Abstract
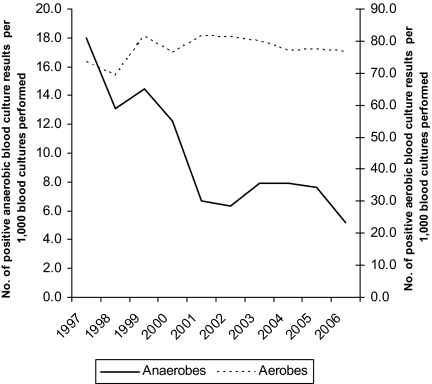
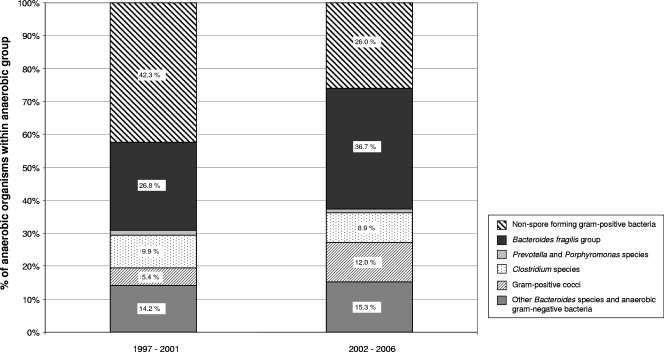
The number of positive anaerobic blood culture results per 1,000 blood cultures performed decreased from 12.6 in the period from 1997 to 2001 to 7.0 in the period from 2002 to 2006 (P < 0.001), as did the proportion of isolated anaerobic organisms compared to the number of all organisms isolated from blood cultures (7.6% to 4.3% [P < 0.001]), while positive aerobic cultures remained stable. In contrast, the proportion of Bacteroides fragilis group members and gram-positive cocci within the anaerobic group increased (26.8% to 36.7% [P = 0.004] and 5.4% to 12% [P < 0.001], respectively). The number of patients with anaerobic bacteremia decreased from 122 patients in 1997 to 69 in 2006.
Anaerobic organisms account for about 4% of bacteremias (range, 0.5% to 9%) depending on geographic location, hospital patient demographics, and patient age (5).
From 1974 to 1988, the incidence of anaerobic bacteremia at the Mayo Clinic (Rochester, MN) decreased by 45% (3). Recently, a study from the same institution indicated the reemergence of anaerobic bacteremia from 1993 to 2004 (7). In contrast, a report from a U.S. community hospital provided no evidence for an increase (1). Therefore, we examined the occurrence of anaerobic and aerobic bacteremias at the University Hospital Basel (UHBS), Basel, Switzerland, and analyzed the proportions of six important groups of anaerobes in relation to 1,000 blood cultures as well as in relation to positive aerobic blood culture results over a 10-year period.
The UHBS is a 680-bed tertiary care center in Switzerland with 27,000 inpatients and 167,000 outpatients per year. It provides all medical services for adults and is one of the major centers for hematopoietic stem cell transplants in Switzerland (9). We retrospectively analyzed blood culture data for a 10-year period between 1997 and 2006 at UHBS. During the entire study period, the same blood culture system (BacT/ALERT; bioMérieux, Hazelwood, MO) and the same pair of aerobic/anaerobic bottles (BacT/ALERT FA/FN; bioMérieux) were used according to the manufacturer's instructions and incubated for 6 days. Since clinical data were not available for the entire study period, determination of sepsis versus contaminant was not possible for the isolates. Bacterial identification was performed according to the Wadsworth-KTL anaerobic bacteriology manual (6). Anaerobic organisms were categorized into six groups (Bacteroides fragilis group, Clostridium spp., gram-positive cocci, non-spore-forming gram-positive bacteria, Prevotella/Porphyromonas spp., other Bacteroides spp., and anaerobic gram-negative bacteria) as previously published (7). The rates of bacteremia during two time periods were compared using an incidence rate calculation (Stata 9.2; College Station, TX).
