Abstract
Aim
To assess the implementation of the Alcohol Screening and Brief Intervention (SBI) strategy as part of a routine practice of nurses in 18 primary health care services in Vhembe district, South Africa.
Method
We performed a cross-sectional study to assess the success of implementation of the SBI in 18 primary health care services. We examined all anonymously completed questionnaires (n = 2670) collected from all practices after a 6-month implementation period. Clinic managers were interviewed on SBI implementation after 4 months of implementation. The success of implementation was assessed on the basis of perceived benefits, beliefs, values, past history, current needs, competing priorities, complexity of innovation, trialability and observability, and feedback on SBI performance.
Results
In the 6-month period, nurses screened 2670 patients and found that 648 (23.4%) patients (39.1% men and 13.8% women) were hazardous or harmful drinkers. Nine clinics had good and 9 poor SBI implementation. Factors discriminating the clinics with good or poor SBI implementation included the percentage of nurses trained in SBI, support visits, clinical workload, competing priorities, team work, innovation adoption curve, perceived complexity of innovation, compatibility beliefs, trialability, and observability of SBI.
Conclusion
To improve SBI implementation as a routine practice, more attention should be paid to training modalities, clinic organization, and changes in the attitudes of nurses.
Alcohol consumption in amounts that significantly increase the chances of health problems is common among patients presenting to primary care and imposes a significant economic burden on the health care system (1). Primary health care is the first point of contact with individuals, families, and communities in most countries’ health systems (2). Primary care is, therefore, a particularly valuable point of delivery of community-based interventions for excessive alcohol consumption due to both its universality and the large proportion of the population who access it each year (3). Moreover, problem drinkers present to primary health care twice as often as other patients and constitute approximately 20% of patients on practice lists (4).
Increasing emphasis has been placed on the detection and treatment of hazardous and harmful drinking disorders, particularly among patients in primary care settings (5). Hazardous drinking is defined as a quantity or pattern of alcohol consumption that places patients at risk for adverse health events, while harmful drinking is defined as alcohol consumption that results in adverse events (eg, physical or psychological harm) (5). The White Paper for Transformation of the Health System in South Africa (6) and the National Drug Master Plan (7) in South Africa have prioritized prevention and management of alcohol abuse and the integration of substance abuse management in primary health care. The South African Department of Health (3) has included in the service description of clinics the prevention and management of substance abuse. Standards for primary health care include health-learning materials on alcohol in local languages and competence of health staff in identifying alcohol abuse, as well as provide basic counseling for behavior changes and referral to non-governmental organizations specializing in substance abuse.
Screening procedures have been developed to identify at-risk drinkers (8), and brief interventions can achieve significant reductions in drinking and related risks (9). Screening for alcohol consumption among patients in primary care carries many potential benefits. It provides an opportunity to educate patients about low-risk consumption levels and the risks of excessive alcohol use. Information about the amount and frequency of alcohol consumptions may contribute to making the patient’s diagnosis and may alert clinicians to the need to advise patients whose alcohol consumption might adversely affect their use of medications and other aspects of their treatment. Screening can also identify persons likely to be alcohol dependent, and referral for diagnostic evaluation may encourage patients to seek treatments that have been shown to be effective (8). Brief interventions are characterized by their low intensity and short duration. They typically consist of one to three sessions of counseling and education. They are intended to provide early intervention, before or soon after the onset of alcohol-related problems. Most programs are designed to motivate high-risk drinkers to moderate their alcohol consumption, rather than to promote total abstinence with specialized treatment techniques. Brief interventions also provide a valuable framework to facilitate referral of severe cases of alcohol dependence to specialized treatment (10).
Introducing new screening and prevention activities into primary care practices presents significant logistical, attitudinal, and behavioral challenges. Many nurses feel inadequately trained when faced with patients who have alcohol-related problems (11,12). Barriers to adequate coverage of alcohol-related problems in both nursing schools and continuing professional education include traditional attitudes about the moral culpability of chronic alcoholics, confusion as to whether problem drinking is a medical or psychological concern, lack of faculty role models, lack of training materials, and role ambiguity regarding who is responsible for screening and intervention (13). Another factor could be the relative lack of awareness that Screening and Brief Intervention (SBI) leads to significant reductions in drinking and risk.
