Abstract
This study evaluated 1) the efficacy of packing autologous fat grafts around temporomandibular joint (TMJ) total joint prosthetic reconstructions to prevent fibrosis and heterotopic bone formation and 2) the effects on postsurgical joint mobility and jaw function. One hundred fifteen patients (5 males and 110 females) underwent TMJ reconstruction with total joint prostheses and simultaneous fat grafts (88 bilateral and 27 unilateral) for a total of 203 joints. The abdominal fat grafts were packed around the articulating portion of the joint prostheses after the fossa and mandibular components were stabilized. Patients were divided into two groups: group 1 (n = 76 joints) received Christensen total joint prostheses, and group 2 (n = 127 joints) received TMJ Concepts total joint prostheses. Clinical and radiographic assessments were performed before surgery, immediately after surgery, and at long-term follow-up. In group 1, maximal incisal opening (MIO) increased 3.5 mm, lateral excursions (LE) decreased 0.2 mm, and jaw function improved 1.9 levels. In group 2, MIO increased 6.8 mm, LE decreased 1.4 mm, and jaw function improved 2.4 levels. The improvement for MIO and patient perception of jaw function in both groups was statistically significant; no significant difference was found for LE. There was no radiographic or clinical evidence of heterotopic calcifications or limitation of mobility secondary to fibrosis in either group. Twenty-five Christensen prostheses (33%) were removed because of device failure and/or metal hypersensitivity; no fibrosis or heterotopic bone formation was seen at surgical removal. Four TMJ Concepts prostheses (3%) were removed because of metal hypersensitivity. In all instances, removal of the prostheses was unrelated to the autologous fat grafting. Ten patients (8.7%) developed complications involving the fat donor site: two patients (1.8%) developed abdominal cysts requiring surgery, and eight patients (6.9%) developed seroma formation requiring aspiration. Autologous fat transplantation is a useful adjunct to prosthetic TMJ reconstruction to minimize the occurrence of excessive joint fibrosis and heterotopic calcification, consequently providing improved range of motion and jaw function.
The first report of autologous fat transplantation appeared in the literature in 1893 (1). Since then, autologous fat grafting has been used extensively in humans for various applications. Among these are aesthetic procedures for contour augmentation, particularly in the maxillofacial region, and ablative procedures, as in the treatment of various injuries of the frontal sinus. The use of autologous fat grafts in the treatment of ankylosis of the temporomandibular joint (TMJ) was reported by Blair (2) in 1913 and by Murphy (3) in 1914. In 1992, Tomas (4) reported the use of autologous fat transplantation to prevent heterotopic bone formation after hip replacement surgery in six patients. In orthopedics, radiation of the operated area is generally used to prevent het-erotopic bone formation (5–7).
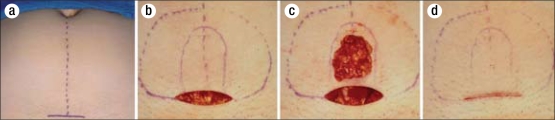
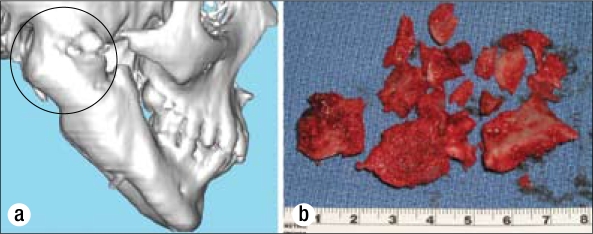
The problem of heterotopic calcification is frequently seen after placement of alloplastic materials in the TMJ, particularly when alloplasts of Proplast/Tefon (Vitek Inc., Houston, TX) or Silastic (Dow-Corning, Midland, MO) have been previously implanted (8) (Figure 1). Heterotopic bone can also result from trauma, reactive arthritis, osteoarthritis, sepsis, inflammation, and connective tissue/autoimmune diseases such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and scleroderma. These calcifications can cause continued worsening pain and a progressive decrease in range of motion that may lead to bony ankylosis. A variable amount of fibrosis and possibly reactive tissue are commonly associated with the heterotopic bone, thereby worsening the effect. Pharmacologic treatment cannot predictably prevent the development of these unwanted tissues in the TMJ. Durr and Turlington (9) have reported favorable outcomes in two thirds of their patients with TMJ ankylosis by using postsurgical radiation. However, significant concerns exist about the effects of this treatment on nearby structures (e.g., brain, orbit, parotid gland). Additionally, the TMJ region is more vascular than the hip, and the frequent presence of particulated polymeric materials may preclude a successful result with radiation. Other surgeons' experiences with radiation therapy in patients with recurrent TMJ ankylosis have not been favorable (personal communication, Dr. Robert V. Walker, Dallas, TX, and Dr. Stephen S. Fennell, Athens, GA).
