Abstract
Dural arteriovenous fistulae are rare lesions composed of abnormal connections between meningeal arteries and the dural sinuses or lepto-meningeal veins. Treatment is challenging because of the small size and wide distribution of the myriad sites of fistulous connection. We present a case of a dural arteriovenous fistula presenting with visual deterioration, pulsatile tinnitus, and intracranial hypertension that was successfully treated with a multidisciplinary approach combining angiographic, surgical, and radiosurgical intervention. This is one of the largest of these formidable lesions treated in this fashion that has been reported.
Dural arteriovenous fstulae (DAVFs) are rare intracra-nial lesions consisting of direct, abnormal connections between meningeal arteries and the dural sinuses or leptomeningeal veins. The resulting shunt between the arterial and venous circulation can produce signifcant intracra-nial hypertension leading to hemorrhage, visual impairment, and hydrocephalus. Treatment is often demanding because of the ability of these lesions to recruit additional vessels (1, 2) and because of the small size of the individual fistulae, which can be distributed widely over a long extent of sinus wall. These difficulties are reflected by the long list of therapeutic strategies—surgical resection (3), occlusion of leptomeningeal drainage (4, 5), arterial or venous embolization (6, 7), radio-surgery (8–11), and a variety of combinations (12)—that have been used to treat these formidable lesions.
We report the successful treatment of a large DAVF presenting with progressive intracranial hypertension using a combined angiographic, surgical, and radiosurgical approach.
CASE DESCRIPTION
A 21-year-old woman presented with intractable headache, progressive visual loss, and pulsatile tinnitus. Physical examination demonstrated an occipital bruit and papilledema with optic nerve swelling. Magnetic resonance (MR) and computed tomography (CT) scans were obtained and a lumbar puncture performed. An ophthalmologist made the diagnosis of pseudotumor cerebri and treated her with acetazolamide and bilateral optic nerve sheath fenestrations. After recurrence of her headache and continued decline in her vision, an angiogram was obtained at an outside hospital that revealed a massive DAVF fed by meningohypophyseal and middle meningeal vessels, with fistulous involvement of the sagittal sinus, straight sinus, and both transverse sinuses (Figure 1).
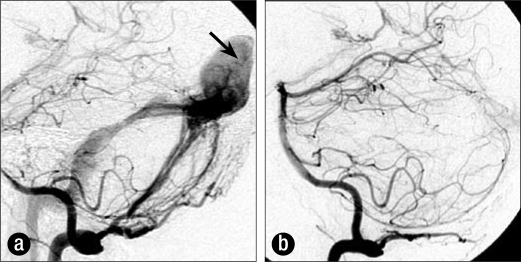
Figure 1.
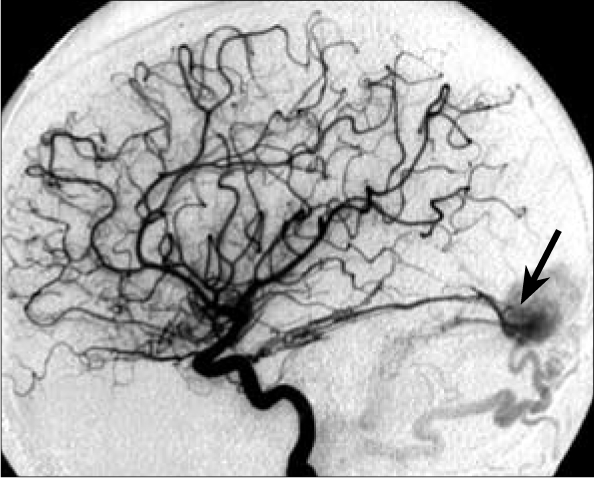
Lateral carotid angiogram prior to treatment showing large DAVF fed by meningohypophyseal vessels. Arrow indicates site of fistula.
She was referred to Baylor University Medical Center 7 months after initial presentation for multidisciplinary care. A treatment plan was formulated to perform multiple staged preoperative embolizations of the feeding vessels followed by craniotomy and surgical ligation of the remainder of the DAVF. Five intraarterial embolizations were conducted utilizing polyvinyl alcohol particles ranging in size from 250 to 500 microns in diameter. A total of 12 vascular pedicles arising from bilateral occipital, vertebral, middle meningeal, and superficial temporal arteries were occluded. Figures 2 and 3 progressive reduction of flow following two of these successive embolizations.
