Abstract
The past 2 decades have brought worrying increases in severe Streptococcus pyogenes diseases globally. To investigate and compare the epidemiological patterns of these diseases within Europe, data were collected through a European Union FP-5-funded program (Strep-EURO). Prospective population-based surveillance of severe S. pyogenes infection diagnosed during 2003 and 2004 was undertaken in 11 countries across Europe (Cyprus, the Czech Republic, Denmark, Finland, France, Germany, Greece, Italy, Romania, Sweden, and the United Kingdom) using a standardized case definition. A total of 5,522 cases were identified across the 11 countries during this period. Rates of reported infection varied, reaching 3/100,000 population in the northern European countries. Seasonal patterns of infection showed remarkable congruence between countries. The risk of infection was highest among the elderly, and rates were higher in males than in females in most countries. Skin lesions/wounds were the most common predisposing factor, reported in 25% of cases; 21% had no predisposing factors reported. Skin and soft tissue were the most common foci of infection, with 32% of patients having cellulitis and 8% necrotizing fasciitis. The overall 7-day case fatality rate was 19%; it was 44% among patients who developed streptococcal toxic shock syndrome. The findings from Strep-EURO confirm a high incidence of severe S. pyogenes disease in Europe. Furthermore, these results have identified targets for public health intervention, as well as raising awareness of severe S. pyogenes disease across Europe.
Streptococcus pyogenes (group A streptococcus) is responsible for a diverse range of clinical manifestations, from mild skin/soft tissue infections and pharyngitis to more serious diseases, such as bacteremia, cellulitis, puerperal sepsis, meningitis, pneumonia, and necrotizing fasciitis. Development of streptococcal toxic shock syndrome (STSS) in these patients increases the risk of death substantially (35). The nonsuppurative complications, rheumatic fever and glomerulonephritis, continue to affect children in nonaffluent countries, underscoring the medicosocial impact of streptococcal disease (5).
Scarlet fever and puerperal sepsis have historically been leading causes of morbidity and mortality, with case fatality rates of 25 to 30% reported toward the end of the 19th century, decreasing to less than 2% by 1900, suggesting a natural variation in the virulence of the pathogen (18, 20, 36). In the late 1980s, an unexplained recrudescence of invasive S. pyogenes infections was reported from Europe and the United States, remarkable for the severity of localized tissue destruction and life-threatening systemic toxicity in the cases described (3, 15, 19, 25, 37, 39). Observations of a clinical syndrome analogous to the toxic shock syndrome induced by Staphylococcus aureus led to the proposal of a case definition for STSS by an international working group in 1993 (3, 14, 45).
A large number of virulence mechanisms are involved in the complex pathogenicity of this organism (5). Among host factors, age; underlying disease, such as diabetes, varicella, or other acute or chronic skin lesions; or specific risk behaviors, such as injecting drug use, are known to influence the risk of S. pyogenes infection (7, 12, 13, 34). Environmental factors, such as household size and overcrowding (33), are also known to play an important role in influencing S. pyogenes transmission. As the majority of cases occur spontaneously in the community, possibilities for prevention remain limited.
Increases in invasive S. pyogenes disease have been reported from various European countries during the 1990s and into the 2000s (21). Comparison of these estimates of incidence has been limited by substantial variations in case definitions and surveillance methods and a lack of data from central, eastern, and southern European countries. In order to obtain more robust, comparable, and widespread estimates of disease incidence, a multinational network for invasive S. pyogenes disease surveillance was created in 2002—Strep-EURO—funded by the European Union (21, 32). The Strep-EURO project initiated collaboration between several European public health institutes and associated reference laboratories to meet several program objectives, including unified surveillance of invasive S. pyogenes disease for a 2-year period. This report supplements national analyses already undertaken on the Strep-EURO data by comparing the epidemiological patterns of invasive S. pyogenes disease among the 11 participating countries in 2003 and 2004 (4, 6, 22, 24, 38).
MATERIALS AND METHODS
Case ascertainment.
Eleven countries (Cyprus, the Czech Republic, Denmark, Finland, France, Germany, Greece, Italy, Romania, Sweden, and the United Kingdom) participated in the Strep-EURO project, coordinated by the University of Lund in Sweden. All countries undertook prospective enhanced surveillance between 1 January 2003 and 31 December 2004 to identify cases of severe S. pyogenes disease diagnosed during this period. Cases were identified through invited submission of isolates from local microbiology laboratories to the national streptococcal reference center. Three countries (Finland, Sweden, and the United Kingdom) also identified cases from national laboratory reporting schemes to maximize case ascertainment, with cases reconciled to avoid duplicate counting. Within-country participation was national for most countries. The only exceptions were the Czech Republic and Romania, where sentinel sites across the country were recruited, and Greece and the United Kingdom, where surveillance was restricted to the Athens metropolitan area and to England, Wales, and Northern Ireland, respectively.
Case definitions.
Cases were defined as patients with S. pyogenes isolated from a normally sterile site or a nonsterile site in combination with clinical signs of STSS. The 1993 Working Group on Severe Streptococcal Infections definition of STSS was used (45): hypotensive shock in conjunction with two or more specified clinical indicators (renal impairment, abnormal liver function, respiratory distress, erythematous rash, disseminated intravascular coagulopathy, or soft tissue necrosis), with cases of “definite” (those with sterile-site isolates) and “probable” (those with nonsterile-site isolates) STSS combined.
Data processing.
A standardized surveillance data set was defined, comprising demographic, clinical, and risk factor information for cases collected through questionnaires disseminated to all participants. Mortality outcome data were obtained through the national death registries in Denmark and Finland (2004 only), or else through the questionnaires. In Denmark and Sweden, as enhanced surveillance was already in place, existing questionnaires were used, with any differences from the standardized items noted for future analysis. In Finland, clinical and risk factor data were collected by an infectious-disease clinician's review of patient medical records in a predefined area (Pirkanmaa health district, Western Finland; population, 440,000). Data were formatted and transferred to the data hub in Finland according to the specified protocol and stored in a secure SQL server database. Further validation checks of the combined data were undertaken to identify any inconsistencies and to ensure all cases met the case definition. Cases marked as having STSS were checked to ensure this definition was met according to the clinical indicators given, while the same indicators were also used to identify cases not marked as STSS but that met the case definition.