The World Health Organization SBI program was developed to train medical providers to implement SBI in primary care settings. Some progress has been made in the development and dissemination of SBI in industrial countries (2,8) and the aim of this study was to assess the implementation of the SBI strategy as a routine practice of primary care nurses in a developing country, South Africa. Our study is a part of the World Health Organization Collaborative Study on Brief Interventions for Hazardous and Harmful Alcohol Use in developing countries (14).
Methods
Setting
The assessment of the implementation of the alcohol Screening and Brief Intervention (SBI) was conducted in 18 clinics (16 primary care clinics and 2 community health centers) in two Local Services Areas (Sibasa and William Eadie) of the Thulamela health sub-district, Vhembe District, in the northeastern, mostly rural area of South Africa. The 18 clinics selected for the implementation serve 125 000-130 000 patients per month; the primary health care utilization rate in 2006 was high (mean, 4.6 primary care clinic visits in a year; range, 3.8-6.2) (15).
Nurse training
Primary health care providers including professional nurses, enrolled nurses, and assistant nurses from 18 primary health care clinics from Thulamela sub-district (Vhembe district) had been trained for two days on SBI. The trainings included nurses with different nursing ranks (professional, enrolled or assistant nurses), practice goals, levels of education, and length of experience. However, due to their similar experience in the nursing field, they had a similar goal in preventing alcohol abuse. Training of nurses in SBI for alcohol problems in primary health care is described in more detail elsewhere (16). The SBI implementation program was officially endorsed by the national department of health and the province and district health authorities. Nurses were provided with a certificate of attendance when all the trainings had been completed. When the trainings were completed, each clinic received at least two support visits by a trainer on SBI procedures during the first three months of implementation.
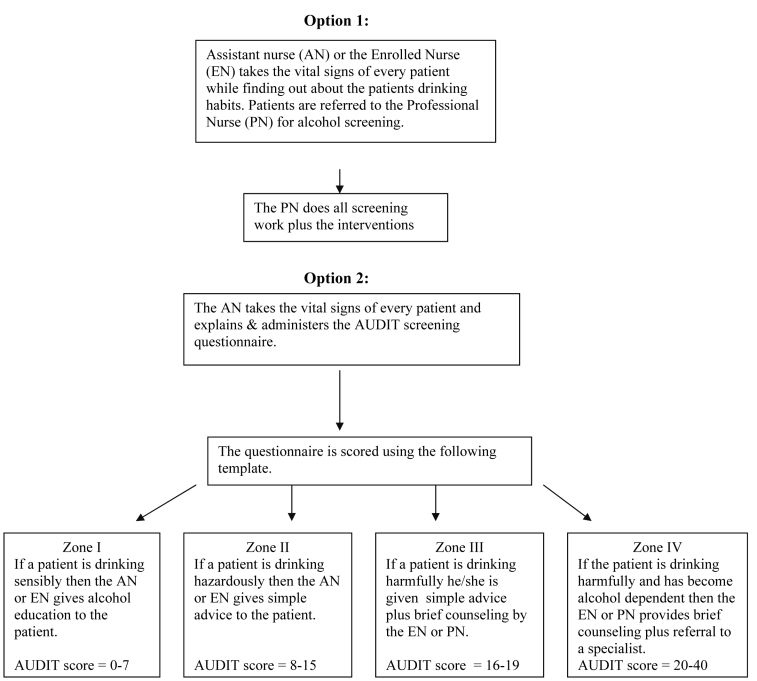
Two main intervention modalities were practiced in the clinics as follows: 1) a modality where an assistant nurse or enrolled nurse inquired about drinking habits while taking vital signs and referred for SBI to the professional nurse, and 2) a modality where the enrolled or assistant nurse administered the Alcohol Use Disorder Identification Test (AUDIT) screening questionnaire while taking vital signs from the patient. Depending on the drinking risk level or zone, either the enrolled nurse or assistant nurse provided some form of intervention. In case of Zone I (non- or low-risk drinkers) they provided alcohol education, whereas to Zone II drinkers they gave simple advice. In case of Zone III and Zone IV drinkers, the patient was mostly referred to the professional nurse for a brief counseling and referral, and in some cases the enrolled nurse also provided brief counseling and referral (Figure 1).
Figure 1.
Screening and brief intervention implementation modalities in primary care clinics in Vhembe District, South Africa.