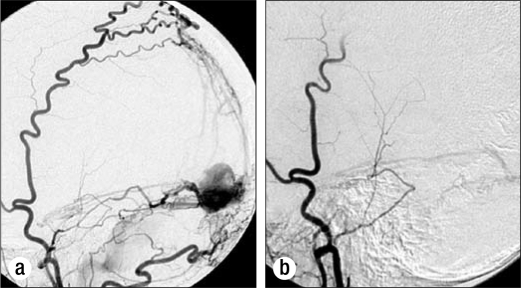
Figure 2.
(a) Right vertebral angiogram obtained prior to embolization of C1 muscular branches arising from the right vertebral artery. Note high flow within massively dilated torcular (arrow). (b) Angiogram after embolization.
Figure 3.
(a) Left external carotid angiogram 1 month following embolization shown in Figure 2. (b) Angiogram after embolization of left middle meningeal, superficial temporal, and occipital branches.
The patient subsequently underwent bilateral occipital and suboccipital craniotomies with ligation of the remaining feeding vessels and skeletonization of the sagittal sinus, straight sinus, and both transverse sinuses. Her vision improved and her headaches and bruit resolved. A small residual fistulous tract along the undersurface of the straight sinus was occluded by transvenous fibered platinum coil embolization.
An angiogram obtained 3 months after surgery demonstrated that the areas of fistulae were smaller but still present illustrate at the torcular and fed by tiny vessels inside the walls of the sagittal and straight sinus. Her visual felds again deteriorated and her headache and bruit returned. She then underwent Gamma Knife radiosurgery, receiving 20 Gy to a 45% isodose line encompassing the DAVF. The radiosurgical feld included all possible sites of fistulous connections, incorporating large segments of the sagittal sinus, straight sinus, torcular, and both transverse sinuses (Figure 4). Te volume of the 45% treatment isodose line was 54.5 cc.
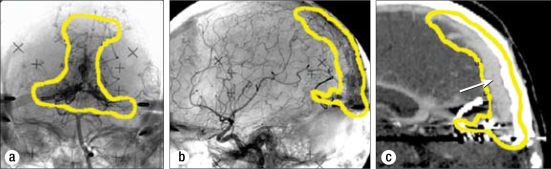
Figure 4.
(a) Anteroposterior vertebral angiogram showing 50% isodose line used to deliver Gamma Knife radiosurgery. (b) Lateral carotid angiogram showing 50% isodose line used to deliver radiosurgery. (c) Sagittal CT reconstruction showing that the majority of tissue within the radiation field was venous sinus (arrow) or bone. The wall of the venous sinuses—the presumed location of the fistulae—was contained within the isodose line.
Three months after radiosurgical treatment, the patient awoke without a bruit. Thirteen months later her bruit and headache had not recurred, and her visual acuity was 20/30. One year after that, a cerebral angiogram showed complete resolution of the DAVF (Figure 5).
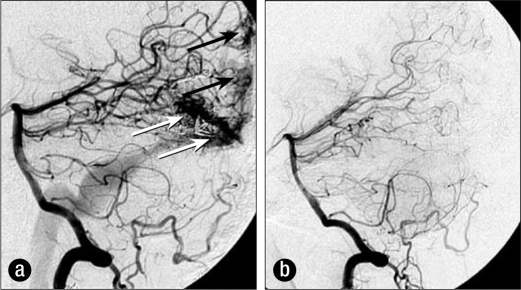
Figure 5.
(a) Left vertebral angiogram prior to Gamma Knife radiosurgery. Arrows indicate site of fistula. (b) Angiogram 2 years after radiosurgery showing complete obliteration of lesion.
DISCUSSION
Several series con-firm the importance of a multidisciplinary approach for the treatment of DAVFs. Seven patients with tentorial DAVFs were treated by Lewis et al (8) with linear accelerator radiosurgery; at least six also received embolization. Angiograms of three of these lesions (43%) showed obliteration, and a fourth lesion was obliterated during a subsequent embolization procedure. Two of the lesions were persistent, and one patient developed radiation-induced brainstem injury. The authors advocate a staged, multimodality approach to these lesions.
