Abstract
Medication errors in critical care are frequent, serious, and predictable. Critically ill patients are prescribed twice as many medications as patients outside of the intensive care unit (ICU) and nearly all will suffer a potentially life-threatening error at some point during their stay. The aim of this article is to provide a basic review of medication errors in the ICU, identify risk factors for medication errors, and suggest strategies to prevent errors and manage their consequences.
Introduction
Health care delivery is not infallible. Errors are common in most health care systems and are reported to be the seventh most common cause of death overall [1]. The 1999 Institute of Medicine (IOM) report, To Err is Human: Building a Safer Health System, drew public attention to the importance of patient safety [2]. This was followed with considerable interest by the medical community [3]. However, to date, there is little evidence that patient safety has improved [4]. In the intensive care unit (ICU), on average, patients experience 1.7 errors per day [5] and nearly all suffer a potentially life-threatening error at some point during their stay [6]. Medication errors account for 78% of serious medical errors in the ICU [7]. The aim of this article is to provide a basic review of medication errors in the ICU as well as strategies to prevent errors and manage their consequences.
What is a medication error?
Providing a single hospitalized patient with a single dose of a single medication requires correctly executing 80 to 200 individual steps [8]. This hospital medication use process can be categorized into five broad stages: prescription, transcription, preparation, dispensation, and administration [9]. An error can occur at any point in this process. A medication error is any error in the medication process, whether there are adverse consequences or not (Table 1) [10]. Most errors occur during the administration stage (median of 53% of all errors), followed by prescription (17%), preparation (14%), and transcription (11%) [11]. The earlier in the medication process an error occurs, the more likely it is to be intercepted [12]. Administration appears to be particularly vulnerable to error because of a paucity of system checks as most medications are administered by a single nurse [13]. Nurses and pharmacists intercept up to 70% of prescription errors [14]. Preparation errors occur when there is a difference between the ordered amount or concentration of a medication and what is actually prepared and administered. The industry standard for pharmaceutical preparations is a concentration difference of less than 10% [15]. However, approximately two thirds of infusions prepared by nurses are outside industry-accepted standards and 6% contain a greater than twofold concentration error [16]. Transcription errors are usually attributed to handwriting, abbreviation use, unit misinterpretation ('mg' for 'mcg'), and mistakes in reading.
Table 1.
Definitions
| Medical error | The failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim [2]. |
| Medication error | Any error in the medication process, whether there are adverse consequences or not [10]. |
| Adverse drug event | Any injury related to the use of a drug [77]. Not all adverse drug events are caused by medical error, nor do all medication errors result in an adverse drug event [26]. |
| Preventable adverse event | Harm that could be avoided through reasonable planning or proper execution of an action [6]. |
| Near miss | The occurrence of an error that did not result in harm [6]. |
| Slip | A failure to execute an action due to a routine behavior being misdirected [17]. |
| Lapse | A failure to execute an action due to lapse in memory and a routine behavior being omitted [17]. |
| Mistake | A knowledge-based error due to an incorrect thought process or analysis [17]. |
| Error of omission | Failure to perform an appropriate action [6]. |
| Error of commission | Performing an inappropriate action [6]. |
How are medication errors classified?
James Reason developed a well-recognized system for human error classification based on observations from industries that have become highly reliable such as aviation and nuclear power [17]. He states that errors arise for two reasons: active failures and latent conditions.
Active failures are unsafe acts committed by people who are in direct contact with the patient. They take a variety of forms: slips, lapses, and mistakes (Table 1). Slips and lapses are skill-based behavior errors, when a routine behavior is misdirected or omitted. The person has the right idea but performs the wrong execution. For example, forgetting to restart an infusion of heparin postoperatively is a lapse. Restarting the heparin infusion but entering an incorrect infusion rate despite knowing the correct rate is a slip. Mistakes are knowledge-based errors (perception, judgment, inference, and interpretation) and occur due to incorrect thought processes or analyses. For example, prescribing heparin in a patient diagnosed with heparin-induced thrombo-cytopenia is a mistake. Situational factors (fatigue, drugs, alcohol, stress, and multiple activities) can divert attention and increase the risk of active failures.
Latent conditions are resident pathogens within the system. They can affect the rate at which employees execute active failures and the risks associated with active failures. Latent failures occur when individuals make decisions that have unintended consequences in the future [17]. Prevention requires an ongoing tenacious search and corrective actions once latent conditions are identified. For example, institutions that use staffing models that depend on providers to routinely perform clinical duties above and beyond their regular responsibilities paradoxically risk introducing time pressures, fatigue, and low morale into their work force.