Statistical, geographical, and seasonal analysis.
Data were extracted from the SQL server and imported into STATA software (release 8.2, 2005; Stata Corporation, College Station, TX) for statistical analysis. Descriptive statistics were undertaken, with χ2 and Kruskal-Wallis tests applied to test for statistical significance of differences between subgroups in proportions and distributions of continuous variables, respectively, and linear regression to evaluate associations between continuous variables. Rates of infection were calculated using midyear resident population estimates as denominators for the respective countries for each year (or the closest available year) according to age and sex. Overall country rates were age standardized according to the European Standard Population to facilitate comparison. Exact 95% confidence intervals (CI) around rates and rate ratios (RR) were calculated according to the Poisson distribution. Country-specific rates were mapped using MapInfo Professional (version 8.0, 2005; release build 18; MapInfo Corporation, Troy, NY). Six-week moving averages of counts of infection were calculated to smooth out weekly random variations in incidence for the assessment of seasonal patterns of infection.
RESULTS
Outcome of surveillance.
During 2003 and 2004, a total of 5,522 cases meeting the definition of severe S. pyogenes infection were identified across the 11 participating countries (Table 1). The numbers of cases identified varied from 4 in Cyprus (0.1% of all cases) to 3,630 in the United Kingdom (66% of all cases). Participation came from across the entire surveillance area for Finland, Denmark, Sweden, and the United Kingdom. In France, Germany, and Greece, participation by hospitals across the surveillance area was incomplete, with participation in Greece limited to two pediatric (65% of cases) and seven general hospitals. For Italy and Romania, participation was good for the defined areas of Lombardia and Bucharest and seven other counties of Romania, respectively.
TABLE 1.
Summary results for severe cases of S. pyogenes infection identified through the Strep-EURO program in 2003 and 2004
| Country | Cases
|
Rate per 100,000 population
|
Age distribution (yr)
|
Males
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | Crude | Age adjusted | Mean | Median | Range | 0-17
|
18-64
|
65+
|
||||||
| No. | % | No. | % | No. | % | No. | % | ||||||||
| Cyprus | 4 | <1 | 0.27 | 0.30 | 20 | 14 | 0-53 | 3 | 75 | 1 | 25 | 0 | 0 | 2 | 50 |
| Czech Republic | 137 | 2 | 1.50 | 1.48 | 43 | 47 | 0-91 | 34 | 25 | 72 | 52 | 31 | 23 | 78 | 57 |
| Denmark | 278 | 5 | 2.58 | 2.19 | 56 | 61 | 0-100 | 29 | 10 | 122 | 44 | 127 | 46 | 127 | 46 |
| Finland | 257 | 5 | 2.46 | 2.28 | 49 | 53 | 0-92 | 23 | 9 | 176 | 68 | 58 | 23 | 139 | 54 |
| France | 272 | 5 | NAa | NA | 42 | 42 | 0-97 | 63 | 23 | 145 | 53 | 64 | 24 | 125 | 46 |
| Germany | 203 | 4 | NA | NA | 50 | 55 | 0-93 | 34 | 17 | 92 | 47 | 72 | 36 | 105 | 55 |
| Greece | 67 | 1 | NA | NA | 22 | 8 | 1-90 | 44 | 66 | 14 | 21 | 9 | 13 | 37 | 55 |
| Italy | 83 | 2 | 0.38 | 0.40 | 38 | 39 | 0-94 | 20 | 24 | 45 | 55 | 17 | 21 | 48 | 59 |
| Romania | 33 | 1 | 0.30 | 0.36 | 29 | 28 | 0-83 | 14 | 42 | 17 | 52 | 2 | 6 | 17 | 52 |
| Sweden | 558 | 10 | 3.10 | 2.28 | 65 | 70 | 0-99 | 26 | 5 | 201 | 36 | 331 | 59 | 281 | 50 |
| United Kingdom | 3,630 | 66 | 3.31 | 2.94 | 49 | 48 | 0-104 | 463 | 13 | 1,792 | 50 | 1,324 | 37 | 1,953 | 55 |
| Total | 5,522 | 100 | 2.79 | 2.37 | 50 | 52 | 0-104 | 753 | 14 | 2,677 | 49 | 2,035 | 37 | 2,912 | 53 |
NA, not available.
Overall rates of infection.
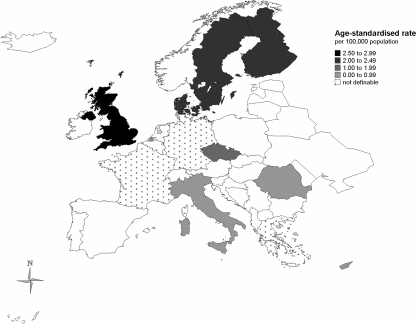
Rates of infection were calculated using data from all countries except Germany, France, and Greece, owing to incomplete participation among hospitals across those countries' entire surveillance areas or within any definable catchment zone. Of the remaining eight countries where the rate could be calculated for the entire country or a specified region, the overall (crude) rate was 2.79 (95% CI, 2.72 to 2.87) per 100,000 population. A general north-south pattern could be discerned among participants, with the four northernmost European countries having the highest rates of reports (Finland, 2.46; Denmark, 2.58; Sweden, 3.10; United Kingdom, 3.31), with a combined rate of 3.17/100,000. Age-adjusted rates were calculated to provide more comparable estimates of rates of infection (Fig. 1). Within the northern European countries, age-adjusted rates in the United Kingdom (2.94) remained significantly higher than those for Finland or Sweden (2.28 for each; RR = 0.78; 95% CI, 0.65 to 0.92) or Denmark (2.19; RR = 0.74; 95% CI, 0.63 to 0.89). In the two Central European countries, the highest age-adjusted rate was reported for the Czech Republic (1.48), with rates for Romania (0.36) more similar to those observed in Italy (0.40) and Cyprus (0.30).
