportunities for trainees, together with a consultant free of other commitments available to supervise and teach.
With the reduction in trainee hours to comply with the New Deal MMC and EWTD directives for surgical trainees, registrars coming through the system are now less experienced in the assessment of emergency admissions and in emergency surgery. This is reflected in the increased number of minor and intermediate operations undertaken out-of-hours under consultant supervision, even for appendicectomies (from 17% to 37%).
In a climate where there is increasing tendency to early specialisation, the position of consultant emergency surgeon offers significant opportunities to individuals who have, or are seeking, a broader scope of general surgical exposure.
Financial impact
This new post is primarily an investment in the quality of the emergency service as well as the training and supervision of surgical trainees. However, the financial implications are important and must be considered. The salary of the new appointment is more than offset by the quantifiable savings of approximately £90,000 per annum based on the increased proportion of earlier discharges alone. There are, in addition, unquantifiable savings such as decreased cost of out-of-hours operating, reduced number of unnecessary investigations, and prompt diagnosis and surgery that have to be taken into consideration.
Conclusions
The model of a dedicated emergency surgeon represents an effective and efficient emergency surgery service which has had a major positive impact on the management of emergency surgical patients as well as improved training for trainees and more efficient use of hospital resources.
References
- 1.Capewell S. The continuing rise in emergency admissions. BMJ. 1996;312:991–2. doi: 10.1136/bmj.312.7037.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chezhian C, Pye J, Jenkinson LR. The next millennium – are we becoming emergency surgeons? A seven year audit of surgical and urological admissions in a rural district general hospital. Ann R Coll Surg Engl. 2001;83:117–20. [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell WB, Lee EJK, Van de Sijpe K, Gooding J, Cooper MJ. A 25-year study of emergency surgical admissions. Ann R Coll Surg Engl. 2002;84:273–7. doi: 10.1308/003588402320439739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dookeran KA, Bain I, Moshakis V. Audit of general practitioner referrals to a surgical assessment unit: new methods to improve the efficiency of the acute surgical service. Br J Surg. 1996;83:1544–7. doi: 10.1002/bjs.1800831115. [DOI] [PubMed] [Google Scholar]
- 5.Gaskell DJ, Crosby DL, Fenn N, Lewis PA, Roberts CJ, Roberts SM. Improving the primary management of emergency surgical admissions: a controlled trial. Ann R Coll Surg Engl (Suppl) 1995;77:239–41. [PubMed] [Google Scholar]
- 6.Mohammed MS, Mufti GR. The surgical assessment unit – effective strategy for improvement of the emergency surgical pathway? J R Soc Med. 2005;98:14–7. doi: 10.1258/jrsm.98.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watkin DLF, Layer GT. A 24-hour snapshot of emergency general surgery in the UK. Ann R Coll Surg Engl (Suppl) 2002;84:194–9. [Google Scholar]
- 8.Hammersmith Hospitals NHS Trust Finance Department
- 9.Rowe PH, Lawrence WT, Fellows E. The management of emergency surgical patients in a surgical assessment unit. Ann R Coll Surg Engl (Suppl) 2003;85:274–7. [Google Scholar]
- 10.Currie IC, Earnshaw JJ, Heather BP. Cutting the cost of emergency surgical admissions. Ann R Coll Surg Engl (Suppl) 1996;78:180–3. [PubMed] [Google Scholar]
- 11.Hammersmith Hospitals NHS Trust Surgery and Anaesthetics database