Errors can alternatively be classified as errors of omission or errors of commission (Table 1). Errors of omission are defined as failure to perform an appropriate action [6]. On average, patients receive only half of the recommended care they should receive [18]. Errors of commission are defined as performing an inappropriate action [6]. Most studies in the patient safety literature focus on errors of commission such as wrong drug or wrong dose. Problems with effectiveness and access to drug therapy have been studied much less frequently [19].
How common are medication errors?
The reported incidence of medication errors varies widely between clinical settings and patient populations and between studies. Errors appear to occur in approximately 6% of hospital medication use episodes [11]. Among critically ill adults, the rate of medication errors ranges from 1.2 to 947 errors per 1,000 patient ICU days with a median of 106 errors per 1,000 patient ICU days [20]. In children, 100 to 400 prescribing errors have been reported per 1,000 patients [21]. Several factors account for this large variation in reported medication errors. First, the definition of medication error, including both the numerator and denominator selected for rate calculations, is critical. For example, medication errors and adverse drug events (ADEs) are frequently reported as individual events, as a numerator, but with no denominator [6]. Furthermore, selecting an appropriate denominator that reflects exposure to risk can be difficult [6]. Should medication errors be reported per patient, patient day, medication day, or dose administered? Second, the process node (prescription, transcription, and so on) under investigation will influence incidence estimates [20]. Third, the method of reporting medication errors influences rate estimates [22,23]. Spontaneous reporting of medication errors may under-report events [11,22]. Review of the medical records is considered by many experts the benchmark for estimating the extent of errors and adverse events in hospitals but is dependent on accurate documentation [24]. Automation of medical record reviews with computers can be used to improve efficiency and allow for prospective reviews [22]. Direct patient monitoring may be the ultimate reference standard but is dependent on observer expertise and is very labor-intensive [25]. Fourth, the culture of individual ICUs, the number of ICUs participating in error reporting, and the technologies employed can significantly influence error reporting. Medication error trends over time using the same standardized measurement tools are more likely to provide valuable information than periodic cross-sectional surveys.
What are the consequences of medication errors?
Medication errors are an important cause of patient morbidity and mortality [9]. Although only 10% of medication errors result in an ADE, these errors have profound implications for patients, families, and health care providers [13,26,27]. The IOM report highlights that 44,000 to 98,000 patients die each year as a result of medical errors, a large portion of these being medication-related [2]. Approximately one fifth (19%) of medication errors in the ICU are life-threatening and almost half (42%) are of sufficient clinical importance to warrant additional life-sustaining treatments [28]. However, deaths are only the tip of the iceberg. The human and societal burden is even greater with many patients experiencing costly and prolonged hospital stays and some patients never fully recovering to their premorbid status [29,30]. Bates and colleagues [30] estimated that in American hospitals the annual cost of serious medication errors in 1995 was $2.9 million per hospital and that a 17% decrease in incidence would result in $480,000 savings per hospital. Finally, the psychological impact of errors should not be ignored [30]. Errors erode patient, family, and public confidence in health care organizations [31]. Memories of error can haunt providers for many years [32].
What is unique about the ICU and medication errors?
The ICU brings together high-risk patients and interventions in a complex environment (Table 2) [33]. The single strongest predictor of an ADE is patient illness severity [34]. Critically ill patients are prescribed twice as many medications as patients outside of the ICU [35]. Most medications in the ICU are administered as weight-based infusions. These infusions require mathematical calculations and frequently are based on estimated weights increasing the risk of error [20,28]. Multicentered studies by Ridley and colleagues [36] and Calabrese and colleagues [13] identified potassium chloride, heparin, magnesium sulphate, vasoactive drugs, sedatives, and analgesics as the medications with the greatest risk of error. Antibiotics frequently are empirically prescribed in the ICU and errors have potential implications both for individual patients and populations [37,38]. Patients are prescribed these medications in an environment that is stressful, complex, changing, under the stewardship of multiple providers, and frequently managing patients in crisis [20]. It is important to remember that critically ill patients have fewer defenses against adverse events than other patients do. They have limited ability to participate in their medical care and they lack the physiological reserve to tolerate additional injury. Moreover, they are reliant on sophisticated technologies and equipment to deliver essential care and yet relatively little is known about medical equipment failures and the associated safety risks. Finally, lack of continuity of care at discharge from the ICU is a well-known feature putting the patient at risk for errors and highlights the importance of communication with the future caregivers [39].
Table 2.
