Abstract
INTRODUCTION
The merit of using D-dimer estimations in patients following total hip and knee replacement has been previously questioned. A survey of radiology protocols in 70 hospitals ascertained that the test continues to be mandatory in 51 prior to formal radiological investigation of suspected deep vein thrombosis (DVT) in this patient population.
PATIENTS AND METHODS
In this study, D-dimer levels were measured pre-operatively and during the first 7 days following primary total hip and knee replacement to estimate the range of normal values in these patients.
RESULTS
All 78 patients were ultrasonographically shown to be clear of DVT. D-Dimer levels were significantly raised in all patients at all measurements during the first week. Levels after total knee replacement were higher than after total hip replacement. Comparison was made with an age-matched group who had a proven DVT. There was no difference in D-dimer levels between patients with or without a DVT.
CONCLUSIONS
The use of this test in this patient group is a waste of resource and merely delays appropriate radiological investigation and treatment.
Keywords: D-Dimer, Deep vein thrombosis, Total hip replacement, Total knee replacement
Measurement of plasma D-dimer levels has been shown as a useful diagnostic aid in suspected deep vein thrombosis (DVT) in medical patients.1,2 Previous studies have shown that the test may also be useful to exclude the presence of DVT following general abdominal surgery.4,5 Its role in the investigation of DVT in patients undergoing major orthopaedic surgery including total hip replacement (THR) and total knee replacement (TKR) remains controversial.6,7 The test is, however, frequently mandatory in the UK prior to definitive radiological investigations to investigate DVT.
In this prospective study, we aimed to determine the normal range of plasma D-dimer concentration in patients undergoing elective total hip and knee arthroplasty in the first 7 days following surgery. We also compared these levels with those in patients with a known DVT following total joint replacement.
Patients and Methods
All patients under the care of one consultant orthopaedic surgeon who were listed for primary hip or knee arthroplasty for osteoarthritis were eligible for the study. Those with a previous history of thrombo-embolism and those at high risk for thrombo-embolism were excluded. Any patient who received LMWH or other chemical prophylaxis during their in-patient stay and those who were found to have a DVT during admission were also excluded. This left 78 patients for analysis.
The study was approved by the regional ethics committee and all patients gave written, informed consent.
All TKRs were performed using a tourniquet, which was inflated prior to commencing surgery and deflated after application of the dressings. Total hip replacements consisted of cemented (n = 28) and hybrid (n = 11) designs. Postoperative DVT prophylaxis was in the form of a Flowtron calf pump applied to the opposite leg in theatre and of bilateral foot-pumps applied immediately following surgery and continued until discharge. An attempt was made to commence mobilisation on the first postoperative day.
Plasma D-dimer levels were measured in all patients pre-operatively and postoperatively on days 1, 3, 5 and 7. All tests were carried out within 3 h of obtaining the samples. All study patients underwent duplex ultrasound scanning of both lower limbs on day 7 postoperatively by the same consultant radiologist to confirm the absence of thrombus.
A separate analysis was carried out on 43 patients with radiologically proven DVT following 16 THRs and 27 TKRs. All these patients had D-dimer estimation prior to their DVT being diagnosed.
We contacted 70 radiology departments to ascertain whether a D-dimer test was mandatory prior to radiological investigation of suspected DVT in patients following hip and knee replacement.
Statistical analysis
All data were recorded and analysed using Microsoft Excel spreadsheet. Unpaired t-tests were used to analyse the differences between groups and a P-value of < 0.05 was considered statistically significant.
Results
Seventy-eight patients completed the study. Thirty-nine patients underwent primary THR (28 cemented, 11 hybrid) and 39 an uncemented TKR.
There were an equal number of male and female patients in the groups. The mean (SD) age at the time of the index procedure was 70 (9.3) years
The mean (SD) D-dimer value pre-operatively was 0.59 (0.31) mg/l with a median value of 0.57 mg/l.
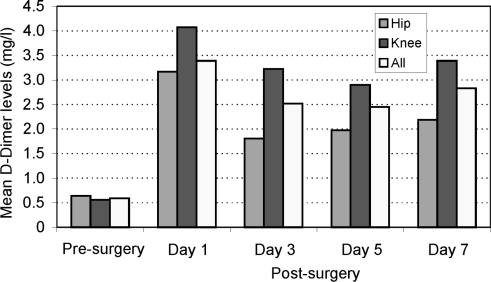
In the first week after surgery, the D-dimer level was raised on every measurement. The highest levels were on days 1 and 7 but even the lowest mean, on day 5, was over 3 times the pre-operative level (Fig. 1). This pattern was seen in both the THR and TKR patients although on days 3, 5 and 7 the levels were significantly higher in the TKR patients (Table 1).
Figure 1.
