Abstract
Objective
Evaluate whether, in a primary care setting, Caucasians (C) and African Americans (AA) with moderately to severely disabling migraines differed in regards to: utilizing the health-care system for migraine care, migraine diagnosis and treatment, level of mistrust in the health-care system, perceived communication with their physician, and perceived migraine triggers.
Background
Research has documented ethnic disparities in pain management. However, almost no research has been published concerning potential disparities in utilization, diagnosis, and/or treatment of migraine. It is also important to consider whether ethnic differences exist for trust and communication between patients and physicians, as these are essential when diagnosing and treating migraine.
Methods
Adult patients with headache (n = 313) were recruited from primary care waiting rooms. Of these, 131 (AA = 77; C = 54) had migraine, moderate to severe headache-related disability, and provided socioeconomic status (SES) data. Participants completed measures of migraine disability (MIDAS), migraine health-care utilization, diagnosis and treatment history, mistrust of the medical community, patient–physician communication (PPC), and migraine triggers. Analysis of covariance (controlling for SES and recruitment site), chi-square, and Pearson product moment correlations were conducted.
Results
African Americans were less likely to utilize the health-care setting for migraine treatment (AA = 46% vs. C = 72%, P < .001), to have been given a headache diagnosis (AA = 47% vs. C = 70%, P < .001), and to have been prescribed acute migraine medication (AA = 14% vs. C = 37%, P < .001). Migraine diagnosis was low for both groups, and <15% of all participants had been prescribed a migraine-specific medication or a migraine preventive medication despite suffering moderate to severe levels of migraine disability. African Americans had less trust in the medical community (P < .001, η2 = 0.26) and less positive PPC (P < .001, η2 = 0.11). Also, the lower the trust and communication, the less likely they were to have ever seen (or currently be seeing) a doctor for migraine care or to have been prescribed medication.
Conclusions
Migraine utilization, diagnosis, and treatment were low for both groups. However, this was especially true for African Americans, who also reported lower levels of trust and communication with doctors relative to Caucasians. The findings highlight the need for improved physician and patient education about migraine diagnosis and treatment, the importance of cultural variation in pain presentation, and the importance of communication when diagnosing and treating migraine.
Keywords: migraine, ethnicity, health-care disparities, utilization, migraine diagnosis and treatment, patient–physician communication
The Institute of Medicine (IOM) defines healthcare disparities as “racial or ethnic differences in the quality of health care that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.”1 The IOM’s recent report “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care”1 highlighted health-care disparities across an array of acute and chronic disease conditions,1–7 even after accounting for socioeconomic status (SES), insurance coverage, age, and comorbidities.1,8 The identification of minority health disparities, including migraine, is a priority of the National Institutes of Health (NIH)9 and at the National Institute of Neurological Disorders and Stroke within NIH.10 Research into potential ethnic disparities in pain management have consistently found evidence of disparities in acute pain, cancer pain, and chronic pain.11–16 For example, non-Caucasians are less likely than Caucasians to be prescribed analgesics.14–16
Little research has investigated potential disparities in migraine care. More Caucasians (20%) than African Americans (16%) have migraines;17 this is likely due to variations in genetic vulnerability.17 Thus, one would expect ethnic differences in health-care utilization for migraine care. However, an analysis of National Hospital Ambulatory Health Care Survey data found that 91% of those presenting for care were Caucasians compared to 6% African Americans.18 After accounting for population and migraine prevalence group differences, African Americans were 67% less likely to present for care than would be expected. This suggests a disparity in utilizing care. One common rationale given for differences in utilization rates is access to care.8,19,20 However, there are examples of disease entities where different ethnic groups with the same access to care differ in utilizing the health-care system.21,22 One way to correct this is to compare individuals with similar access to health care.
In addition to utilization, it is important to consider whether ethnic differences exist for managing migraine. A recent study found that African Americans, Hispanics, and Caucasians responded similarly to triptans.23 Thus, one would expect treatment regimens (eg, prescribing migraine-specific medications or migraine preventive medications as appropriate) to be similar. However, an observation of ethnic differences in treatment regimens would not necessarily imply intention on the part of the physician or the health-care system. It is possible that patient–physician communication (PPC) and/or level of trust influences the care individuals receive. It appears that ethnic minorities are more skeptical of the health-care system1,24,25 and have a more negative view of perception of PPC.26
Transparent, trusting communication is essential for efficacious disease management. This need is heightened in migraine and other pain disorders where there is no viable external measure (eg, MRI, blood test) available to establish the presence or severity of pain that is more reliable or valid than the patient’s report to their physician. Any breakdown in PPC will negatively impact treatment quality in pain disorders. Thus, when evaluating potential ethnic disparities in migraine care, it is important to assess not only whether migraineurs of different ethnicities access and receive equitable care, but also whether they have similar perceptions of trust and communication regarding their health-care provider.
It has been proposed by some that disparities are a simple result of environmental or genetic differences. For example, SES (commonly associated with income, education, or employment) contributes to healthcare disparities.1,27–29 However, ethnic health-care disparities exist even after controlling for SES.24,29 Others have suggested that disparities in prescriptions of pain medication are due to ethnic differences in pain perception and need for pain medication. However, in pain patients who are able to control the amount of medication they receive, there are no ethnic differences.16
The purpose of the current study was to evaluate whether Caucasians and African Americans with moderately to severely disabling migraines differed in regards to: (a) utilization of the health-care system for headache treatment; (b) physician-guided diagnosis and treatment for migraine; (c) mistrust in the healthcare system and perceived communication with their physician; and (d) perceived headache triggers. The local Institutional Review Board approved the protocol for the current study.