A total of 114,338 blood cultures were submitted to the laboratory between 1997 and 2006. From those, 1,084 (0.95%) anaerobic organisms were isolated from blood cultures. The total number of blood cultures steadily increased over the 10-year period (from 9,212 blood cultures in 1997 to 13,504 in 2006), whereas the number of isolated anaerobic organisms decreased between 1997 and 2001 (from 166 [1.8%] anaerobic isolates in 1997 to 70 [0.5%] in 2006). The number of positive anaerobic blood culture results (with one or more anaerobic organisms) per 1,000 blood cultures performed decreased from 12.6 between 1997 and 2001 to 7.0 between 2002 and 2006 (P < 0.001) (Fig. 1). The decrease was also observed when gram-positive anaerobes were excluded (7.3 versus 5.2 [P < 0.001]). At the same time, positive aerobic blood culture results per 1,000 blood cultures performed remained stable (76.7 versus 78.4 [P = 0.16]). Although fungemia increased significantly from 2.7 to 4.6 fungal isolates per 1,000 blood cultures from the 1997-to-2001 period to the 2002-to-2006 period (P < 0.001), the rate never exceeded that of anaerobic bacteremia. During the study period, the proportion of isolated anaerobic organisms compared to the number of all organisms isolated from blood cultures declined from 7.6% between 1997 and 2001 to 4.3 between 2002 and 2006 (P < 0.001); the proportion steadily fell from 10.9% in 1997 to 3.3% in 2006. Similar to the decrease in the number of anaerobic isolates, the number of patients with anaerobic bacteremia decreased from 122 patients in 1997 to 69 patients in 2006. Looking at the proportions of anaerobic organisms isolated from blood cultures, the percentage of B. fragilis group members and gram-positive cocci within the anaerobe group increased from 26.8% to 36.7% (P = 0.004) and from 5.4% to 12% (P < 0.001), respectively (Fig. 2). In terms of the rate per 1,000 blood cultures performed, these two anaerobic groups leveled off or decreased (from 3.4 during the 1997-to-2001 period to 2.6 during the 2002-to-2006 period for B. fragilis group members and from 0.7 to 0.8 for gram-positive cocci). On the other hand, the percentage of non-spore-forming gram-positive anaerobes fell, while the percentages of Prevotella spp., Porphyromonas spp., Clostridium spp., and gram-negative anaerobes other than B. fragilis remained unchanged (Fig. 2).
FIG. 1.
Positive anaerobic and aerobic blood culture results per 1,000 blood cultures, per year, between 1997 and 2006 at UHBS, Basel, Switzerland.
FIG. 2.
Proportions of the major groups of anaerobic bacteria among the total number of anaerobes isolated during 1997 to 2001 and during 2002 to 2006.
The observed decrease in anaerobic bacteremia challenges a previous report suggesting an increase in anaerobic bacteremia (7). The authors postulated that an increased number of patients with complex underlying diseases might explain the reemergence of anaerobes that were observed in a tertiary-care center but had not been observed in a community hospital in New York (1, 7). However, our center more than doubled the number of transplantations during the study period and still observed a decrease in anaerobes (9). Complete clinical and demographic data from our patients with anaerobes were not available, but underlying diseases likely increased over the study period, as observed by Lassmann et al (7). Similar to the decrease in the number of anaerobic isolates, the number of patients with anaerobic bacteremia decreased between 1997 and 2006. The described trend in anaerobic bacteremias was seen both in the decreasing number of positive anaerobic blood culture results per 1,000 blood cultures and in the decreasing proportion of anaerobic organisms compared to the number of all organisms causing bacteremias. It is also noteworthy that the absolute number of positive anaerobic blood culture results per 1,000 blood cultures performed at our institution is higher than previously published (7). Similarly, however, the proportions of B. fragilis group and gram-positive cocci within the anaerobe group increased (7). Gram-positive anaerobic cocci are associated with malignancies (2, 7) and B. fragilis group members with a more severe clinical outcome (8, 10). Importantly, B. fragilis group members are known to be more resistant to antibiotics than are other anaerobic organisms (8, 11). The increased number of patients with severe immunosuppression and treatment for malignancies at our institution may explain the increase found for this group of anaerobes. In addition, new species associated with underlying diseases have emerged (4).
