Abstract
Rapid social and economic change is transforming China with enormous implications for its population and economy. China is a huge transition toward a country with over a fifth of adults being overweight with related dietary and physical activity patterns. Overweight and poor diets are shifting to be a greater burden for the poor with subsequent large increases in hypertension, stroke and adult onset diabetes. The related economic costs represent 4–8% of the economy. Public investments in China are needed to head off a huge increase in the morbidity, disability, absenteeism and medical care costs linked with this nutritional shift.
Keywords: dietary change, obesity, physical activity change, economic costs, health care costs
Introduction
China is a transformed country in the new millennium. Rapid economic and social change, including an economy that has grown at an annual rate greater than 8% for more than two decades, have truly transformed urban China and a sizable portion of its rural sector.1 Poverty, environmental degradation, and other major problems still exist; the effects of these changes are readily seen in the rapid shift of the nutrition transition stage for China. Obesity and other noncommunicable diseases (NCDs) are the major causes of morbidity, disability, and mortality in the country resulting in a major growth of the health system to care for them.
The unseen changes are (a) the enormous shifts in the nutritional status of the Chinese population and (b) the increasing impact of this shift on morbidity and mortality. The proportion of the population residing in urban areas has grown equally rapid.2 Technological shifts have reduced physical activity at work, travel, home production, and leisure. Shifts in food technology, importation controls, food pricing, and mass media, among others, have truly transformed Chinese consumption patterns.
A recent paper traced the changes in Chinese health care—in particular those following the privatization of the Chinese economy.3 Blumenthal and Hsiao particularly point out the massive reduction of the national government’s share of health care costs and the large increase in the population not covered by any health insurance or effective health safety net. Recent results from the China Health and Nutrition Survey (CHNS) reveal that today, less than 25% of the Chinese are effectively covered by health insurance. National expenditures on health care have risen to well over 5.5% of gross domestic product (GDP) and are rapidly increasing. Blumenthal and Hsiao also note ways the government is attempting to respond to the challenges of providing health care to its population, but do not discuss the underlying monumental shifts in (a) the health of the population and (b) the lack of preparation or attention to the coming NCD epidemic in China.4
This study provides an overview of the rapid shifts in China’s dietary and physical activity patterns; related high levels of smoking and other key risk factors; and the subsequent rapid shifts in obesity and other NCDs. In addition, medical costs and other data are presented to highlight the large costs already seen in China linked with these nutrition-related problems.
China’s Nutrition Transition
For this paper, we utilize mainly data from the China Health and Nutrition Surveys (CHNS, 1991, 2000 and 2006). The CHNS longitudinal surveys covered nine provinces that vary substantially in geography, economic development, and health indicators, that provide a broad-based indication of the trends China is facing. Although the CHNS are not national representative surveys, previous findings regarding the patterns and trends in people’s diet and body composition from CHNS are almost identical with those from national surveys and the China National Bureau of Statistics.5 Anthropometric measurements were carried out by well trained health workers who followed standard protocol. Weight was measured in light weight clothing to the nearest tenth of a kilogram with a beam balance scale. Height was measured without shoes to the nearest tenth of a centimeter, using a portable stadiometer. Dietary data utilized 3 days of in-depth 24-hour recall data supplemented with household weighing and measurement at the beginning and ending of each day of all inventory and all purchases.6
China has undergone many marked shifts since 1949. These include (a) a period (1949–1957) when food production was inadequate and low cereal consumption patterns existed, (b) the famine (1957–1962) linked with the great leap forward, (c) a strong recovery (1962–1979), (d) the subsequent reform period (1979–1985)—after the liberalization of food production when the annual economic growth rate was over 10%, and (e) the current period (since 1985) with continued rapid economic growth and a remarkable shift in the diet structure.7 This paper explores the shifts during the past two decades (since 1985) and the full implications of the obesity epidemic resulting from these changes in the Chinese diet and activity patterns.
