Abstract
Nonfermenting bacteria are ubiquitous environmental opportunists that cause infections in humans, especially compromised patients. Due to their limited biochemical reactivity and different morphotypes, misidentification by classical phenotypic means occurs frequently. Therefore, we evaluated the use of matrix-assisted laser desorption ionization-time-of-flight mass spectrometry (MALDI-TOF MS) for species identification. By using 248 nonfermenting culture collection strains composed of 37 genera most relevant to human infections, a reference database was established for MALDI-TOF MS-based species identification according to the manufacturer's recommendations for microflex measurement and MALDI BioTyper software (Bruker Daltonik GmbH, Leipzig, Germany), i.e., by using a mass range of 2,000 to 20,000 Da and a new pattern-matching algorithm. To evaluate the database, 80 blind-coded clinical nonfermenting bacterial strains were analyzed. As a reference method for species designation, partial 16S rRNA gene sequencing was applied. By 16S rRNA gene sequencing, 57 of the 80 isolates produced a unique species identification (≥99% sequence similarity); 11 further isolates gave ambiguous results at this threshold and were rated as identified to the genus level only. Ten isolates were identified to the genus level (≥97% similarity); and two isolates had similarity values below this threshold, were counted as not identified, and were excluded from further analysis. MALDI-TOF MS identified 67 of the 78 isolates (85.9%) included, in agreement with the results of the reference method; 9 were misidentified and 2 were unidentified. The identities of 10 randomly selected strains were 100% correct when three different mass spectrometers and four different cultivation media were used. Thus, MALDI-TOF MS-based species identification of nonfermenting bacteria provided accurate and reproducible results within 10 min without any substantial costs for consumables.
The genera Pseudomonas, Burkholderia, Stenotrophomonas, and others belong to the large group of nonfermenting bacteria that are unable to ferment sugars. Nonfermenting bacteria are ubiquitous environmental opportunists, and some species can cause severe infections, especially in immunocompromised patients (30). In the group of cystic fibrosis patients in particular, nonfermenting bacteria are the main causes of morbidity and mortality (18). Furthermore, the antibiotic resistance of some nonfermenting bacterial species often complicates therapy (25, 30). Accurate species identification is therefore critical not only because the prognosis for an infected patient differs significantly depending on the species identified (33) but also because in some cases, e.g., infections with Burkholderia cepacia genomovar III (5), strict infection control measures must be established for cystic fibrosis patients (5, 31).
In a routine clinical laboratory, species identification of cultured isolates usually relies on phenotypic methods, such as panels of biochemical reactions, antibiotic resistance, and fatty acid patterns (28). However, due to their limited biochemical reactivity and variable morphology, nonfermenters are frequently misidentified by classical methods (21, 26). Moreover, isolates from patients with chronic infections often loose their characteristic phenotypes (12, 26). To overcome these drawbacks, genotypic identification methods have become widely used, and most of them are based on the polymorphism of the 16S rRNA genes. Species-specific PCRs, restriction patterns, and more recently, partial DNA sequencing are used for species identification. Nowadays, sequencing of the 16S rRNA gene is accepted as the reference method for species identification, and several studies have shown its superiority to phenotypic methods for the identification of various groups of bacteria, including nonfermenting bacteria (2, 3, 8, 9, 14, 15, 27). However, a prerequisite for the retrieval of valid identification results is the use of an extensive and comprehensive quality-controlled database (6, 16).
Matrix-assisted laser desorption ionization-time-of-flight mass spectrometry (MALDI-TOF MS), which can be used to analyze the protein composition of a bacterial cell, has emerged as a new technology for species identification. By measuring the exact sizes of peptides and small proteins, which are assumed to be characteristic for each bacterial species, it is possible to determine the species within a few minutes when the analysis is started with whole cells, cell lysates, or crude bacterial extracts (13, 17, 22). However, due to difficulties with the reproducibility of results because of the use of different cultivation conditions and the limited availability of reference data sets, MALDI-TOF MS has not yet been widely used for species identification.
In this study, we therefore established a reference database for MALDI-TOF MS-based nonfermenter identification, analyzed the reproducibility using different cultivation conditions and mass spectrometer instruments, and evaluated the methodology with 80 blind-coded clinical nonfermenter strains that were analyzed by partial 16S rRNA gene sequencing, which was used as the reference method.
(This study was presented in part at the 47th Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL, 17 to 20 September 2007.)
MATERIALS AND METHODS
Bacterial strains.
To establish a reference database for MALDI-TOF MS-based species identification, 248 nonfermenter culture collection strains composed of 37 genera most relevant to human infections were used (Table 1).
TABLE 1.
Nonfermenter culture collection strains used to establish the reference database for MALDI-TOF MS-based species identification
| Genus | Straina |
|---|---|
| Achromobacter | Achromobacter denitrificans DSM 30026, A. insolitus LMG 6003, A. piechaudii DSM 10342, A. ruhlandii DSM 653, A. spanios LMG 5911, A. xylosoxidans subsp. xylosoxidans DSM 2402 |
| Acidovorax | Acidovorax avenae subsp. avenae DSM 7227, A. avenae subsp. citrulli LMG 5376, A. defluvii DSM 12644, A. delafieldii DSM 64, A. facilis DSM 649, A. konjaci DSM 7481, A. temperans DSM 7270 |
| Acinetobacter | Acinetobacter baumannii DSM 30007, A. baumannii LMG 994, A. baylyi DSM 14961, A. bouvetii DSM 14964, A. calcoaceticus DSM 30006, A. gerneri DSM 14967, A. grimontii DSM 14968, A. haemolyticus DSM 6962, A. haemolyticus LMG 1033, A. johnsonii DSM 6963, A. johnsonii LMG 10584, A. junii DSM 6964, A. lwoffii DSM 2403, A. lwoffii LMG 1138, A. lwoffii LMG 1154, A. lwoffii LMG 1300, A. parvus DSM 16617, A. radioresistens DSM 6976, A. radioresistens LMG 10614, A. schindleri DSM 16038, A. tandoii DSM 14970, A. tjernbergiae DSM 14971, A. towneri DSM 14962, A. ursingii DSM 16037 |