Figure 1.
A coronal tomogram of a prosthetically reconstructed TMJ joint demonstrates heterotopic bone formation (arrows) between the mandibular ramous and medial side of the fossa. No fat graft was placed around the prosthesis at surgery.
In 1992 Wolford developed the philosophy and technique for placing fat grafts around TMJ total joint prostheses to prevent heterotopic bone formation, decrease fibrosis, improve pain levels, and increase jaw function. Wolford and Karras (10) published the first study evaluating fat grafts placed around TMJ total joint prostheses. Fifteen patients (2 males and 13 females) underwent TMJ reconstruction with Techmedica (Techmedica, Inc., Camarillo, CA) custom-made total joint prostheses (currently manufactured by TMJ Concepts Inc., Ventura, CA). Surgery was bilateral in 7 patients and unilateral in 8, for a total of 22 joints. All patients had autologous fat harvested from the abdomen grafted around the articulating portion of the joint prostheses after the fossa and mandibular components had been stabilized. Twenty patients (2 males and 18 females) who received Techmedica total joint prostheses without fat grafts served as a control. There were 17 bilateral and 3 unilateral cases, for a total of 37 joints.
In the fat graft group, average maximum incisal opening (MIO) was 26.9 mm preoperatively and 38.7 mm at long-term follow-up, an improvement of 11.8 mm. Contralateral excursive movements (LE) averaged 2.3 mm preoperatively and 2.2 mm at long-term follow-up. In the non–fat-grafted group, the average MIO was 26.8 mm preoperatively and 33.1 mm at long-term follow-up, an improvement of 6.3 mm. Contralateral excursive movements averaged 3.2 mm preoperatively and 1.7 mm at long-term follow-up. The differences in measured function between the two groups were statistically significant (P ≤ 0.01). Although both groups experienced a decrease in pain, no significant difference was noted in the patients' perception of their pain level at long-term follow-up. There was no radiographic or clinical evidence of heterotopic calcifications or limitation of mobility secondary to fibrosis in any of the fat-grafted group, while 7 control patients (35%) developed heterotopic bone and required reoperation. This initial study proved that autologous fat transplantation was a useful adjunct to prosthetic TMJ reconstruction. The technique minimizes the occurrence of excessive joint fibrosis and heterotopic calcification and consequently provides improved range of motion. No other published studies in the literature involve the placement of fat grafts around total joint prostheses.
This study evaluates the treatment outcomes after TMJ reconstruction with total joint prostheses and fat grafts in a much larger group of patients.
PATIENTS AND METHODS
Inclusion criteria for this study were as follows: 1) patients had unilateral or bilateral TMJ reconstruction using total joint prostheses with abdominal fat grafts packed around the prostheses' area of articulation; 2) all patients were operated on by one surgeon (LMW) at Baylor University Medical Center in Dallas, Texas; 3) adequate records were available for analysis; and 4) the minimum follow-up was 1 year. Records of 115 consecutive patients (5 males and 110 females) meeting these criteria were evaluated; 88 patients had bilateral and 27 had unilateral TMJ reconstruction, for a total of 203 joints. The patients were divided into two groups. Group 1 (n = 42; 76 joints) received Christensen total joint prostheses (TMJ Implants Inc., Golden, CO) (Figure 2), and group 2 (n = 73; 127 joints) received TMJ Concepts total joint prostheses (TMJ Concepts Inc., Ventura, CA) (Figure 3).