Cheap, Plentiful, Edible Oil Fueled Major Dietary Changes
Worldwide supply and demand for vegetable fats has accelerated11 beginning with major technological breakthroughs in the development of high-yield oilseeds and in the refining of high-quality vegetable oils in the post-WW II period. This was fueled by concerns of the 1950–70 time period, related to the effects on heart disease of excessive consumption of animal fats—many of which were saturated. A number of concomitant major economic and political initiatives led to the development of oil crops, not only in Europe and the United States, but in South East Asia (palm oils) and in Brazil and Argentina (soybean oils). There was a major delay between the time edible oil reached the higher income countries and then most of the developing world The nutrition transition (a series of collective changes in diet, physical activity, health, and nutrition) in developing nations typically begins with major increases in the domestic production and imports of oilseeds and vegetable oils, rather than increased imports of meat and milk. While the shifts in edible oil reached all nations and the poor, the large increases in animal source food intake discussed below was more focused on selected countries.8
Major shifts in Chinese tax and import regulations during 1990 and 1991 began this rapid shift in the dietary intake of oils. One of the major edible oils consumed in China is soybean oil. Chinese soybean oil importation, for instance, skyrocketed from a miniscule level to over 14 million metric tons per annum and represented a per capita basis of 78 kilocalories per day. Domestic production also skyrocketed and a large number of vegetable oils—many containing highly pathogenic products—were consumed.9
Globally, the edible oil revolution allowed low-income countries to increase their intake of fats and shift overall consumption patterns. The shift in China led to the excessive use of edible oil by all social classes; the price and income elasticities indicate that the most rapid shifts in edible oil consumption are now occurring among the poor.10 Intake of edible oil almost doubled between 1989 and 1991 as per capita intake increased from 23.2 to 41.6 grams per day (209 to 374 kilocalories) among adults.11
The Animal Source Foods Revolution has hit China
Edible oils certainly led the initial stages in the shift of Chinese diets; nevertheless, the long-term global declines in the price of beef, other animal source foods, and feed grains have led to a second major set of dietary shifts in China and selected other low and moderate income countries. For example, Delgado and others have shown that worldwide beef prices have declined in real terms by more than 400% over the past four decades. The worldwide livestock revolution continues with increased open trade and large global subsidies helping to fuel the changes.12
Rapid shifts are equally dramatic in China.13 Egg, poultry, beef, and pork consumption have increased rapidly in China and milk intake has recently begun to rise. Today, the average Chinese adult consumes more than 1300 kcals per day of pork, poultry, beef, mutton, fish, eggs, and dairy food. As we have shown elsewhere, the structure of consumption shifts in China is such that for each additional increase in income, adults proportionally increase their intake of animal source foods.14
The Resultant Shift Toward Increasingly Energy-Dense Diets
The increase in animal source foods and edible oils intake, concomitant with declines in cereal intake and minimal changes in vegetable intake, has led to large increases in the energy density of the diet and equally large shifts in fat intake. While accurate data on the total shift in saturated and hydrogenated fats in the Chinese diet are not available, the proportion of energy from fat and animal source foods has certainly increased significantly. The classical Chinese diet—rich in vegetables and carbohydrates with minimal animal food—no longer exists. In 2006, less than 1% of all Chinese adults consumed a diet with less than 10% of energy derived from fat. In contrast—more than 44% of adults (44.1%) consumed a higher fat diet with more than 30% of energy derived from fat and close to two-thirds of adults (67.0%) consumed a diet with more than 10% of their energy derived from animal source food fats—primarily saturated (Table 1).
Table 1.