| Alcaligenes | Alcaligenes faecalis subsp. faecalis DSM 30030, A. faecalis subsp. parafaecalis DSM 13975 |
| Alishewanella | Alishewanella fetalis DSM 16032 |
| Arsenophonus | Arsenophonus nasoniae DSM 15247 |
| Arthrobacter | Arthrobacter monumenti DSM 16405 |
| Balneatrix | Balneatrix alpica CIP 103589 |
| Bergeyella | Bergeyella zoohelcum LMG 8351 |
| Blastomonas | Blastomonas natatoria DSM 3183, B. ursincola DSM 9006 |
| Brevundimonas | Brevundimonas aurantiaca DSM 4731, B. diminuta DSM 7234, B. intermedia DSM 4732, B. nasdae DSM 14572, B. subvibrioides DSM 4735, B. vesicularis DSM 7226 |
| Burkholderia | Burkholderia ambifaria LMG 11351, B. andropogonis DSM 9511, B. anthina LMG 16670, B. caledonica LMG 19076, B. caribensis DSM 13236, B. cenocepacia LMG 12614, B. cepacia DSM 7288, B. cepacia LMG 2161, B. dolosa DSM 16088, B. fungorum LMG 20227, B. gladioli DSM 4285, B. glathei DSM 50014, B. glumae DSM 9512, B. multivorans LMG 14293, B. phenazinium DSM 10684, B. phymatum LMG 21445, B. plantarii DSM 9509, B. pyrrocinia LMG 14191, B. sacchari LMG 19450, B. stabilis LMG 14294, B. terricola LMG 20594, B. thailandensis DSM 13276, B. tropica DSM 15359, B. tuberum LMG 21444, B. vietnamiensis LMG 10929, B. xenovorans LMG 21463 |
| Chryseobacterium | Chryseobacterium joostei LMG 18212, C. scophthalmum LMG 13028 |
| Comamonas | Comamonas aquatica LMG 2370, C. kerstersii DSM 16026, C. nitrativorans DSM 13191, C. terrigena DSM 7099, C. testosteroni DSM 50244 |
| Delftia | Delftia acidovorans DSM 39 |
| Elizabethkingia | Elizabethkingia meningoseptica DSM 2800, E. miricola DSM 14571 |
| Empedobacter | Empedobacter brevis LMG 4011 |
| Flavobacterium | Flavobacterium flevense DSM 1076, F. gelidilacus DSM 15343, F. hibernum DSM 12611, F. hydatis DSM 2063, F. johnsoniae DSM 2064, F. pectinovorum DSM 6368, F. resinovorum DSM 7478, F. saccharophilum DSM 1811 |
| Inquilinus | Inquilinus limosus DSM 16000 |
| Malikia | Malikia spinosa DSM 15801 |
| Microbulbifer | Microbulbifer elongatus DSM 6810 |
| Myroides | Myroides odoratimimus LMG 4029, M. odoratus DSM 2811 |
| Novosphingobium | Novosphingobium aromaticivorans DSM 12444, N. rosa DSM 7285, N. subarcticum DSM 10700, N. subterraneum DSM 12447 |
| Ochrobactrum | Ochrobactrum anthropi DSM 6882, O. gallinifaecis DSM 15295, O. grignonense DSM 13338, O. intermedium LMG 3301, O. tritici DSM 13340 |
| Pandoraea | Pandoraea apista LMG 16407, P. norimbergensis DSM 11628, P. pnomenusa LMG 18817, P. pulmonicola LMG 18106 |
| Pannonibacter | Pannonibacter phragmitetus LMG 5414, P. phragmitetus LMG 5430 |
| Pseudomonas | Pseudomonas abietaniphila CIP 106708, P. aeruginosa DSM 50071, P. agarici DSM 11810, P. alcaligenes DSM 50342, P. amygdali DSM 7298, P. anguilliseptica DSM 12111, P. antarctica DSM 15318, P. asplenii LMG 2137, P. aurantiaca CIP 106718, P. avellanae DSM 11809, P. azotoformans DSM 106744, P. balearica DSM 6083, P. beteli LMG 978, P. boreopolis LMG 979, P. brassicacearum DSM 13227, P. brenneri DSM 106646, P. caricapapayae LMG 2152, P. cedrina DSM 105541, P. chloritidismutans DSM 13592, P. chlororaphis DSM 50083, P. cichorii DSM 50259, P. citronellolis DSM 50332, P. congelans DSM 14939, P. corrugata DSM 7228, P. extremorietalis DSM 15824, P. flavescens DSM 12071, P. fluorescens DSM 50090, P. fragi DSM 3456, P. frederiksbergensis DSM 13022, P. fulva LMG 11722, P. fuscovaginae DSM 7231, P. geniculata LMG 2195, P. gessardii CIP 105469, P. graminis DSM 11363, P. grimontii DSM 106645, P. hibiscicola LMG 980, P. huttiensis DSM 10281, P. indica DSM 14015, P. jessenii CIP 105274, P. jinjuensis LMG 21316, P. kilonensis DSM 13647, P. koreensis LMG 21318, P. libanensis CIP 105460, P. lundensis DSM 6252, P. lutea LMG 21974, P. luteola DSM 6975, P. mandelii CIP 105273, P. marginalis DSM 13124, P. mendocina DSM 50017, P. mephitica CIP 106720, P. migulae CIP 105470, P. monteilii DSM 14164, P. mosselii CIP 105259, P. mucidolens LMG 2223, P. multiresinivorans LMG 20221, P. nitroreducens DSM 14399, P. oleovorans DSM 1045, P. orientalis CIP 105540, P. oryzihabitans DSM 6835, P. pertucinogena LMG 1874, P. pictorum LMG 981, P. plecoglossicida DSM 15088, P. poae DSM 14936, P. proteolytica DSM 15321, P. pseudoalcaligenes DSM 50188, P. putida DSM 291, P. putida DSM 50198, P. resinovorans LMG 2274, P. rhizosphaerae LMG 21640, P. rhodesiae DSM 14020, P. savastanoi LMG 2209, P. savastanoi subsp. savastanoi LMG 5011, P. straminea CIP 106745, P. stutzeri DSM 5190, P. synxantha LMG 2190, P. syringae DSM 6693, P. syringae subsp. syringae LMG 1247, P. taetrolens LMG 2336, P. thermotolerans DSMZ 14292, P. thivervalensis DSM 13194, P. tolaasii LMG 2342, P. trivialis DSM 14937, P. umsongensis LMG 21317, P. vancouverensis CIP 106707, P. veronii DSM 11331, P. viridiflava DSM 11124 |
| Ralstonia | Ralstonia eutropha DSMZ 531, R. mannitolilytica LMG 6866, R. pickettii DSM 6297, R. syzygii DSM 7385 |
| Rhizobium | Rhizobium radiobacter DSM 30147, R. rubi DSM 6772, R. tropici DSM 11418 |
| Shewanella | Shewanella algae DSMZ 9167, S. baltica DSM 9439, S. fidelis LMG 20552, S. frigidimarina DSM 12253, S. profunda DSM 15900, S. putrefaciens DSM 6067 |
| Sphingobacterium | Sphingobacterium faecium DSM 11690, S. mizutaii DSM 11724, S. multivorum DSM 11691, S. spiritivorum DSM 11722, S. thalpophilum DSM 11723 |
| Sphingobium | Sphingobium chlorophenolicum DSM 7098, S. herbicidovorans DSM 11019, S. xenophagum DSM 6383 |
| Sphingomonas | Sphingomonas adhaesiva DSM 7418, S. aerolata DSM 14746, S. aquatilis DSM 15581, S. aurantiaca DSM 14748, S. cloacae DSM 14926, S. faeni DSM 14747, S. koreensis DSM 15582, S. melonis DSM 14444, S. parapaucimobilis DSM 7463, S. paucimobilis DSM 1098, S. pituitosa DSM 13101, S. trueperi DSM 7225, S. wittichii DSM 6014, S. yabuuchiae DSM 14562 |
| Sphingopyxis | Sphingopyxis macrogoltabida DSM 8826, S. terrae DSM 8831 |
| Stenotrophomonas | Stenotrophomonas acidaminiphila DSM 13117, S.africana CIP 104854, S. maltophilia DSM 50170, S. nitritireducens DSM 12575, S. rhizophila DSM 14405 |
| Terrimonas | Terrimonas ferruginea DSM 30193 |
| Weeksella | Weeksella virosa LMG 12995 |
| Wolinella | Wolinella succinogenes DSM 1740 |
A total of 248 nonfermenter culture collection strains were used. Abbreviations: CIP, Collection de l'Institut Pasteur, Paris, France; DSM, Deutsche Sammlung von Mikroorganismen und Zellkulturen, Braunschweig, Germany; LMG, culture collection of the Laboratorium voor Microbiologie, Universiteit Ghent, Ghent, Belgium.
