Abstract
Ebola virus infects a wide variety of adherent cell types, while nonadherent cells are found to be refractory. To explore this correlation, we compared the ability of pairs of related adherent and nonadherent cells to bind a recombinant Ebola virus receptor binding domain (EboV RBD) and to be infected with Ebola virus glycoprotein (GP)-pseudotyped particles. Both human 293F and THP-1 cells can be propagated as adherent or nonadherent cultures, and in both cases adherent cells were found to be significantly more susceptible to both EboV RBD binding and GP-pseudotyped virus infection than their nonadherent counterparts. Furthermore, with 293F cells the acquisition of EboV RBD binding paralleled cell spreading and did not require new mRNA or protein synthesis.
The filovirus Ebola causes severe hemorrhagic fever in humans and nonhuman primates, with mortality rates reaching 90% (8, 15). Ebola virus encodes a single glycoprotein (GP) that is both necessary and sufficient for virus binding to and penetration of host cells. Ebola virus GP confers broad cellular tropism and binds to an as-yet unidentified proteinaceous host cell receptor (3, 9, 11, 18, 20, 22, 23). To date, a wide array of adherent cell types, including fibroblasts and epithelial cells, have been shown to be susceptible to Ebola virus GP-mediated infection (14, 20, 22, 23). These adherent cells are anchorage dependent, requiring adhesion to extracellular matrix components in order to survive and proliferate, with these processes being mediated at least in part by integrin signaling through extracellular signal-regulated kinase, phosphatidylinositol 3-kinase, and Rac (17). Conversely, the cell types that have been shown to be refractory to Ebola virus infection are human B and T lymphocytes, which exhibit anchorage-independent growth and can survive and proliferate as nonadherent suspension cultures.
A receptor binding domain of Ebola virus GP (EboV RBD) has been defined (3, 11, 12). Human 293T and African green monkey Vero cells, both of which are adherent cells that are permissive for Ebola virus GP-mediated infection, were reported to bind an EboV RBD-Fc construct, whereas Jurkat T cells bound only minimal levels of the EboV RBD (11). These observations suggested that anchorage-dependent cells may, as a general rule, be more susceptible to Ebola virus GP-mediated RBD binding and infection than cells capable of anchorage-independent growth.
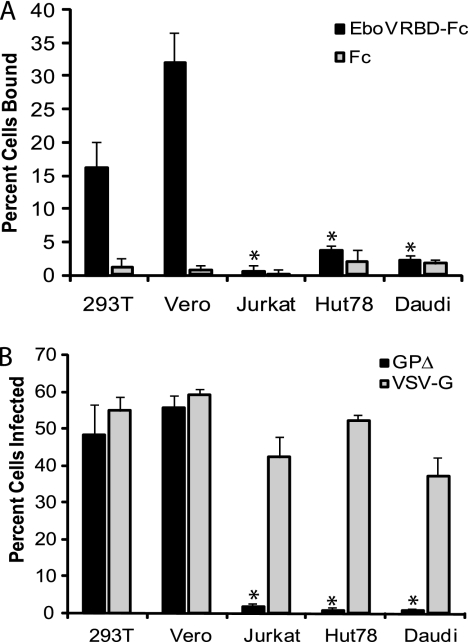
To begin to test this hypothesis, we first confirmed and extended basic observations on EboV RBD binding and GP-mediated infection. As seen in Fig. 1A, 293T and Vero cells (adherent) bind significant levels of EboV RBD (16 and 31% of cells, respectively). We examined the infection status of these cells using vesicular stomatis virus (VSV)-pseudotyped particles bearing a mucin domain-deleted Ebola virus GP (GPΔ) and encoding green fluorescent protein (GFP) (VSV-GPΔ) (16). As seen in Fig. 1B, 293T and Vero cells were well infected by VSV-GPΔ (48 and 56% of cells, respectively). In contrast, and as previously shown (11), Jurkat T cells (nonadherent) bind only low levels of the RBD (1% of cells) and are minimally susceptible to VSV-GPΔ (2% of cells) (Fig. 1). In addition to Jurkat cells, two other (nonadherent) lymphocyte cell lines, Hut78 and Daudi, bound minimal amounts of EboV RBD (4 and 1.6% of cells, respectively) (Fig. 1A) and were poorly infected by VSV-GPΔ (<2% of cells) (Fig. 1B). All cell lines were well infected with VSV-pseudotyped particles that bore the native VSV glycoprotein (VSV-G).