METHODS
Participants and Procedures
Initially, 313 adult patients with headache were recruited from 3 primary care practices in a large midwestern metropolitan area. Individuals were recruited in the waiting room of these practices and were required to identify themselves as experiencing at least one headache a month. This method was selected over contacting only those who were known to the practice as headache patients since the purpose of the current study was to identify healthcare utilizers who may or may not be headache care utilizers. This also ensured that “lack of access” did not threaten the validity of the results. The questionnaires were completed anonymously.
In order to identify individuals with symptoms consistent with migraine, individuals answered questions about their headaches using diagnostic criteria outlined by the International Classification of Headache Disorders-II (ICHD-II30). Individuals also completed the Migraine Disability Assessment Scale (MIDAS31–34), questions about their headache treatment history, prescription medication use for treating and preventing headaches, a measure of mistrust of the health-care system, questions about communication with their physician, demographic questions, and perceived migraine triggers.
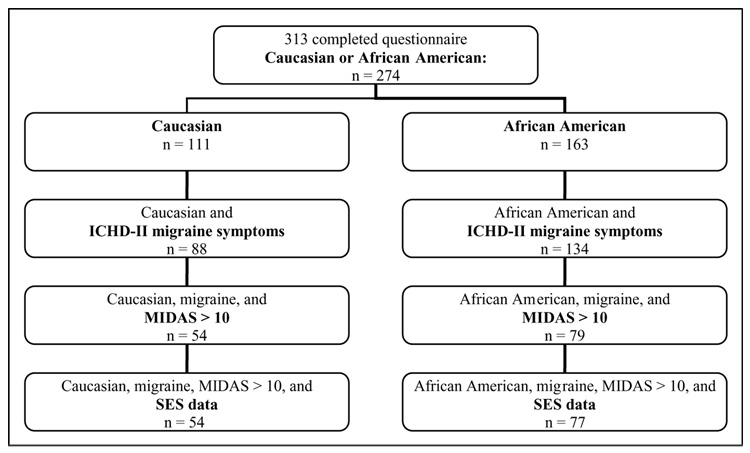
When investigating potential ethnic differences in regards to health-care utilization, diagnosis, and treatment patterns for migraine, it is important to identify those most likely to benefit from physician-guided treatment; specifically, those with at least a moderate level of migraine-related disability. Those most likely to benefit are those who experience at least a moderate level of migraine-related disability.35,36 Given that the purpose of the current study was to look at those who would benefit from physician-guided treatment, individuals were required to report at least a moderate level of headache-related disability as measured by the MIDAS31–34 to be included in the analyses. Also, since SES is an important factor in disparities, individuals were required to provide SES data. Figure 1 shows the numbers that met these criteria for both Caucasians (n = 54) and African Americans (n = 77) at each step.
Fig 1.
Flow chart showing how many individuals met each level of inclusion requirement.
Measures
Headache Screening Questionnaire
Individuals answered questions that covered the diagnostic criteria outlined by the ICHD-II30 for primary migraine headache (eg, moderate to severe pain lasting 4 to 72 hours, experiencing nausea/vomiting or photo/phonophobia, unilateral, throbbing pain, pain worsened by activity). This screening questionnaire has been used in a previously published study37 to ascertain symptoms of migraine.
Headache Characteristics
Participants completed self-report measures of headache pain frequency, duration, and intensity based on procedures outlined by the International Headache Society.38 Specifically, individuals reported how many days a month they experience headaches, headache pain severity (0 = no headache pain; 1 = mild headache pain, can do normal activity; 2 = moderate headache pain, disturbing but not prohibiting normal activity, no need to lie down and rest, and 3 = severe headache pain, normal activity has to be discontinued, may have to lie down and rest), the length of a typical headache, and the number of years they had experienced headache.
Migraine Disability Questionnaire
Headache-related disability was assessed using the MIDAS, a 5-item self-report measure designed to quantify headache-related disability during the past 3 months.31–34 Results categorize the individual into 1 of 4 levels of disability (minimal/infrequent, mild/infrequent, moderate, severe). The MIDAS has strong internal consistency, test–retest reliability, and validity. In order to qualify for inclusion in the study, individuals had to report at least a moderate level of disability.
Health-Care Utilization for Headache Care
Individuals answered questions about utilizing the health-care system for headache care. The questions were based on the National Health Information Survey39 and the Medical Expenditures Panel Survey.40 Individuals answered yes/no to the following: (a) “Have you ever seen a primary care doctor for treatment of your headaches?” and (b) “Headache specialists are doctors who specialize in headache care. They may be neurologists, pain specialists, or a different doctor whose specialty is treating headaches. Have you ever seen a headache specialist for treatment of your headaches?” Individuals also indicated whether they were currently seeing a primary care doctor or specialist for headache treatment and whether their current office visit was for headache.