FIG. 1.
Annual age-standardized rates of severe S. pyogenes infection by country for 2003 and 2004. The rates are standardized against the European standard population. Rates were calculated nationally for Cyprus, the Czech Republic, Denmark, Finland, and Sweden and for the following areas in other countries: Italy, the Lombardia region; Romania, Bucharest and seven other counties; the United Kingdom, England, Wales, Northern Ireland, the Channel Islands, and the Isle of Man.
Age and sex distribution of cases.
Overall, 53% of patients with severe S. pyogenes infection were male, with most countries observing slightly higher numbers of cases in men than women (Table 1) with no significant variation between countries in this ratio (χ2 [10 df] = 17.39; P = 0.07). Age- and sex-specific rates were calculated for the Czech Republic, Denmark, Finland, Sweden, and the United Kingdom and sex-specific rates only for Cyprus, Italy, and Romania owing to the small numbers of cases reported. In all countries except Denmark, the rates of infection reported were higher in males than females (Fig. 2), overall 3.03 versus 2.55 per 100,000 population (RR = 1.19; 95% CI, 1.12 to 1.26). Age distributions of cases varied between countries, with a high proportion of cases from Greece being children (66% less than 18 years old). Excluding Greece, significant variations in age distributions between countries were apparent, (Kruskal-Wallis test, χ2 [9 df] = 261.47; P < 0.001), with cases being notably older in Sweden (median, 70 years) than all other countries (Table 1). Rates of infection were highest in the elderly and to a much lesser extent in young children (0 to 4 years old) (Fig. 2). For Finland and the Czech Republic, the elevation in the elderly (75+ years) was less pronounced than for the other countries (less than 6/100,000 for both sexes), whereas in Sweden the reverse was true, with rates of 16 and 13/100,000 in males and females, respectively. A slight elevation in women of childbearing age could also be discerned, most markedly in Denmark. Data from the United Kingdom were unusual in showing a prominent increased rate in young males (25 to 44 years old).
FIG. 2.
Annual age-specific rates of severe S. pyogenes infection for 2003 and 2004.
Seasonal patterns of infection.
Analyses of seasonal patterns were undertaken using 6-week moving averages for all countries that reported more than 250 cases of severe S. pyogenes infection over the 2 years: Denmark, Finland, France, Sweden, and the United Kingdom. Seasonal patterns were similar across all these countries, with a high incidence in winter/spring and a low incidence in late summer/autumn (Fig. 3) . The inflections in incidence were nearly simultaneous at several points over the 2 years.
FIG. 3.
Seasonal patterns of severe S. pyogenes infection by country for 2003 and 2004.
Clinical and risk factor information.
Of the 5,522 cases identified, questionnaires were returned for 79% (4,334 cases). Comparison of variables available for cases with and without questionnaires returned identified those with questionnaires to be slightly older than cases without questionnaires (median age, 53 versus 45 years; Kruskal-Wallis test, χ2 [1 df] = 7.24; P < 0.01), although the sex distributions were similar (χ2 [1 df] = 1.11; P = 0.29), as were peak seasons for cases (January to March; χ2 [1 df] = 3.07; P = 0.08).
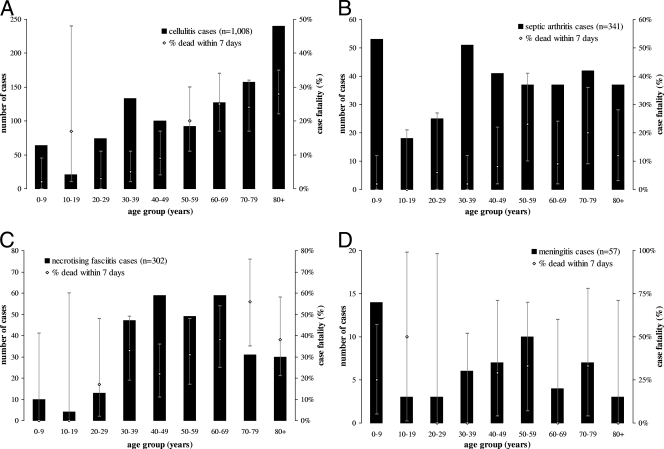
Clinical information was available for 3,894 (71%) cases in total (Table 2). Of these, 19% (631) had no focus of infection reported. None of the cases from Romania and 1% (177/179) of those from Germany were reported as nonfocal, whereas 10 to 26% of the cases in other countries were reported as bacteremic without focal symptoms. Of the focal infections, cellulitis was the most commonly reported overall (32%) and for a majority of the countries, with the exception of the Czech Republic, France, and Italy, where necrotizing fasciitis was more often identified. The age distribution of cellulitis cases showed increasing frequency with increasing age, although cases in 10- to 19-year-olds were relatively uncommon (Fig. 4). In total, 308 cases of necrotizing fasciitis were identified, 8% of all cases, with cases occurring primarily in adults aged 30 to 69 years old. Other presentations reported included septic arthritis (9%), puerperal sepsis (3%), and meningitis (2%), with the latter most common in children <10 years old. Thirteen percent (493/3,894) of cases developed STSS, rising to 50% among cases of necrotizing fasciitis. France reported relatively high numbers of puerperal sepsis cases (9%) compared to other countries (5% or less).
TABLE 2.