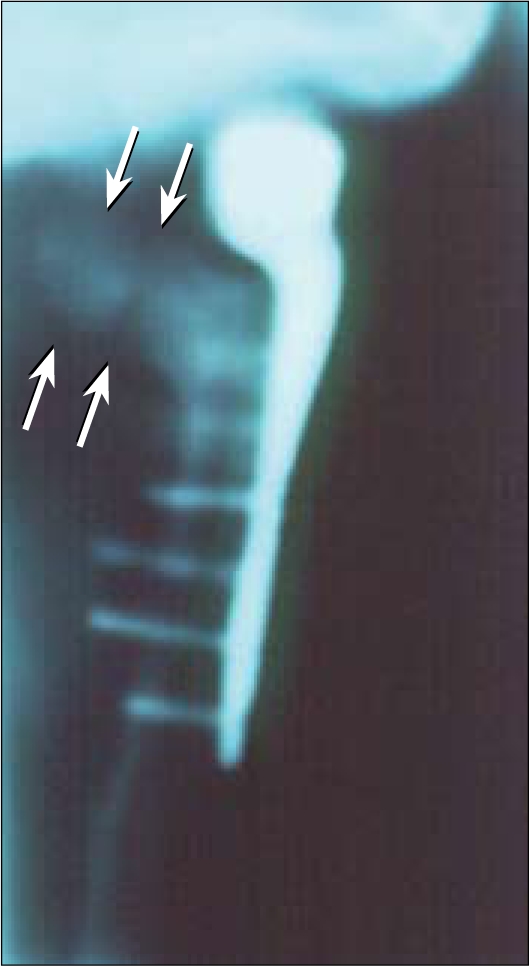
Figure 2.
The Christensen prosthesis is an off-the-shelf device with three selections for the man-dibular component and over 40 selections for the fossa component. The best-fitting components are selected to fit the anatomy. These devices have metal-on-metal articulations.
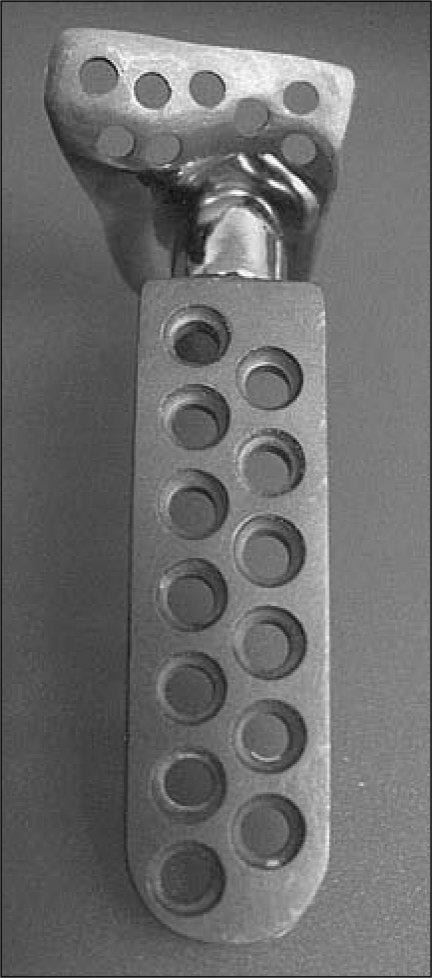
Figure 3.

The TMJ Concepts total joint prosthesis is a patient-fitted device, constructed on a three-dimensional model and designed for each patient's specific anatomical requirements. The devices have metal-on-polyethylene articulations.
For all patients, total joint prostheses were placed and stabilized, and then autologous fat harvested from the abdomen was packed around the articulating portion of the prostheses. Clinical and radiographic assessments were performed before surgery (T1), immediately after surgery (T2), and at longest follow-up (T3). Objective clinical evaluations of MIO and LE were determined from T1 and T3 data, whereas jaw function was subjectively evaluated according to a numerical analog scale (0 = normal jaw function and 10 = no jaw function). Student's t test was used to determine statistical significance at the P ≤ 0.01 level. Radiographic evaluation compared T2 and T3 x-rays (panographic x-rays, linear tomograms, and lateral cephalograms) for the presence of postsurgical heterotopic bone formation around the prostheses. Donor site complications were also evaluated.