Risk factors for medication errors in the intensive care unit
| Factors | Specific risk factors |
| Patient | Severity of illness |
| Strongest predictor of ADE [25,34] | |
| ICU patients more likely to experience ADE than patients in other units [35] | |
| Extreme of ages | |
| Increased susceptibility to ADEs [2,78] | |
| Prolonged hospitalization | |
| Increased exposure and susceptibility to ADEs [2,78] | |
| Sedation | |
| Patients unable to participate in care and defend themselves against errors [9] | |
| Medications | Types of medications |
| Frequent use of boluses and infusions [9] | |
| Weight-based infusions derived from estimated weights or unreliable determinations [79] | |
| Mathematical calculations required for medication dosages [9] | |
| Programming of infusion pumps [44] | |
| Number of medications | |
| Twice as many medications prescribed as for patients in other units [35] | |
| Increased probability of medication error and medication interactions [35] | |
| Number of interventions | |
| Increased risk of complications [80] | |
| ICU environment | Complex environment |
| Difficult working conditions make errors more probable [81] | |
| High stress [20] | |
| High turnover of patients and providers [82,83] | |
| Emergency admissions | |
| Risk of an adverse event increases by approximately 6% per day [25,84] | |
| Multiple care providers | |
| Challenges the integration of different care plans [83] |
ADE, adverse drug event; ICU, intensive care unit.
How can we prevent medication errors?
Improved medication safety can be accomplished by optimizing the safety of the medication process, eliminating situational risk factors, and providing strategies to both intercept errors and mitigate their consequences. Several interventions have been shown to decrease medical error in the ICU (Table 3).
Table 3.
Sample strategies to prevent medication errors
| Optimize the medication process |
| 1. Medication standardization |
| 2. Computerized physician order entry and clinical decision support |
| 3. Bar code technology |
| 4. Computerized intravenous infusion devices |
| 5. Medication reconciliation |
| Eliminate situational risk factors |
| 1. Avoid excessive consecutive and cumulative working hours |
| 2. Minimize interruptions and distractions |
| 3. Trainee supervision and graduated responsibility |
| Oversight and error interception |
| 1. Intensivist participation in ICU care |
| 2. Adequate staffing |
| 3. Pharmacist participation in ICU care |
| 4. Incorporation of quality assurance into academic education |
ICU, intensive care unit.
The safest and most efficient means of improving patient safety is to improve the safety of the medication process. Strategies that have been shown to be successful include medication standardization [40,41], computerized physician order entry (CPOE) [42,43], bar code technology [44,45], computerized intravenous infusion devices [9], and medication reconciliation [46]. CPOE targets the prescription and transcription stages of the medication process. The technology permits clinicians to enter orders directly into a computer workstation that is linked to a hospital clinical information system [47]. The main advantages of these systems are that they can track allergies, recommend drug dosages, provide adjustments for patients with altered renal or hepatic function, and identify potential drug-drug interactions [11]. Major limitations for implementation include capital costs, provider willingness to adopt the technology, and worries about technical malfunctions and paradoxical increases in medication errors during implementation periods [9,48]. Two systematic reviews have documented that CPOE systems increase clinician adherence to guidelines and alerts, improve organizational efficiency, reduce costs, and even prevent medication errors, but there is limited evidence to support improved patient safety [42,43]. In this regard, CPOE technology highlights the important distinction between error and harm; errors are an important intermediate outcome, but preventing patient harm is the ultimate goal [49]. CPOE technology currently is not used in the majority of ICUs [50].
Bar code technologies target the administration phase of the medication process. Used in conjunction with CPOE, bar code labels for the medication, the patient, and the provider administering the medication are scanned, reconciled, and documented electronically. This process helps ensure that the correct patient gets the correct dose of the correct drug by the correct route at the correct time [44]. Administration errors have been documented to be reduced by 60% [45]. Computerized intravenous infusion devices allow incorporation of CPOE and bar code technology for intravenous medications such that standardized concentrations, infusion rates, and dosing limits can be provided to help prevent intravenous medication errors [9].
Three quarters of patient medications are stopped on patient admission to the ICU [39,51]. Many of these medications are not restarted by the time of patient discharge from the ICU (88%) or hospital (30%) [39,51]. Medication reconciliation is a process that matches a patient's current hospital medication regimen against a patient's long-term medication regimen. A coordinated medication reconciliation program can prevent drug withdrawal and ensure that life-saving medications are continued or restarted as soon as appropriate [46].
Situational risk factors can divert providers' attention and increase the risk of active failures. These need to be minimized. For example, acute and chronic sleep deprivation among residents has been shown to increase the risk of error [52,53]. Therefore, it seems reasonable to establish clinical routines that balance the risk of provider fatigue against the risk of frequent patient sign-over [54]. Trainee supervision and graduated responsibility represent additional risk factors that need to be managed. Clinical inexperience can have a major impact on errors. First-year residents are five times more likely to make prescribing errors than those with more experience [55], as are residents at the start of new rotations [56]. Pharmacological knowledge is an independent predictor of medication errors by health care providers [11]. It is important to capture providers when they start in new environments, train them, and then provide graduated supervision as they develop experience [57]. Although efforts should be directed at targeting situational risk factors, it is important to note that most medication errors occur when individuals are working under what they perceive to be reasonably normal conditions and denying fatigue, stress, or distractions at the time of the error [35].