Headache Diagnosis and Treatment
Individuals indicated (yes/no) whether a doctor had ever given them a headache diagnosis. If the individual answered yes, they then indicated the diagnosis (or multiple diagnoses). Individuals also answered questions about preventive and acute prescription for headache. The primary author ensured that the medication written down by the patient was placed in the appropriate category (preventive or acute). In addition, individuals indicated whether a doctor had discussed the importance of headache triggers or discussed behavioral options (eg, stress management, relaxation, biofeedback) for managing headaches.
Medical Mistrust Scale
The Medical Mistrust Scale (MMS), an 11-item self-report measure, is a valid41 measure of mistrust in the medical community. Questions are rated on a scale of 1 to 5, with lower scores indicating less mistrust of the medical community. Reliability in the current study was strong (α = 0.88).
Patient–Physician Communication
The PPC, a 5-item self-report measure, was administered in order to assess the patients’ perception of the communication between themselves and their physician.39,40 The items on the PPC are rated on a scale of 1 to 5, with lower scores indicating a more positive view of PPC. The questions came from well-established surveys.39,40 Reliability in the current study was strong (α = 0.94).
Demographics
Individuals answered questions about their age, gender, education, race, current employment, SES, and insurance status. SES was a dichotomous variable, with those making <$20K, annually or (if they chose to not provide their annual income) receiving Medicaid being labeled “low SES”; otherwise they were labeled “not low SES.”
Perceived Triggers
Individuals indicated (yes/no/unsure) whether they believed certain factors triggered individual headache episodes. The factors were chosen based on lists previously produced concerning potential headache triggers.42–45
Data Analyses
Initial analyses were conducted in order to determine whether differences existed between the two ethnicities on demographic factors. A between group analysis of covariance evaluated possible differences on headache characteristics, PPC, and mistrust of the health-care system. SES and recruitment site served as covariates. Given that each of the variable groups contained multiple comparisons, a Bonferroni adjustment for multiple comparisons was used.46 Chi-square analysis was used to evaluate potential differences between the two groups in regards to health-care utilization, prescriptions and other treatment, and perceived migraine triggers. Pearson product moment correlations were calculated between level of mistrust, PPC, whether the individual had ever seen or was currently seeing a doctor for care of their headaches (regardless of whether the care was specifically for migraine), and whether they had received a prescription for acute treatment of their headaches. Analyses were conducted using Statistical Package for the Social Sciences version 13.0.1 for Windows.47
RESULTS
Initial Analysis
Overall, 131 individuals (C =54, AA = 77) were included in the analyses (see Fig. 1). The groups did not differ in regards to age, gender, employment status, or having at least a high school education. There were more African Americans in the low SES category (56%) than Caucasians (43%; χ2 = 4.53, P < .05). Thus, we controlled for SES in the analyses. In addition, we controlled for recruitment site.
Headache and Disability
Table 1 shows the means for each group in regards to years with headache, days per month with headache, headache duration, and pain severity. No significant differences were found between the 2 groups.
Table 1.
Comparison of Caucasians (n = 54) and African Americans (n = 77) on Headache Characteristics, MIDAS, MMS, and PPC
| Caucasian |
African American |
||||||
|---|---|---|---|---|---|---|---|
| Measure | M | SD | M | SD | F | η2 | 99% CI |
| HA years | 15.85 | 10.35 | 11.85 | 10.31 | 3.08 | – | – |
| HA days/month | 9.83 | 5.41 | 7.67 | 5.40 | 3.21 | – | – |
| HA duration | 14.84 | 14.33 | 11.14 | 14.31 | 1.55 | – | – |
| HA severity | 2.51 | 0.62 | 2.59 | 0.62 | 0.57 | – | – |
| MIDAS | 25.40 | 22.88 | 31.21 | 22.82 | 2.00 | – | – |
| MMS | 19.88 | 6.68 | 26.80 | 7.73 | 22.68** | 0.17 | |
| PPC | 12.02 | 5.50 | 16.97 | 7.34 | 13.98** | 0.11 | 1.48 to 8.41 |
HA = headache; MIDAS = migraine disability assessment scale; MMS = medical mistrust scale; PPC = patient–physician communication; MMS score range: 11 to 55, Scale α = 0.88; PPC score range: 6 to 30, Scale α = 0.95.
P < .001.