The 80 clinical nonfermenting strains that were used to evaluate the MALDI-TOF MS reference database were recovered from clinical specimens received by the Cleveland Clinic Foundation (Cleveland, OH), the University of Texas Medical Branch (Galveston, TX), Cook Children's Medical Center (Fort Worth, TX), and the University of Nebraska Medical Center (Omaha, NE) during the 2004 calendar year.
16S rRNA gene sequencing and sequence analysis.
DNA isolation, amplification, and cycle sequencing of the clinical isolates were performed at the ARUP Institute for Clinical and Experimental Pathology (Salt Lake City, UT). DNA was extracted as described previously (27). Four microliters of the extract was used in each PCR. PCR was performed in a total volume of 40 μl containing 1× FastStart DNA Master Plus SYBR green (Roche Diagnostics Corp., Indianapolis, IN), 500 nM each primer 16S-27f and 16S-519r (27), and 4 mM Mg2+. The thermal cycling reactions were performed with a RotorGene 3000 real-time PCR instrument (Corbett Research, Sydney, Australia) and consisted of an initial denaturation (10 min at 95°C), followed by 35 cycles of denaturation (30 s at 95°C), annealing (20 s at 55°C), and extension (30 s at 72°C) and then a single final extension (2 min at 72°C). Negative controls, which contained water instead of template DNA, were run in parallel in each run. The PCR product was purified by an enzymatic method, modified from the method of Dugan et al. (11), with exonuclease I (New England Biolabs GmbH, Frankfurt-Hoechst, Germany) and shrimp alkaline phosphatase (Amersham Pharmacia Biotech, Freiburg, Germany). Briefly, 5 μl of the PCR product was incubated with 1 U of each enzyme at 37°C for 30 min. The enzymes were then inactivated at 80°C for 15 min, and the PCR products were stored at 4°C. The amplicons were sequenced with an ABI Prism BigDye Terminator (version 3.0) ready reaction cycle sequencing kit (Applied Biosystems, Foster City, CA). The sequencing reaction required 0.5 μl of premix from the kit, 1.8 μl Tris-HCl-MgCl2 buffer (400 mM Tris-HCl, 10 mM MgCl2), 10 pmol of the sequencing primers (which were the same as the PCR primers), and 2 μl of the cleaned PCR product in a total volume of 10 μl.
For the sequencing chemistry mixtures, the same primer used for PCR (primer 16S-27f or 16S-519r) was used to obtain forward and reverse sequence data for partial 5′ 16S rRNA gene sequencing. All sequencing reactions were performed with a standard thermocycler to complete 25 cycles of denaturation (10 s at 96°C), annealing (5 s at 53°C), and extension (4 min at 60°C). The sequencing products were purified with Centri-Sep spin columns (Princeton Separations, Adelphia, NJ), followed by preparation for analysis on an ABI Prism 310 or a 3100 Avant genetic analyzer, in accordance with the instructions of the manufacturer (Applied Biosystems). The double-stranded sequences corresponding to Escherichia coli 16S rRNA gene positions 54 to 510 were analyzed in accordance with the procedure described for the Ribosomal Differentiation of Medical Micro-Organisms (RIDOM) database (16).
Sample preparation for MALDI-TOF MS, spectrum generation, and data analysis.
A colony of a fresh overnight culture was used for sample preparation before measurement. The material was thoroughly suspended in 300 μl double-distilled water, 900 μl ethanol was added, and the components were mixed well. Prior to shipment to the place of measurement, the samples in ethanol-water were centrifuged, the supernatant was removed, and the pellets were dried. For sample extraction, 50 μl of formic acid (70% in water) was added to the bacterial pellet, the components were mixed thoroughly, and 50 μl of acetonitrile was added. After centrifugation at 13,000 × g for 2 min, 1 μl of the supernatant containing the bacterial extract was transferred to a sample position on a ground steel MALDI target plate and allowed to dry at room temperature. Subsequently, the sample was overlaid with 2 μl of MALDI matrix (a saturated solution of α-cyano-4-hydroxy-cinnamic acid in 50% acetonitrile-2.5% trifluoroacetic acid) and dried again.
For database construction and validation, measurements were performed with a microflex LT (Bruker Daltonik GmbH, Leipzig, Germany) bench-top mass spectrometer equipped with a 20-Hz nitrogen laser (parameter settings: ion source 1 (IS1), 20 kV; IS2, 18.5 kV; lens, 8.5 kV; detector gain, 2,650 V; and gating, none). Spectra were recorded in the positive linear mode for the mass range of 2,000 to 20,000 Da at the maximum laser frequency. The database references (main spectra) for the newly investigated bacteria were constructed by using the automated functionality of the MALDI BioTyper (version 1.1) software package (Bruker Daltonik GmbH). Briefly, for each database entry, 20 individually measured mass spectra were imported into the software. After smoothing of the spectra, baseline correction, and peak picking, the resulting peak lists were used by the program to calculate and to store a main spectrum containing the average peak mass, average peak intensity, and frequency information.
For microorganism identification, the raw spectra of the unknown bacteria were imported into the MALDI BioTyper software and analyzed by standard pattern matching (with default parameter settings) against the main spectra of 2,506 microorganisms, used as reference data, in the BioTyper database (these spectra are an integrated part of the BioTyper software). The reference database consisted of the 248 newly created main spectra for the nonfermenting bacteria investigated and other clinical, veterinary, and environmental bacterial strains. Preparation of samples of the 248 nonfermenter reference strains was performed at the Institute for Hygiene, University Hospital Muenster (Muenster, Germany). The clinical nonfermenting strains being evaluated were prepared at the ARUP Institute for Clinical and Experimental Pathology.
Preparation of the ground steel plate, MS of 96 samples, and a search of the database for similarity for species identification took about 3 h with the microflex instrument. A single sample could be identified in approximately 10 min.
MALDI-TOF MS reproducibility testing.
Complementary to the already determined intraspecies (4, 36) and interlaboratory (37) reproducibilities of MALDI-TOF MS-based species identification, the spectra of 10 randomly chosen nonfermenter strains (Brevundimonas aurantiaca DSM 4731, Brevundimonas intermedia DSM 4732, Brevundimonas andropogonis DSM 9511, Brevundimonas caribensis DSM 13236, Flavobacterium johnsoniae DSM 2064, Flavobacterium mizutaii DSM 11724, Pseudomonas aeruginosa DSM 50071, Pseudomonas beteli LMG 978, Pseudomonas boreopolis LMG 979, Pseudomonas extremorietalis DSM 15824) were determined under different conditions. First, the testing was done by parallel measurement on three different MALDI-TOF MS instruments (the microflex LT instrument, the autoflex II TOF/TOF instrument with a 50-Hz nitrogen laser, and the ultraflex III TOF/TOF instrument with a 200-Hz smart-beam laser, all from Bruker Daltonik GmbH) to test the comparabilities of the results obtained with the different instruments. The parameter settings for the additional instruments were as follows: IS1, 20 kV; IS2, 18.7 kV; lens, 8.0 kV; detector gain, 1,756 V; and gating, maximum, 1,500 Da, for the autoflex instrument and IS1, 25 kV; IS2, 23.45 kV; lens, 6.0 kV; detector gain, 1,650 V; and gating, maximum, 1,500 Da, for the ultraflex instrument. Second, the influence of different cultivation conditions was characterized by cultivation of the 10 strains on four different media (Columbia blood agar, chocolate agar, Mueller-Hinton agar, and tryptic soy agar; Heipha, Eppelheim, Germany) at 30°C under aerobic conditions for 48 h. Finally, the influence of the age of the bacterial cultures was investigated by analyzing three strains (B. aurantiaca DSM 4731, B. caribensis DSM 13236, P. aeruginosa DSM 50071) that were cultivated for 48 h at 30°C on Columbia blood agar and subsequently stored for 2, 5, and 7 days at room temperature. All samples for reproducibility testing were blind coded for MALDI-TOF MS analysis.