FIG. 1.
EboV RBD binding to, and pseudotype infection of, adherent 293T and Vero cells compared to those of B and T lymphocytes. (A) RBD-Fc binding assays were conducted essentially as described by Kuhn et al. (11), using a construct with similar binding properties (D. Dube, S. E. Delos, and J. M. White, unpublished data). Briefly, EboV RBD or control rabbit Fc (200 nM) was added to 5 × 105 cells for 1.5 h at 4°C. The cells were washed three times with 3% bovine serum albumin-phosphate-buffered saline with Ca2+ and Mg2+, and Alexa Fluor 488-conjugated Protein A (Invitrogen) was added at a dilution of 1:250 for 45 min at 4°C. The cells then were washed twice and fixed with 4% paraformaldehyde. The cell surface binding of the EboV RBD was determined by flow cytometry. The percentage of cells that were positive for binding is presented. (B) Infection assays were performed as described by Schornberg et al. (16). Indicated cells were challenged for 18 h with VSV-GPΔ or VSV-G at a multiplicity of infection of 1 and fixed, and the percentage of GFP-positive cells was determined by flow cytometry. Results shown are the averages from three or more experiments, and error bars represent standard deviations. Asterisks indicate statistically significant differences from 293T cell data (P < 0.01).
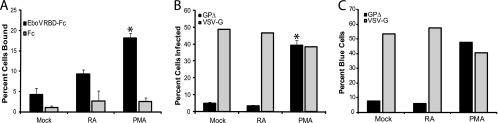
To test the hypothesis that there is a general block to Ebola virus entry into nonadherent cell lines, we compared the ability of two pairs of highly related cells, grown either in suspension or as adherent cells, to bind EboV RBD and to be infected with VSV-GPΔ. THP-1 cells are a human monocyte cell line that can be differentiated into macrophage-like cells with phorbol 12-myristate 13-acetate (PMA) or retinoic acid (RA) (7). Untreated (and mock-treated) THP-1 cells grow in suspension. RA-treated cells remain in suspension but express the macrophage differentiation markers CD11a and CD11b; CD11b is restricted to mature myeloid cells. PMA-treated cells express CD11a and CD11b, but in contrast to mock-treated or RA-treated THP-1 cells, they become adherent (10, 13). Mock-treated THP-1 cells displayed a low level of EboV RBD binding (4.7% of cells). RA-treated cells showed somewhat increased binding (9.3% of cells), but the difference was not statistically significant. In contrast, PMA-treated THP-1 cells bound significantly higher levels of EboV RBD (19% of cells) (Fig. 2A). We next examined these cells for susceptibility to VSV-GPΔ. Both mock- and RA-treated THP-1 cells (which remain in suspension) were poorly infected with VSV-GPΔ (5 and 4% of cells, respectively), whereas PMA-treated THP-1 cells (which are adherent) were well infected (39% of cells) (Fig. 2B). There was no significant difference in the susceptibility of these cells to infection with VSV-G. A viral entry assay that used human immunodeficiency virus pseudovirions harboring β-lactamase and bearing Ebola virus GPΔ or VSV-G supported these infection results; a significant increase of Ebola virus GP-mediated viral entry was seen in PMA-treated THP-1 cells compared to that of mock- or RA-treated cells (Fig. 2C).
FIG. 2.