There are probably multiple reasons behind the changes in anaerobic bacteremias, possibly explaining the different observations in other studies (1, 7). The reemergence of anaerobic bacteremias may depend on the geographical region, the antibiotic use policies of the institution, and the case mix of the study population, including the frequencies of patient comorbidities and immunosuppression (1, 7). For now, routine anaerobic blood cultures should not be abandoned. Further studies focusing on the clinical and demographic background of patients are needed to evaluate the trends seen for anaerobic bacteremias.
Acknowledgments
We are indebted to the microbiology laboratory and the entire infection control team at the UHBS, Basel, Switzerland.
Footnotes
Published ahead of print on 7 May 2008.
REFERENCES
- 1.Bengualid, V., H. Singh, V. Singh, and J. Berger. 2008. An increase in the incidence of anaerobic bacteremia: true for tertiary care referral centers but not for community hospitals? Clin. Infect. Dis. 46323-324. [DOI] [PubMed] [Google Scholar]
- 2.Brook, I., and E. H. Frazier. 1998. Aerobic and anaerobic infection associated with malignancy. Support. Care Cancer 6125-131. [DOI] [PubMed] [Google Scholar]
- 3.Dorsher, C. W., J. E. Rosenblatt, W. R. Wilson, and D. M. Ilstrup. 1991. Anaerobic bacteremia: decreasing rate over a 15-year period. Rev. Infect. Dis. 13633-636. [DOI] [PubMed] [Google Scholar]
- 4.Fenner, L., V. Roux, P. Ananian, and D. Raoult. 2007. Alistipes finegoldii in blood cultures from colon cancer patients. Emerg. Infect. Dis. 131260-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finegold, S. M. 1979. Taxonomy, enzymes, and clinical relevance of anaerobic bacteria. Rev. Infect. Dis. 1248-253. [DOI] [PubMed] [Google Scholar]
- 6.Jousimies-Somer, H., P. Summanen, D. M. Citron, J. Barry, H. M. Wexler, and S. Finegold. 2002. Wadsworth-KTL anaerobic bacteriology manual, 6th ed. Star Publishing Company, Belmont, CA.
- 7.Lassmann, B., D. R. Gustafson, C. M. Wood, and J. E. Rosenblatt. 2007. Reemergence of anaerobic bacteremia. Clin. Infect. Dis. 44895-900. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen, M. H., V. L. Yu, A. J. Morris, L. McDermott, M. W. Wagener, L. Harrell, and D. R. Snydman. 2000. Antimicrobial resistance and clinical outcome of Bacteroides bacteremia: findings of a multicenter prospective observational trial. Clin. Infect. Dis. 30870-876. [DOI] [PubMed] [Google Scholar]
- 9.Passweg, J., H. Baldomero, B. Chapuis, K. Leibundgut, U. Schanz, and A. Gratwohl. 2006. Haematopoietic stem cell transplantation in Switzerland. Report from the Swiss Transplant Working Group Blood and Marrow Transplantation (STABMT) Registry 1997-2003. Swiss Med. Wkly. 13650-58. [DOI] [PubMed] [Google Scholar]
- 10.Redondo, M. C., M. D. Arbo, J. Grindlinger, and D. R. Snydman. 1995. Attributable mortality of bacteremia associated with the Bacteroides fragilis group. Clin. Infect. Dis. 201492-1496. [DOI] [PubMed] [Google Scholar]
- 11.Wybo, I., D. Pierard, I. Verschraegen, M. Reynders, K. Vandoorslaer, G. Claeys, M. Delmee, Y. Glupczynski, B. Gordts, M. Ieven, P. Melin, M. Struelens, J. Verhaegen, and S. Lauwers. 2007. Third Belgian multicentre survey of antibiotic susceptibility of anaerobic bacteria. J. Antimicrob. Chemother. 59132-139. [DOI] [PubMed] [Google Scholar]