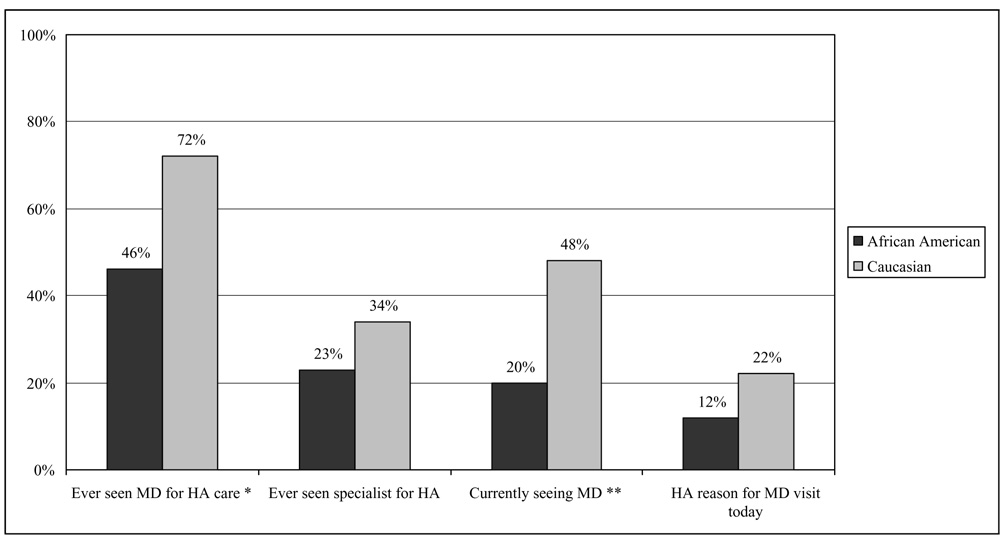
Health-Care Utilization for Migraine
Caucasians (see Fig. 2) were more likely to have ever seen a doctor for headache care (C = 72% vs. AA = 46%; χ2 = 9.25, P < .01) and to be currently seeing a doctor for headache care (C = 48% vs. AA = 20%; χ2 = 11.22, P < .001). Despite being prime candidates for benefiting from physician-guided migraine management, less than half of Caucasians and African Americans were currently seeing a physician for migraine care. In addition, African Americans were significantly less likely to be seeing a physician. No other significant differences were found.
Fig 2.
Percentage of individuals who have utilized the health-care system for headache care (n = 131). Percentages are those responding “Yes” to the question. * P < .01; ** P < .001. HA = headache.
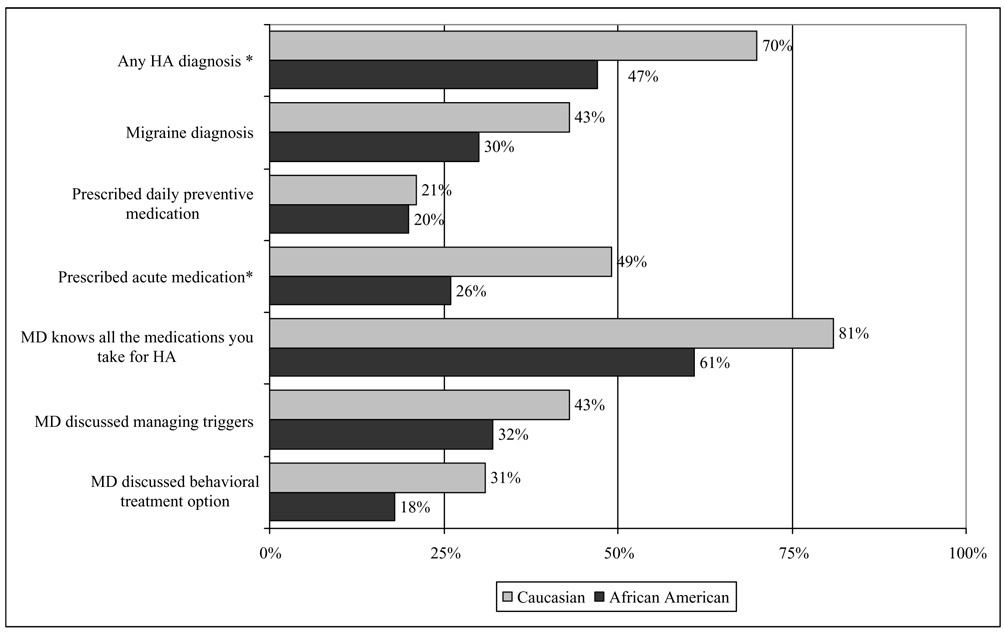
Headache Diagnosis and Treatment
Caucasians (see Fig. 3) were more likely to have received any headache diagnosis (C = 70% vs. AA = 47%; χ2 = 7.78, P < .01). Although there were no significant differences in regards to migraine diagnosis (C = 43% vs. AA = 30%; P = ns), it is interesting to note the low percentages of migraine diagnosis (35%) for both groups.
Fig 3.
Percentage of individuals who have been diagnosed with headache and received treatment for headache care (n = 131). Percentages are those responding “Yes” to the question. * P < .01. HA = headache.
Only those who had seen a physician for headache care were included in analyses of headache treatment. Both groups had woeful percentages of prescriptions for preventive medication (C = 21% vs. AA = 20%, P = ns). For acute medication, although the percentages were low for both groups (C = 49% vs. AA = 26%; χ2 = 9.10, P < .01), African Americans were less likely to have been prescribed acute medication. The percentages were also low for whether a physician had discussed behavioral options (C = 31% vs. AA = 18%; χ2 = 1.04, P = ns) or discussed the importance of managing triggers (C = 43% vs. AA = 32%; χ2 = 3.42, P = ns). The results indicate that both groups were receiving inadequate migraine care, with African Americans being less likely to have been diagnosed as having headaches or to have been prescribed acute medication.
Level of Mistrust of the Health-Care System and PPC
Table 2 shows the results of the MMS and PPC for all participants. Table 3 shows the results only for those who had ever seen a physician for their headaches. African Americans reported more mistrust (C = 19.88 vs. AA = 26.80, F = 22.69, P < .001; η2 = 0.17) and lower quality communication (C = 12.02 vs. AA = 16.97, F = 13.98, P < .001; η2 = 0.11). Table 3 shows that those with lower trust and lower PPC were less likely to have been prescribed acute headache medication (r = −0.22 and −0.23) and those with lower PPC were less likely to have seen a doctor for headache care (r = −0.25). Also, lower levels of trust were correlated with lower PPC (r = 0.43).