Shifts in energy sources in Chinese diet, for adults aged 20 to 45 years
| 1. | 2. | Receiving more than 30% energy from fat (%) | 3. | Received more than 10% energy from animal source food (%) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4. | 5. | 6. | |||||||||||||||||||
| 7. | 8. | 1989 | 9. | 1993 | 10. | 1997 | 11. | 2000 | 12. | 2006 | 13. | 1989 | 14. | 1993 | 15. | 1997 | 16. | 2000 | 17. | 2006 | |
| 18. | Urban | 19. | 19.8 | 20. | 44.0 | 21. | 52.0 | 22. | 56.9 | 23. | 57.9 | 24. | 49.8 | 25. | 59.8 | 26. | 57.2 | 27. | 62.0 | 28. | 81.9 |
| 29. | Rural | 30. | 12.1 | 31. | 18.8 | 32. | 26.5 | 33. | 38.3 | 34. | 38.7 | 35. | 33.3 | 36. | 37.6 | 37. | 37.6 | 38. | 44.0 | 39. | 61.1 |
| 40. | Low-income | 41. | 9.3 | 42. | 11.6 | 43. | 15.8 | 44. | 27.1 | 45. | 33.5 | 46. | 26.2 | 47. | 28.7 | 48. | 27.1 | 49. | 35.4 | 50. | 53.8 |
| 51. | Mid-income | 52. | 16.2 | 53. | 23.7 | 54. | 30.9 | 55. | 44.6 | 56. | 39.4 | 57. | 42.8 | 58. | 45.3 | 59. | 42.4 | 60. | 51.3 | 61. | 60.6 |
| 62. | High-income | 63. | 18.5 | 64. | 43.9 | 65. | 51.3 | 66. | 56.3 | 67. | 53.4 | 68. | 47.8 | 69. | 61.5 | 70. | 61.6 | 71. | 60.7 | 72. | 79.5 |
| 73. | Total | 74. | 14.7 | 75. | 26.0 | 76. | 34.2 | 77. | 43.9 | 78. | 44.1 | 79. | 38.8 | 80. | 34.9 | 81. | 43.5 | 82. | 49.4 | 83. | 67.0 |
Source: China Health and Nutrition Surveys for 1989, 1993, 1997, 2000 and 2006
Is Westernization Of The Food Supply And The Pattern Of Eating Occurring?
Many scholars have suggested that the fast food chain and soft drink consumption patterns that are dominant in the United States will become a global issue;14 however, this does not appear to be the global pattern of change we find.15 For example, the major changes one sees in China are in the rapid transformations of the food marketing landscape. As with Latin America, the food marketing landscape in Asia is being rapidly dominated by supermarkets, particularly large superstores.16 In China, Carrefour and Wal-Mart supermarkets are not only expanding as rapidly as possible, but they are also being matched by domestic clones.17 China is now experiencing the fastest global growth in supermarkets with sales of these stores growing by 3–40% annually.18 By 2003, more than $55 billion was expended on construction of supermarkets and urban, let alone rural areas, have only begun to be reached by this construction boom. These supermarkets are spreading to secondary cities and towns and starting to reach out to higher income rural areas.
One might also expect with all these changes that the Chinese would have followed the U.S. model and would be excessive consumption of caloric sweeteners and large amounts of soft drinks and fruit drinks; however, this is certainly not the case. The Chinese, while starting to consume limited amounts of soft drinks and other sweetened beverages and foods, still consume only a small proportion of energy from these sources; moreover, they consume very little away-from-home food and Western-style fast foods.19 Among Chinese children aged 2–18y, for example, less than 10% of their calories were consumed from food purchased away-from-home, while comparative data from a neighboring country—the Philippines—found almost 40% of children’s calories were consumed from similar foods.20 This same study showed that less than a tenth of a percent (< 0.1%) of Chinese children’s energy was obtained from fast foods and soft drinks—compared with about 3% of Philippine children’s energy. Western and Chinese variants of pizza, hamburgers, fried chicken, and related fast food chains are rapidly expanding in Chinese cities, but the total reach of these chains into the broader population is still very small.
Shifts In Physical Activity At Work, Travel, And Leisure Are Equally Profound!
