Abstract
We discovered an emerging non-metropolitan mortality penalty by contrasting 37 years of age-adjusted mortality rates for metropolitan versus nonmetropolitan US counties. During the 1980s, annual metropolitan–nonmetropolitan differences averaged 6.2 excess deaths per 100000 nonmetropolitan population, or approximately 3600 excess deaths; however, by 2000 to 2004, the difference had increased more than 10 times to average 71.7 excess deaths, or approximately 35 000 excess deaths. We recommend that research be undertaken to evaluate and utilize our preliminary findings of an emerging US nonmetropolitan mortality penalty.
The dominant trend in recent US mortality has been one of decreasing death rates. However, population subgroups and geographic regions have differing mortality experiences. Early in US history, there was a substantially higher mortality rate in the cities often referred to as the urban “mortality penalty.” The spread of contagious diseases in densely populated sites, poor water quality, and inadequate sewage and garbage disposal explained the urban or metropolitan penalty.1 By 1940, improvements in public health, a growing public service infrastructure, and advances in health-care had eliminated the metropolitan penalty.1 Metropolitan–nonmetropolitan mortality rates had become similar.
The metropolitan–nonmetropolitan distinction, however, continues to be a fundamental framework in health discussions of residential aspects of public health policy, and of access to and disparities in health-care.2–5 Once metropolitan–nonmetropolitan mortality rates became similar, the focus of mortality research shifted to subnational regions and neighborhoods (e.g., the mortality disadvantages of the inner city or of the nonmetropolitan poor).6–7 In our study, we revisited national trends in mortality by examining 37 years of metropolitan–nonmetropolitan mortality patterns as part of a larger study investigating healthful and unhealthful places in the United States. We had anticipated demonstrating the advantages of using other spatial definitions as being more valuable in identifying geographic disparities in health outcomes. Instead, we found a recent emerging pattern of nonmetropolitan mortality disparities.
METHODS
We examined metropolitan–nonmetropolitan trends in mortality using the National Center for Health Statistics Compressed Mortality File.8–10 This file contains data on US county-level deaths by year from 1968 to 2004 (N = 3108). County mortality rates are calculated per 100 000 and age-adjusted to the year 2000 standard. Counties are classified according to the Office of Management and Budget definition of metropolitan and nonmetropolitan areas.11–12 A metropolitan area is a “core area containing a large population nucleus together with adjacent communities having a high degree of economic and social integration,” and non-metropolitan counties are those outside of the metropolitan statistical areas.12 The Rural–Urban Continuum (RUC) codes are used to classify metropolitan and non-metropolitan counties. Counties are reclassified every decade on the basis of revised RUC codes: 1974 codes were used for 1968 to 1975, 1983 codes were used for 1976 to 1985, 1993 codes were used for 1986 to 1995, and 2003 codes were used for 1996 to 2004.
Using these data, we calculated metropolitan–nonmetropolitan disparities as the difference in age-adjusted mortality per 100 000 between metropolitan and nonmetropolitan counties. Excess deaths for nonmetropolitan counties were calculated for a given time period as the difference between age-adjusted mortality rates per 100 000 for nonmetropolitan and metropolitan counties that was then multiplied by the nonmetropolitan population divided by 100 000.