Clinical presentations of severe cases of S. pyogenes infection, 2003-04
| Parameter | Cases with clinical information
|
Bacteremia with no focal symptoms
|
Necrotizing fasciitis
|
Cellulitis
|
Septic arthritis
|
Puerperal sepsis
|
Meningitis
|
Othera
|
Death within 7 daysb
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. of deaths/total no. of cases | % | |
| Country | ||||||||||||||||||
| Cyprus | 4 | 100 | 1 | 25 | 0 | 0 | 1 | 25 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 50 | 0/4 | 0 |
| Czech Republic | 136 | 99 | 26 | 19 | 28 | 21 | 23 | 17 | 12 | 9 | 0 | 0 | 4 | 3 | 32 | 24 | 22/92 | 24 |
| Denmark | 254 | 91 | 51 | 20 | 16 | 6 | 67 | 26 | 14 | 6 | 12 | 5 | 8 | 3 | 92 | 37 | 43/277 | 16 |
| Finland | 20 | 8 | 2 | 10 | 1 | 5 | 3 | 15 | 1 | 5 | 1 | 5 | 2 | 10 | 10 | 50 | 7/147 | 5 |
| France | 272 | 100 | 39 | 14 | 48 | 18 | 40 | 15 | 26 | 10 | 25 | 9 | 13 | 5 | 67 | 25 | 53/198 | 27 |
| Germany | 179 | 88 | 2 | 1 | 22 | 12 | 26 | 15 | 3 | 2 | 2 | 1 | 11 | 6 | 97 | 55 | 17/42 | 40 |
| Greece | 66 | 99 | 14 | 22 | 5 | 8 | 25 | 38 | 8 | 12 | 0 | 0 | 3 | 5 | 14 | 22 | 1/65 | 2 |
| Italy | 72 | 87 | 19 | 26 | 14 | 19 | 9 | 13 | 2 | 3 | 2 | 3 | 0 | 0 | 31 | 43 | 11/51 | 22 |
| Romania | 32 | 97 | 0 | 0 | 4 | 14 | 9 | 31 | 1 | 3 | 0 | 0 | 1 | 3 | 14 | 48 | 3/33 | 9 |
| Sweden | 486 | 87 | NAc | 51 | 11 | NA | 73 | 16 | 13 | 3 | 0 | 0 | NA | 40/447 | 9 | |||
| United Kingdom | 2,373 | 65 | 477 | 21 | 119 | 5 | 833 | 37 | 209 | 9 | 52 | 2 | 19 | 1 | 1,052 | 47 | 446/2,114 | 21 |
| Total | 3,894 | 71 | 631 | 19 | 308 | 8 | 1,036 | 32 | 349 | 9 | 107 | 3 | 61 | 2 | 1,411 | 43 | 643/3,470 | 19 |
| STSS | 493 | 13 | 32 | 5 | 153 | 50 | 102 | 10 | 34 | 10 | 14 | 13 | 9 | 15 | 115 | 8 | 184/415 | 44 |
| Death within 7 days | - | 100 | 20 | 80 | 32 | 152 | 17 | 28 | 9 | 4 | 4 | 12 | 23 | 275 | 24 | - | ||
Excluding cases with necrotizing fasciitis, cellulitis, septic arthritis, puerperal sepsis, or meningitis.
Information on mortality is derived from the study questionnaire for all countries except Denmark and Finland, where it was obtained from the national death registries.
NA, not available.
FIG. 4.
Age distribution of key clinical presentations of severe cases of S. pyogenes infection in Europe for 2003 and 2004 (data from all countries except Greece). The error bars indicate 95% confidence intervals.
Overall, 19% (643/3,470) of patients died within 7 days of diagnosis (Table 2). Case fatality rates were highest among cases of necrotizing fasciitis at 32% (80/254) overall, rising with increasing age to reach 56% in patients aged 70 to 79 (Fig. 4). Of the defined clinical presentations, the highest absolute number of deaths occurred in patients with cellulitis, 152 of 895 cases with outcome information. Development of STSS was strongly associated with death, with 44% (184/415) of patients with STSS versus 15% (409/2,707) of those without dying within 7 days (χ2 [1 df] = 199.79; P < 0.001). Case fatality rates varied between countries and were highest for those reporting more cases of necrotizing fasciitis. Cases from Finland and Sweden had much lower mortalities of 5% and 9%.
Information on risk factors was available for 3,178 (58%) of the cases. For 21% (683) of patients, no particular risk factors were identified; this varied substantially between countries, from 0% to 27% (Table 3). The most common single risk factor reported was skin lesions, reported in 25% (681) of cases overall, with 10% (66) of these being patients with diabetes and 9% (60) injecting drug users. In total, 471 (15%) cases were injecting drug users, with 93% (440) of these coming from the United Kingdom, where 22% of cases were injecting drug users compared to 6% or less in other countries. Nearly half (45%; 21 cases) of the cases from Greece were patients with chickenpox, a reflection of the largely pediatric setting of the surveillance in this country, with all but 1 of the 21 cases being children. Other notable differences included the proportions of patients with diabetes in the Czech Republic (22%) and Sweden (14%). These proportions remained high even among patients less than 75 years old, with 20% and 12% of Czech and Swedish cases, respectively, in this age group noted as having diabetes compared to less than 6% in all other countries. Eight percent of cases (265/3,178) were associated with health care interventions, although the rates were higher in the Czech Republic and France at 26% and 17%, respectively, with postsurgical infections accounting for most of these.
TABLE 3.