Nurses had agreed to implement a screening and brief alcohol intervention program in their clinics. All nurses were requested to screen all consecutive adults (aged over 16 years) presenting to their clinic and follow an identical structured protocol for giving SBI.
Questionnaire
Anonymously completed questionnaires were collected from all practices after a 6-month implementation period. All clinic managers were interviewed by a Human Sciences Research Council researcher and trainer 4 months after the implementation of SBI with a semi-structured questionnaire on SBI implementation attitudes. Informed consent was obtained from the clinic managers and the study was approved by the University of Limpopo ethics committee.
The screening questionnaire used was the AUDIT, a 10-item questionnaire designed specifically for use in primary care. The total score of the questionnaire was 40 and the cut-off point for risk drinking was set at 8 points, resulting in a sensitivity of 92% and a specificity of 94% (17). Risk drinking consists of both hazardous consumption, which incurs increased risk of psychological or physical harm, and harmful consumption, which is defined by the presence of physical or psychological symptoms (18,19). Because AUDIT is reported to be less sensitive at identifying risk drinking in women (20), the cut-off points of binge drinking for women were reduced by one unit as compared with men.
In addition to the 10 alcohol-related items, the screening questionnaire contained two questions regarding patients’ age and sex.
Ten SBI implementation attitude questions (web-extra material), derived from a literature review, were asked, including items on perceived benefits, beliefs, values, past history, current needs, competing priorities, complexity of innovation, trialability and observability, and feedback on SBI performance (defined as 120 and more AUDIT questionnaires retrieved) (21,22).
Trialability and observability
The process of the role play was used during the trainings to give nurses a chance to try the implementation before actually carrying it out on patients. Some clinics took the first opportunity right after the training workshops to practice alcohol screening. They went through a process of trial and error (as they reported) and this is what contributed to their success in implementing the project. During the trainings nurses engaged in role plays where they practiced alcohol screening and brief intervention on one another – one taking the role of a patient and the other of a nurse. After each role-play session, the session was evaluated by everyone and this allowed for mistakes to be corrected. In the clinics, the trainers functioned as observers in some alcohol screening and brief intervention sessions with nurses. The professional nurses often needed help from the trainer with providing brief advice and intervention. Nurses who attended the first trainings gave other nurses who still had to attend the training a chance to watch them as they implemented alcohol screening.
Statistical analysis
Data were presented as frequencies and percentages. Differences in proportions between the groups were tested with χ2 test. Fisher's exact test was used for the analysis of small-sample categorical data. Statistical analysis was performed with Statistical Package for the Social Sciences, version 14.0 (SPSS Inc., Chicago, IL, USA). The significance level was set at P<0.05.
Results
Patient screening data were provided from 18 clinics in two local service areas of Thulamela sub-district. Clinics had 101 professional nurses (83% had been trained in SBI), 47 enrolled nurses (85% had been trained in SBI), and 48 assistant nurses (73% had been trained in SBI).
Nurses implemented SBI in 2670 patients (none refused) during a 6-month implementation period in the 18 clinics. Of the nurses who implemented SBI, 83.4% had received formal SBI training. Different SBI components, screening, alcohol education, simple advice, brief counseling, and brief counseling and referral were done by professional nurses (75%) and enrolled nurses (25%). A total AUDIT score was available on all screening questionnaires. Overall, 648 (23.4%) patients were hazardous or harmful drinkers: 13.4% were Zone II drinkers, 4.7% were Zone III drinkers, and 6.2% were Zone IV (or probable alcohol dependent) drinkers. Significantly more men (39.1%) than women (13.8%) were drinking at hazardous or harmful levels. The highest levels of hazardous or harmful drinking were reported in the age groups 41 to 60 years (33.6%) and 25 to 40 years (26.5%) (Table 1).
Table 1.