Evaluation of MALDI-TOF MS-based species identification by use of clinical isolates.
To evaluate the MALDI-TOF MS reference database, 80 blind-coded clinical nonfermenters were analyzed. As the reference method for species designation, partial 16S rRNA gene sequencing was used. The reference partial 16S rRNA gene sequence database (E. coli 16S rRNA gene positions 54 to 510) included all 248 nonfermenter culture collection strains used as a reference for MALDI-TOF MS (Table 1). Sequence data were stored and analyzed by using the RIDOM framework (27). Sequence similarity of ≥99% was used for identification to the species level, and sequence similarity of ≥97% was used for identification to the genus level (3). Further differentiation to the species level was made between unique and ambiguous similarity search results (multiple top-scoring results); the latter were rated as identification to the genus level only. Sequence similarities below 97% were rated as not identifiable. MALDI-TOF MS results based on the log(score) values calculated by the BioTyper software were compared to the 16S rRNA gene sequence similarity search results. BioTyper software requires log(score) values of ≥2.0 for identification to the species level and values of between <2 and ≥1.7 for identification to the genus level. Results based on log(score) values of <1.7 were rated as not identifiable by the software. These BioTyper thresholds were empirically determined on the basis of information in an in-house database with data for more than 2,800 bacterial strains that were either culture collection strains or well-characterized clinical strains.
To determine the discriminatory ability of 16S rRNA gene sequencing and MALDI-TOF MS within certain groups of strains, the pairwise distances were calculated and displayed in a tree created by the unweighted pair group method with arithmetic averaging by using MEGA software (version 4.0) (37).
RESULTS
The cell extracts from all 248 culture collection strains, which represented the majority of all clinically relevant nonfermenter species, gave sufficient spectra and were included in the MALDI-TOF MS reference database (database version 1.0).
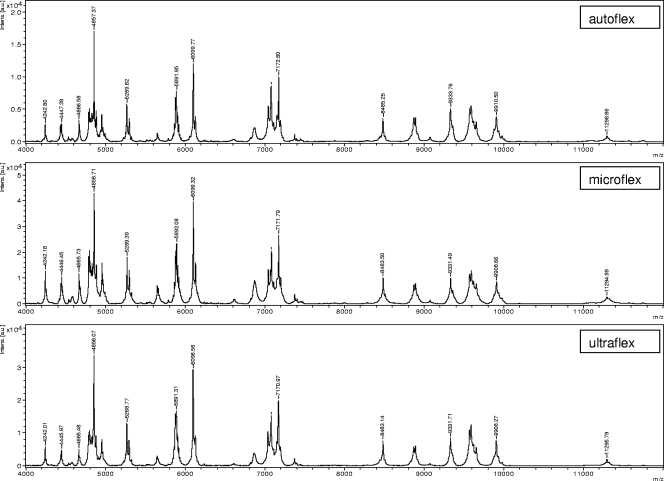
To investigate the reproducibility of the spectra generated with different mass spectrometers, 10 culture collection strains were randomly chosen to be analyzed with three different mass spectrometers. For all 10 strains, the log(score) results gave the same species identification result irrespective of the mass spectrometer used, with all log(score) values being above 2.0. Figure 1 shows representative results for strain Galv12 measured with the three different spectrometers. To determine the influence of different cultivation media on the quality of the spectra, the 10 cultured strains were also analyzed after cultivation on four different media. Furthermore, three strains were analyzed after up to 7 days storage on Columbia blood agar at room temperature. In all cases, MS resulted in identical, correct identification results relative to those in the reference database.
FIG. 1.
Comparison of mass spectra for one exemplary nonfermenting strain (strain Galv12) generated on three different MALDI-TOF MS instruments (autoflex, microflex, ultraflex). Exemplary masses (in daltons) are depicted. Intens. [a.u.], intensity (in arbitrary units).
All 80 nonfermenting strains from the clinical specimens gave spectra sufficient for species identification. In parallel with MALDI-TOF MS identification, all strains were analyzed by partial 16S rRNA gene sequencing, which was used as the reference method. By sequence comparison analysis, 57 isolates were unambiguously identified to the species level (≥99% sequence similarity) and 10 isolates were unambiguously identified to the genus level (≥97% sequence similarity) by partial 16S rRNA gene sequencing and a search for sequence similarity against the sequences in the RIDOM database. Eleven isolates (isolates W35, W12, NF18, W29, W23, W26, W14, W10, W06, Galv17, and Galv23) gave multiple species as results, and these were therefore treated as identified to the genus level only. The remaining two isolates (isolates NF08 and Neb38) had results below the sequence threshold of 97% similarity and were therefore excluded from further analysis.
The identification results obtained by MALDI-TOF MS and 16S rRNA gene sequencing, used as the reference method, are shown in Table 2, together with the achievable levels of identification. In total, MALDI-TOF MS identified 67 of the 78 isolates (85.9%), concordant with the sequencing results; of these, 47 of 57 (82.5%) were identified to the species level [log(score), ≥2.0] and 20 of 21 (95.2%) were identified to the genus level [log(score), between <2.0 and ≥1.7] (Table 3). Of the remaining 11 isolates, 4 isolates (isolates Neb14, Neb20, W15, and W18) had log(score) values of ≥2.0 and were correctly identified to the genus level but had discordant species designations in comparison to the results of the reference method. For four isolates (isolates W03, W08, W22, and W28), the correct genus was determined by the MALDI BioTyper software, with log(score) values of between 1.7 and 2.0, whereas 16S rRNA gene sequencing gave a species identification. For isolate NF18, the genus determination result was discordant with the 16S rRNA gene sequencing result. Finally, the two isolates with log(score) values of <1.7 (isolates Neb37 and W16) were rated as nonidentifiable by MALDI-TOF MS (Table 3).
TABLE 2.