Friedman et al (10) reported the use of Gamma Knife ra-diosurgery in the treatment of 23 patients with DAVFs of the transverse and/or sigmoid sinuses. Twenty of these patients also underwent transarterial embolization. Angiographic “total or near-total” obliteration was confirmed in 11 of the patients (48%), and a reduction in lesion size by more than 50% was confirmed in an additional six patients. No hemorrhage or radiation-related complication was seen over the mean follow-up period of 50 months. These authors also advocated a staged approach using both embolization and radiosurgery.
Pan et al (9) reported 19 patients with DAVFs of the transverse or sigmoid sinus treated with Gamma Knife radiosurgery. Nine of the patients had prior craniotomy or embolization, and 11 were treated primarily with radiosurgery. Angiographic obliteration was confirmed in nine patients (47%), and MR evidence of obliteration was obtained in an additional two patients. No radiation-associated morbidity was seen in the median follow-up period of 19 months.
Koebbe et al (11) reported 23 DAVFs in 18 patients. The n patients were treated with embolization and Gamma Knife radiosurgery, and eight patients received radiosurgery alone. An-giographic obliteration was confirmed in eight patients (44%), and MR or CT evidence of obliteration was obtained in an additional four patients. During the mean follow-up period of 43 months, one patient developed a temporary hemiparesis after radiosurgery.
Overall, these data suggest that the angiographic obliteration rate of DAVFs treated with multimodality therapy that included radiosurgery is >40%, with higher rates of subtotal obliteration and low morbidity.
Intracranial hypertension has been reported as a presenting event for DVAFs (13, 14), and six of the 13 such patients reported by Cognard harbored DVAFs involving the transverse sinus (13). Our patient presented with intracranial hypertension associated with persistent headache and progressive visual loss despite treatment with acetazolamide and optic nerve sheath fenestration. A lumbar shunt was not offered due to the high risk of herniation (13).
For our patient, each of the three treatment options for this lesion—embolization, surgical occlusion, and radiosur-gery—held significant disadvantages when offered as the sole treatment. Definitive treatment with embolization alone would not have been feasible because of the large number of small feeding vessels and the difficulty of obliterating all of the myriad fistulae. Likewise, surgical skeletonization of the large venous sinuses and torcular would not have been effective because of the inability to directly obliterate the tiny fistulous vessels within the sagittal and straight sinus. Radiosurgery alone would have been prohibited by the difficulties in imaging the fistulous connections, the radiosurgical risk of treating such a large volume, and the almost certain progression of visual impairment during the interval of the 1 or 2 years required by radiosurgery to produce obliteration of the fistulae. In contrast, a multidisciplinary approach provided several advantages: initial embolization reduced the vascular burden and made surgery safer, early use of em-bolization and surgery addressed her rapidly declining vision, and radiosurgery obliterated the remaining small and difficult fistulous connections. As others have noted (8–11), the optimal treatment of these difficult lesions seems to be a combination of modalities tailored to the individual lesion rather than use of a single modality alone.
The radiosurgical plan was aggressive: the treatment volume is one of the highest that has been reported, the dose was relatively high, and the treatment isodose line was 45% rather than 50%. Although this combination of parameters usually poses a high risk of radionecrosis for parenchymal lesions, it was felt that the risks were relatively low because the treatment volume consisted mostly of sinus wall, blood, and bone and a relatively small amount of brain tissue. Furthermore, in analogy with doses for treatment of arteriovenous malformations and guided by prior series of DVAFs treated with Gamma Knife radiosurgery (9–11), it was felt that a high dose would be most likely to achieve obliteration. These dose-volume considerations for DAVFs have been discussed previously (9).
CONCULUSION
This case illustrates that large DAVFs presenting with significant intracranial hypertension can be successfully treated by a multidisciplinary approach that includes embolization, surgery, and radiosurgery. The lesion described here is among the largest that has been reported.