Risk drinking level by sex and age of 2670 patients screened for alcohol in primary care in Vhembe District, South Africa
| AUDIT score* | No. (%) of patients in: |
χ2 | P | |||
|---|---|---|---|---|---|---|
| Zone I (0-7) | Zone I (I8-15) | Zone III (16-19) | Zone IV (20-40) | |||
| Total patients | 2022 (75.7) | 357 (13.4) | 125 (4.7) | 166 (6.2) | ||
| Sex: | 212.40 | <0.001 | ||||
| male | 611 (60.9) | 210 (20.9) | 84 (8.4) | 99 (9.9) | ||
| female | 1282 (86.2) | 115 (7.7) | 31 (2.1) | 59 (4.0) | ||
| Age: | 77.86 | <0.001 | ||||
| 16-24 | 613 (87.0) | 56 (7.9) | 19 (2.7) | 17 (2.4) | ||
| 25-40 | 800 (73.5) | 157 (14.4) | 52 (4.8) | 79 (7.3) | ||
| 41-60 | 374 (66.4) | 99 (17.6) | 37 (6.6) | 53 (9.4) | ||
| >60 | 89 (75.4) | 14 (11.9) | 7 (5.9) | 8 (6.8) | ||
*AUDIT – Alcohol Use Disorder Identification Test.
SBI implementation evaluation
Enabling factors and barriers in SBI implementation were divided into two broad areas – structure and organization of clinics and perceptions of innovation (Table 2).
Table 2.
Evaluation summary ratings of screening and brief intervention (SBI) implementation in primary care in Vhembe District, South Africa
| SBI implementation factors | No. of clinics which answered “yes” or (strongly) agree |
P* | |
|---|---|---|---|
| clinics with good implementation (n = 9)† | clinics with poor implementation (n = 9) | ||
| Structure and organization of clinics: | |||
| all nurses in the clinic trained in SBI | 8 | 3 | 0.050 |
| feedback provided | 4 | 2 | 0.637 |
| nurse clinical workload <35 patients a day‡ | 7 | 2 | 0.057 |
| competing priorities (eg, voluntary HIV counseling and testing, tuberculosis, antenatal care, Papanicolaou smear examinations) | 1 | 5 | 0.131 |
| teamwork | 7 | 3 | 0.153 |
| tension in the clinic | 2 | 4 | 0.620 |
| Perceptions of innovation: | |||
| early adopters (first 2 mo) | 6 | 0 | 0.009 |
| perceived benefit from SBI | 9 | 8 | >0.95 |
| compatibility with beliefs, values, past history and current needs | 6 | 4 | 0.637 |
| low perceived complexity of innovation | 8 | 4 | 0.131 |
| trialability and observability | 4 | 3 | >0.95 |
*Fisher exact test.
†The cut-off for clinics with good SBI implementation was 120 and more Alcohol Use Disorder Identification Test questionnaires retrieved.
‡According to District Health Information System Database (15).
Structure and organization of clinics. Significantly more clinics with good SBI implementation had all nurses trained in SBI (P = 0.050, Table 2). Clinics with good SBI implementation also more often received feedback from support visits, had lower nurse clinical workload, less prioritized other health goals, more often exhibited team work, and had less tension in the clinic than clinics with poor implementation, but these differenceswere not significant (Table 2).
Perceptions of innovation. Clinics with good implementation were significantly more often early adopters (P = 0.009; Table 2). Clinics with good implementation also more often perceived the SBI innovation as less complex or difficult, more compatible with their beliefs, values, past history, and current needs, and had more chance to try and observe SBI, but these differences were not significant (Table 2). Both clinics with good and poor implementation acknowledged the perceived benefits of SBI (Table 2).
Perceived benefit and risks of change. One-hundred and ten of the professional and enrolled nurses (75%) reported that they did not know how to handle and help patients with alcohol-related problems. Some believed that this program could be a solution in helping them to handle and help alcohol-abusing patients. Sixteen out of 18 clinic managers believed in the following benefits of SBI:
• “getting more experience on alcohol screening”
• “knowing which questions to ask a person who is abusing alcohol”
• “be able to explain the dangers of drinking alcohol”
• “be able to identify at risk drinkers and those who are already having a problem and then intervene”
• “be able to prevent serious illness caused by alcohol”
• “know the target group, who abuses alcohol the most, and following-up and referring when necessary”
• “be able to help in reducing the conditions caused by alcohol”
• “to identify alcohol problems in our community”
• “to know if a person is taking alcohol so that the person may take it with moderation”
Compatibility with the values, beliefs, past history, and current needs of individuals. Some of the nurses who attended the trainings believed that drinking alcohol was against their Christian beliefs and that alcohol had become a problem in today’s life. They felt that there was a need to have a program aimed at preventing alcohol abuse and that SBI could be that program. There were those who did not attend the training because they felt that they would not serve as good examples as they were alcohol drinkers themselves.