Surgical technique
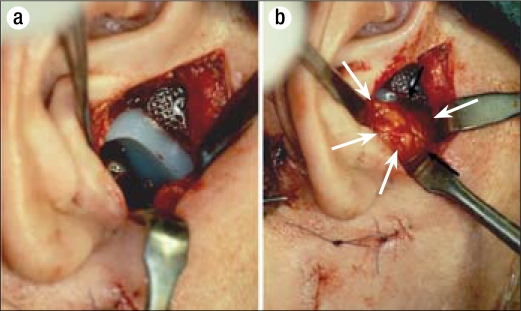
The prostheses were placed through endaural or preauricular and submandibular incisions, as previously described (8), after thorough debridement of the region. Following stabilization of all condylar and fossa components, fat was harvested from the abdomen. The abdomen was prepared and draped in routine fashion from above the umbilicus to the pubic region. The superior portion of the pubic hair was shaved, if necessary, to place the incision as low as possible on the abdomen for optimal cosmesis. If an existing scar was present in the lower abdomen, this site was used instead.
A 4- to 5-cm transverse incision was made in the midline through skin and subcutaneous tissue to expose the abdominal fat pad (Figure 4a, 4b). The skin was widely undermined superiorly and laterally, taking care to maintain a 3- to 5-mm layer of fat on the skin side. The initial incision was then deepened into the fat a variable distance depending on the fat pad thickness and the amount of graft required (usual range per joint, 5–20 cc). The fat was then widely undermined superficial to the rectus abdominis muscle fascia to a similar extent as the overlying skin dissection. The desired amount of graft was harvested in a single block from the midline region (Figure 4c). To allow for shrinkage and errors in estimation, this amount was 20% to 30% more than the estimated amount needed to fill the dead space in the TMJ region. Meticulous hemostasis was achieved with electrocautery, and the defect in the fat pad was closed by advancing the lateral fat faps toward the midline and suturing with 3-0 polyglactin. The skin incision was closed with subcutaneous sutures of 4-0 polydioxanone (Figure 4d), and adhesive skin closures were placed for reinforcement. To minimize the incidence of hematoma and seroma formation, a pressure dressing of fluffed gauze and elastic tape was applied and maintained for approximately 3 days before removal.
Figure 4.
Fat graft harvesting technique used in this study. (a) The fat graft is harvested from the abdomen, usually through a 4- to 5-cm incision generally made in the suprapubic area. (b) The outer dashed line is the extent of undermining of the skin and beneath the fat pad. The inner solid line denotes the fat graft to be harvested. (c) The abdominal fat graft harvesting is complete. (d) 3-0 polyglactin sutures are used to close the deep fat layers so no depression in the harvest area will be evident. The skin is closed with subcuticular suturing.
The graft was immediately placed through the endaural or preauricular incision to fill the dead space around the articulating portion of the prosthetic components (Figure 5). In bilateral cases, the graft was divided into equal portions, and one portion was stored in iced normal saline until placement in the second side. The fat was packed into the TMJ region relatively firmly, without causing excessive tissue damage to the graft. The wound was closed in routine layered fashion.
Figure 5.
Surgical technique used in this study. (a) The fossa component prosthesis is placed through an endaural or preauricular incision. The mandibular component is placed through a submandibular incision. (b) The abdominal fat graft (arrows) is packed into the joint space to prevent heterotopic bone formation and fibrosis.
RESULTS
The average patient follow-up period was 31.2 months (range, 12–65 months). The study results are summarized in the Table. Both groups had a statistically significant improvement in MIO and patient perception of jaw function at longest follow-up, but the improvement was greater for group 2. Neither group had a significant difference in LE. There was no radiographic evidence of heterotopic bone formation in either group at longest follow-up.
Table.
Objective and subjective clinical data for 115 patients before and ≥1 year after temporomandibular joint total joint prosthetic reconstructions with autologous fat grafts
| MIO (mm) | LE (mm) | Jaw function∗ | |||||||
| Group | T1 | T3 | T3 – T1 | T1 | T3 | T3 – T1 | T1 | T3 | T3 – T1 |
| 1: Christensen total joint prostheses (n = 76 joints) | 23.6 | 27.1† | 3.5 | 1.5 | 1.3 | –0.2 | 7.7 | 5.8† | 1.9 |
| 2: TMJ Concepts total joint prostheses (n = 127 joints) | 27.6 | 34.4† | 6.8 | 3.4 | 2.0 | –1.4 | 7.6 | 5.2† | 2.4 |
∗Assessed through a numerical analog score: 0 = normal function; 10 = no function.
†P ≤ 0.01 for T3 vs T1.
MIO indicates maximum incisal opening; LE, maximum lateral excursion; T1, before surgery; T3, at long-term follow-up.