Physicians, nurses, and pharmacists are integral to medication oversight and error interception. Participation of an intensivist in patient care in the ICU has been reported to decrease medication errors from 22% to 70% [58], complications by 50% [59], ICU mortality, ICU length of stay, and hospital length of stay and to improve patient safety [60]. Pharmacists, similarly, have an important role to play in medication safety. First, all intravenous medications should be prepared within the pharmacy department by pharmacists using a standardized process and standardized medication concentrations. Second, participation of a pharmacist in clinical rounds improves patient safety by reducing preventable ADEs by 66% [61] while shortening patients' length of hospital stay [62,63], decreasing mortality [64], and decreasing medication expenditures [65,66].
Nurses play a particularly important role in patient safety because they are the health care providers with whom patients are likely to spend the greatest amount of time. This has two important implications. One, decreasing nurse-to-patient staffing ratios may be associated with an increased risk of medical errors [67,68]. Nurse-to-patient ratios of 1:1 or 1:2 appear to be safest in the ICU [69]. Second, nursing experience may have an important influence on patient safety. Experienced nurses are more likely to intercept errors compared with less experienced nurses [70].
What can we learn from errors?
Incompetent or irresponsible clinicians do not cause most adverse events. James Reason provides a compelling explanation of error using Swiss cheese as a model (Figure 1). In the real world, our defenses against adverse events, like slices of Swiss cheese, are imperfect. These holes continually open, close, and shift their locations. An adverse event occurs when the holes in many layers of defense momentarily line up [71]. Therefore, it is not surprising that models of quality improvement based on identifying and removing 'bad apple' clinicians have not been effective in improving the safety of health care [72].
Figure 1.
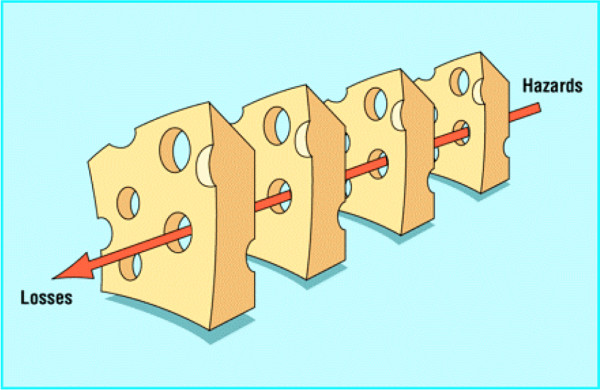
James Reason's Swiss cheese model of defenses. Reprinted from the BMJ [71] (copyright 2000) with permission from the BMJ Publishing Group Ltd.
Conversely, high-reliability organizations such as aircraft carriers, nuclear power plants, and air traffic controllers have markedly improved safety by standardizing practices and investing in safety training and research [71,73]. Three simple strategies to change medicine's approach to medication errors have been proposed [74]: (a) recognize that current approaches for preventing medication errors are inadequate; (b) improve the error-reporting system, avoid punishment, and focus on identifying performance improvement opportunities; and (c) understand and enhance human performance within the medication use process.
We should focus on developing systems that view humans as fallible and assume that errors will occur, even in the best organizations. In this model, multiple barriers and safeguards can be developed to reduce the frequency of ADEs. Error reporting is an important component of this strategy because it reveals the active failures and latent conditions in the system [6]. Near misses are incidents that did not lead to harm but could have resulted in patient injury. Reporting these as well as adverse events offers several advantages over reporting only adverse events. These include greater event frequency for quantitative analysis, fewer reporting barriers partly owing to fewer liability concerns, and an opportunity to study recovery patterns [75]. Ideally, error reporting should be voluntary, anonymous, centralized to increase the pool of data, and designed to identify opportunities for performance improvement. However, error reporting alone will not improve patient safety but rather is the first step in a continuous quality improvement cycle [6]. In addition, error reporting has its limitations. Like any intervention, it can have unintended consequences such as creating incentives for gaming the health care system, particularly if penalties or rewards are directly or indirectly associated with reporting [76]. In addition, error reporting can be labor-intensive. For example, a 10-bed ICU could be anticipated to produce more than 6,200 error reports per year (1.7 errors per patient per day × 10 beds × 365 days). Reporting near misses would substantially increase the number of reports. Some systems such as the AIMS-ICU (Australian Incident Monitoring Study in Intensive Care) and the ICUSRS (Intensive Care Unit Safety Reporting System) have been developed with the goal of balancing the strengths and limitations of error reporting [72].