Identification results for the 80 clinical nonfermenter isolates obtained by MALDI-TOF MS in comparison to those obtained by partial 16S rRNA gene sequence-based species identificationa
| Level of ID and isolate | 16S rRNA gene sequencingb
|
MALDI-TOF MS
|
||
|---|---|---|---|---|
| Species ID | Level of IDc | Species ID | Log(score)d | |
| Concordance | ||||
| Galv01 | S. maltophilia | Species | S. maltophilia | 2.481 |
| Galv02 | P. aeruginosa | Species | P. aeruginosa | 2.418 |
| Galv03 | P. aeruginosa | Species | P. aeruginosa | 2.505 |
| Galv04 | P. aeruginosa | Species | P. aeruginosa | 2.477 |
| Galv05 | P. aeruginosa | Species | P. aeruginosa | 2.565 |
| Galv07 | Achromobacter xylosoxidans subsp. xylosoxidans | Species | Achromobacter xylosoxidans | 2.415 |
| Galv08 | P. aeruginosa | Species | P. aeruginosa | 2.445 |
| Galv10 | P. oleovorans | Species | P. oleovorans | 2.188 |
| Galv12 | S. maltophilia | Species | S. maltophilia | 2.364 |
| Galv14 | S. maltophilia | Species | S. maltophilia | 2.422 |
| Galv20 | S. maltophilia | Species | S. maltophilia | 2.516 |
| Galv24 | S. maltophilia | Species | S. maltophilia | 2.438 |
| Galv25 | S. maltophilia | Species | S. maltophilia | 2.335 |
| Neb06 | P. aeruginosa | Species | P. aeruginosa | 2.502 |
| Neb07 | P. aeruginosa | Species | P. aeruginosa | 2.510 |
| Neb15 | P. aeruginosa | Species | P. aeruginosa | 2.434 |
| Neb16 | P. aeruginosa | Species | P. aeruginosa | 2.516 |
| Neb17 | S. maltophilia | Species | S. maltophilia | 2.328 |
| Neb22 | S. maltophilia | Species | S. maltophilia | 2.501 |
| Neb23 | P. aeruginosa | Species | P. aeruginosa | 2.456 |
| Neb27 | S. maltophilia | Species | S. maltophilia | 2.494 |
| Neb32 | S. maltophilia | Species | S. maltophilia | 2.418 |
| Neb33 | Alcaligenes faecalis subsp. faecalis | Species | Alcaligenes faecalis subsp. faecalis | 2.299 |
| Neb34 | Alcaligenes faecalis subsp. faecalis | Species | Alcaligenes faecalis subsp. faecalis | 2.373 |
| Neb40 | Achromobacter xylosoxidans subsp. xylosoxidans | Species | Achromobacter xylosoxidans | 2.328 |
| NF02 | S. maltophilia | Species | S. maltophilia | 2.489 |
| NF03 | P. aeruginosa | Species | P. aeruginosa | 2.587 |
| NF05 | S. maltophilia | Species | S. maltophilia | 2.529 |
| NF07 | P. aeruginosa | Species | P. aeruginosa | 2.318 |
| NF09 | P. aeruginosa | Species | P. aeruginosa | 2.444 |
| NF11 | S. maltophilia | Species | S. maltophilia | 2.296 |
| NF16 | P. aeruginosa | Species | P. aeruginosa | 2.545 |
| NF17 | P. aeruginosa | Species | P. aeruginosa | 2.524 |
| NF19 | S. maltophilia | Species | S. maltophilia | 2.519 |
| NF21 | S. maltophilia | Species | S. maltophilia | 2.386 |
| NF23 | S. maltophilia | Species | S. maltophilia | 2.450 |
| NF24 | Alcaligenes faecalis subsp. faecalis | Species | Alcaligenes faecalis subsp. faecalis | 2.417 |
| W01 | P. koreensis | Species | P. koreensis | 2.300 |
| W05 | P. stutzeri | Species | P. stutzeri | 2.198 |
| W07 | P. putida | Species | P. putida | 2.014 |
| W09 | P. stutzeri | Species | P. stutzeri | 2.460 |
| W11 | P. stutzeri | Species | P. stutzeri | 2.372 |
| W13 | Delftia acidovorans | Species | Delftia acidovorans | 2.253 |
| W17 | P. aeruginosa | Species | P. aeruginosa | 2.613 |
| W19 | P. citronellolis | Species | P. citronellolis | 2.434 |
| W20 | Brevundimonas diminuta | Species | Brevundimonas diminuta | 2.292 |
| W30 | P. fulva | Species | P. fulva | 2.024 |
| Galv13 | Pseudomonas spp. | Genus | P. savastanoi | 1.782 |
| Galv19 | Stenotrophomonas spp. | Genus | S. maltophilia | 2.303 |
| Galv21 | Pseudomonas spp. | Genus | P. monteilii | 2.034 |
| Galv22 | Stenotrophomonas spp. | Genus | S. maltophilia | 2.350 |
| Neb26 | Pseudomonas spp. | Genus | P. savastanoi | 1.797 |
| Neb28 | Stenotrophomonas spp. | Genus | S. maltophilia | 1.792 |
| Neb36 | Pseudomonas spp. | Genus | P. putida | 2.149 |
| NF04 | Pseudomonas spp. | Genus | P. putida | 1.832 |
| NF10 | Pseudomonas spp. | Genus | P. putida | 1.852 |
| W02 | Pseudomonas spp. | Genus | P. putida | 2.446 |
| W35 | B. cepacia complex | B. cepacia complex | B. multivorans | 2.379 |
| W12 | P. synxantha/P. mucidolens/ P. libanesis/P. gessardii | Four different species possible | P. tolaasii | 2.148 |
| Galv17 | P. monteilii/P. putida | Two different species possible | P. putida | 2.477 |
| Galv23 | P. psychrotolerans/P. oryzohabitans | Two different species possible | P. oryzihabitans | 1.704 |
| W06 | P. monteilii/P. putida | Two different species possible | P. putida | 2.127 |
| W10 | P. monteilii/P. putida | Two different species possible | P. monteilii | 2.011 |
| W14 | P. monteilii/P. putida | Two different species possible | P. monteilii | 1.941 |
| W23 | P. monteilii/P. putida | Two different species possible | P. putida | 2.048 |
| W26 | Achromobacter xylosoxidans subsp. xylosoxidans/A. ruhlandii | Two different species possible | Achromobacter ruhlandii | 2.395 |
| W29 | P. monteilii/putida | Two different species possible | P. putida | 2.124 |
| Discrepant | ||||
| Neb14 | Elizabethkingia meningoseptica | Species | Elizabethkingia miricola | 2.159 |
| Neb20 | Sphingomonas sanguinis | Species | Sphingomonas paucimobilis | 2.182 |
| W03 | P. plecoglossicida | Species | P. putida | 1.873 |
| W08 | Achromobacter spanius | Species | Achromobacter denitrificans | 1.845 |
| W15 | P. putida | Species | P. fluorescens | 2.142 |
| W18 | Achromobacter xylosoxidans subsp. xylosoxidans | Species | Achromobacter ruhlandii | 2.333 |
| W22 | P. plecoglossicida | Species | P. putida | 1.770 |
| W28 | P. plecoglossicida | Species | P. putida | 1.854 |
| Neb37 | Chryseobacterium indologenes | Species | No ID | 1.547 |
| W16 | Ralstonia insidiosa | Species | No ID | 1.678 |
| NF18 | Brevundimonas nasdae/B. intermedia/B. vesicularis | Three different species possible | Arthrobacter castelli | 1.800 |
| None | ||||
| Neb38 | No ID | No ID possible | Acinetobacter sp. strain DSM 30009 | 2.283 |
| NF08 | No ID | No ID possible | Acinetobacter sp. strain DSM 30009 | 1.922 |
Abbreviations: S., Stenotrophomonas; P., Pseudomonas; B., Burkholderia; subsp., subspecies; spp., species; DSM, Deutsche Sammlung von Mikroorganismen und Zellkulturen, Braunschweig, Germany; ID, identification.