EboV RBD binding to, and pseudotype infection of, RA- and PMA-treated THP-1 cells. (A) THP-1 cells were mock treated or treated with 0.1 μM RA or PMA for 24 h. Cells then were assayed for EboV RBD binding as described in the legend to Fig. 1A. (B) THP-1 cells were treated as described for panel A (in a 96-well dish) and then challenged with VSV-GPΔ or VSV-G (multiplicity of infection [MOI] of 2), incubated, and analyzed as described in the legend to Fig. 1B. Results shown in panel A and those for VSV-GPΔ in panel B are the averages from three or more experiments and error bars represent standard deviations, with asterisks indicating statistically significant differences from mock-treated THP-1 cell data (P < 0.02). The data for VSV-G shown in panel B are the averages from duplicate samples from one experiment; similar results were seen at a lower MOI. (C) Mock-, RA-, and PMA-treated THP-1 cells were infected with β-lactamase containing human immunodeficiency virus type 1 virions bearing Ebola virus GPΔ or VSV-G and then loaded with the β-lactamase substrate CCF2/AM. Cells loaded only with CCF2/AM served as a negative control. The extent of CCF2/AM cleavage by the virus-introduced cytoplasmic β-lactamase, which was detected by the change in the dye emission from green to blue, was evaluated using a BD LSR II cell analyzer equipped with a violet laser (407 nm) and appropriate filters for the blue (HQ 450/50; Chroma Technology) and green (HQ 530/30; Chroma Technology) emissions. The averages from duplicate samples from one representative of two experiments are shown. Similar results were seen at a lower MOI.
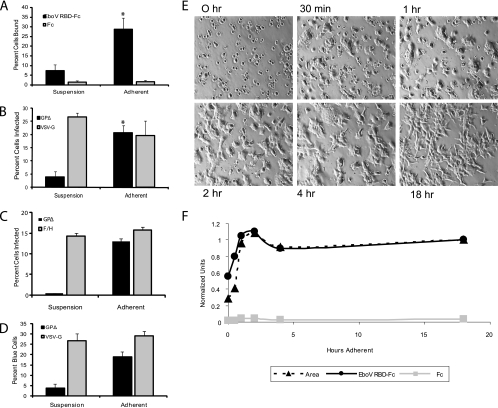
293F cells are derivatives of 293 cells. They remain in suspension if grown on a shaking platform but will become adherent and spread if left in static culture (5, 6). We compared the EboV RBD binding ability and susceptibility to VSV-GPΔ infection of 293F cells in suspension to those of ones allowed to adhere for 18 h. As seen in Fig. 3A, there was an approximately fourfold increase in EboV RBD binding to adherent 293F cells compared to that of cells kept in suspension (29 and 7% of cells, respectively). Correspondingly, suspension 293F cells were poorly infected (4%), while those allowed to adhere were well infected (20%), representing a fivefold increase in susceptibility (Fig. 3B). This increase in the susceptibility of the adherent cells was not seen with VSV particles bearing either VSV-G or measles virus F and H (Fig. 3B and C). A similar increase in susceptibility to GP-mediated viral entry was seen using the β-lactamase entry assay (Fig. 3D).
FIG. 3.
EboV RBD binding to, and pseudotype infection of, adherent and suspension 293F cells. (A) 293F cells were maintained in suspension on a rotating platform or allowed to adhere without being shaken for 18 h in the same CO2 incubator. Cells then were assayed for EboV RBD binding as described in the legend to Fig. 1A. (B) 293F cells were treated as described for panel A, challenged with VSV-GPΔ or VSV-G at a multiplicity of infection (MOI) of 2 for 18 h, and scored for infection by flow cytometry. Results shown in panels A and B are the averages from three or more experiments and error bars represent standard deviations, with asterisks indicating statistically significant differences from the suspension 293F cell data (P < 0.015). (C) 293F cells were treated as described for panel A, challenged with VSV-GPΔ or VSV-measles virus F/H at an MOI of 2 for 18 h, and scored for infection by flow cytometry. The averages from duplicate samples from one representative of two experiments are shown. (D) 293F cells were treated as described for panel A and assayed as described in the legend to Fig. 2C, using Ebola virus GPΔ or VSV-G bearing human immunodeficiency virus pseudoparticles harboring β-lactamase. The average results from duplicate samples are shown. (E) 293F cells were left in suspension or allowed to adhere. Cells were photographed at the indicated times using a Spot Insight Color camera attached to a Nikon Diaphot microscope. (F) The cells shown in panel E were examined for cell spreading (▴) and EboV RBD binding (•). Cell spreading was determined by a blind analysis of micrographs such as those shown in panel E by using EZ-C1 Freeviewer 3.0 software from Nikon. The perimeter of 10 cells per field (for 3 or more fields) was outlined to generate cell area data. Cell areas for each time point were averaged and normalized to the area of cells that were plated for 18 h. The binding of the EboV RBD (•) and Fc control (▪) were assayed as described in the legend to Fig. 1B and normalized to the values for EboV RBD binding to cells that were allowed to adhere for 18 h. The data in panels E and F are from one of three experiments that yielded virtually identical results.