Table 2.
Comparison of Caucasians (n = 54) and African Americans (n = 77) on Medical Mistrust and Patient–Physician Communication Items Among Those Who Have Seen a Doctor for Care of Their Headaches
| Caucasian |
African American |
||||||
|---|---|---|---|---|---|---|---|
| Measure | M | SD | M | SD | F | η2 | 99% CI |
| MMS | 19.56 | 7.17 | 28.13 | 7.85 | 23.92** | 0.26 | 4.44 to 15.02 |
| PPC | 11.57 | 5.70 | 15.79 | 6.64 | 8.32* | 0.11 | 0.35 to 8.09 |
MMS = medical mistrust scale, MMS score range: 11 to 55, Scale α = 0.88; PPC = patient–physician communication; PPC score range: 6 to 30, Scale α = 0.95.
P < .01
P < .001.
Table 3.
Correlations Between Headache-Care Utilization, Acute Prescription History, Mistrust, and Communication (n = 131)
| Currently Seeing Doctor for HA Care | Ever Seen Doctor for HA Care | Taking Acute Prescription HA Meds | MMS Total | PPC Total | |
|---|---|---|---|---|---|
| Currently seeing a doctor for HA care | – | ||||
| Ever seen doctor for HA care | 0.592** | – | |||
| Taking acute prescription HA meds | 0.428** | 0.380** | – | ||
| MMS total | −0.248* | −0.065 | −0.227* | – | |
| PPC total | −0.303** | −0.248** | −0.231* | 0.433** | – |
MMS = medical mistrust scale, MMS score range: 11 to 55, Scale α = 0.88; PPC = patient–physician communication, Score range: 6 to 30, Scale α = 0.95.
P < .01
P < .001.
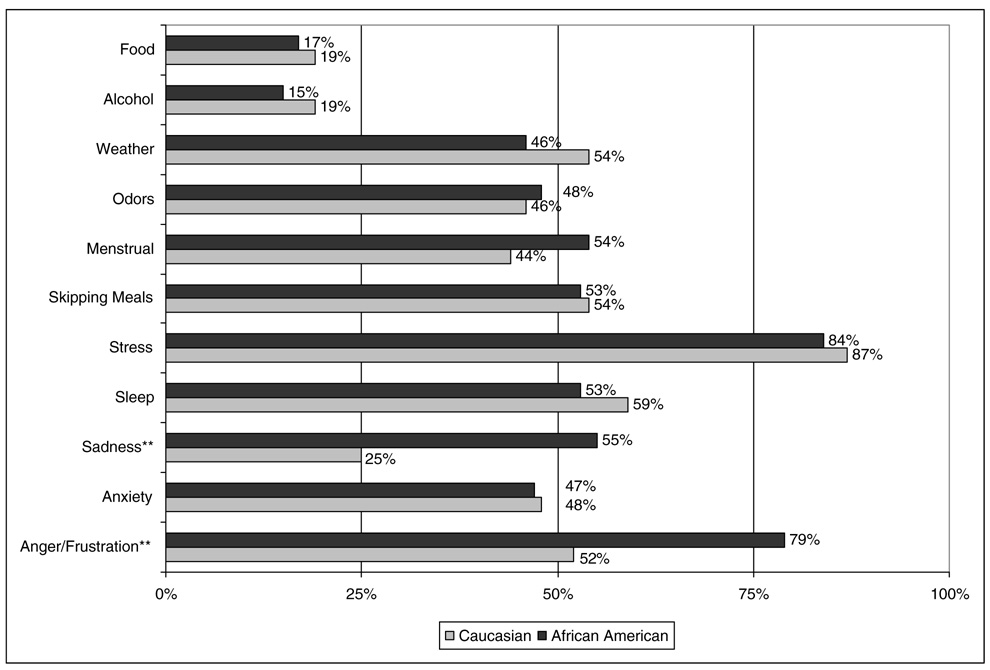
Perceived Triggers
Figure 4 shows the percentages of individuals who answered “yes” versus “no” or “unsure” whether an item was a headache trigger. The only differences were for sadness (“Yes”; C = 25% vs. AA= 55%; χ2 = 11.55, P < .01) and anger/frustration (“Yes”; C = 52% vs. AA = 79%; χ2 = 13.62, P <.001).
Fig 4.
Percentage of individuals who reported the item as a trigger for their headaches (n = 131). Percentages are those responding “Yes” rather than “No” or “Unsure.” ** P < .001.
COMMENTS
The purpose of the current study was to evaluate whether, in a primary care setting, Caucasian and African Americans with moderate to severely disabling migraines differed in regards to: (a) utilizing the health-care system for headache treatment; (b) physician-guided headache diagnosis and treatment; (c) mistrust in the health-care system and PPC; and (d) perceived headache triggers. Results indicated that, even after controlling for SES and recruitment site, African Americans were less likely to utilize the health-care setting for headache management, less likely to have been diagnosed as having any kind of headache, and less likely to have been prescribed acute medication. African Americans also had lower trust in the medical community and lower PPC. Overall, the lower the level of trust and PPC, the less likely the individual is to have ever seen (or currently be seeing) a physician for headache care or to have been prescribed an acute headache medication. Across the 11 triggers measured, differences were found only for sadness and anger/frustration, where African Americans were more likely to cite these as triggers.