Risk factors reported among cases of severe S. pyogenes infection for 2003 and 2004
| Country | Cases with risk factor information
|
Diabetes
|
Injecting drug use
|
Chicken pox
|
Immuno-compro-mised
|
Skin lesions
|
Surgery
|
Health care-associated infectiona
|
Otherb
|
None reported
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Cyprus | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 50 | 1 | 25 | 0 | 0 | 0 | 0 | 1 | 25 | 1 | 25 |
| Czech Republic | 72 | 53 | 16 | 22 | 2 | 3 | 3 | 4 | 23 | 32 | 5 | 7 | 11 | 15 | 19 | 26 | 23 | 32 | 0 | 0 |
| Denmark | 235 | 85 | 13 | 6 | 6 | 3 | 3 | 1 | 16 | 7 | 42 | 18 | 0 | 0 | 26 | 11 | 80 | 34 | 61 | 26 |
| Finland | 20 | 8 | 1 | 5 | 0 | 0 | 1 | 5 | 1 | 5 | 10 | 50 | 1 | 5 | 2 | 10 | 3 | 15 | 3 | 15 |
| France | 151 | 56 | 10 | 7 | 0 | 0 | 5 | 3 | 20 | 13 | 38 | 25 | 19 | 13 | 25 | 17 | 61 | 40 | 0 | 0 |
| Germany | 50 | 25 | 0 | 0 | 0 | 0 | 3 | 6 | 9 | 18 | 23 | 46 | 3 | 6 | 6 | 12 | 16 | 32 | 0 | 0 |
| Greecec | 47 | 70 | 2 | 4 | 3 | 6 | 21 | 45 | 7 | 15 | 13 | 28 | 4 | 9 | 4 | 9 | 3 | 6 | 0 | 0 |
| Italy | 48 | 58 | 3 | 6 | 3 | 6 | 1 | 2 | 9 | 19 | 14 | 29 | 2 | 4 | 5 | 10 | 10 | 21 | 11 | 23 |
| Romania | 26 | 79 | 0 | 0 | 1 | 4 | 1 | 4 | 3 | 12 | 10 | 38 | 1 | 4 | 1 | 4 | 5 | 19 | 5 | 19 |
| Sweden | 483 | 87 | 67 | 14 | 16 | 3 | NA | 82 | 17 | NA | 16 | 3 | 23 | 5 | 188 | 39 | 128 | 27 | ||
| United Kingdom | 2042 | 56 | 150 | 7 | 440 | 22 | 44 | 2 | 356 | 17 | 525 | 26 | 109 | 5 | 154 | 8 | 167 | 8 | 474 | 23 |
| All countries | 3,178 | 58 | 262 | 8 | 471 | 15 | 82 | 3 | 528 | 17 | 681 | 25 | 166 | 5 | 265 | 8 | 557 | 18 | 683 | 21 |
Includes postsurgical infections.
Excluding cases with any other risk factors specified in the table.
Cases primarily drawn from a children's hospital.
c NA, not available.
DISCUSSION
Analysis of data gathered in the 11 countries participating in the Strep-EURO program has yielded some interesting new insights into the epidemiology of severe S. pyogenes disease in Europe during the 2000s. The project succeeded in establishing the first dedicated international surveillance network for these infections, through which over 5,000 cases were identified over the 2 years, with a wealth of clinical and microbiological information accompanying the majority. Comprehensive epidemiological data on severe S. pyogenes infections were obtained for the first time from France, Greece, and Romania.
Estimation of the incidence of severe S. pyogenes infection identified a general north-south gradient from high to low. Similar age-standardized rates were observed among the three Nordic participants, Finland, Denmark, and Sweden, between 2.2 and 2.3 per 100,000 population, with rates in the United Kingdom higher still at 2.90/100,000. The crude rates from these countries (Finland, 2.46; Denmark, 2.58; Sweden, 3.10; United Kingdom, 3.31) were reasonably close to the those observed in the United States and Australia during this period (28, 29). The large number of cases among injecting drug users in the United Kingdom—22% of all the United Kingdom's cases compared to 6% or less in other countries—is likely to have elevated this rate. In contrast, the rates of reports in the more central and southern countries, the Czech Republic, Romania, Cyprus, and Italy, were substantially lower at 0.3 to 1.5 per 100,000 population, likely a reflection of poorer uptake of microbiological investigative methods within these countries. Data provided by hospitals participating in the European Antimicrobial Resistance Surveillance System further support this explanation, with the rate of blood culture sets taken per head of population much higher for the United Kingdom, Sweden, and Finland (approximately 30 to 40 per 1,000 population) than for Italy, Romania, Cyprus, or the Czech Republic (<15 per 1,000) (11). Failure to report diagnosed cases could also account for the lower rates observed in some countries, although evidence to support this assertion would be difficult to find.
In broad terms, the demographic profiles of patients diagnosed with severe S. pyogenes infection were similar across countries, with a male excess in rates of infection seen wherever it was calculable, with the exception of Denmark, in line with findings from North America (23, 30). The elderly and, to a lesser extent, infants were universally found to be at the highest risk of infection. However, some interesting differences emerged between countries. Within the United Kingdom, the large number of infections in drug injectors fundamentally reshaped the age distribution, resulting in a clear excess of young male cases. That the same excess could not be discerned in other countries provides further evidence of the confinement of this epidemic to the United Kingdom, which could otherwise be explained by better recognition or reporting of this risk factor. Within the Czech Republic and Finland, rates of infection were relatively low in the elderly, conceivably due to differences in the provision of institutional care, assuming an elevated risk in such settings (1, 41). Differences in strain type distribution may also explain such variation. These and other hypotheses warrant further investigation, as they may lead to some unique insights into the transmission of S. pyogenes infection in the elderly.
Although many countries have reported strong seasonal patterns of infection (23, 25, 27, 42, 43), simultaneous comparison of these patterns in different countries has not been undertaken. Comparison of the data from the countries that reported the highest numbers of cases identified remarkable similarities, both in terms of the broad pattern of infection, which peaked in the winter and spring months in all countries and fell markedly during the late summer and autumn, and also in the timing of these changes. The drivers behind these seasonal patterns remain poorly understood, although the nearly simultaneous changes seen in this project point to an influence whose timing of effect would be very similar between countries. An environmental explanation, such as decreased levels of absolute humidity affecting mucosal defense barriers or an influence of lowered levels of sunlight exposure on immunological function, seems plausible, as suggested by modeling studies of meningococcal and pneumococcal infection, respectively (9, 26). Seasonal changes in behavioral patterns, in particular, indoor gatherings versus outdoor activities and school attendance according to the academic term-holiday cycle, could also play a significant role in transmission patterns, which could also explain the late-summer/autumn nadir. Seasonal patterns of viral respiratory infections might also play a role in inducing vulnerability to S. pyogenes infection.