To further assess if EboV RBD binding correlated with the cell adhesion phenotype, we examined the ability of 293F cells to bind EboV RBD after various lengths of time in static culture. At time zero, suspension 293F cells displayed a low average cell area (a measure of cell adhesion and spreading) and low EboV RBD binding. However, within 2 h in static culture, both the average cell area and EboV RBD binding reached maximal values (Fig. 3E and F). For reasons that we do not understand, we saw a small decrease in cell area and RBD binding at the 4-h time point. Nevertheless, these results clearly demonstrate that, at least in the case of 293F cells, the ability to bind EboV RBD is acquired in parallel with cell spreading.
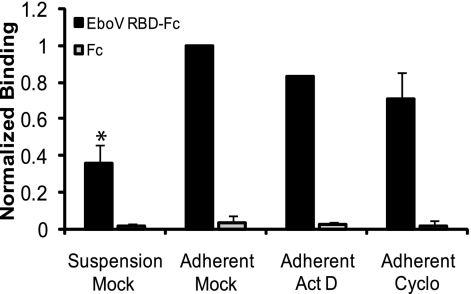
To examine the mechanism by which cell adhesion promotes the binding of the EboV RBD, we tested the effects of actinomycin D, an inhibitor of transcription, and cycloheximide, an inhibitor of protein translation (4, 6). Neither inhibitor significantly affected the binding of the EboV RBD to adherent 293F cells (Fig. 4). This suggests that the increase in EboV RBD binding that accompanies cell adhesion and spreading does not require the synthesis of new mRNA or protein.
FIG. 4.
Effects of actinomycin D and cycloheximide on EboV RBD binding to 293F cells. 293F cells maintained on a shaking platform were pretreated with 1 μM actinomycin D (Act D), 10 μM cycloheximide (Cyclo), or vehicle (0.1% dimethylsulfoxide; mock) for 2 h. Cells then were removed from the shaker and allowed to adhere for an additional 2 h in the continued presence of the indicated inhibitor (Adherent Act D or Adherent Cyclo). Mock-treated cells either were allowed to adhere (Adherent Mock) or were kept on the shaker (Suspension Mock) for an additional 2 h. The cells then were examined for EboV RBD binding as described in the legend to Fig. 1A, and the data were normalized to those for EboV RBD binding to mock-treated adherent cells. Results shown are the averages from five determinations from two experiments, and error bars represent standard deviations. The asterisk indicates a statistically significant difference from mock-treated adherent 293F cell data (P < 0.015). Parallel cells were transfected with a GFP expression plasmid and treated with 1 μM Act D, 10 μM cycloheximide, or 0.1% dimethylsulfoxide (mock). Whereas GFP was robustly expressed in the mock-treated samples, no GFP was detected in samples treated with Act D or cycloheximide.