There are several linked changes in physical activity occurring jointly. One is a shift away from the high-energy expenditure activities such as farming, mining, and forestry towards the service sector; we have shown this large effect elsewhere21. Reduced energy expenditures in the same occupation are a second dimension of the shift in energy expenditures linked with economic work.22 For instance, Table 2 shows that the proportion of Chinese urban adults (male and female) working in occupations where they participate in moderate- and high-activity patterns has decreased, but increased in low-activity occupations. In rural areas, however, there has been a much lower shift for some (high-activity occupations) towards decreased physical activity linked to holding multiple jobs and more intensive effort, but moderate-effort occupations are decreasing for many. While some initial research between 1989 and 1991 found an increase in adult underweight status in rural China, most of these individuals with increased heavy activity at work are those with higher income who combine work in the agricultural and modern sectors. Thus most of our research on occupational energy expenditures has not found increased high activity work linked with reduced weight.23 There is also an overall clear income gradient in those involved in high and low energy expenditure occupations.
Table 2.
Shifts in the distribution, by the physical activity requirements of their primary occupation, for adults aged 20 to 45 years
| 84. | 85. 1989 | 86. 2006 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 87. | 88. | Low (%) | 89. | Moderate (%) | 90. | High (%) | 91. | Low (%) | 92. | Moderate (%) | 93. | High (%) | |||
| 94. | Urban | 95. | 44.8 | 96. | 46.1 | 97. | 9.1 | 98. | 66.7 | 99. | 29.3 | 100. | 4.0 | ||
| 101. | Rural | 102. | 21.8 | 103. | 39.1 | 104. | 39.1 | 105. | 33.2 | 106. | 28.2 | 107. | 38.6 | ||
| 108. | Low-income | 109. | 21.5 | 110. | 36.0 | 111. | 42.5 | 112. | 32.9 | 113. | 30.2 | 114. | 36.9 | ||
| 115. | Mid-income | 116. | 28.0 | 117. | 44.5 | 118. | 27.5 | 119. | 37.2 | 120. | 27.6 | 121. | 35.2 | ||
| 122. | High-income | 123. | 37.6 | 124. | 44.2 | 125. | 18.2 | 126. | 52.4 | 127. | 27.7 | 128. | 19.9 | ||
| 129. | Total | 130. | 28.6 | 131. | 41.3 | 132. | 30.1 | 133. | 42.4 | 134. | 28.3 | 135. | 29.3 | ||
Source: China Health and Nutrition Surveys for 1989 and 2006
Other major changes relate to the mode of transportation and activity patterns during leisure hours. China again provides interesting illustrations. In China, 14% of households acquired a motorised vehicle between 1989 and 1997. In one study, we showed that the odds of being obese were 80% higher (p<0.05) for men and women in households that owned a motorised vehicle, compared to those that did not.24
Television ownership has skyrocketed in China, leading to greater inactivity during leisure time.25 In 1989, only 63% of households owned a television set, whereas by 2004 more than 95% of all households owned one with color television sets being owned by two-thirds of the households. Furthermore, programming in 1989 was focused on traditional political and state controlled topics. Over the past 15 years, we have documented enormous shifts in the content of even the national Beijing TV system while Hong Kong Star, a Hong Kong-based cable system which shows predominantly western movies and entertainment and uses only the most modern advertisements, is now available in a large number of communities. Moreover, modern advertisement is now shown on most cable systems.
Adult Overweight Is Increasing Rapidly!