Of the 76 Christensen prostheses, 25 (33%) were removed because of elevated pain levels due to device failure (fracture or loosening of the fossa component) or metal hypersensitivity caused by metallosis from the metal-on-metal articulation. No fibrosis or heterotopic bone formation around the prostheses was observed at surgical removal. The removed Christensen prostheses were replaced with TMJ Concepts total joint prostheses and simultaneous fat grafting around the articulating area of the prostheses. Of the 127 TMJ Concepts prostheses, 4 (3%) were removed from two patients because of severe metal hypersensitivity: one patient was sensitive to molybdenum and one to nickel. The latter patient developed dense fibrous tissue around the prostheses, but no bone. The other patient maintained the fat grafts around her prostheses. The prostheses in these patients were replaced with TMJ Concepts prostheses that had ion-treated titanium condylar heads, eliminating the cobalt-chromium-molybdenum alloy head that also contained 1% nickel. Fat grafts were again placed around the prostheses.
The fat donor sites were evaluated, and 10 patients (8.7%) developed complications: two extremely obese patients (1.2%) developed abdominal cysts superficial to the rectus abdominis muscle that required surgical removal; eight patients (6.9%) developed seroma formation requiring aspiration, and two of these eight patients required drain placement postsurgery for evacuation of persistent seroma formation.
CASE PRESENTATIONS
Case 1
This 45-year-old man (Figure 6a, 6b) was referred to the senior author after undergoing 14 previous failed right TMJ surgeries, including procedures using devices that contained Proplast/Teflon. He was 2 years post–TMJ reconstruction with an Osteomed total joint prosthesis (Osteomed Inc., Dallas, TX) without the placement of a fat graft around it at that surgery. He had severe TMJ and myofascial pain, headaches, and difficulty eating. He presented with a class I occlusion on the left side and a class II occlusion on the right side (Figure 7a–c). There was massive heterotopic bone development and bony ankylosis surrounding the right TMJ (Figure 8a), a foreign body giant cell reaction secondary to the previous Proplast/Teflon materials, and a severely limited incisal opening of 20 mm with no translation of the right condyle.
Figure 6.
Case 1. (a, b) This 45-year-old man was referred after 14 previous failed right TMJ surgeries; the most recent involved right TMJ reconstruction with a total joint prosthesis (Osteomed system) without a fat graft. He had severe TMJ and myofascial pain, headaches, and difficulty eating. (c, d) The patient 2 years after right TMJ debridement, removal of heterotopic bone and the Osteomed prosthesis, TMJ reconstruction with a TMJ Concepts patient-fitted total joint prosthesis, and fat grafting.
Figure 7.
Case 1. (a, b, c) Presurgery, the patient had a class I occlusion on the left side and a class II occlusion on the right side. (d, e, f) The occlusion remained stable 2 years after surgery.
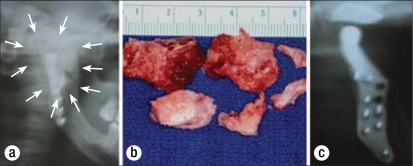
Figure 8.
Case 1. (a) The presurgical panographic x-ray showed massive heterotopic bone formation (outlined by arrows) around the Osteomed prosthesis. (b) The heterotopic bone was removed in sections. (c) A 10-year postsurgical radiograph shows the effectiveness of the fat graft in preventing heterotopic bone development.
The TMJ reconstructive surgery was performed in one operation and included 1) unilateral right TMJ debridement and removal of heterotopic bone formation around the old prosthesis (Figure 8b); 2) removal of the Osteomed prosthesis; 3) unilateral right TMJ reconstruction with patient-fitted TMJ Concepts total joint prosthesis (Figure 5a); and 4) packing of autologous fat graft around the right TMJ prosthesis (Figure 5b). At 2 years postsurgery, the patient showed good stability (Figure 6c, 6d) with elimination of TMJ pain, headaches, and myofascial pain and improved jaw function. The occlusion remained stable (Figure 7d–f). At 10 years postsurgery, his incisal opening was 42 mm with 2 to 3 mm of translation of the right condyle and no radiographic evidence of heterotopic bone formation (Figure 8c).