Conclusion
Patient safety is an important health care issue because of the consequences of iatrogenic injuries. Medication errors in critical care are frequent, serious, and predictable. Human factor research in nonmedical settings suggests that demanding greater vigilance from providers of medical care may not result in meaningful safety improvement. Instead, the approach of identifying failures and redesigning faulty systems appears to be a more promising way to reduce human error.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EC and EM performed the literature search and partially drafted and revised the manuscript. HTS designed the literature search strategy and partially drafted and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
The authors thank Sharon Straus and Heather Jeppesen for their comments on an earlier draft of this manuscript.
See related commentary by Parshoram, http://ccforum.com/content/12/2/137
References
- Medical errors: the scope of the problem http://www.ahrq.gov/qual/errback.htm
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington: National Academy Press; 1999. [PubMed] [Google Scholar]
- Stelfox HT, Palmisani S, Scurlock C, Orav EJ, Bates DW. The 'To Err is Human' report and the patient safety literature. Qual Saf Health Care. 2006;15:174–178. doi: 10.1136/qshc.2006.017947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384–2390. doi: 10.1001/jama.293.19.2384. [DOI] [PubMed] [Google Scholar]
- Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung CL, Pizov R, Cotev S. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294–300. doi: 10.1097/00003246-199502000-00015. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Thompson DA, Holzmueller CG, Lubomski LH, Morlock LL. Defining and measuring patient safety. Crit Care Clin. 2005;21:1–19. doi: 10.1016/j.ccc.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Rothschild JM, Landrigan CP, Cronin JW, Kaushal R, Lockley SW, Burdick E, Stone PH, Lilly CM, Katz JT, Czeisler CA, Bates DW. The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33:1694–1700. doi: 10.1097/01.CCM.0000171609.91035.BD. [DOI] [PubMed] [Google Scholar]
- Pharmacy-nursing shared vision for safe medication use in hospitals: executive summary session. Am J Health Syst Pharm. 2003;60:1046–1052. doi: 10.1093/ajhp/60.10.1046. [DOI] [PubMed] [Google Scholar]
- Hussain E, Kao E. Medication safety and transfusion errors in the ICU and beyond. Crit Care Clin. 2005;21:91–110. doi: 10.1016/j.ccc.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Leape LL. Preventing adverse drug events. Am J Health Syst Pharm. 1995;52:379–382. doi: 10.1093/ajhp/52.4.379. [DOI] [PubMed] [Google Scholar]
- Krahenbuhl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krahenbuhl S. Drug-related problems in hospitals: a review of the recent literature. Drug Safety. 2007;30:379–407. doi: 10.2165/00002018-200730050-00003. [DOI] [PubMed] [Google Scholar]
- Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, Laffel G, Sweitzer BJ, Shea BF, Hallisey R. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA. 1995;274:29–34. doi: 10.1001/jama.274.1.29. [DOI] [PubMed] [Google Scholar]
- Calabrese AD, Erstad BL, Brandl K, Barletta JF, Kane SL, Sherman DS. Medication administration errors in adult patients in the ICU. Intensive Care Med. 2001;27:1592–1598. doi: 10.1007/s001340101065. [DOI] [PubMed] [Google Scholar]
- Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T, Hallisey R, Ives J, Laird N, Laffel G, Nemeskal R, Petersen LA, Porter K, Servi D, Shea BF, Small SD, Sweitzer BJ, Thompson T, Vander Vliet M, for the ADE Prevention Study Group Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA. 1995;274:35–43. doi: 10.1001/jama.274.1.35. [DOI] [PubMed] [Google Scholar]
- The United States Pharmacopeial Convention: 1999. Rockville, MD: United States Pharmacopeia; 1999. pp. 1131–1132. [Google Scholar]
- Parshuram CS, Ng GYT, Ho TKL, Klein J, Moore AM, Bohn D, Koren G. Discrepancies between ordered and delivered concentrations of opiate infusions in critical care. Crit Care Med. 2003;31:2483–2487. doi: 10.1097/01.CCM.0000089638.83803.B2. [DOI] [PubMed] [Google Scholar]
- Reason J. Human Error. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Kanjanarat P, Winterstein AG, Johns TE, Hatton RC, Gonzalez-Rothi R, Segal R. Nature of preventable adverse drug events in hospitals: a literature review. Am J Health Syst Pharm. 2003;60:1750–1759. doi: 10.1093/ajhp/60.17.1750. [DOI] [PubMed] [Google Scholar]