As one might expect, the rapid declines in energy expenditures of the population, linked with the enormous shift toward a diet with more energy density from edible oils and animal source foods, have resulted in a rapid increase in the distribution of the body mass index (BMI) of the Chinese population, particularly adults. Adult male overweight status tripled and female overweight status doubled between 1989 and 2000. By 2004, nearly a quarter of all adults in China were overweight. Moreover, we have shown in a number of studies that the rate of change of Chinese overweight status, in particular among adults, is one of the most rapid in the world and far larger than that for the United States.26
We put the level of overweight and obesity into a larger global context. We examine examines data from studies that are nationally representative, weighted, and with direct measurements of weight and height. The most standard measure of adult obesity is body mass index (BMI) which is weight (kg)/height (m)2. A BMI greater than 30 is considered obese and a BMI between 25 and 29.9 is considered overweight. Age-gender standards equivalent to adult overweight and obesity standards exist and are used for children and adolescents.27 This is a globe where more than 25% of Chinese adults are now overweight or obese and about two-thirds of the adult populations are overweight or obese in countries as diverse as the lower income countries of Egypt, Mexico, South Africa and the higher incomes ones -- Australia, the U.K., and the United States. China and Indonesia’s overweight and obesity prevalence are somewhat similar.28
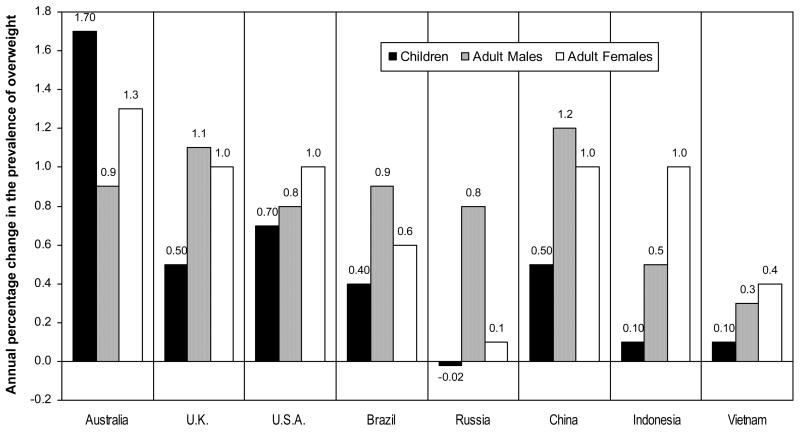
Figure 1 shows changes per year in the prevalence rate of overweight plus obesity. This figure shows, for example, that more than 1.2% of the Chinese adult male population has become overweight or obese each year over the past decade while among adult men from Australia, the U.K., and the United States, the annual rate of increase was slightly less. Interestingly Indonesia women are quite comparable in terms of the change in the prevalence whereas Indonesian children and adult men are much lower.
Figure 1.
Annual Absolute Change in The Prevalence of Overweight and Obesity in 7 Countries from 1985/1995 to 1995/2004 (BMI≥25.0 for Adults; IOTF Equivalent for Children)
Source: B.M. Popkin, “Understanding global nutrition dynamics as a step toward controlling cancer morbidity and mortality,” Nature Reviews Cancer 7, (2007): 61–67.
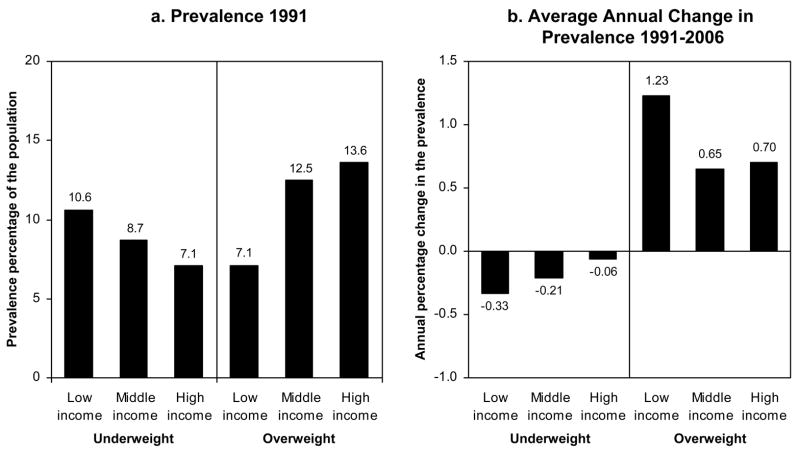
While overweight status has increased greatly in China, the proportion of underweight adults, age 20–45y, dropped in this time period. The largest decline in change per year is found among the low income for underweight and among both the low income and high income tertiles for overweight status. Figure 2 presents the annual rate of change for adults who are under- and overweight by income tertile.
Figure 2.
Average Annual Change in Underweight and Overweight among Chinese Adults (1991–2004)
Source: China Health and Nutrition Surveys for 1991 and 2004
Overweight Is Becoming A Problem Of The Poor!