The clinical manifestations reported across the participating countries delineated the severity of the infections reported, with one in five patients dying within 7 days of infection diagnosis. Development of STSS was a strong predictor of subsequent death, with nearly half of these patients dying within 7 days. Around a fifth of infections had no apparent focus identified, broadly in line with reports from other countries, which tend to range from 10 to 25% (2, 28, 42). How many of these cases were true cases of primary bacteremia remains unclear, as identifying a focus for the infection can present a diagnostic challenge. A substantial proportion of the cases identified during the 2 years had clinical presentations other than those outlined on the questionnaire. Broadening of the standard clinical presentations given to include at a minimum peritonitis and pneumonia would be of future benefit, as individual countries have found through their own detailed analyses of additional items they chose to include (4, 10, 22, 38).
Variations were noted between countries in the clinical presentations reported. France reported proportionally high numbers of cases of puerperal sepsis as a result of several maternity unit clusters occurring during this period (8, 31). A predominance of necrotizing fasciitis was apparent within the Czech Republic, France, and Italy, where such cases made up one in five of all the cases identified, suggestive of a possible bias either in the application of microbiological investigation or in the reporting of more severe cases. Case fatality rates varied markedly between countries, in part a reflection of the severity of the clinical syndromes reported and possibly also affected by differences in dominant serotypes. However, the completeness of mortality reporting varied between counties, which could introduce a bias into the estimates obtained. Obtaining mortality data by linking case reports to death registries, as undertaken by Denmark and Finland in this study, would obviate this potential problem.
One of the more striking features of S. pyogenes is its ability to cause severe disease in the otherwise fit and healthy. The results from our study showed that a quarter to a fifth of cases in most countries had no particular factors predisposing to severe infection. A certain degree of caution should be exercised in interpreting these results, as it was left to the discretion of the reporting clinicians (or country coordinators in further cleaning the data) to decide what would be considered a risk factor beyond the standard options given on the study questionnaire. In some countries, for example, Sweden, coronary heart disease was included in this list, a condition sufficiently common in the elderly to have had a strong influence on the estimation of the numbers of patients without risk factors. This limitation notwithstanding, some interesting patterns do emerge, aside from the dominance of injecting drug use in the United Kingdom noted above. Two countries, the Czech Republic (26%) and France (17%), reported substantially higher proportions of their cases being health care intervention associated than other countries (most were around 10%). The maternity clusters in France probably account for their figure, although it remains unclear why the Czech Republic figure should be so high. A further notable difference between countries lies in the high proportion of cases from the Czech Republic (22%), and to a lesser extent Sweden (14%), having diabetes. The prevalence of diabetes in the general population is known to be high in the Czech Republic, possibly explaining their figure, although it remains unclear why the Swedish cases should be so different (44).
Despite efforts to capture standardized data, some biases became apparent when the results were analyzed, as discussed above, which is to be expected given the different clinical practices and surveillance traditions among participating countries. Nonetheless, the data collected constitute a valuable resource that has already been used in the United Kingdom and France to form an evidence base for the prevention and control of S. pyogenes infections in hospital and community settings (16, 17, 33, 40). The size of the collection has provided a powerful basis to address longstanding questions, including the interrelationship between host and pathogen characteristics in specific clinical manifestations and patient outcomes and the drivers for seasonal patterns of infection, hitherto poorly understood. Continued surveillance on a global basis is essential given the dynamic nature of these infections, which are capable of infiltrating new subpopulations over time, if public health measures are to be targeted effectively to reduce the burden of these life-threatening diseases.
Acknowledgments
We extend our sincere thanks to all the clinicians and microbiologists in the 11 participating countries who took the time to report cases to their respective country leads. The following additional members of country teams also contributed significantly to the project: Cyprus, Maria Alexandrou, Nasia Hannidou, and Eleni Konteatou; Czech Republic, Radmila Dousova and Iveta Mouchova; Finland, Jari Jalava, Sari Rantala, and Petri Ruutu; Germany, Claudia Brandt; Greece, Nicholas J. Legakis, Anastasia Pangalis, and Panayotis T. Tassios; Italy, Monica Imperi, Marco Pataracchia, and Simona Recchia; Sweden, Lars Björck, Hans Tapper, Ulrich von Pawel-Rammingen, Christina Johansson, Gunnel Möllerberg, and Ingrid Andersson; and United Kingdom, Neelam Alhaddad, Chenchal Dhami, Asha Tanna, Georgia Duckworth, and Robert George.
This work was supported by a grant from the EU Fifth Framework Research Programme (QLK2.CT.2002.01398).
Footnotes
Published ahead of print on 7 May 2008.