In summary, we have shown that when two nonadherent human cell lines (THP-1 and 293F) are treated so as to render them adherent, they concomitantly acquire the abilities to bind the EboV RBD and to be infected with Ebola virus GP-pseudotyped viral particles. Previous work suggested that circulating monocytes can be infected by Ebola virus (19). However, infection occurred in concert with the activation and aggregation of the cells (cell-cell adhesion), and it is unclear whether infection occurred in isolated nonadherent monocytes. Thus, the inability of nonadherent cell lines (e.g., cells in addition to lymphocytes) to be infected by Ebola virus GP pseudotypes may be due, at least in part, to a deficiency in binding the RBD of the Ebola virus GP. Moreover, our findings suggest that the acquisition of RBD binding and Ebola virus GP pseudotype infection occur in parallel with cell adhesion and spreading, and that these properties arise due to posttranslational events.
Several possible explanations can account for these observations. For one, an Ebola virus receptor or binding cofactor(s) already present in the cell may relocate from the cell interior to the cell surface upon cell adhesion. Such relocation would allow virus binding and infection. Precedence for protein relocation in concert with cell adhesion has been shown for components of lipid raft domains (1), which have been proposed to be important for Ebola virus binding and entry (2). Our initial studies suggest that there are comparable levels of the lipid raft marker GM1 on the surfaces of adherent and nonadherent 293F cells (data not shown). It remains possible, however, that other raft or nonraft components involved in facilitating Ebola virus GP binding are inserted into the plasma membrane upon cell adhesion. Alternatively, cell adhesion may promote a conformational change or posttranslational modification in a cell surface protein(s) that confers the ability to bind the RBD of the Ebola virus GP. With respect to the correlation between cell adhesion and EboV RBD binding and infection, it is interesting that we (K. L. Schornberg, A. H. Bouton, and J. M. White, unpublished data) and others (21) have found that β1 integrins promote Ebola virus GP-mediated entry, since β1 integrins are central to cell adhesion and signaling for anchorage-dependent cell growth. Studies are in progress to determine how cell adhesion and spreading promote Ebola virus GP-mediated binding and infection.
Acknowledgments
Work in our laboratories was supported by grants from the NIH (AI22470 and U54AI57168 to J.M.W.; AI050733 to A.H.B.; and AI057168 to C.C.B.). D.D. and K.L.S. were supported in part by training grants 5T32 AI055432 and 5T32 AI0704627 to the University of Virginia.
We thank Edward Park for excellent technical assistance, Kirsten Kabsch for the production of the measles virus F and H pseudovirions, and Yusuke Yanagi for supplying the measles virus F and H cDNAs.
Footnotes
Published ahead of print on 30 April 2008.
REFERENCES
- 1.Balasubramanian, N., D. W. Scott, J. D. Castle, J. E. Casanova, and M. A. Schwartz. 2007. Arf6 and microtubules in adhesion-dependent trafficking of lipid rafts. Nat. Cell Biol. 91381-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bavari, S., C. M. Bosio, E. Wiegand, G. Ruthel, A. B. Will, T. W. Geisbert, M. Hevey, C. Schmaljohn, A. Schmaljohn, and M. J. Aman. 2002. Lipid raft microdomains: a gateway for compartmentalized trafficking of Ebola and Marburg viruses. J. Exp. Med. 195593-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brindley, M. A., L. Hughes, A. Ruiz, P. B. McCray, Jr., A. Sanchez, D. A. Sanders, and W. Maury. 2007. Ebola virus glycoprotein 1: identification of residues important for binding and postbinding events. J. Virol. 817702-7709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chesnokov, V. N., and N. P. Mertvetsov. 1990. The effect of translation inhibitor cycloheximide on expression of mammalian genes. Biokhimiia 551276-1278. [PubMed] [Google Scholar]