The current finding of ethnic differences in utilizing the health-care system (among those with similar access to care) is consistent with previous research.18,21,27 It is important to note that more than 25% of Caucasians and 50% of African Americans had never seen a physician for headache care despite having moderate to severely disabling migraines that could benefit from physician-guided migraine management. Even more concerning is that 50% of Caucasians and 80% of African Americans were not currently seeing a physician for headache care. This lack of utilization, especially among African Americans, is likely not the result of 1 factor. For example, the population surveyed may not know much (be as “health literate”) about efficacious migraine-specific medications. Also, it is likely that the target of direct-to-patient advertising for migraine medications is not low SES (which comprised half of the sample). In addition, it may be that the African American community is less likely to endorse seeing physicians for headache care (however, this has not been researched). More relevant may be the fact that the lower the trust and communication, the less likely individuals were to utilize care. It is vital that physicians (and staff) work to engender trust and engage in quality communication, particularly in situations where the patient perceives the physician as inherently different from them.26,48
Differences in headache diagnosis and acute headache prescription are likely a result of poor communication between patient and physician. Although communication is important in managing any disease, poor communication can be overcome in some disease entities because objective measures exist that identify the presence of disease or determine its severity. However, in pain disorders, there are no objective measures that reliably establish the presence or severity of pain. Given the benefit of proper diagnosis and treatment of migraine (eg, triptans vs. opioids) for reduced pain and disability, communication may be the single most important factor in determining whether physicians diagnose and treat migraine in the best possible manner. Problems with communication may be more acute in situations where the physician and patient come from different cultures26,48 since verbal and nonverbal communications of pain may differ, making proper diagnosis and treatment more difficult. Thus, it is vital that physicians treating migraine be as culturally competent as possible to maximize their likelihood of properly diagnosing and treating migraine.
At least some of the problems with physicians diagnosing and treating migraine accurately come from physician’s not fully appreciating the importance of treating migraine with migraine-specific medications and using preventive medication where appropriate. Only 35% of the current sample had been diagnosed as having migraine, a lower percentage than has been recently reported.49 Also, although ethnic disparities existed for acute headache prescription in general, the percentage of individuals from either ethnic group being prescribed migraine-specific medications was 14%. It is possible that the low percentage of migraine diagnosis and treatment comes from the lower priority physicians place on migraine relative to other chronic conditions that seem more important to address in the brief primary care visit. However, among the group of patients analyzed (having moderate to severely disabling migraines), it is vital that migraine be addressed using evidence-based treatment guidelines.50–54
The groups were similar in regards to perceived triggers. What was interesting was the high percentage indicating stress as a trigger and, among African Americans, the number indicating sadness and anger/frustration as triggers. However, considering the population sampled (50% considered “low SES”) it is possible that negative affectivity (eg, stress/anxiety, sadness, anger/frustration) is persistently elevated among this population. Another possibility is that due to cultural variations in emotional descriptions, African Americans may use a variety of words to describe emotional arousal (eg, stress, sadness, anger/frustration) rather than an all-encompassing word “stress” used by Caucasians.
It is important to keep in mind that the current study used a convenience sample that provided self-report data. Anytime a convenience sample or self-report measures are employed, one cannot make far-reaching conclusions. However, given the lack of data that exist in evaluating potential ethnic disparities in utilization and management of migraine, the current findings provide a starting point to a more systematic evaluation of potential ethnic disparities in headache care. Another limitation of the current study is its cross-sectional nature, which allows for observations of relationships, but not for causal determination. Finally, in order to fully understand the varying influences on ethnic differences in utilization and treatment, future research needs to include measures at the patient, provider, health-care system, cultural, insurer, and environmental levels. However, given the purpose of the current study, to identify potential disparities rather than determine their cause, it appears to have met its goal.
In summary, ethnic disparities appear to exist for headache utilization, diagnosis, and treatment. Also, the trust and communication that exist between patient and physician may influence migraine care regardless of ethnicity. Thus, patients and physicians need to be educated about the benefits of appropriate migraine diagnosis and treatment. Also, physicians need to be aware of cultural variations in patient pain presentation and how cultural differences can influence PPC.
Acknowledgments
The authors would like to thank Mark Mengel, MD, MPH, for his support as chair for this project; Ray Tait, PhD, and John Chibnall, PhD, for their contributions to the ideas behind the design and research questions to be addressed for this project; and Daniel Morris, MS, for his work inputting and managing the database.