Some enrolled nurses and assistant nurses felt that the training would be a waste of time for them, since they reported that they did not advise patients but only took vital signs. They did not foresee a situation where they were going to apply the knowledge they acquired during the training. For some nurses, it was their first in-service training since they started working and they were happy about it. However, there were others who felt that it was not necessary for them to attend, since they were approaching retirement age. More clinics (but not significantly) with good than poor implementation disagreed that SBI went against their beliefs, values, past history, and current needs.
Some of the reasons in favor of screening were as follows:
• “people should be screened to prevent alcohol-related conditions”
• “some treatments contradict with alcohol”
• “too much alcohol intake is not good for human health”
• “it is of use to people in order for them to use alcohol correctly”
• “some religions are against alcohol”
• “as a Christian I believe that I must not drink”
• “as a Christian I should also assist people to quit drinking alcohol“
• “I stand for an alcohol-free community”
• “drinking should not be a habit”
The remaining clinic managers agreed that SBI went against their beliefs, values, past history, and current needs, and stated the following reasons:
• “some people use alcohol for traditional purposes, some say it gives them power, some say their grannies have been drinking since long ago“
• “asking the elderly people about their drinking status is a sign of disrespect”
Complexity of innovation. Clinics with poor implementation perceived the SBI innovation as more complex or difficult to implement than clinics with good implementation.
Trialability and observability
Clinics with good implementation had higher scores on trialability and observability than clinics with poor implementation.
Discussion
Factors influencing the implementation of SBI in routine primary care practice in this study included the percentage of nurses trained in SBI, support visits, clinical workload, competing priorities, team work, early adoption, compatibility beliefs, perceived complexity of innovation, trialability, and observability of SBI, which concurs with findings from other studies (22,23). Other factors influencing the adoption of innovations seem not to have played a role in this study, such as perceptions of innovation (perceived benefit and risks of change), contextual factors (communication, incentives, leadership, management), nurturing environment for innovators (praise, resources, security), group education sessions, education by respected colleagues (ie, opinion leaders), that the continuing education in SBI is based on demonstrated need, that the needs are translated into specific measurable objectives, that the length of the education offered is appropriate to the objectives to be achieved, that the participants are a homogeneous group with similar practice goals and learning readiness, that learning activities and teaching methods are varied, and that objectives are developed jointly with sponsors and evaluated in practice afterwards (21,22).
In this study, the nurses found a high prevalence of hazardous or harmful drinkers. Peltzer (24) found an even higher prevalence of hazardous or harmful drinking among men but lower among women in rural primary care clinics in South Africa. Lock and Kaner (25) also found a similar prevalence of risky drinkers when brief alcohol interventions were implemented by nurses in primary care in the UK. When compared with the UK study, South African primary care patients develop higher levels of risk drinking at older age. Saunders et al (26) found a prevalence of hazardous alcohol use of 18% (after non-drinkers and alcoholics had been excluded) among patients attending primary health care facilities in Australia, Bulgaria, Kenya, Mexico, Norway, and the USA. In Nigeria hazardous drinking was present in over a quarter of primary care outpatients (27) and in Harare, Zimbabwe the prevalence was 25% (17). The prevalence of alcohol dependency or harmful drinking in Nigeria was low (28).
In this study, clinics with poor implementation perceived the SBI innovation as more complex or difficult to implement than clinics with good implementation. However, according to Babor et al (8), the AUDIT questionnaire is simple, short, and straight to the point. The total score and the categories into which the scores fall are easy to understand and implement. Each category of intervention stipulates clearly what has to be done in helping the patient.
In addition, early adopter activity should be made observable and one should invest more in early adopters. High levels of perceived benefits from SBI were not translated into better implementation of SBI. Finnish health care providers found increasing motivational skills also to be a challenge (29). Other studies also indicate difficulties in the effective implementation of SBI routine practice in primary care. Ronzani et al (5) found that health care professionals in Brazil limit the approach to alcohol-dependent patients and demonstrate a lack of motivation for preventive work, and health service managers experience difficulties in the organization and administration of such instruments, despite affirming their interest in the project. Segura et al (30) found that clinical histories contained less information on screening and counseling related to alcohol consumption than what patients said they received and professionals said they performed. In addition, most of the at-risk drinkers who were seen in primary care were not detected. Aalto et al (29) found that attitudes and skills did not develop positively in the implementation of brief alcohol intervention in primary health care in Finland. Johansson et al (31) studied under what circumstances Swedish nurses were willing to engage in brief alcohol interventions and found that they mainly wanted to engage in screening patients with alcohol-related symptoms or diagnoses and other risk groups. Reasons for refraining from alcohol screening and intervention included lack of self-efficacy, time consumption, and fear of harming their relationship with the patient. Barry et al (23) studied the implementation and barriers of use of alcohol screening and brief interventions in primary care settings and in the US Veterans health administration and found that lack of time was the most important perceived barrier to implementing screening and brief alcohol interventions for at-risk and problem drinkers.