- Kane-Gill S, Weber RJ. Principles and practices of medication safety in the ICU. Crit Care Clin. 2006;22:273–290. doi: 10.1016/j.ccc.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Miller MR, Robinson KA, Lubomski LH, Rinke ML, Pronovost PJ. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16:116–126. doi: 10.1136/qshc.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neil AC, Petersen LA, Cook EF, Bates DW, Lee TH, Brennan TA. Physician reporting compared with medical-record review to identify adverse medical events. Ann Intern Med. 1993;119:370–376. doi: 10.7326/0003-4819-119-5-199309010-00004. [DOI] [PubMed] [Google Scholar]
- Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm. 2002;59:436–446. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- Michel P, Quenon JL, de Sarasqueta AM, Scemama O. Comparison of three methods for estimating rates of adverse events and rates of preventable adverse events in acute care hospitals. BMJ. 2004;328:199. doi: 10.1136/bmj.328.7433.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews LB, Stocking C, Krizek T, Gottlieb L, Krizek C, Vargish T, Siegler M. An alternative strategy for studying adverse events in medical care. Lancet. 1997;349:309–313. doi: 10.1016/S0140-6736(96)08268-2. [DOI] [PubMed] [Google Scholar]
- Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. Relationship between medication errors and adverse drug events. J Gen Intern Med. 1995;10:199–205. doi: 10.1007/BF02600255. [DOI] [PubMed] [Google Scholar]
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–1903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- Tissot E, Cornette C, Demoly P, Jacquet M, Barale F, Capellier G. Medication errors at the administration stage in an intensive care unit. Intensive Care Med. 1999;25:353–359. doi: 10.1007/s001340050857. [DOI] [PubMed] [Google Scholar]
- Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA. 1997;277:301–306. doi: 10.1001/jama.277.4.301. [DOI] [PubMed] [Google Scholar]
- Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–1316. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- Cohen H, Mandrack MM. Application of the 80/20 rule in safeguarding the use of high-alert medications. Crit Care Nurs Clin North Am. 2002;14:369–374. doi: 10.1016/S0899-5885(02)00018-7. [DOI] [PubMed] [Google Scholar]
- Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med. 1992;7:424–431. doi: 10.1007/BF02599161. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Weast B, Holzmueller CG, Rosenstein BJ, Kidwell RP, Haller KB, Feroli ER, Sexton JB, Rubin HR. Evaluation of the culture of safety: survey of clinicians and managers in an academic medical center. Qual Saf Health Care. 2003;12:405–410. doi: 10.1136/qhc.12.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraud T, Dhainaut JF, Vaxelaire JF, Joseph T, Journois D, Bleichner G, Sollet JP, Chevret S, Monsallier JF. Iatrogenic complications in adult intensive care units: a prospective two-center study. Crit Care Med. 1993;21:40–51. doi: 10.1097/00003246-199301000-00011. [DOI] [PubMed] [Google Scholar]
- Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care and general care units. Crit Care Med. 1997;25:1289–1297. doi: 10.1097/00003246-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Ridley SA, Booth SA, Thompson CM, Clayton T, Eddleston J, Mackenzie S, Thomas T, Webb A, Wright D. Prescription errors in UK critical care units. Anaesthesia. 2004;59:1193–1200. doi: 10.1111/j.1365-2044.2004.03969.x. [DOI] [PubMed] [Google Scholar]
- Kollef MH, Sherman G, Ward S, Fraser VJ. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115:462–474. doi: 10.1378/chest.115.2.462. [DOI] [PubMed] [Google Scholar]
- Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–155. doi: 10.1378/chest.118.1.146. [DOI] [PubMed] [Google Scholar]
- Campbell AJ, Bloomfield R, Noble DW. An observational study of changes to long-term medication after admission to an intensive care unit. Anaesthesia. 2006;61:1087–1092. doi: 10.1111/j.1365-2044.2006.04831.x. [DOI] [PubMed] [Google Scholar]
- Larsen GY, Parker HB, Cash J, O'Connell M, Grant MC. Standard drug concentrations and smart-pump technology reduce continuous-medication-infusion errors in pediatric patients. Pediatrics. 2005;116:e21–25. doi: 10.1542/peds.2004-2452. [DOI] [PubMed] [Google Scholar]