References
- 1.Nishijima M, Takaku A, Endo S, Kuwayama N, Koizumi F, Sata H, Owada K. Etiological evaluation of dural arteriovenous malformations of the lateral and sigmoid sinuses based on histopathological examinations. J Neurosurg. 1992;76(4):600–606. doi: 10.3171/jns.1992.76.4.0600. [DOI] [PubMed] [Google Scholar]
- 2.Uranishi R, Nakase H, Sakaki T. Expression of angiogenic growth factors in dural arteriovenous fstula. J Neurosurg. 1999;91(5):781–786. doi: 10.3171/jns.1999.91.5.0781. [DOI] [PubMed] [Google Scholar]
- 3.Sundt TM, Jr, Piepgras DG. Te surgical approach to arteriovenous malformations of the lateral and sigmoid dural sinuses. J Neurosurg. 1983;59(1):32–39. doi: 10.3171/jns.1983.59.1.0032. [DOI] [PubMed] [Google Scholar]
- 4.Collice M, D'Aliberti G, Talamonti G, Branca V, Boccardi E, Scialfa G, Versari PP. Surgical interruption of leptomeningeal drainage as treatment for intracranial dural arteriovenous fstulas without dural sinus drainage. J Neurosurg. 1996;84(5):810–817. doi: 10.3171/jns.1996.84.5.0810. [DOI] [PubMed] [Google Scholar]
- 5.Tompson BG, Doppman JL, Oldfeld EH. Treatment of cranial dural arteriovenous fstulae by interruption of leptomeningeal venous drainage. J Neurosurg. 1994;80(4):617–623. doi: 10.3171/jns.1994.80.4.0617. [DOI] [PubMed] [Google Scholar]
- 6.Bellon RJ, Liu AY, Adler JR, Jr, Norbash AM. Percutaneous transfemoral embolization of an indirect carotid-cavernous fstula with cortical venous access to the cavernous sinus. Case report. J Neurosurg. 1999;90(5):959–963. doi: 10.3171/jns.1999.90.5.0959. [DOI] [PubMed] [Google Scholar]
- 7.Roy D, Raymond J. Te role of transvenous embolization in the treatment of intracranial dural arteriovenous fstulas. Neurosurgery. 1997;40(6):1133–1144. doi: 10.1097/00006123-199706000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Lewis AI, Tomsick TA, Tew JM., Jr Management of tentorial dural ar-teriovenous malformations: transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg. 1994;81(6):851–859. doi: 10.3171/jns.1994.81.6.0851. [DOI] [PubMed] [Google Scholar]
- 9.Pan DH, Chung WY, Guo WY, Wu HM, Liu KD, Shiau CY, Wang LW. Stereotactic radiosurgery for the treatment of dural arteriovenous fstulas involving the transverse-sigmoid sinus. J Neurosurg. 2002;96(5):823–829. doi: 10.3171/jns.2002.96.5.0823. [DOI] [PubMed] [Google Scholar]
- 10.Friedman JA, Pollock BE, Nichols DA, Gorman DA, Foote RL, Staford SL. Results of combined stereotactic radiosurgery and transarterial em-bolization for dural arteriovenous fstulas of the transverse and sigmoid sinuses. J Neurosurg. 2001;94(6):886–891. doi: 10.3171/jns.2001.94.6.0886. [DOI] [PubMed] [Google Scholar]
- 11.Koebbe CJ, Singhal D, Sheehan J, Flickinger JC, Horowitz M, Kondziolka D, Lunsford DL. Radiosurgery for dural arteriovenous fstulas. Surg Neurol. 2005;64(5):392–399. doi: 10.1016/j.surneu.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 12.Kopitnik TA, Samson DS. Management of dural arteriovenous malformations. Contemp Neurosurg. 1995;17(1):1–8. [Google Scholar]
- 13.Cognard C, Casasco A, Toevi M, Houdart E, Chiras J, Merland JJ. Dural arteriovenous fstulas as a cause of intracranial hypertension due to impairment of cranial venous outfow. J Neurol Neurosurg Psychiatry. 1998;65(3):308–316. doi: 10.1136/jnnp.65.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silberstein P, Kottos P, Worner C, Glenn D, Shnier R, Davies M, Halmagyi GM, Hersch M. Dural arteriovenous fstulae causing pseudotumor cerebri syndrome in an elderly man. J Clin Neurosci. 2003;10(2):242–243. doi: 10.1016/s0967-5868(02)00329-6. [DOI] [PubMed] [Google Scholar]