Case 2
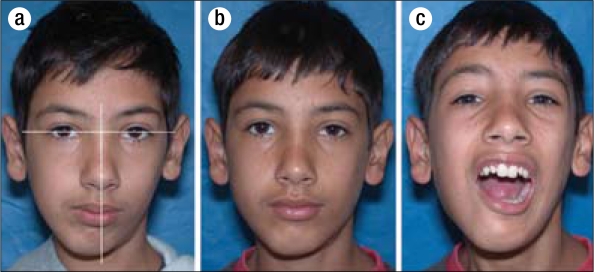
This 12-year-old boy developed right TMJ ankylosis at the age of 1 year secondary to sepsis (Figure 9a). Two previous attempts at surgical correction by rib grafting had failed. He had only 3 mm of incisal opening and was developing significant dental problems because of his inability to receive dental care; he also had severe facial asymmetry as well as sleep apnea symptoms. A 3-D computed tomography scan demonstrates the magnitude of the ankylosis (Figure 10a). A TMJ Concepts total joint prosthesis was manufactured to reconstruct the TMJ as well as advance and vertically lengthen the right mandibular ramus (Figure 11a). He underwent the following procedures in one stage: 1) right TMJ removal of a large mass of heterotopic bone (Figure 10b); 2) reconstruction of the TMJ and mandibular advancement with TMJ Concepts total joint prosthesis (Figure 11a); and 3) fat graft packed around the prosthesis and area of previous heterotopic bone formation to prevent bone from redeveloping. The patient was evaluated 2 years postsurgery and showed improved facial balance and good jaw function (35-mm opening) without pain (Figure 9b, 9c). At the 2-year evaluation, there was no radiographic evidence of heterotopic bone formation (Figure 11b).
Figure 9.
Case 2. (a) This 12-year-old boy had right TMJ ankylosis, and two attempts at correction by rib grafting (without fat grafts) had failed. With only 3 mm of incisal opening, he was developing significant dental problems, marked facial asymmetry, and sleep apnea. (b, c) The patient 2 years after right-side TMJ reconstruction and mandibular advancement with a TMJ Concepts total joint prosthesis and fat graft. He had improved facial balance and good jaw function (35-mm opening) without pain.
Figure 10.
Case 2. (a) A 3-D computed tomography scan demonstrates the magnitude of the heterotopic bone and joint ankylosis. (b) The heterotopic bone was removed in sections.
Figure 11.
Case 2. (a) A TMJ Concepts total joint prosthesis was custom made to reconstruct the TMJ and advance and vertically lengthen the right mandibular ramus. A fat graft was packed around the prosthesis to prevent heterotopic bone from redeveloping. (b) The tomogram shows no heterotopic bone formation around the prosthesis 2 years after surgery.
DISCUSSION
The formation of extensive fibrosis and heterotopic bone has been problematic after total joint reconstruction of the TMJ, as well as from other types of TMJ arthrotomies (Figures 1, 8a, 10a). This is particularly true of multiply operated joints and joints with previously failed alloplastic implants. These complications have been reported to occur after both prosthetic and autologous joint reconstructions (11). Fibrosis is related to scar tissue deposition, especially in multiply operated joints, with a persistent inflammatory response possibly contributing in joints with previously failed alloplasts. Heterotopic bone may be deposited in a similar reaction after alloplastic implant failure. Additionally, the presence of dead space after extensive joint debridement leads to hematoma formation in this area, with subsequent organization. Pluripotent cells may then be induced to differentiate into fibroblasts and osteoblasts, with deposition of collagen and bone, respectively. In excessively fibrotic joints, there is a decrease in vascularity and thereby a decrease in oxygen tension in the surrounding tissues that can lead to the transformation of fibrous tissue into cartilage and bone (12).
In the orthopedic experience, various pharmacologic agents, most notably indomethacin and etidronate, have been used with varying success (13, 14). Pharmacologic therapy has been suggested for use after prosthetic TMJ reconstruction, but no substantial data exist regarding its effectiveness (8). In the senior author's (LMW's) experience with these medications, the results have been very disappointing.
Radiation treatment of the operated area within 4 days of prosthetic hip reconstruction is now common practice to control heterotopic bone formation in orthopedic procedures. However, local radiation of the TMJ raises concerns regarding potential adverse effects on adjacent vital structures (i.e., eye and associated structures, brain, middle ear, and parotid gland), and it may be ineffective due to the substantially greater vascularity of the maxillofacial region. However, Durr et al (9) reported on 10 patients (15 TMJs) with bony ankylosis surgically managed with either costochondral grafts, gap arthroplasty, or debridement of heterotopic bone and treated early postoperatively with radiation, 10 Gy in five fractions. With a mean follow-up of 19 months, 10 of 15 TMJs did not show heterotopic bone development. The only complication identified was parotitis in three patients (30%).