REFERENCES
- 1.Auerbach, S. B., B. Schwartz, D. Williams, M. G. Fiorilli, A. A. Adimora, R. F. Breiman, and W. R. Jarvis. 1992. Outbreak of invasive group A streptococcal infections in a nursing home. Lessons on prevention and control. Arch. Intern. Med. 1521017-1022. [PubMed] [Google Scholar]
- 2.Ben Abraham, R., N. Keller, R. Vered, R. Harel, Z. Barzilay, and G. Paret. 2002. Invasive group A streptococcal infections in a large tertiary center: epidemiology, characteristics and outcome. Infection 3081-85. [DOI] [PubMed] [Google Scholar]
- 3.Cone, L. A., D. R. Woodard, P. M. Schlievert, and G. S. Tomory. 1987. Clinical and bacteriologic observations of a toxic shock-like syndrome due to Streptococcus pyogenes. N. Engl. J. Med. 317146-149. [DOI] [PubMed] [Google Scholar]
- 4.Creti, R., M. Imperi, L. Baldassarri, M. Pataracchia, S. Recchia, G. Alfarone, and G. Orefici. 2007. emm types, virulence factors, and antibiotic resistance of invasive Streptococcus pyogenes isolates from Italy: what has changed in 11 years? J. Clin. Microbiol. 452249-2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunningham, M. W. 2000. Pathogenesis of group A streptococcal infections. Clin. Microbiol. Rev. 13470-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darenberg, J., B. Luca-Harari, A. Jasir, A. Sandgren, H. Pettersson, C. Schalen, M. Norgren, V. Romanus, A. Norrby-Teglund, and B. H. Normark. 2007. Molecular and clinical characteristics of invasive group A streptococcal infection in Sweden. Clin. Infect. Dis. 45450-458. [DOI] [PubMed] [Google Scholar]
- 7.Davies, H. D., A. McGeer, B. Schwartz, K. Green, D. Cann, A. E. Simor, D. E. Low, et al. 1996. Invasive group A streptococcal infections in Ontario, Canada. N. Engl. J. Med. 335547-554. [DOI] [PubMed] [Google Scholar]
- 8.Denoeud, L., A. Lepoutre, A. Bouvet, and B. Coignard. 2005. Description of nosocomial post-operative or postpartum invasive Streptococcus pyogenes infection in France from 1st August 2003 to 31st December 2003. Bull. Epidemiol. Hebdomadaire 33165-166. http://www.invs.sante.fr/beh/2005/33/beh_33_2005.pdf. (In French.) [Google Scholar]
- 9.Dowell, S. F., C. G. Whitney, C. Wright, C. E. Rose, Jr., and A. Schuchat. 2003. Seasonal patterns of invasive pneumococcal disease. Emerg. Infect. Dis. 9573-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekelund, K., P. Skinhoj, J. Madsen, and H. B. Konradsen. 2005. Invasive group A, B, C and G streptococcal infections in Denmark 1999-2002: epidemiological and clinical aspects. Clin. Microbiol. Infect. 11569-576. [DOI] [PubMed] [Google Scholar]
- 11.European Antimicrobial Resistance Surveillance System. 2006. EARSS annual report 2005. National Institute of Public Health and the Environment, Bilthoven, The Netherlands. http://www.rivm.nl/earss/Images/EARSS%202005_tcm61-34899.pdf.
- 12.Factor, S. H. 2003. Invasive group A streptococcal disease: risk factors for adults. Emerg. Infect. Dis. 9970-977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Factor, S. H., O. S. Levine, L. H. Harrison, M. M. Farley, A. McGeer, T. Skoff, C. Wright, B. Schwartz, and A. Schuchat. 2005. Risk factors for pediatric invasive group A streptococcal disease. Emerg. Infect. Dis. 111062-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fanta, J., J. Drabkova, F. Rehak, V. Smat, K. Votocek, and K. Frankova. 1984. Primary peritonitis imitating the toxic shock syndrome (TSS). Prakt. Lek. (Prague) 64674-676. [Google Scholar]
- 15.Gaworzewska, E., and G. Colman. 1988. Changes in the pattern of infection caused by Streptococcus pyogenes. Epidemiol. Infect. 100257-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Protection Agency Group A Streptococcus Working Group. 2004. Interim UK guidelines for management of close community contacts of invasive group A streptococcal disease. Commun. Dis. Public Health 7354-361. [PubMed] [Google Scholar]
- 17.High Council of Public Hygiene in France. 2005. Recommendations relating to the guidance around one or more cases of community-acquired invasive Streptococcus pyogenes infection. Department of Health, Paris, France. http://www.sante.gouv.fr/htm/dossiers/cshpf/a_mt_181105_streptococcus.pdf. (In French.)
- 18.Hopkins, S., and A. B. Maclean. 2006. Group A streptococcus: a continued threat. J. Obstet. Gynaecol. 26593-595. [DOI] [PubMed] [Google Scholar]
- 19.Hribalova, V. 1988. Streptococcus pyogenes and the toxic shock syndrome. Ann. Intern. Med. 108772. [DOI] [PubMed] [Google Scholar]
- 20.Katz, A. R., and D. M. Morens. 1992. Severe streptococcal infections in historical perspective. Clin. Infect. Dis. 14298-307. [DOI] [PubMed] [Google Scholar]
- 21.Lamagni, T. L., A. Efstratiou, J. Vuopio-Varkila, A. Jasir, C. Schalén, and Strep-EURO. 2005. The epidemiology of severe Streptococcus pyogenes associated disease in Europe. Euro. Surveill. 10179-184. [DOI] [PubMed] [Google Scholar]
- 22.Lamagni, T. L., S. Neal, C. Keshishian, N. Alhaddad, R. George, G. Duckworth, J. Vuopio-Varkila, and A. Efstratiou. 2008. Severe Streptococcus pyogenes infections, United Kingdom, 2003-2004. Emerg. Infect. Dis. 14201-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laupland, K. B., T. Ross, D. L. Church, and D. B. Gregson. 2006. Population-based surveillance of invasive pyogenic streptococcal infection in a large Canadian region. Clin. Microbiol. Infect. 12224-230. [DOI] [PubMed] [Google Scholar]