Mean D-dimer levels pre- and post-surgery.
Table 1.
D-Dimer levels in the study group showing differences between THR and TKR patients
| Day | Total group | THR | TKR | Significance of difference between THR and TKR |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | P-value | ||
| Presurgery | 0.59 (0.31) | 0.64 (0.32) | 0.56 (0.32) | NS |
| 1 | 3.39 (2.72) | 3.17 (2.05) | 4.07 (3.20) | NS |
| 3 | 2.52 (2.26) | 1.81 (1.32) | 3.22 (2.74) | 0.007 |
| 5 | 2.45 (1.41) | 1.98 (0.95) | 2.90 (1.63) | 0.008 |
| 7 | 2.83 (1.58) | 2.19 (0.84) | 3.39 (1.85) | 0.003 |
NS, not significant.
Comparison was made with a historical group of age-matched patients who had been diagnosed with DVT following hip or knee arthroplasty at our institution. Of the 43 patients with a DVT, 16 were diagnosed on or before day 7. The mean (SD) D-dimer in this group was 2.7 (0.76) mg/l.
Our survey of radiology departments in hospitals that performed hip and knee replacement surgery confirmed that D-dimer estimation was mandatory in 51 (73%) of 70 departments.
Discussion
Postoperative DVT is a well-recognised complication following THR and TKR and can be difficult to diagnose clinically due to the presence of lower limb swelling and pain as a result of the surgery. Prompt diagnosis and treatment is essential to avoid clot propagation and pulmonary embolism.
Plasma D-dimer is a specific fibrin degradation product and has been shown to be a useful tool in the diagnosis of DVT in certain patient groups. A normal level effectively rules out a DVT; however, elevated levels do not accurately confirm the diagnosis because of its poor specificity. Hip and knee arthroplasty like all major surgery activates the fibrinolytic system, giving rise to elevated levels of plasma D-dimer in postoperative patients.10
Currently, estimation of the D-dimer level is commonly required by radiology departments in patients with a joint replacement prior to venography. This was confirmed by our survey of 70 hospitals in the UK of which 51 followed the above protocol.
The aim of this study was to ascertain the normal levels of D-dimer in a group of patients undergoing hip and knee arthroplasty without DVT. We felt that knowledge of this new ‘normal’ would aid in determining whether the test has a role in diagnosing thrombo-embolism in this patient group. Testing was restricted to the first week as this is the time that most patients are in hospital in our institution. Patients who develop symptoms in the weeks following discharge following surgery are often admitted under a physician and the orthopaedic surgeon is frequently unaware of anything untoward until the next orthopaedic out-patient visit. This made extending the study beyond the first week difficult.
The present study confirmed a significant increase in the mean postoperative D-dimer level on all days it was measured during the first postoperative week as compared with the mean pre-operative value. The elevated levels followed a similar trend to that found by Shiota et al.,7 i.e. a double-peaked distribution with peaks at days 1 and 7 postoperatively. However, the study of Shiota et al.7 included primary and revision cases and those with and without DVT, including some with pre-operative DVT.
We also found that, although the pattern of rise in postoperative levels was the same in the THR and TKR groups, the TKR group showed significantly higher mean D-dimer levels on days 3, 5 and 7 as compared to the THR group. Shiota et al.7 also noted this difference but only on day 1 postoperatively. It has been suggested by McKenna et al.13 that the local mechanical effect of the tourniquet and resultant ischaemia during TKR may be responsible.
Although the primary aim of the study was to show what the normal D-dimer range was after hip and knee replacement, we felt that comparison with a group of patients who had a proven DVT was of interest given the wide-spread policy of insisting on the test prior to definitive investigation of thrombo-embolism. There was no statistical difference between the elevated postoperative D-dimer levels in our study group when compared with the group of radiologically confirmed DVT cases; however, given the relatively small numbers, we no more than suggest that these groups are indistinguishable in terms of their D-dimer level. It is, therefore, difficult to predict a threshold level whereby a diagnosis of DVT can be confirmed with any degree of certainty. These findings differ from those of Shiota et al.7 and Bongard et al.11 but are consistent with the results of Dunn et al.6 who, although noting that a combined measurement of D-dimer over a number of days may differentiate between patients with and without DVT, stated that individual measurements in this patient group were not predictive of thrombo-embolism.
Conclusions
This study indicates that D-dimer levels are always elevated for a week postoperatively following total hip or knee arthroplasty in the absence of a DVT. Levels in those patients with a DVT cannot be differentiated from those without. The use of this test in this patient group is a waste of resource and merely delays appropriate radiological investigation and treatment.
Acknowledgments
The authors would like to thank Dr Pauline Cook and Dr David Donaldson for their help in the conduct of this study.