- 5.Graham, F. L., J. Smiley, W. C. Russell, and R. Nairn. 1977. Characteristics of a human cell line transformed by DNA from human adenovirus type 5. J. Gen. Virol. 3659-74. [DOI] [PubMed] [Google Scholar]
- 6.Harrison, T., F. Graham, and J. Williams. 1977. Host-range mutants of adenovirus type 5 defective for growth in HeLa cells. Virology 77319-329. [DOI] [PubMed] [Google Scholar]
- 7.Hickstein, D. D., D. M. Baker, K. A. Gollahon, and A. L. Back. 1992. Identification of the promoter of the myelomonocytic leukocyte integrin CD11b. Proc. Natl. Acad. Sci. USA 892105-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoenen, T., A. Groseth, D. Falzarano, and H. Feldmann. 2006. Ebola virus: unravelling pathogenesis to combat a deadly disease. Trends Mol. Med. 12206-215. [DOI] [PubMed] [Google Scholar]
- 9.Ito, H., S. Watanabe, A. Takada, and Y. Kawaoka. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J. Virol. 751576-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kohro, T., T. Tanaka, T. Murakami, Y. Wada, H. Aburatani, T. Hamakubo, and T. Kodama. 2004. A comparison of differences in the gene expression profiles of phorbol 12-myristate 13-acetate differentiated THP-1 cells and human monocyte-derived macrophage. J. Atheroscler. Thromb. 1188-97. [DOI] [PubMed] [Google Scholar]
- 11.Kuhn, J. H., S. R. Radoshitzky, A. C. Guth, K. L. Warfield, W. Li, M. J. Vincent, J. S. Towner, S. T. Nichol, S. Bavari, H. Choe, M. J. Aman, and M. Farzan. 2006. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J. Biol. Chem. 28115951-15958. [DOI] [PubMed] [Google Scholar]
- 12.Manicassamy, B., J. Wang, H. Jiang, and L. Rong. 2005. Comprehensive analysis of Ebola virus GP1 in viral entry. J. Virol. 794793-4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matikainen, S., and M. Hurme. 1994. Comparison of retinoic acid and phorbol myristate acetate as inducers of monocytic differentiation. Int. J. Cancer 5798-103. [DOI] [PubMed] [Google Scholar]
- 14.Peters, C. J., P. B. Jahrling, T. G. Ksiazek, E. D. Johnson, and H. W. Lupton. 1992. Filovirus contamination of cell cultures. Dev. Biol. Stand. 76267-274. [PubMed] [Google Scholar]
- 15.Sanchez, A., T. W. Geisbert, and H. Feldmann. 2007. Filoviridae: Marburg and Ebola viruses, p. 1409-1448. In David M. Knipe, Peter M. Howley, D. E. Griffin, R. A. Lamb, and M. A. Martin (ed.), Fields Virology, 5th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia, PA.
- 16.Schornberg, K., S. Matsuyama, K. Kabsch, S. Delos, A. Bouton, and J. White. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J. Virol. 804174-4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz, M. A. 1997. Integrins, oncogenes, and anchorage independence. J. Cell Biol. 139575-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shimojima, M., A. Takada, H. Ebihara, G. Neumann, K. Fujioka, T. Irimura, S. Jones, H. Feldmann, and Y. Kawaoka. 2006. Tyro3 family mediated cell entry of Ebola and Marburg viruses. J. Virol. 8010109-10116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ströher, U., E. West, H. Bugany, H. D. Klenk, H. J. Schnittler, and H. Feldmann. 2001. Infection and activation of monocytes by Marburg and Ebola viruses. J. Virol. 7511025-11033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takada, A., C. Robison, H. Goto, A. Sanchez, K. G. Murti, M. A. Whitt, and Y. Kawaoka. 1997. A system for functional analysis of Ebola virus glycoprotein. Proc. Natl. Acad. Sci. USA 9414764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takada, A., S. Watanabe, H. Ito, K. Okazaki, H. Kida, and Y. Kawaoka. 2000. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology 27820-26. [DOI] [PubMed] [Google Scholar]
- 22.Wool-Lewis, R. J., and P. Bates. 1998. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J. Virol. 723155-3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang, Z., R. Delgado, L. Xu, R. F. Todd, E. G. Nabel, A. Sanchez, and G. J. Nabel. 1998. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science 2791034-1037. [DOI] [PubMed] [Google Scholar]