- Bullock J, Jordan D, Gawlinski A, Henneman EA. Standardizing IV infusion medication concentrations to reduce variability in medication errors. Crit Care Nurs Clin North Am. 2006;18:515–521. doi: 10.1016/j.ccell.2006.08.008. [DOI] [PubMed] [Google Scholar]
- Shamliyan TA, Duval S, Du J, Kane RL. Just what the doctor ordered. Review of the evidence of the impact of computerized physician order entry system on medication errors. Health Serv Res. 2008;43(1 Pt 1):32–53. doi: 10.1111/j.1475-6773.2007.00751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eslami S, Abu-Hanna A, De Keizer NF, De Jonge E. Errors associated with applying decision support by suggesting default doses for aminoglycosides. Drug Safety. 2006;29:803–809. doi: 10.2165/00002018-200629090-00004. [DOI] [PubMed] [Google Scholar]
- Williams CK, Maddox RR. Implementation of an i.v. medication safety system. Am J Health Syst Pharm. 2005;62:530–536. doi: 10.1093/ajhp/62.5.530. [DOI] [PubMed] [Google Scholar]
- Cummings J, Bush P, Smith D, Matuszewski K. Bar-coding medication administration overview and consensus recommendations. Am J Health Syst Pharm. 2005;62:2626–2629. doi: 10.2146/ajhp050222. [DOI] [PubMed] [Google Scholar]
- Pronovost P, Weast B, Schwarz M, Wyskiel RM, Prow D, Milanovich SN, Berenholtz S, Dorman T, Lipsett P. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18:201–205. doi: 10.1016/j.jcrc.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Sittig DF, Stead WW. Computer-based physician order entry: the state of the art. J Am Med Inform Assoc. 1994;1:108–123. doi: 10.1136/jamia.1994.95236142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weant KA, Cook AM, Armitstead JA. Medication-error reporting and pharmacy resident experience during implementation of computerized prescriber order entry. Am J Health Syst Pharm. 2007;64:526–530. doi: 10.2146/ajhp060001. [DOI] [PubMed] [Google Scholar]
- Eslami S, Keizer NF, Abu-Hanna A. The impact of computerized physician medication order entry in hospitalized patients-A systematic review. Int J Med Inform. 2007, Nov 17. [DOI] [PubMed]
- Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in U.S. hospitals: results of a 2002 survey. J Am Med Inform Assoc. 2004;11:95–99. doi: 10.1197/jamia.M1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CM, Rahimi-Darabad P, Orner AI. Discontinuity of chronic medications in patients discharged from the intensive care unit. J Gen Intern Med. 2006;21:937–941. doi: 10.1007/BF02743141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stampi C. Ultrashort sleep/wake patterns and sustained performance. In: Dinges DFB, Broughton RJ, editor. Sleep and Alertness: Chronobiological, Behavioral, and Medical Aspects of Napping. New York: Raven Press; 1989. p. 456. [Google Scholar]
- Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- Drazen JM. Awake and informed. N Engl J Med. 2004;351:1884. doi: 10.1056/NEJMe048276. [DOI] [PubMed] [Google Scholar]
- Lesar TS, Briceland LL, Delcoure K, Parmalee JC, Masta-Gornic V, Pohl H. Medication prescribing errors in a teaching hospital. JAMA. 1990;263:2329–2334. doi: 10.1001/jama.263.17.2329. [DOI] [PubMed] [Google Scholar]
- LaPointe NM, Jollis JG. Medication errors in hospitalized cardiovascular patients. Arch Intern Med. 2003;163:1461–1466. doi: 10.1001/archinte.163.12.1461. [DOI] [PubMed] [Google Scholar]
- Wasserfallen JB, Butschi AJ, Muff P, Biollaz J, Schaller MD, Pannatier A, Revelly JP, Chiolero R. Format of medical order sheet improves security of antibiotics prescription: The experience of an intensive care unit. Crit Care Med. 2004;32:655–659. doi: 10.1097/01.CCM.0000114835.97789.AB. [DOI] [PubMed] [Google Scholar]
- Van Den Bemt PMLA, Fijn R, Van Der Voort PHJ, Gossen AA, Egberts TCG, Brouwers JRBJ. Frequency and determinants of drug administration errors in the intensive care unit. Crit Care Med. 2002;30:846–850. doi: 10.1097/00003246-200204000-00022. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- Durbin CG., Jr Team model: advocating for the optimal method of care delivery in the intensive care unit. Crit Care Med. 2006;34(3 Suppl):S12–17. doi: 10.1097/01.CCM.0000199985.72497.D1. [DOI] [PubMed] [Google Scholar]
- Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, Hebert L, Newhouse JP, Weiler PC, Hiatt H. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–384. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- Bjornson DC, Hiner WO, Jr, Potyk RP, Nelson BA, Lombardo FA, Morton TA, Larson LV, Martin BP, Sikora RG, Cammarata FA. Effect of pharmacists on health care outcomes in hospitalized patients. Am J Hosp Pharm. 1993;50:1875–1884. [PubMed] [Google Scholar]
- Boyko WL, Jr, Yurkowski PJ, Ivey MF, Armitstead JA, Roberts BL. Pharmacist influence on economic and morbidity outcomes in a tertiary care teaching hospital. Am J Health Syst Pharm. 1997;54:1591–1595. doi: 10.1093/ajhp/54.14.1591. [DOI] [PubMed] [Google Scholar]
- Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27:481–493. doi: 10.1592/phco.27.4.481. [DOI] [PubMed] [Google Scholar]
- Montazeri M, Cook DJ. Impact of a clinical pharmacist in a multidisciplinary intensive care unit. Crit Care Med. 1994;22:1044–1048. doi: 10.1097/00003246-199406000-00027. [DOI] [PubMed] [Google Scholar]
- Baldinger SL, Chow MS, Gannon RH, Kelly ET., 3rd Cost savings from having a clinical pharmacist work part-time in a medical intensive care unit. Am J Health Syst Pharm. 1997;54:2811–2814. doi: 10.1093/ajhp/54.24.2811. [DOI] [PubMed] [Google Scholar]
- Beckmann U, Baldwin I, Durie M, Morrison A, Shaw L. Problems associated with nursing staff shortage: an analysis of the first 3600 incident reports submitted to the Australian Incident Monitoring Study (AIMS-ICU) Anaesth Intensive Care. 1998;26:396–400. doi: 10.1177/0310057X9802600410. [DOI] [PubMed] [Google Scholar]
- Whitman GR, Kim Y, Davidson LJ, Wolf GA, Wang SL. The impact of staffing on patient outcomes across specialty units. J Nurs Adm. 2002;32:633–639. doi: 10.1097/00005110-200212000-00008. [DOI] [PubMed] [Google Scholar]
- Pronovost P, Wu AW, Dorman T, Morlock L. Building safety into ICU care. J Crit Care. 2002;17:78–85. doi: 10.1053/jcrc.2002.34363. [DOI] [PubMed] [Google Scholar]
- Hanneman SK. Advancing nursing practice with a unit-based clinical expert. Image J Nurs Sch. 1996;28:331–337. doi: 10.1111/j.1547-5069.1996.tb00383.x. [DOI] [PubMed] [Google Scholar]
- Reason J. Human error: models and management. BMJ. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Ansari MA, Hijazi MH. Medical errors and adverse events: focus on the intensive care unit. Clinical Intensive Care. 2006;17:9–17. doi: 10.1080/09563070600576196. [DOI] [Google Scholar]
- Bion JF, Heffner JE. Challenges in the care of the acutely ill. Lancet. 2004;363:970–977. doi: 10.1016/S0140-6736(04)15793-0. [DOI] [PubMed] [Google Scholar]
- Crane VS. New perspectives on preventing medication errors and adverse drug events. Am J Health Syst Pharm. 2000;57:690–697. doi: 10.1093/ajhp/57.7.690. [DOI] [PubMed] [Google Scholar]
- Barach P, Small SD. Reporting and preventing medical mishaps: lessons from non-medical near miss reporting systems. BMJ. 2000;320:759–763. doi: 10.1136/bmj.320.7237.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290:1899–1905. doi: 10.1001/jama.290.14.1899. [DOI] [PubMed] [Google Scholar]
- ASHP guidelines on preventing medication errors in hospitals. Am J Hosp Pharm. 1993;50:305–314. [PubMed] [Google Scholar]
- Weingart SN, Wilson RM, Gibberd RW, Harrison B. Epidemiology of medical error. BMJ. 2000;320:774–777. doi: 10.1136/bmj.320.7237.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herout PM, Erstad BL. Medication errors involving continuously infused medications in a surgical intensive care unit. Crit Care Med. 2004;32:428–432. doi: 10.1097/01.CCM.0000108876.12846.B7. [DOI] [PubMed] [Google Scholar]
- Stambouly JJ, McLaughlin LL, Mandel FS, Boxer RA. Complications of care in a pediatric intensive care unit: a prospective study. Intensive Care Med. 1996;22:1098–1104. doi: 10.1007/BF01699236. [DOI] [PubMed] [Google Scholar]
- Donchin Y, Seagull FJ. The hostile environment of the intensive care unit. Curr Opin Crit Care. 2002;8:316–320. doi: 10.1097/00075198-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA. 1999;281:1310–1317. doi: 10.1001/jama.281.14.1310. [DOI] [PubMed] [Google Scholar]
- Bria WF, 2nd, Shabot MM. The electronic medical record, safety, and critical care. Crit Care Clin. 2005;21:55–79. doi: 10.1016/j.ccc.2004.08.001. viii. [DOI] [PubMed] [Google Scholar]
- Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]