Our findings are subjected to some limitations. First, the population sample that participated in the survey was limited to patients screened when nurses were able to perform the screening, which did not happen to the same extent in all the implementation clinics. As such, our findings may not be representative of all patients visiting the clinics in the study area. We, however, believe that the findings are likely to be representative of the patient population due to 100% overall response rate and a large sample.
Second, the data were based on self-reports on alcohol consumption of patients, who might have underreported or may not have been truthful about their drinking. Even though no biomakers were used in establishing alcohol consumption levels, Babor et al (10) state that assessments of alcohol consumption with the AUDIT seem fairly accurate compared with biomarkers.
In order to improve on SBI implementation as routine practice, more attention should be paid to the following factors: 1) training modalities (greater number of nurses trained in SBI in each clinic, the provision of support visits, trialability and obervability of SBI); 2) clinic organization (low clinical workload, fewer competing priorities, and better team work); and 3) attitudinal changes (early adoption, better compatibility of intervention with beliefs, and less perceived complexity of innovation).
Acknowledgments
The National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health, USA, provided support for the project.
References
- 1.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Med Care. 2000;38:7–18. doi: 10.1097/00005650-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kaner EF, Wutzke S, Saunders JB, Powell A, Morawski J, Bouix JC, et al. Impact of alcohol education and training on general practitioners' diagnostic and management skills: findings from a World Health Organization collaborative study. J Stud Alcohol. 2001;62:621–7. doi: 10.15288/jsa.2001.62.621. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. The primary health care package for South Africa: a set of norms and standards. Pretoria: Department of Health; 2001. Available from: www.doh.gov.za/docs/policy/norms/full-norms.html Accessed: March 17, 2007.
- 4.Anderson P. Management of alcohol problems: the role of the general practitioner. Alcohol Alcohol. 1993;28:263–72. [PubMed] [Google Scholar]
- 5.Ronzani TM, Ribeiro MS, Amaral MB, Formigoni ML. Hazardous alcohol use: screening and brief intervention as routine practice in primary care. Cad Saude Publica. 2005;21:852–61. doi: 10.1590/s0102-311x2005000300019. [in Portuguese] [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. The White Paper for Transformation of the Health System in South Africa. Pretoria: Department of Health; 1997. Available from: http://www.info.gov.za/whitepapers/1997/health.htm Accessed: April 1, 2008.
- 7.Department of Welfare. National drug master plan. Pretoria: Department of Welfare; 1999. Available from: http://www.info.gov.za/otherdocs/1999/drugplan.pdf Accessed: March 17, 2008.