The rationale for placing autologous fat grafts is to obliterate the dead space present around the joint prosthesis, thus preventing the formation and subsequent organization of a hematoma. Creating this physical barrier serves to minimize the presence of pluripotent cells and prevents the formation of extensive fibrosis and heterotopic calcifications. It may also isolate any residual reactive tissue from previous alloplastic failure to the periphery of the region, minimizing its formation around the joint components. The net result, as evidenced by the data collected, is a decrease in and perhaps elimination of the incidence of heterotopic bone formation and an improvement in jaw function.
The ultimate fate of the transplanted fat is unknown. Studies of fat transplantation to other anatomic areas show a variable amount of resorption, with a decrease in volume ranging from 20% to 75% (15, 16). As an adjunct to prosthetic joint reconstruction, the ultimate resorption of a portion of the graft may not be detrimental to the result. If the formation of the initial hematoma, fibrosis, and reactive tissue can be prevented, the incidence of complications may be reduced. We have had an occasional opportunity to clinically and histo logically evaluate fat-grafted TMJ Concepts joints postsurgery (Figure 12). Clinically, the fat grafts appeared viable, with some samples with strands of collagen present but no evidence of an inflammatory process. The consistency of the tissue around the prosthesis was significantly softer than that seen in the non–fat-grafted patients. Histologically, viable fat was observed (Figure 12).
Figure 12.
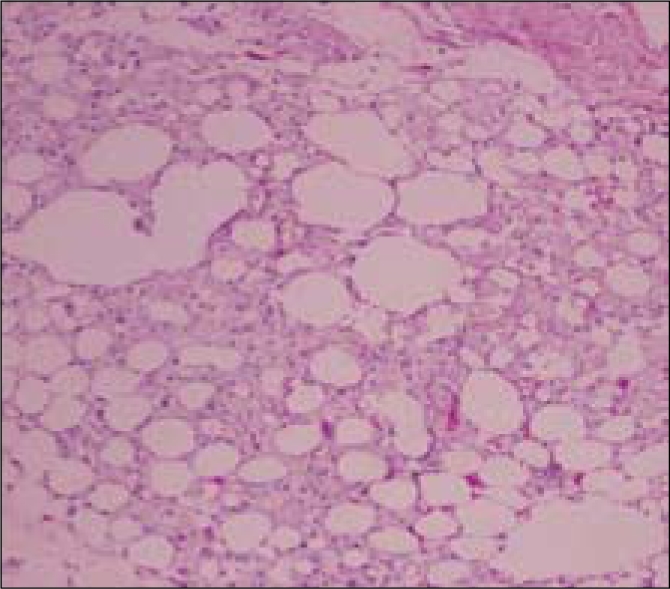
Histological examination of a fat graft biopsy taken 4 years after implantation around a TMJ Concepts total joint prosthesis shows viable fat still present without evidence of inflammation, heterotopic bone formation, or significant fibrosis.
The technique of graft procurement is straightforward, with minimal potential for complications. In our surgeries, the senior author harvests the fat grafts just prior to graft placement, requiring only about 15 minutes of additional surgical time. However, some surgeons may prefer to have two surgical teams working concurrently so the operation is not prolonged. Harvesting the fat grafts prior to beginning the TMJ reconstruction is not recommended, as this would require the grafts to be “on the table” for an extended time, likely resulting in significant loss of graft viability. In bilateral cases, it usually takes at least 4 hours to prepare the TMJs and place the prostheses before the fat grafts can be placed. Therefore, procuring the fat graft just before placement will maximize graft viability.
Possible complications of abdominal fat graft harvesting include hematoma, seroma, infection, ileus, and inadvertent peritoneal perforation. To date, we have had no infections, peritoneal perforations, or post-surgical ileus. In our first several patients, we inserted a suction drain and left it in position for approximately 3 days to prevent hematoma or seroma formation. However, with careful attention to hemostasis, drain placement at surgery is rarely needed. Placing a fluffed gauze dressing and securing with elastic tape or, alternatively, placing a Velcro-secured abdominal binder minimizes the incidence of this complication.