Sequences were compared by the RIDOM procedure (16).
The achievable level of identification derived from 16S rRNA gene sequencing as the reference method is given. Sequence similarities of ≥99% were used for identification to the species level, and sequence similarities of ≥97% were used for identification to the genus level. A further differentiation to the species level was made between sequences with unique and ambiguous similarity search results (multiple top-scoring results); the latter were rated as identification to the genus level only. Sequence similarities below 97% were rated as not identifiable and the numbers of different species possible are given.
Log(score) values of ≥2.0 were required for the identification to the species level, and values of ≥1.7 were required for identification to the genus level. Log(score) values below 1.7 were rated as not identifiable.
TABLE 3.
Aggregated identification results for 78 clinical nonfermenter isolates obtained by MALDI-TOF MS in comparison to those obtained by partial 16S rRNA gene sequencing as the reference method
| Level of identification (no. of isolates) by 16S rRNA gene | No. (%) of isolates with the following MALDI-TOF MS IDa:
|
||
|---|---|---|---|
| Concordance | Discrepant | None | |
| Species (57) | 47 (82.5) | 8 (14.0) | 2 (3.5) |
| Genus (21) | 20 (95.2) | 1 (4.8) | |
| Total (78) | 67 (85.9) | 9 (11.5) | 2 (2.6) |
The MALDI-TOF MS identification (ID) was based on the resulting log(score) values after a similarity search against the MALDI-TOF MS reference database. Log(score) values of ≥2.0 were required for identification to the species level, and values of ≥1.7 were required for identification to the genus level. Log(score) values of <1.7 were rated as not identifiable.
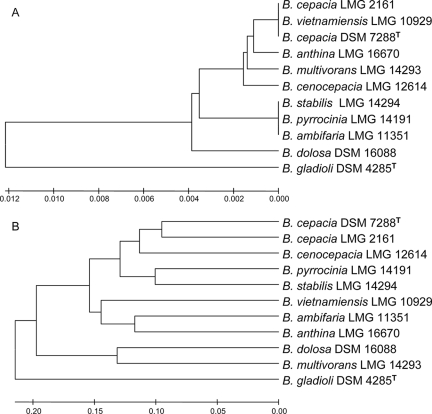
To investigate the discriminatory ability of closely related species by MALDI-TOF MS in comparison to that by 16S rRNA gene sequencing, nine species of the former Burkholderia cepacia complex were investigated in detail. By partial 16S rRNA gene sequencing, three strains, B. cepacia DSM 7288 (B. cepacia type strain), B. cepacia LMG 2161 (the former reference strain for B. cepacia complex genomovar I), and Burkholderia vietnamiensis LMG 10929 (formerly genomovar V), were indistinguishable (Fig. 2A). Likewise, three other strains, Burkholderia stabilis LMG 14294 (formerly genomovar IV), Burkholderia pyrrocinia LMG 14191 (formerly genomovar IX), and Burkholderia ambifaria LMG 11351 (formerly genomovar VII), were also indistinguishable. In contrast, MALDI-TOF MS was able to differentiate among all species of the former B. cepacia complex (Fig. 2B).
FIG. 2.
Comparison of discriminatory abilities of partial 16S rRNA gene sequencing and MALDI-TOF MS for strains within the former Burkholderia cepacia complex. Nine reference strains of the former B. cepacia complex, a B. cepacia type strain (DSM 7288), and Burkholderia gladioli DSM 4285 (which was used as the outgroup) are shown on a rooted tree created by the unweighted pair group method with arithmetic averaging. MEGA software (version 4.0) was used for tree construction (34). (A) Tree based on partial 16S rRNA gene sequences (453 bp, E. coli gene positions 54 to 510). The sequence distances are given as the percent difference. (B) Tree based on the MALDI-TOF MS results. The log(score)-derived distances are given in percent. Abbreviations: LMG, culture collection of the Laboratorium voor Microbiologie, Universiteit Ghent, Ghent, Belgium; DSM, Deutsche Sammlung von Mikroorganismen und Zellkulturen, Braunschweig, Germany.
DISCUSSION
The correct species identification of nonfermenting bacteria from clinical specimens and from samples from the patient's environment is of major importance for optimal patient management and the establishment of effective infection control measures. To overcome the problems related to classical phenotypic species identification methods, this study evaluated the capability of MALDI-TOF MS to identify these species. As a reference method for comparison, partial 16S rRNA gene sequencing was chosen. This method has been shown to be a reliable and universal technique for species identification in clinical microbiology (6, 35). A reference database of MALDI-TOF MS spectra comprising well-characterized culture collection strains only was established and evaluated by using blind-coded nonfermenter isolates from clinical specimens (Table 2). With 82.5% isolates correctly identified to the species level and 95.2% isolates correctly identified to the genus level (Table 3), the results of MALDI-TOF MS-based identification showed a high concordance to those of the reference method. In contrast, the use of two current phenotypic identification methods (the API 20NE and Vitek 2 systems) resulted in correct identification rates of only 61% and 54%, respectively, in a different study with nonfermenters (3).
The identification of species belonging to the former B. cepacia complex, which was reclassified on the basis of recA polymorphisms due to variations within the rRNA operon that are too small (10, 23), is especially problematic and has often led to misidentifications in the past (21, 26). In this study, one clinical strain (strain W35) was identified as a member of the former B. cepacia complex. Since the reference method (16S rRNA gene sequencing) was shown to be unable to differentiate among strains of the former B. cepacia complex (Fig. 2A), identification was achieved only to the level of the B. cepacia complex. However, MALDI-TOF MS identified this strain as Burkholderia multivorans with a high log(score) of 2.379, showing the possible ability of this method to differentiate the species within this complex. Due to the clinical relevance of these species, a detailed MALDI-TOF MS analysis of the former B. cepacia complex reference strains was performed (Fig. 2B). This analysis corroborated the higher discriminatory ability of MALDI-TOF MS in comparison to that of 16S rRNA gene sequencing (36) and enabled the valid identification of all members of the former B. cepacia complex.
The proof of principle of the utilization of MALDI-TOF MS for bacterial species determination was already shown a decade ago (7, 17, 22). However, MALDI-TOF MS has not been widely used in clinical microbiology due to difficulties with the reproducibility of the results with different MALDI-TOF mass spectrometer instruments and with variations in cultivation conditions and the limited availability of reference data sets. To address these challenges, we analyzed the spectra generated by our method from 10 randomly chosen strains with three different mass spectrometers and four different cultivation media. Furthermore, the influence of the storage of cultures at room temperature before processing for MALDI-TOF MS was also investigated. Under all conditions with a defined culture set, the spectra showed high degrees of uniformity (Fig. 1), and a search of a reference database gave the correct identification, with log(score) values of ≥2.0 for all samples tested. We conclude that by using the established MALDI BioTyper database, the reproducibility is high and independent of the mass spectrometer instrument used and the conditions tested.