RESULTS
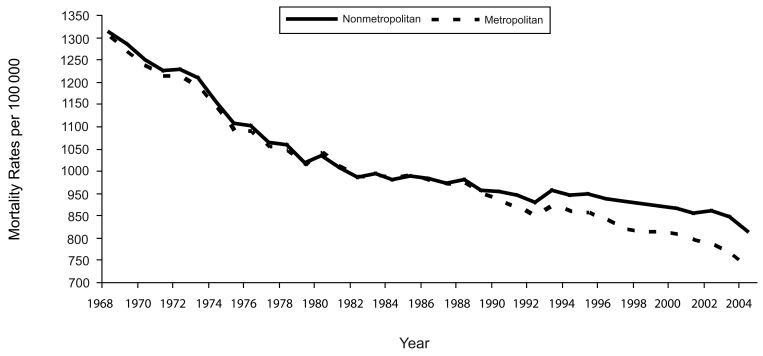
In Figure 1 ▶, mortality trends over 37 years are depicted for metropolitan–nonmetropolitan United States. The rates for 1968 through 1989 were consistent with the metropolitan transition, in that metropolitan and nonmetropolitan mortalities were similar and declining at about the same rates (average annual decline: metropolitan, 1.48%; nonmetropolitan, 1.47%). However, beginning in 1990, there appears to be a significant nonmetropolitan transition. Annual metropolitan mortality rates continued to decline at an average rate of 1.23%, but the decline in nonmetropolitan rates slowed markedly to an average of only 0.68% per year resulting in an increasing metropolitan–nonmetropolitan mortality disparity.
FIGURE 1—
Annual metropolitan and nonmetropolitan age-adjusted mortality per 100 000: United States, 1968–2004.
Note. The Rural–Urban Continuum codes were used to classify metropolitan and nonmetropolitan counties; 1974 codes were used for 1968 to 1975, 1983 codes were used for 1976 to 1985, 1993 codes were used for 1986 to 1995, and the 2003 codes were used for 1996 to 2004. Data were derived from the National Center for Health Statistics Compressed Mortality File numbers 2A, 2E, and 2J.8–10
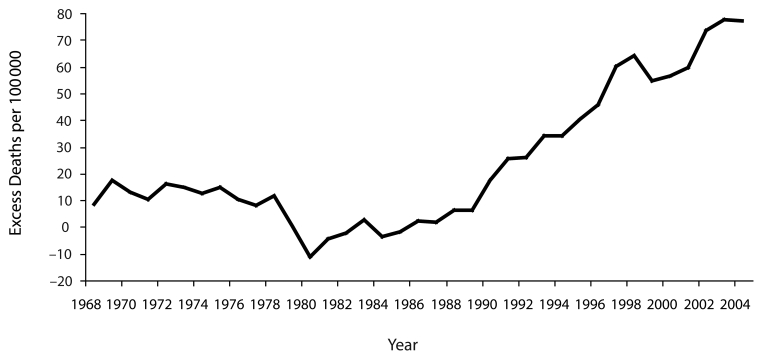
Metropolitan–nonmetropolitan mortality disparities have steadily increased (Figure 2 ▶). Before 1990, the average annual difference in mortality rates was approximately 5.8 excess deaths per 100000 in nonmetropolitan counties. Since 1990, the disparity has averaged 49.5 excess deaths per 100000. In the most recently available data, 2001 to 2004, the difference has increased to 71.7 excess deaths per 100000. This translates into about 35000 excess deaths each year. These excess deaths are equivalent to approximately 9% of the total mortality in the nonmetropolitan United States. During the period of 1990 to 2004, the total number of excess deaths attributable to the nonmetropolitan penalty is estimated to be about 389000 deaths in the nonmetropolitan United States. Table 1 ▶ provides summary data in multiyear increments for metropolitan–nonmetropolitan comparisons of age-adjusted mortality rates, excess deaths, and average annual percentage change in mortality as well as population data.8–10
FIGURE 2—
The magnitude of nonmetropolitan mortality disparities expressed in excess deaths per 100 000: United States, 1968–2004.