References
- 1.Gaffney PJ, Edgell T, Creighton-Kempsford LJ, Wheeler S, Tarelli E. Fibrin degradation product (FnDP) assays: analysis of standardization issues and target antigens in plasma. Br J Haematol. 1995;90:187–94. doi: 10.1111/j.1365-2141.1995.tb03399.x. [DOI] [PubMed] [Google Scholar]
- 2.Lip GYH, Lowe GDO. Fibrin D-dimer: a useful clinical marker of thrombogenesis? Clin Sci. 1995;89:205–14. doi: 10.1042/cs0890205. [DOI] [PubMed] [Google Scholar]
- 3.Bournameaux H, Miron MJ, Blanchard J, De Moerloose P, Hoffmeyer P, Leyvraz PF. Measurement of plasma D-dimer is not useful in the prediction or detection of postoperative deep vein thrombosis in patients undergoing total knee arthroplasty. Blood Coag Fibrinol. 1998;9:749–52. doi: 10.1097/00001721-199811000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bournameaux H, Khabiri E, Huber O, Schneider PA, Didier D, De Moerloose P, et al. Value of liquid crystal thermography and plasma D-dimer for screening of deep vein thrombosis following general abdominal surgery. Thromb Haemost. 1992;67:603–6. [PubMed] [Google Scholar]
- 5.Rowbotham BJ, Whitaker AN, Harrison J, Murtaugh P, Reasbeck P, Bowie EJW. Measurement of cross linked fibrin degratives in patients undergoing abdominal surgery: use in the diagnosis of postoperative venous thrombosis. Blood Coag Fibrinol. 1992;3:25–31. doi: 10.1097/00001721-199202000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Dunn I, Hui A, Triffitt P, Crozier A, Gregg P, Sinclair M, et al. Plasma D-dimer as a marker of postoperative deep vein thrombosis. Thromb Haemost. 1994;72:663–5. [PubMed] [Google Scholar]
- 7.Shiota N, Sato T, Nishida K, Matsuo M, Takahra Y, Mitani S, et al. Changes in LPIA D-dimer levels after total hip or knee arthroplasty relevant to deep vein thrombosis by bilateral ascending venography. J Orthop Sci. 2002;7:444–50. doi: 10.1007/s007760200077. [DOI] [PubMed] [Google Scholar]
- 8.Leutz DW, Stauffer S. Color duplex Doppler ultrasound scanning for detection of deep venous thrombosis in total knee and hip arthroplasty patients. J Arthroplasty. 1994;9:543–8. doi: 10.1016/0883-5403(94)90103-1. [DOI] [PubMed] [Google Scholar]
- 9.Haines ST, Bussey HI. Diagnosis of deep vein thrombosis. Am J Healthsyst Pharm. 1997;54:66–74. doi: 10.1093/ajhp/54.1.66. [DOI] [PubMed] [Google Scholar]
- 10.Sharrock N, Go G, Harpel P, Ranawat C, Sculco T, Salvati E. Thrombogenesis during total hip arthroplasty. Clin Orthop. 1995;319:16–27. [PubMed] [Google Scholar]
- 11.Bongard O, Wicky J, Peter R, et al. D-Dimer plasma measurement in patients undergoing major hip surgery. Use in the prediction and diagnosis of postoperative proximal vein thrombosis. Thromb Res. 1994;74:487–93. doi: 10.1016/0049-3848(94)90269-0. [DOI] [PubMed] [Google Scholar]
- 12.Dahl OE, Aspelin T, Arnesen H, Seljeflot I, Kierulf P, Ruyter R, et al. Increased activation of coagulation and formation of late deep venous thrombosis following discontinuation of thromboprophylaxis after hip replacement surgery. Thromb Res. 1995;80:299–306. doi: 10.1016/0049-3848(95)00180-y. [DOI] [PubMed] [Google Scholar]
- 13.McKenna R, Bachmann F, Kaushal SP, Gallante JO. Thromboembolic disease in patients undergoing total knee replacement. J Bone Joint Surg Am. 1976;58:928–32. [PubMed] [Google Scholar]
- 14.Well PS, Brill-Edwards P, Stevens P, Panju A, Patel A, Douketis J, et al. A novel and rapid whole blood assay for D-dimer in patients with clinically suspected deep vein thrombosis. Circulation. 1995;91:2184–7. doi: 10.1161/01.cir.91.8.2184. [DOI] [PubMed] [Google Scholar]
- 15.Perrier A, Desmarais S, Miron MJ, de Moerloose P, Lepage R, Slosman D, et al. Non-invasive diagnosis of venous thromboembolism in outpatients. Lancet. 1999;353:190–5. doi: 10.1016/S0140-6736(98)05248-9. [DOI] [PubMed] [Google Scholar]