In contrast to earlier work (7), which applied a mass range of 550 to 2,200 Da, a range of 2,000 to 20,000 Da was used in this study. This mass range represents predominantly ribosomal proteins obtained from whole bacteria or crude bacterial extracts (24, 32). These proteins are abundant in the cell and are positively charged, which favors their measurement by MALDI-TOF MS and which results in a relative robustness under different culture conditions. Another reason for the improved reproducibility is the use of a dedicated algorithm of MALDI BioTyper software based on pattern comparisons. Different approaches for bacterial identification based on MADLI-TOF MS fingerprint spectra have been described (1, 19, 20, 29). The MALDI BioTyper software applies pattern matching to compare unknown mass spectra with reference data stored in a database. In the first step, the software extracts a list of the mass spectrum peaks after smoothing and baseline subtraction. This list of peaks is compared with each entry in the reference database, and thereby, the unknown peak in the list is aligned with each main spectrum by a dedicated recalibration algorithm. Therefore, even suboptimal mass accuracies of measurements are sufficient for a successful analysis. In addition, the correlation of intensities of matching peaks is determined. On the basis of the peak matches and intensity correlations, a score and the logarithm of this score are calculated, with values from 0 to 3 indicating 0 to 100% pattern matches, respectively. After comparison of an unknown spectrum with all main spectra in the database, all log(score) values are ranked. Finally, MALDI-TOF MS-based species identification was hampered in the past due to the lack of a comprehensive reference database built with data for well-characterized strains, e.g., culture collection strains, which is a prerequisite to reflect at least partially the natural diversity of bacteria. In this study, a database of spectra for 248 reference nonfermenting bacteria was initially established and subsequently evaluated by using blind-coded clinical isolates.
One advantage to the current study is that the same reference strains were used both in the 16S rRNA gene database and in the MALDI-TOF MS database. Comparison of databases with different strains would have prevented an accurate comparison between the methods. One limitation of the present study is the exclusive use of 16S rRNA gene sequencing as the reference method of identification. This method was not able to identify all clinical isolates to the species level (≥99% sequence similarity). Ideally, a polyphasic approach to identification, with the combined use of phenotypic and genotypic characteristics, should be considered. However, due to the diversity among the species of nonfermenting bacteria and the current changes in bacterial nomenclature within this group, there is no clearly defined strategy for the identification of nonfermenting bacteria. Moreover, 16S rRNA gene sequencing has already been found to be superior to phenotypic identification techniques for nonfermenting bacteria (3, 14). It is noteworthy that for 12 of the 21 isolates identified to the genus level only by 16S rRNA gene sequencing in this study, MALDI-TOF MS gave species results [with log(score) values of ≥2.0]. Although it is difficult to prove, MALDI-TOF MS most likely outperformed the reference method in these cases.
For nonfermenting bacteria, the MALDI-TOF MS method achieved a high degree of reproducibility of measurements in a mass range that included characteristic signals, which are little influenced by culture conditions. In addition, a new algorithm for pattern matching was developed, and a high-quality reference database was created. The more stringent control of cultivation conditions might, however, be necessary for other bacterial strains that accumulate storage products (36), sporulate (e.g., for Bacillus species), or show autolysis during long-time storage (e.g., Streptococcus species).
In summary, a MALDI-TOF MS method that provided accurate and fast species identification of nonfermenting bacteria and that can be used for routine detection was described. These results also showed that MALDI-TOF MS is more accurate than partial 16S rRNA gene sequencing for species identification of members of the B. cepacia complex. Further expansion of the MALDI-TOF MS database with other bacterial groups of clinical importance will help enhance the utility of this methodology for the identification of unknown bacterial pathogens. In the future, a polyphasic approach with the combined use of 16S rRNA gene sequencing and MALDI-TOF MS (with its higher discriminatory ability) might be an attractive alternative for the identification of those bacterial species that are hard to identify.
Acknowledgments
The work was partially funded by a grant from the Sächsische Aufbaubank (SAB10634) and by the ARUP Institute for Clinical and Experimental Pathology.
M. Kostrzewa and T. Maier have declared potential conflicts of interest. They are both employees of Bruker Daltonik GmhH, the company that produces the MALDI-TOF MS instruments and the software mentioned in the report. All other authors have declared that no competing interests exist.
Footnotes
Published ahead of print on 9 April 2008.
REFERENCES
- 1.Arnold, R. J., and J. P. Reilly. 1998. Fingerprint matching of E. coli strains with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry of whole cells using a modified correlation approach. Rapid Commun. Mass Spectrom. 12630-636. [DOI] [PubMed] [Google Scholar]
- 2.Becker, K., D. Harmsen, A. Mellmann, C. Meier, P. Schumann, G. Peters, and C. von Eiff. 2004. Development and evaluation of a quality-controlled ribosomal sequence database for 16S ribosomal DNA-based identification of Staphylococcus species. J. Clin. Microbiol. 424988-4995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosshard, P. P., R. Zbinden, S. Abels, B. Böddinghaus, M. Altwegg, and E. C. Böttger. 2006. 16S rRNA gene sequencing versus the API 20 NE system and the VITEK 2 ID-GNB card for identification of nonfermenting gram-negative bacteria in the clinical laboratory. J. Clin. Microbiol. 441359-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bright, J. J., M. A. Claydon, M. Soufian, and D. B. Gordon. 2002. Rapid typing of bacteria using matrix-assisted laser desorption ionisation time-of-flight mass spectrometry and pattern recognition software. J. Microbiol. Methods 48127-138. [DOI] [PubMed] [Google Scholar]
- 5.Chen, J. S., K. A. Witzmann, T. Spilker, R. J. Fink, and J. J. LiPuma. 2001. Endemicity and inter-city spread of Burkholderia cepacia genomovar III in cystic fibrosis. J. Pediatr. 139643-649. [DOI] [PubMed] [Google Scholar]
- 6.Clarridge, J. E. 2004. Impact of 16S rRNA gene sequence analysis for identification of bacteria on clinical microbiology and infectious diseases. Clin. Microbiol. Rev. 17840-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Claydon, M. A., S. N. Davey, V. Edwards-Jones, and D. B. Gordon. 1996. The rapid identification of intact microorganisms using mass spectrometry. Nat. Biotechnol. 141584-1586. [DOI] [PubMed] [Google Scholar]