There is a global shift in transitional and lower income countries toward more overweight among lower socioeconomic individuals. In a study of women from 38 countries, we showed that when countries achieved a GNP of $2500 in 1995 dollars, they had more overweight lower-educated women than higher-educated women.29
China with its much lower GNP also has greater overweight plus obesity among lower-educated women than upper-educated women.30 The income differentials are not dramatic yet but they do show a decline in underweight across all income tertiles. Figure 3 presents the annual rate of change for adults who are under- and overweight by income tertile. While overweight status has increased greatly in China, the proportion of underweight adults, age 20–45y, dropped to 6.5% in this time period.
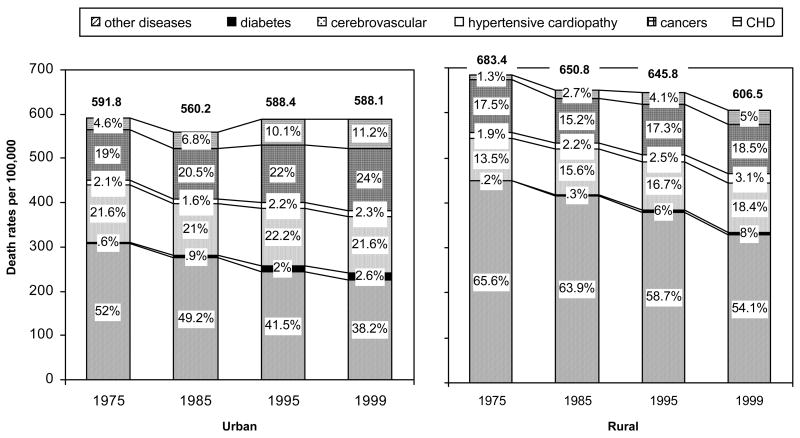
Figure 3.
Trends in the Causes of Mortality in China, 1975–1999
The shift in China toward more overweight among the poor is also seen in more complex longitudinal research on dietary change. This work, published in both social science and economics journals, shows that increased income among the poor is associated with a greater increase in the income elasticity and a greater income elasticity overall than it is among higher-income adults.31
Are These Changes Slowing Down Or Accelerating?
Studies of overweight and dietary pattern shifts indicate rates of change are accelerating. The prevalence rate of change in overweight persons in the 1997–2000 period accelerated from less than 0.5% in the 1980–90 period to 1.9% and 0.9% for men and women, respectively; preliminary data for 2004 indicates that these changes are accelerating.32 In the dietary area, we have documented longitudinally that the income elasticity, or the proportion of food purchases with a 1% increase in income has accelerated at an increasing rate in the past 15 years.33
What Do These Changes Mean For Health Status In China?
While mortality rates from coronary heart disease (CHD) are dropping in higher-income countries, China—along with many other developing countries—is seeing a large increase in nutrition-related causes of death.34 The causes of this CHD and cancer increases in China are directly linked to diet, activity, and obesity.35 In Figure 3 we present Ministry of Health data for China on estimates of cause of death over the past several decades. In both urban and rural areas we see large absolute and relative declines in nonnutrition-related other deaths—deaths from infectious and parasitic infections, hunger and accidents. In contrast, in urban areas we see an increase in the overall death rate between 1985 and 1995.
Moreover over this 24-year period the total shift toward nutrition-related noncommunicable diseases is from 48 to 61.8% of the death in urban areas and 34.5% to 45.9% in rural areas.
What Do These Changes Mean For The Chinese Health Care System?
Over the past 25 years, China has accelerated the decentralization of its public health and medical care systems. A major reduction in central government funding, coupled with an increased focus on local funding from private economic activities, has led to a major neglect of public health activities.36 At the same time, health care expenses are burgeoning as has been shown in a recent review of this topic.37 During the 1978–2002 time period, there was a forty fold increase in personal health costs and more importantly, the national spending on health care has nearly doubled, with a major element being the increased costs of pharmaceuticals.