Abbreviations
- SES
socioeconomic status
- IOM
Institute of Medicine
- NIH
National Institutes of Health
- NHAHCS
National Hospital Ambulatory Health Care Survey
- MIDAS
migraine disability scale
- ICHD-II
International Classification of Headache Disorders-II
- MMS
Medical Mistrust Scale
- PPC
patient–physician communication
- ANCOVA
analysis of covariance
- SPSS
Statistical Package for the Social Sciences
Footnotes
Conflicts of Interest: None
REFERENCES
- 1.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.The Morehouse Medical Treatment and Effectiveness Center. Racial & Ethnic Differences in Access to Medical Care: A Synthesis of the Literature. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2000. [Google Scholar]
- 3.Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson JA, Tierney WM, Westmoreland GR, et al. Examination of racial differences in management of cardiovascular disease. J Am Coll Cardiol. 1997;30:1707–1713. doi: 10.1016/s0735-1097(97)00365-3. [DOI] [PubMed] [Google Scholar]
- 5.Moore RD, Stanton D, Gopalan R, Chaisson RE. Racial differences in the use of drug therapy for HIV disease in an urban community. N Engl J Med. 1994;330:763–768. doi: 10.1056/NEJM199403173301107. [DOI] [PubMed] [Google Scholar]
- 6.Sirey JA, Meyers BS, Bruce ML, Alexopoulos GS, Perlick DA, Raue P. Predictors of antidepressant prescription and early use among depressed outpatients. Am J Psychiatry. 1999;156:690–696. doi: 10.1176/ajp.156.5.690. [DOI] [PubMed] [Google Scholar]
- 7.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 8.Mayberry R, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57:108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 9.National Institute of Health. [Accessed on October 2005];Healthy People 2010. Available at: http://www.healthypeople.gov/.
- 10.National Institute of Neurologic Disorders and Stroke. [Accessed on May 2005];Five-year strategic plan on minorty health disparities [Internet] Available at: http://www.ninds.nih.gov/about_ninds/plans/disparities.htm.
- 11.Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. Ann Intern Med. 1997;127:813–816. doi: 10.7326/0003-4819-127-9-199711010-00006. [DOI] [PubMed] [Google Scholar]
- 12.Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 13.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35:11–16. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- 14.Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: Combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002;20:83–87. doi: 10.1053/ajem.2002.31578. [DOI] [PubMed] [Google Scholar]
- 15.Ng B, Dimsdale JE, Shragg GP, Deutsch R. Ethnic differences in analgesic consumption for postoperative pain. Psychosom Med. 1996;58:125–129. doi: 10.1097/00006842-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Ng B, Dimsdale J, Rollnik J, Shapiro H. The effect of ethnicity on prescriptions for patient controlled analgesia for post-operative pain. Pain. 1996;66:9–12. doi: 10.1016/0304-3959(96)02955-7. [DOI] [PubMed] [Google Scholar]
- 17.Stewart WF, Lipton RB, Liberman J. Variation in migraine prevalence by race. Neurology. 1996;47:52–59. doi: 10.1212/wnl.47.1.52. [DOI] [PubMed] [Google Scholar]
- 18.Gibbs TS, Fleischer ABJ, Feldman SR, Sam MC, O’Donovan CA. Health care utilization in patients with migraine: Demographics and patterns of care in the ambulatory setting. Headache. 2003;43:330–335. doi: 10.1046/j.1526-4610.2003.03067.x. [DOI] [PubMed] [Google Scholar]
- 19.Geiger H. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. Racial and ethnic disparities in diagnosis and treatment: A review of the evidence and a consideration of causes. [Google Scholar]
- 20.Weinick R, Zuvekas S, Cohen J. Racial and ethnic differences in access to and use of health care services, 1977–1996. Med Care Res Rev. 2000;57(suppl 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- 21.Escarce JJPF. Black–White differences in the use of medical care by the elderly. In: Martin LG, Soldo BJ, editors. Racial and Ethnic Differences in the Health of Older Americans. Washington, DC: National Academy Press; 1997. pp. 183–209. [PubMed] [Google Scholar]
- 22.Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998;36:180–189. doi: 10.1097/00005650-199802000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Burke-Ramirez P, Asgharnejad M, Webster C, Davis R, Laurenza A. Efficacy and tolerability of subcutaneous sumatriptan for acute migraine: A comparison between ethnic groups. Headache. 2001;41:878–882. [PubMed] [Google Scholar]
- 24.Blendon R, Scheck A, Donelan K, Hill C, Beatrice D, Altman D. How White and African Americans view their health and social problems. JAMA. 1995;273:341–346. [PubMed] [Google Scholar]
- 25.Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M. Race, ethnicity, and the health care system: Public perceptions and experiences. Med Care Res Rev. 2000;57:218–235. doi: 10.1177/1077558700057001S10. [DOI] [PubMed] [Google Scholar]
- 26.Cooper L, Roter D. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. Patient–provider communication: The effect of race and ethnicity on process and outcomes of healthcare. [Google Scholar]
- 27.Fiscella K, Franks P, Gold M, Clancy C. Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2002;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 28.Bonham VL. Race, ethnicity, and pain treatment: Striving to understand the causes and solutions to the disparities in pain treatment. J Law Med Ethics. 2001;29:52–68. doi: 10.1111/j.1748-720x.2001.tb00039.x. [DOI] [PubMed] [Google Scholar]