- 8.Cloud, J. L., P. S. Conville, A. Croft, D. Harmsen, F. G. Witebsky, and K. C. Carroll. 2004. Evaluation of partial 16S ribosomal DNA sequencing for identification of Nocardia species by using the MicroSeq 500 system with an expanded database. J. Clin. Microbiol. 42578-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cloud, J. L., H. Neal, R. Rosenberry, C. Y. Turenne, M. Jama, D. R. Hillyard, and K. C. Carroll. 2002. Identification of Mycobacterium spp. by using a commercial 16S ribosomal DNA sequencing kit and additional sequencing libraries. J. Clin. Microbiol. 40400-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coenye, T., P. Vandamme, J. R. Govan, and J. J. LiPuma. 2001. Taxonomy and identification of the Burkholderia cepacia complex. J. Clin. Microbiol. 393427-3436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dugan, K. A., H. S. Lawrence, D. R. Hares, C. L. Fisher, and B. Budowle. 2002. An improved method for post-PCR purification for mtDNA sequence analysis. J. Forensic Sci. 47811-818. [PubMed] [Google Scholar]
- 12.Fegan, M., P. Francis, A. C. Hayward, G. H. Davis, and J. A. Fuerst. 1990. Phenotypic conversion of Pseudomonas aeruginosa in cystic fibrosis. J. Clin. Microbiol. 281143-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fenselau, C., and P. A. Demirev. 2001. Characterization of intact microorganisms by MALDI mass spectrometry. Mass Spectrom. Rev. 20157-171. [DOI] [PubMed] [Google Scholar]
- 14.Ferroni, A., I. Sermet-Gaudelus, E. Abachin, G. Quesne, G. Lenoir, P. Berche, and J. Gaillard. 2002. Use of 16S rRNA gene sequencing for identification of nonfermenting gram-negative bacilli recovered from patients attending a single cystic fibrosis center. J. Clin. Microbiol. 403793-3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harmsen, D., S. Dostal, A. Roth, S. Niemann, J. Rothgänger, M. Sammeth, J. Albert, M. Frosch, and E. Richter. 2003. RIDOM: comprehensive and public sequence database for identification of Mycobacterium species. BMC Infect. Dis. 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harmsen, D., J. Rothgänger, M. Frosch, and J. Albert. 2002. RIDOM: ribosomal differentiation of medical micro-organisms database. Nucleic Acids Res. 30416-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holland, R. D., J. G. Wilkes, F. Rafii, J. B. Sutherland, C. C. Persons, K. J. Voorhees, and J. O. J. Lay. 1996. Rapid identification of intact whole bacteria based on spectral patterns using matrix-assisted laser desorption/ionization with time-of-flight mass spectrometry. Rapid Commun. Mass Spectrom. 101227-1232. [DOI] [PubMed] [Google Scholar]
- 18.Hudson, V. L., C. L. Wielinski, and W. E. Regelmann. 1993. Prognostic implications of initial oropharyngeal bacterial flora in patients with cystic fibrosis diagnosed before the age of two years. J. Pediatr. 122854-860. [DOI] [PubMed] [Google Scholar]
- 19.Jarman, K. H., S. T. Cebula, A. J. Saenz, C. E. Petersen, N. B. Valentine, M. T. Kingsley, and K. L. Wahl. 2000. An algorithm for automated bacterial identification using matrix-assisted laser desorption/ionization mass spectrometry. Anal. Chem. 721217-1223. [DOI] [PubMed] [Google Scholar]
- 20.Jarman, K. H., D. S. Daly, C. E. Petersen, A. J. Saenz, N. B. Valentine, and K. L. Wahl. 1999. Extracting and visualizing matrix-assisted laser desorption/ionization time-of-flight mass spectral fingerprints. Rapid Commun. Mass Spectrom. 131586-1594. [DOI] [PubMed] [Google Scholar]
- 21.Kiska, D. L., A. Kerr, M. C. Jones, J. A. Caracciolo, B. Eskridge, M. Jordan, S. Miller, D. Hughes, N. King, and P. H. Gilligan. 1996. Accuracy of four commercial systems for identification of Burkholderia cepacia and other gram-negative nonfermenting bacilli recovered from patients with cystic fibrosis. J. Clin. Microbiol. 34886-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krishnamurthy, T., P. L. Ross, and U. Rajamani. 1996. Detection of pathogenic and non-pathogenic bacteria by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Rapid Commun. Mass Spectrom. 10883-888. [DOI] [PubMed] [Google Scholar]
- 23.Mahenthiralingam, E., T. Coenye, J. W. Chung, D. P. Speert, J. R. Govan, P. Taylor, and P. Vandamme. 2000. Diagnostically and experimentally useful panel of strains from the Burkholderia cepacia complex. J. Clin. Microbiol. 38910-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maier, T., and M. Kostrzewa. 2007. Fast and reliable MALDI-TOF MS-based microorganism identification. Chem. Today 2568-71. [Google Scholar]
- 25.McGowan, J. E. 2006. Resistance in nonfermenting gram-negative bacteria: multidrug resistance to the maximum. Am. J. Infect. Control 34S29-S37. [DOI] [PubMed] [Google Scholar]
- 26.McMenamin, J. D., T. M. Zaccone, T. Coenye, P. Vandamme, and J. J. LiPuma. 2000. Misidentification of Burkholderia cepacia in US cystic fibrosis treatment centers: an analysis of 1,051 recent sputum isolates. Chest 1171661-1665. [DOI] [PubMed] [Google Scholar]
- 27.Mellmann, A., J. L. Cloud, S. Andrees, K. Blackwood, K. C. Carroll, A. Kabani, A. Roth, and D. Harmsen. 2003. Evaluation of RIDOM, MicroSeq, and Genbank services in the molecular identification of Nocardia species. Int. J. Med. Microbiol. 293359-370. [DOI] [PubMed] [Google Scholar]
- 28.O'Hara, C. M. 2005. Manual and automated instrumentation for identification of Enterobacteriaceae and other aerobic gram-negative bacilli. Clin. Microbiol. Rev. 18147-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pineda, F. J., J. S. Lin, C. Fenselau, and P. A. Demirev. 2000. Testing the significance of microorganism identification by mass spectrometry and proteome database search. Anal. Chem. 723739-3744. [DOI] [PubMed] [Google Scholar]
- 30.Quinn, J. P. 1998. Clinical problems posed by multiresistant nonfermenting gram-negative pathogens. Clin. Infect. Dis. 27(Suppl. 1)S117-S124. [DOI] [PubMed] [Google Scholar]
- 31.Smith, D. L., L. B. Gumery, E. G. Smith, D. E. Stableforth, M. E. Kaufmann, and T. L. Pitt. 1993. Epidemic of Pseudomonas cepacia in an adult cystic fibrosis unit: evidence of person-to-person transmission. J. Clin. Microbiol. 313017-3022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suh, M., D. Hamburg, S. T. Gregory, A. E. Dahlberg, and P. A. Limbach. 2005. Extending ribosomal protein identifications to unsequenced bacterial strains using matrix-assisted laser desorption/ionization mass spectrometry. Proteomics 54818-4831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tablan, O. C., T. L. Chorba, D. V. Schidlow, J. W. White, K. A. Hardy, P. H. Gilligan, W. M. Morgan, L. A. Carson, W. J. Martone, and J. M. Jason. 1985. Pseudomonas cepacia colonization in patients with cystic fibrosis: risk factors and clinical outcome. J. Pediatr. 107382-387. [DOI] [PubMed] [Google Scholar]
- 34.Tamura, K., J. Dudley, M. Nei, and S. Kumar. 2007. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol. Biol. Evol. 241596-1599. [DOI] [PubMed] [Google Scholar]
- 35.Tang, Y. W., N. M. Ellis, M. K. Hopkins, D. H. Smith, D. E. Dodge, and D. H. Persing. 1998. Comparison of phenotypic and genotypic techniques for identification of unusual aerobic pathogenic gram-negative bacilli. J. Clin. Microbiol. 363674-3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vargha, M., Z. Takats, A. Konopka, and C. H. Nakatsu. 2006. Optimization of MALDI-TOF MS for strain level differentiation of Arthrobacter isolates. J. Microbiol. Methods 66399-409. [DOI] [PubMed] [Google Scholar]
- 37.Wunschel, S. C., K. H. Jarman, C. E. Petersen, N. B. Valentine, K. L. Wahl, D. Schauki, J. Jackman, C. P. Nelson, and E. V. White. 2005. Bacterial analysis by MALDI-TOF mass spectrometry: an inter-laboratory comparison. J. Am. Soc. Mass Spectrom. 16456-462. [DOI] [PubMed] [Google Scholar]