This shift in health and nutritional status results in not only major direct medical care and drug costs but also results in increased disability, mortality, and sickness during the period of active labor force participation prior to retirement. The latter costs represent important drags on the economic system and are termed indirect economic costs. Elsewhere, we have developed some of the linkages and relationships that lead to these economic costs in great detail.38 The range of pathways linking the nutrition transition in China to health and economic costs must include the effects of diet and activity indirectly through obesity, as well as directly on a range of NCDs. A detailed review of the documentation for each pathway and the relative and attributable risks of each pathway is found elsewhere.39 Essentially, the bulk of the research in this field has focused on the biological relationships between obesity, hypertension, dislipidemias, and insulin resistance and in turn of these factors on heart disease and cancer. However, there are other equally important ways that childhood factors, nutrition, and physical activity may affect the costs of NCDs. These include the effects of diet directly on the NCDs, the effects of physical activity directly on these conditions, and the effects of energy imbalance via dietary patterns and physical activity on obesity. The potential for some effects of fetal insults during the fetal and infant development period on either obesity or directly on these NCDs are included.
Using current prevalence data for most of the key nutritional, physical activity, and mortality patterns—as well as available retirement age and medical care costs for China—the economic costs are predicted to be very large. The rate of change in overweight and obesity in China has accelerated over the past decade and even the most conservative assumptions would have this double over the next two decades. The full effects of being unhealthy, immobile, and sick on the current productive economic sector in China are not fully known, but conservative estimates would predict that lost work time will rise as diabetes, osteoarthritis, and many other debilitating conditions increase. Based on fairly conservative assumption, the total impact of these nutrition-related components of poor diets, inactivity, and obesity on NCD medical costs, labor productivity, and national production are very large. In the Chinese case study, the indirect effects of obesity and obesity-related dietary and physical activity patterns range between 3.58% and 8.73% of GNP in 2000 and 2025, respectively.40 These assumptions do not include much of the recent rapid increase in use and cost for pharmaceutical products; the full costs are even greater when these are included.41
Discussion
China is not unique, but its importance in the Asian and the global economy is great. Clearly this same transition in diet, activity, and obesity and related health care and other costs is already affecting the middle East and many other South East Asian and Latin American countries.42 Moreover, these changes appear to be penetrating most countries in the developing world.43 In general rates of change, total worsening dietary and physical activity patterns and increased obesity are greater in many developing and transitional countries than in higher-income ones.44
There is no clear way to fully forecast the health care costs of China’s transition toward a lifestyle linked with nutrition-related NCDs. The current trajectory can not measure the role pharmaceuticals might play—both in economic costs and in impact on the overall economy as the available data do not measure pharmaceutical usage.45 Treatment of hypertension and many other treatable NCDs is low now but are expected to increase.46 Nonetheless, the costs of treating diseases such as diabetes are enormous; a more aggressive system of treatment would most certainly increase health care costs. Studies in China do not exist, that allow us to totally understand the exact impact of obesity on productivity, absenteeism, and retirement in that country. Without them, one must rely on studies undertaken in other countries. This leads to a note of caution about some of the results. This brief layout can certainly provide a strong case for public investment to find ways to improve the dietary, activity, and body composition patterns in China and other developing countries. However, it is very clear that from the individual perspective, having a tastier higher-fat and sweetened diet is desirable. Similarly, a reduction in stressful activity in market and home production is desired. The critical issue is finding effective social investments and regulations that will (a) enhance the components of lifestyle that will reduce these problems and (b) provide for a healthier population. Possible solutions in the food system and physical environment are critical factors to consider.