Note. The nonmetropolitan mortality disparities were calculated as nonmetropolitan age-adjusted mortality per 100 000 minus metropolitan age-adjusted mortality per 100 000. Data were derived from the National Center for Health Statistics Compressed Mortality File numbers 2A, 2E, and 2J.8–10
TABLE 1—
Average Age-Adjusted Mortality Rates (per 100 000), Excess Nonmetropolitan Deaths (per 100 000), and Average Annual Percentage Change in Age-Adjusted Mortality Rates for Metropolitan and Nonmetropolitan US Counties: 1968–2004
| 1968–1970 | 1971–1975 | 1976–1980 | 1981–1985 | 1986–1990 | 1991–1995 | 1996–2000 | 2001–2004 | |
| Age-adjusted mortality rates, per 100 000 | ||||||||
| Metropolitan | 1267.73 | 1169.37 | 1048.61 | 991.88 | 960.51 | 910.95 | 869.83 | 820.44 |
| Nonmetropolitan | 1280.48 | 1182.81 | 1054.96 | 989.63 | 968.98 | 942.69 | 926.72 | 892.1 |
| Excess nonmetropolitan deaths, per 100 000 | 12.75 | 13.44 | 6.36 | −2.26 | 8.47 | 31.74 | 56.89 | 71.66 |
| Average annual change in mortality rates, % | ||||||||
| Metropolitan | 0.026 | 0.025 | 0.008 | 0.01 | 0.011 | 0.006 | 0.01 | 0.022 |
| Nonmetropolitan | 0.024 | 0.024 | 0.013 | 0.009 | 0.007 | 0.001 | 0.006 | 0.014 |
| Population, no. | ||||||||
| Metropolitan | 146 529 956 | 152 418 679 | 167 446 631 | 176 615 363 | 192 200 648 | 203 337 773 | 222 389 186 | 237 354 699 |
| Nonmetropolitan | 53 507 258 | 56 990 756 | 52 910 169 | 55 071 637 | 50 089 805 | 51 695 096 | 47 595 451 | 49 010 211 |
| Counties, no. | ||||||||
| Metropolitan | 630 | 630 | 716 | 716 | 815 | 815 | 1060 | 1060 |
| Nonmetropolitan | 2443 | 2443 | 2357 | 2357 | 2258 | 2258 | 2013 | 2013 |
Note. The 1968 information is the earliest available mortality data for this period, and the 2004 information is the most recently available mortality data for this period. The data provided are average annual estimates calculated for the specified time periods. In the analyses, metropolitan–nonmetropolitan classifications 1974 Rural–Urban Continuum (RUC) codes were used for 1968 to 1975, 1983 RUC codes were used for 1976 to 1985, 1993 RUC codes were used for 1986 to 1995, and 2003 RUC codes were used for 1996 to 2004. The various RUC codes were on the basis of data collected during decennial census (1970, 1980, 1990, and 2000). The metropolitan–nonmetropolitan classification for each RUC-code period was lagged by 5 years with the decennial year as the midpoint. Notable trends in the data include (1) improvements in mortality rates throughout the time period for both metropolitan and nonmetropolitan counties, (2) excess deaths for nonmetropolitan counties increase markedly after 1990, (3) the rate of improvement for nonmetropolitan counties was only about half the rate for metropolitan counties during the 2001 to 2004 period.
Source. Data are derived from the National Center for Health Statistics Compressed Mortality File Nos. 2A, 2E, and 2J.8–10
DISCUSSION
A possible explanation for the emergence of the nonmetropolitan mortality penalty is based on the observation that access to health care is the most pervasive health disparity in the nonmetropolitan United States.2 If health-care is becoming significantly more effective in prolonging life, then limited access to healthcare is becoming profoundly harmful to the nonmetropolitan US population, hence, the nonmetropolitan mortality penalty.
We found substantial evidence that the United States is experiencing a growing non-metropolitan mortality penalty that began about 1990 and is now becoming a major aspect of the nation’s geographic health. Our finding raises several important questions: What is the cause of this shift in nonmetropolitan mortality rates? Does the nonmetropolitan penalty exist for all disease groups or is it limited to 1 or more specific causes of death? Are the metropolitan–nonmetropolitan disparity trends concentrated in specific regions of the United States and among specific population subgroups—e.g., minorities, the poor, etc.?3,13,14 Will an analysis of the 9 RUC categories lead to a better understanding of the nature of metropolitan–nonmetropolitan trends and disparities?3 Are causes underlying the growing nonmetropolitan mortality penalty subject to intervention? What are the health policy implications of a growing nonmetropolitan mortality penalty? We suggest that an ambitious research agenda needs to be undertaken to meaningfully evaluate and utilize our preliminary finding of an emerging nonmetropolitan mortality penalty in the United States.
