The authors have re-implanted the coeliac axis to ensure adequate vascularisation of the upper abdominal viscera as a part of pancreaticoduodenectomy. This and various other techniques of dealing with an intra-operative diagnosis of either coeliac stenosis or occlusion have been described earlier.1 However, the additional morbidity of major vascular reconstruction procedure needs to be carefully considered. With the availability of thin-slice CT scanning, it should be possible to make a pre-operative diagnosis of coeliac stenosis or occlusion either by direct visualisation of the trunk or by indirect means (abnormally large collaterals). Developments in endovascular stenting technology and expertise allow not only peripheral arterial stenting, but aortic, cerebral and visceral (including mesenteric) arterial revascularisation.2 Thus, if there is a suspicion of occlusion or stenosis on pre-operative CT, mesenteric angiography can also be performed with a view to endovascular stenting prior to performing a pancreaticoduodenectomy. Even if the diagnosis of coeliac occlusion was made intra-operatively, retrograde stenting should still be considered if interventional vascular expertise is available.3
One of our recent patients being worked up for a pancreaticoduodenectomy to treat a pancreatic head malignancy was found to have a coeliac occlusion, detected on staging CT scanning. The give away was an abnormally enlarged gastroduodenal artery (Fig. 1). The diagnosis was confirmed by arteriography and pre-operative endovascular stenting of the coeliac trunk was performed (Fig. 2). At surgery, there was no difference in the CHA pulse or Doppler pressures and waveforms before and after clamping the gastroduodenal artery due to an adequate hepatic arterial inflow from the stented coeliac artery. This technique also allows single-stage pancreaticoduodenectomy with perhaps less morbidity than re-implantation of a major visceral artery.
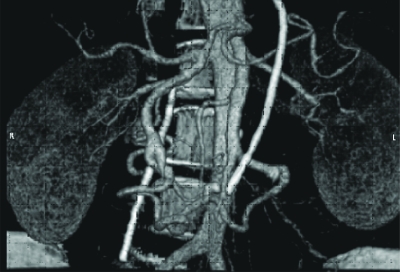
Figure 1.
Reconstruction of CT images demonstrating hypertrophic and enlarged gastroduodenal and pancreaticoduodenal arteries.
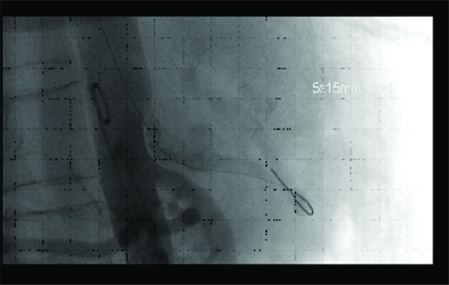
Figure 2.
Endovascular stenting across coeliac occlusion.
Footnotes
COMMENT ON doi 10.1308/147870807X160344 Z Soonawalla, A Ganeshan, P Friend. Celiac artery occlusion encountered during pancreatic resection: a case report. Ann R Coll Surg Engl 2007; online case report
References
- 1.Berney T, Pretre R, Chassot G, Morel P. The role of revascularization in celiac occlusion and pancreatoduodenectomy. Am J Surg. 1998;176:352–6. doi: 10.1016/s0002-9610(98)00195-0. [DOI] [PubMed] [Google Scholar]
- 2.Atkins MD, Kwolek CJ, LaMuraglia GM, Brewster DC, Chung TK, Cambria RP. Surgical revascularization versus endovascular therapy for chronic mesenteric ischemia: a comparative experience. J Vasc Surg. 2007;45:1162–71. doi: 10.1016/j.jvs.2007.01.067. [DOI] [PubMed] [Google Scholar]
- 3.Wyers MC, Powell RJ, Nolan BW, Cronenwett JL. Retrograde mesenteric stenting during laparotomy for acute occlusive mesenteric ischemia. J Vasc Surg. 2007;45:269–75. doi: 10.1016/j.jvs.2006.10.047. [DOI] [PubMed] [Google Scholar]