- 24.Luca-Harari, B., K. Ekelund, L. M. van der, M. Staum-Kaltoft, A. M. Hammerum, and A. Jasir. 2008. Clinical and epidemiological aspects of invasive Streptococcus pyogenes infections in Denmark during 2003 and 2004. J. Clin. Microbiol. 4679-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin, P. R., and E. A. Høiby. 1990. Streptococcal serogroup A epidemic in Norway 1987-1988. Scand. J. Infect. Dis. 22421-429. [DOI] [PubMed] [Google Scholar]
- 26.Molesworth, A. M., L. E. Cuevas, S. J. Connor, A. P. Morse, and M. C. Thomson. 2003. Environmental risk and meningitis epidemics in Africa. Emerg. Infect. Dis. 91287-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Brien, K. L., B. Beall, N. L. Barrett, P. R. Cieslak, A. Reingold, M. M. Farley, R. Danila, E. R. Zell, R. Facklam, B. Schwartz, and A. Schuchat. 2002. Epidemiology of invasive group A streptococcus disease in the United States, 1995-1999. Clin. Infect. Dis. 35268-276. [DOI] [PubMed] [Google Scholar]
- 28.O'Grady, K. A., L. Kelpie, R. M. Andrews, N. Curtis, T. M. Nolan, G. Selvaraj, J. W. Passmore, F. Oppedisano, J. A. Carnie, and J. R. Carapetis. 2007. The epidemiology of invasive group A streptococcal disease in Victoria, Australia. Med. J. Aust. 186565-569. [DOI] [PubMed] [Google Scholar]
- 29.O'Loughlin, R. E., A. Roberson, P. R. Cieslak, R. Lynfield, K. Gershman, A. Craig, B. A. Albanese, M. M. Farley, N. L. Barrett, N. L. Spina, B. Beall, L. H. Harrison, A. Reingold, and C. Van Beneden. 2007. The epidemiology of invasive group A streptococcal infection and potential vaccine implications: United States, 2000-2004. Clin. Infect. Dis. 45853-862. [DOI] [PubMed] [Google Scholar]
- 30.Passaro, D. J., D. S. Smith, E. C. Hett, A. L. Reingold, P. Daily, C. A. van Beneden, and D. J. Vugia. 2002. Invasive group A streptococcal infections in the San Francisco Bay area, 1989-99. Epidemiol. Infect. 129471-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raymond, J., L. Schlegel, F. Garnier, and A. Bouvet. 2005. Molecular characterization of Streptococcus pyogenes isolates to investigate an outbreak of puerperal sepsis. Infect. Control Hosp. Epidemiol. 26455-461. [DOI] [PubMed] [Google Scholar]
- 32.Schalén, C. 2002. European surveillance of severe group A streptococcal disease. Eurosurveillance. http://www.eurosurveillance.org/ew/2002/020829.asp.
- 33.Smith, A., T. Lamagni, I. Oliver, A. Efstratiou, R. George, and J. Stuart. 2005. Invasive group A streptococcal disease: should close contacts routinely receive antibiotic prophylaxis? Lancet Infect. Dis. 5494-500. [DOI] [PubMed] [Google Scholar]
- 34.Stevens, D. L. 1992. Invasive group A streptococcus infections. Clin. Infect. Dis. 142-11. [DOI] [PubMed] [Google Scholar]
- 35.Stevens, D. L. 1995. Streptococcal toxic-shock syndrome: spectrum of disease, pathogenesis, and new concepts in treatment. Emerg. Infect. Dis. 169-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stevens, D. L. 1999. The flesh-eating bacterium: what's next? J. Infect. Dis. 179(Suppl. 2)S366-S374. [DOI] [PubMed] [Google Scholar]
- 37.Stevens, D. L., M. H. Tanner, J. Winship, R. Swarts, K. M. Ries, P. M. Schlievert, and E. Kaplan. 1989. Severe group A streptococcal infections associated with a toxic shock-like syndrome and scarlet fever toxin A. N. Engl. J. Med. 3211-7. [DOI] [PubMed] [Google Scholar]
- 38.Strakova, L., J. Motlova, P. Urbaskova, and P. Krizova. 2004. Surveillance of serious diseases caused by group A streptococci in the Czech Republic in 2003—the Strep-EURO project. Epidemiol. Mikrobiol. Imunol. 53106-111. [PubMed] [Google Scholar]
- 39.Strömberg, A., V. Romanus, and L. G. Burman. 1991. Outbreak of group A streptococcal bacteremia in Sweden: an epidemiologic and clinical study. J. Infect. Dis. 164595-598. [DOI] [PubMed] [Google Scholar]
- 40.Technical Committee of Nosocomial Infections and Infections Related to Healthcare. 2006. Guidelines for the prevention and the investigation of Streptococcus pyogenes hospital-associated infections. Health Public Council of France. Department of Health, Paris, France. http://www.sante.gouv.fr/htm/dossiers/nosoco/rapports_guides/guide_streptococcus.pdf. (In French.)
- 41.Thigpen, M. C., D. M. Thomas, D. Gloss, S. Y. Park, A. J. Khan, V. L. Fogelman, B. Beall, C. A. van Beneden, R. L. Todd, and C. M. Greene. 2007. Nursing home outbreak of invasive group a streptococcal infections caused by 2 distinct strains. Infect. Control Hosp. Epidemiol. 2868-74. [DOI] [PubMed] [Google Scholar]
- 42.Tyrrell, G. J., M. Lovgren, B. Kress, and K. Grimsrud. 2005. Invasive group A streptococcal disease in Alberta, Canada (2000 to 2002). J. Clin. Microbiol. 431678-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vlaminckx, B. J., W. van Pelt, L. M. Schouls, A. van Silfhout, E. M. Mascini, C. P. Elzenaar, T. Fernandes, A. Bosman, and J. F. Schellekens. 2005. Long-term surveillance of invasive group A streptococcal disease in The Netherlands, 1994-2003. Clin. Microbiol. Infect. 11226-231. [DOI] [PubMed] [Google Scholar]
- 44.WHO Regional Office for Europe. 2007. European health for all database. WHO Regional Office for Europe, Copenhagen, Denmark. http://data.euro.who.int/hfadb/. Accessed 8 August 2007.
- 45.Working Group on Severe Streptococcal Infections. 1993. Defining the group A streptococcal toxic shock syndrome. Rationale and consensus definition. JAMA 269390-391. [PubMed] [Google Scholar]