Acknowledgments
The project was supported by the Office of Rural Health Policy, Human Resources and Services Administration (grant 1 D1A RH 00005-01). This study was conducted under the auspices of The Healthy and Unhealthy Places in the United States Project at the Social Science Research Center, Mississippi State University.
Appreciation is expressed to Deborah D. Ingram, Office of Analysis and Epidemiology, for her fine leadership in administering the data use program for the Compressed Mortality File.
Human Participant Protection No institutional review board protocol approval was required for this study.
Peer Reviewed
Contributors A.G. Cosby conceptualized the study and in cooperation with T.T. Neaves developed the article. R.E. Cossman, J.S. Cossman, and D.M. Mirvis assisted with the literature review and interpretations of data. W.L. James was responsible for developing the age-adjusted mortality trends and excess deaths estimates. N. Feierabend was responsible for estimating life expectancies in metropolitan–nonmetropolitan counties. T. Farrigan advised on using Rural–Urban Continuum codes and the measurement for rurality over time. C. A. Jones provided overall critique of the research and helped define the research agenda for further study of the nonmetropolitan mortality penalty.
References
- 1.Haines MR. The urban mortality transition in the United States, 1800–1940. Ann Demogr Hist (Paris). 2001;101:33–64. [Google Scholar]
- 2.Ricketts TC III. Rural Health in the United States. New York, NY: Oxford University Press; 1999.
- 3.Eberhardt MS, Ingram DD, Makuc DM, et al. Health, United States, 2001 with Urban and Rural Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 2001. PHS 2001–1232.
- 4.Gamm LD, Hutchison LL, Dabney BJ, Dorsey AM. Rural Healthy People 2010: A Companion Document to Healthy People 2010. Vol. 1. College Station, TX: School of Rural Public Health, Texas A&M University System Health Science Center; 2003. Available at http://sp.srph.tamhsc.edu/centers/Moved_rhp2010/Volume1.pdf. Accessed July 17, 2007.
- 5.Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Dept of Health and Human Services; 2000. Available at http://www.healthypeople.gov/Document/tableofcontents.htm# under. Accessed July 17, 2007.
- 6.Preston S. Mortality trends. Ann Rev Sociol. 1977; 3:163–178. [Google Scholar]
- 7.Clifford WB, Brannon YS. Rural differentials in mortality. Rural Sociol. 1985;50:210–224. [Google Scholar]
- 8.Compressed Mortality File, 1968–1988 [machine readable data file and documentation, CD-ROM Series 20, No. 2A]. Hyattsville, MD: National Center for Health Statistics; 2000.
- 9.Compressed Mortality File, 1989–1998 [machine readable data file and documentation, CD-ROM Series 20, No. 2E]. Hyattsville, MD: National Center for Health Statistics; 2007.
- 10.Compressed Mortality File, 1999–2004 [machine readable data file and documentation, CD-ROM Series 20, No. 2J]. Hyattsville, MD: National Center for Health Statistics; 2007.
- 11.Measuring Rurality. Washington, DC: Economic Research Service, US Dept of Agriculture. Available at: http://www.ers.usda.gov/briefing/rurality. Accessed July 17, 2007.
- 12.Ingram DD, Franco S. 2006 NCHS Urban–Rural Classification Scheme for Counties. Hyattsville, MD: National Center for Health Statistics. Available at: http://wonder.cdc.gov/wonder/help/cmf/urbanization-methodology.html. Accessed July 17, 2007.
- 13.Murray C, Kulkarni S, Ezzati M. Eight Americas: new perspectives on US health disparities. AM J Prev Med. 2005;29:4–10. [DOI] [PubMed] [Google Scholar]
- 14.Murray C, Kulkarni S, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3:1513–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]