- 8.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: the Alcohol Use Disorders Identification Test. Guidelines for use in primary care. Geneva (Switzerland): World Health Organization; 2001. [Google Scholar]
- 9.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–92. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 10.Babor T, Caetano R, Casswell S, Edwards G, Ggiesbrecht N, Graham K, et al. Alcohol: no ordinary commodity – research and public policy. Oxford (UK): Oxford University Press; 2003. [Google Scholar]
- 11.Church OM, Babor TF. Barriers and breakthroughs: substance abuse curricula in nursing education. J Nurs Educ. 1995;34:278–81. doi: 10.3928/0148-4834-19950901-09. [DOI] [PubMed] [Google Scholar]
- 12.Rendall-Mkosi KM, Siegfried N, Allen S. Sensible Drinking Project: evaluation of health workers training. African Journal of Drug and Alcohol Studies. 2003;2:31–45. [Google Scholar]
- 13.Bendtsen P, Akerlind I. Changes in attitudes and practices in primary health care with regard to early intervention for problem drinkers. Alcohol Alcohol. 1999;34:795–800. doi: 10.1093/alcalc/34.5.795. [DOI] [PubMed] [Google Scholar]
- 14.Monteiro MG, Gomel M. World Health Organization project on brief interventions for alcohol-related problems in primary health care settings. J Subst Abuse. 1998;3:5–9. [Google Scholar]
- 15.District Health Information System (DHIS) Database. Pretoria: National Department of Health. 2006. [Google Scholar]
- 16.Peltzer K, Seoka P, Babor T, Obot I. Training primary care nurses to conduct alcohol screening and brief interventions in South Africa. Curationis. 2006;29:16–21. doi: 10.4102/curationis.v29i2.1067. [DOI] [PubMed] [Google Scholar]
- 17.Chinyadza E, Moyo IM, Katsumbe TM, Chisvo D, Mahari M, Cock DE, et al. Alcohol problems among patients attending five primary health care clinics in Harare city. Cent Afr J Med. 1993;39:26–32. [PubMed] [Google Scholar]
- 18.Edwards G, Arif A, Hadgson R. Nomenclature and classification of drug- and alcohol-related problems: a WHO Memorandum. Bull World Health Organ. 1981;59:225–42. [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. International classification of diseases: 10th revision. Geneva (Switzerland): World Health Organization; 1992. [Google Scholar]
- 20.Freeborn DK, Polen MR, Hollis JF, Senft RA. Screening and brief intervention for hazardous drinking in an HMO: effects on medical care utilization. J Behav Health Serv Res. 2000;27:446–53. doi: 10.1007/BF02287826. [DOI] [PubMed] [Google Scholar]
- 21.Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 22.Fleming MF. Strategies to increase alcohol screening in health care settings. Alcohol Health Res World. 1997;21:340–7. [PMC free article] [PubMed] [Google Scholar]
- 23.Barry KL, Blow FC, Willenbring ML, McCormick R, Brockmann LM, Visnic S. Use of alcohol screening and brief interventions in primary care settings: implementation and barriers. Subst Abus. 2004;25:27–36. doi: 10.1300/J465v25n01_05. [DOI] [PubMed] [Google Scholar]
- 24.Peltzer K. Prevalence of alcohol use by rural primary care outpatients in South Africa. Psychol Rep. 2006;99:176–8. doi: 10.2466/PR0.99.5.176-178. [DOI] [PubMed] [Google Scholar]
- 25.Lock CA, Kaner EF. Implementation of brief alcohol interventions by nurses in primary care: do non-clinical factors influence practice? Fam Pract. 2004;21:270–5. doi: 10.1093/fampra/cmh310. [DOI] [PubMed] [Google Scholar]
- 26.Saunders JB, Aasland OG, Amundsen A, Grant M. Alcohol consumption and related problems among primary health care patients: WHO collaborative project on early detection of persons with harmful alcohol consumption – I. Addiction. 1993;88:349–62. doi: 10.1111/j.1360-0443.1993.tb00822.x. [DOI] [PubMed] [Google Scholar]
- 27.Abiodun OA. Alcohol-related problems in primary care patients in Nigeria. Acta Psychiatr Scand. 1996;93:235–9. doi: 10.1111/j.1600-0447.1996.tb10640.x. [DOI] [PubMed] [Google Scholar]
- 28.Gureje O, Obikoya B, Ikuesan BA. Alcohol abuse and dependence in an urban primary care clinic in Nigeria. Drug Alcohol Depend. 1992;30:163–7. doi: 10.1016/0376-8716(92)90021-4. [DOI] [PubMed] [Google Scholar]
- 29.Aalto M, Pekuri P, Seppa K. Implementation of brief alcohol intervention in primary health care: do nurses' and general practitioners' attitudes, skills and knowledge change? Drug Alcohol Rev. 2005;24:555–8. doi: 10.1080/09595230500292904. [DOI] [PubMed] [Google Scholar]
- 30.Segura Garcia L, Gual Sole A, Montserrat Mestre O, Bueno Belmonte A, Colom Farran J. Detection and handling of alcohol problems in primary care in Catalonia. Aten Primaria. 2006;37:484–8. doi: 10.1157/13089078. [in Spanish] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johansson K, Akerlind I, Bendtsen P. Under what circumstances are nurses willing to engage in brief alcohol interventions? A qualitative study from primary care in Sweden. Addict Behav. 2005;30:1049–53. doi: 10.1016/j.addbeh.2004.09.008. [DOI] [PubMed] [Google Scholar]