- 29.Green CR, Anderson K, Baker T, Campbell LC, Decker S, Fillingim RB, et al. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 30.Headache Classification Committee of the International Headache Society. The international classification of headache disorders. Cephalagia. 2004;24:1–151. [Google Scholar]
- 31.Stewart WF, Lipton RB, Simon DJ, Liberman J, von Korff M. Validity of an illness severity measure for headache in a population sample of migraine sufferers. Pain. 1999;79:291–301. doi: 10.1016/s0304-3959(98)00181-x. [DOI] [PubMed] [Google Scholar]
- 32.Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN. Validity of the migraine disability assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain. 2000;88:41–52. doi: 10.1016/S0304-3959(00)00305-5. [DOI] [PubMed] [Google Scholar]
- 33.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56:20S–28S. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 34.Lipton R, Goadsby PJ, Sawyer J, Blakeborough P, Stewart WF. Migraine: Diagnosis and assessment of disability. Rev Contemp Pharmacother. 2000;11:63–73. [Google Scholar]
- 35.Edmeads J, Lainez JM, Brandes JL, Freitag F. Potential of the migraine disability assessment (MIDAS) questionnaire as a public health initiative and in clinical practice. Neurology. 2001;56:29S–34S. doi: 10.1212/wnl.56.suppl_1.s29. [DOI] [PubMed] [Google Scholar]
- 36.Macgregor EA, Brandes J, Eikerman A. Migraine prevalence and treatment patterns: The global migraine and zolmitriptan evaluation survey. Headache. 2003;43:19–26. doi: 10.1046/j.1526-4610.2003.03004.x. [DOI] [PubMed] [Google Scholar]
- 37.Nicholson R, Nash J, Andrasik F. A self-administered behavioral intervention for migraine using tailored messages. Headache. 2005;45:1124–1139. doi: 10.1111/j.1526-4610.2005.00236.x. [DOI] [PubMed] [Google Scholar]
- 38.International Headache Society Clinical Trials Subcommittee. Guidelines for controlled trials of drugs in migraine: Second edition. Cephalalgia. 2000;20:765–786. doi: 10.1046/j.1468-2982.2000.00117.x. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control National Center for Health Statistics. National Health Information Survey. [Accessed on November 2003]; Available at: http://www.cdc.gov/nchs/nhis.htm.
- 40.United States Department of Health and Human Services Agency for Healthcare Research and Quality. Medical Expenditures Panel Survey. [Accessed on November 2003]; Available at: http://www.meps.ahrq.gov/.
- 41.Thompson H, Valdimarsodottir H, Winkel G, Jandorf L, Redd W. The group-based medical mistrust scale: Psychometric properties and association with breast cancer screening. Prev Med. 2004;38:209–218. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 42.Martin VT. Toward a rational understanding of migraine trigger factors. Med Clin North America. 2001;85:911–941. doi: 10.1016/s0025-7125(05)70351-5. [DOI] [PubMed] [Google Scholar]
- 43.Chabriat H, Danchot J, Michel P. Precipitating factors of headache: A prospective study in a national control-matched survey in migraineurs and non-migraineurs. Headache. 1999;35:335–338. doi: 10.1046/j.1526-4610.1999.3905335.x. [DOI] [PubMed] [Google Scholar]
- 44.Scharff L, Turk DC, Marcus DA. Triggers of headache episodes and coping responses of headache diagnostic groups. Headache. 1995;35:397–403. doi: 10.1111/j.1526-4610.1995.hed3507397.x. [DOI] [PubMed] [Google Scholar]
- 45.Robbins L. Precipitating factors in migraine: A retrospective review of 494 patients. Headache. 1994;34:214–216. doi: 10.1111/j.1526-4610.1994.hed3404214.x. [DOI] [PubMed] [Google Scholar]
- 46.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Northridge, CA: Harper Collins College Publishers; 2001. [Google Scholar]
- 47.Statistical Packages for the Social Sciences (SPSS) [computer program]. Version 13.0.1. Chicago: SPSS Inc.; 2004. [Google Scholar]
- 48.Cooper L, Roter D. Patient–provider communication: The effect of race and ethnicity on process and outcomes of healthcare. In: Smedley B, editor. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. pp. 594–625. [Google Scholar]
- 49.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: Results from the American Migraine Study II. Headache. 2001;41:638–645. doi: 10.1046/j.1526-4610.2001.041007638.x. [DOI] [PubMed] [Google Scholar]
- 50.Ramadan NM, Silberstein SD, Freitag FG, Gilbert TT, Frishberg BM. Evidence-based guidelines for migraine headache in the primary care setting: Pharmacological management for prevention of migraine. [Retrieved October 15, 2002];Am Acad Neurol (online) 2000 Apr; [Google Scholar]
- 51.Campbell K, Penzien D, Wall J. Evidence-based guidelines for migraine headache in the primary care setting: Behavioral and physical intervention for prevention of migraine. [Retrieved October 15, 2002];Am Acad Neurol (online) 2000 Apr; [Google Scholar]
- 52.Matchar DB, Young WB, Rosenberg JH, Pietrzak MP, Silberstein SD, Lipton RB, et al. Evidence-based guidelines for migraine headache in the primary care setting: Pharmacological management of acute attacks. [Retrieved October 15, 2002];Am Acad Neurol (online) 2000 Apr; [Google Scholar]
- 53.Silberstein SD. Practice parameter: Evidence-based guidelines for migraine headache (an evidence-based review): Report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2000;55:538–547. doi: 10.1212/wnl.55.6.754. [DOI] [PubMed] [Google Scholar]
- 54.Silberstein SD, Freitag FG. Preventive treatment of migraine. Neurology. 2003:60. [Google Scholar]