Autologous fat grafting appears to be a useful adjunct to prosthetic reconstruction of the TMJ and may prove to be similarly beneficial in autologous reconstruction. Graft procurement is quick and easy, with minimal morbidity.
CONCLUSION
The results of this study demonstrate the efficacy of TMJ reconstruction with total joint prostheses and simultaneous autologous fat grafts to the articulating area of the joint. A statistically significant improvement in MIO and patient perception of jaw function occurred in both groups. The removal of 25 Christensen prostheses and 4 TMJ Concepts prostheses was due to complications associated with prosthesis failure or metal hypersensitivity, but was not fat graft related. No evidence of fibrosis or heterotopic bone formation was radiographically or clinically observed. The most common complication found in the donor area was seroma, which was usually easily treated with aspiration and a pressure dressing.
References
- 1.Neuber H. Fettransplantation. Chir Kong Verhandl. 1893;1:66. [Google Scholar]
- 2.Blair VP. Operative treatment of ankylosis of the mandible. Trans South Surg Assoc. 1913;28:435. [Google Scholar]
- 3.Murphy JB. Arthroplasty for intra-articular bony and fibrous ankylosis of the temporomandibular articulation. JAMA. 1914;62:1783. [Google Scholar]
- 4.Tomas BJ. Heterotopic bone formation after total hip arthroplasty. Orthop Clin North Am. 1992;23(2):347–358. [PubMed] [Google Scholar]
- 5.Fingeroth RJ, Ahmed AQ. Single dose 6 Gy prophylaxis for heterotopic ossification after total hip arthroplasty. Clin Orthop Relat Res. 1995;317:131–140. [PubMed] [Google Scholar]
- 6.DeFlitch CJ, Stryker JA. Postoperative hip irradiation in prevention of heterotopic ossification: causes of treatment failure. Radiology. 1993;188(1):265–270. doi: 10.1148/radiology.188.1.8511309. [DOI] [PubMed] [Google Scholar]
- 7.Maloney WJ, Jasty M, Willett C, Mulroy RD, Jr, Harris WH. Prophylaxis for heterotopic bone formation after total hip arthroplasty using low-dose radiation in high-risk patients. Clin Orthop Relat Res. 1992;280:230–234. [PubMed] [Google Scholar]
- 8.Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994;52(1):2–10. doi: 10.1016/0278-2391(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 9.Durr ED, Turlington EG, Foote RL. Radiation treatment of heterotopic bone formation in the temporomandibular joint articulation. Int J Radiat Oncol Biol Phys. 1993;27(4):863–869. doi: 10.1016/0360-3016(93)90461-4. [DOI] [PubMed] [Google Scholar]
- 10.Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg. 1997;55(3):245–251. doi: 10.1016/s0278-2391(97)90535-8. [DOI] [PubMed] [Google Scholar]
- 11.MacIntosh RB. Costochondral and dermal grafts in temporomandibular joint reconstruction. Oral Maxillofac Surg Clin North Am. 1989;1:363–397. [Google Scholar]
- 12.Hall BK. Cartilage: Biomedical Aspects, vol. 3. New York: Academic Press; 1988. pp. 322–323. [Google Scholar]
- 13.Francis MD, Russell RG, Fleisch H. Diphosphonates inhibit formation of calcium phosphate crystals in vitro and pathological calcification in vivo. Science. 1969;165(899):1264–1266. doi: 10.1126/science.165.3899.1264. [DOI] [PubMed] [Google Scholar]
- 14.Ritter MA, Gioe TJ. The effect of indomethacin on para-articular ectopic ossification following total hip arthroplasty. Clin Orthop Relat Res. 1982;(167):113–117. [PubMed] [Google Scholar]
- 15.Carpaneda CA, Ribeiro MT. Study of the histologic alterations and viability of the adipose graft in humans. Aesthetic Plast Surg. 1993;17(1):43–47. doi: 10.1007/BF00455048. [DOI] [PubMed] [Google Scholar]
- 16.Hörl HW, Feller AM, Biemer E. Technique for liposuction fat reimplantation and long-term volume evaluation by magnetic resonance imaging. Ann Plast Surg. 1991;26(3):248–258. doi: 10.1097/00000637-199103000-00007. [DOI] [PubMed] [Google Scholar]