Issues to be addressed from the food sector include (a) learning how to increase the intake levels of fruit, vegetables, and higher fibre products and (b) reducing the intake of caloric sweeteners and fat. We should note that there is great controversy about the need to reduce total fat intake or only reduce the intake of selected types of fats (i.e., transfatty acids, erucic acid, and saturated fats).47 Clearly all agree that the removal of carcinogenic or artherogenic edible oils is important, but the role of total fat is not as clear. Similarly, there is some debate about the role of caloric sweeteners. For instance, an expert committee of the World Health Organization (WHO) has recommended a maximum of 10% of energy from caloric sweeteners—a level above that of caloric sweeteners consumed in diets in high-, low-, and moderate-income countries.48 In contrast, the U.S. Institute of Medicine conducted the same review and concluded that 25% of energy from caloric sweeteners was acceptable.49
Similar shifts in the physical environment to enhance physical activity exist. There is a growing body of knowledge that points to the role of a spread of environmental factors ranging (a) from connectivity of streets to availability of walking options and (b) from street safety to the organisation and layout of buildings and communities. Higher density of, and proximity to, opportunities for physical activity, such as recreation facilities (e.g., private and public facilities, parks, recreation centres, green spaces, and shopping centres) and transportation options (e.g., sidewalks, cycle paths, public transportation, high road connectivity, and lower automobile transportation density) will increase physical activity levels and decrease overweight prevalence. Conversely, constraints to physical activity (e.g., crime and air pollution) will decrease physical activity and increase overweight prevalence.
For each of the desired changes in the food supply and the physical environment, there are clearly a myriad of options, some easy to implement and many quite complex. A few countries are already beginning to take some steps to address these issues.50 There have also been some limited successes in the higher-income countries of the world.51 Few other major attempts are being made to address this problem in the scale needed to decrease or reverse this epidemic. This paper provides some sense of how the epidemic will affect one country (i.e., China) if it does not begin to take radical corrective action.
Acknowledgments
We also wish to thank Ms. Frances L. Dancy for administrative assistance, Mr. Tom Swasey for graphics support, and Dr. Du Shufa and Ms. Tracy Dearth-Wesley for research assistance.
Footnotes
Conflict of Interest
Barry Popkin has no financial interests with other people or organizations that could inappropriately influence (bias) this paper.
References
- 1.World Bank. World Development Indicators. Washington DC: World Bank; 2005. [Google Scholar]
- 2.Bureau of State Statistics. China Statistical Yearbook 2000. Beijing: China Statistical Press; 2001. [Google Scholar]; Bureau of State Statistics. China Statistical Yearbook 2004. Beijing: China Statistical Press; 2004. [Google Scholar]
- 3.Blumenthal D, Hsiao W. Privatization and its discontents--the evolving Chinese health care system. New England Journal of Medicine. 2005;353(11):1165–1170. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal Privatization and its discontents--the evolving Chinese health care system. 2005 doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 5.Ge K, et al. The dietary and nutritional status of Chinese population: 1992 National Nutrition Survery. Vol. 1. Beijing: People’s Medical Publishing House; 1996. [Google Scholar]
- 6.Zhai F, et al. Evaluation of the 24-hour individual recall method in China. Food and Nutrition Bulletin. 1996;17:154–161. [Google Scholar]; Popkin BM, et al. Understanding the nutrition transition: measuring rapid dietary changes in transitional countries. Public Health Nutrition. 2002;5(1A):947–953. doi: 10.1079/PHN2002370. [DOI] [PubMed] [Google Scholar]
- 7.Du S, et al. A new stage of the nutrition transition in China. Public Health Nutrition. 2002;5(1A):169–174. doi: 10.1079/PHN2001290. [DOI] [PubMed] [Google Scholar]; Piazza A. Food consumption and nutritional status in the PRC. Boulder, Co; Westview: 1986. [Google Scholar]; Popkin BM, et al. The nutrition transition in China: a cross-sectional analysis. European Journal of Clinical Nutrition. 1993;47(5):333–346. [PubMed] [Google Scholar]
- 8.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutrition Reviews. 1997;55(2):31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 9.Wallingford JC, et al. Fatty acids in Chinese edible oils: Evidence for unexpected impact in changing diet. Food and Nutrition Bulletin. 2004;25:330–336. doi: 10.1177/156482650402500402. [DOI] [PubMed] [Google Scholar]
- 10.Du S, et al. Rapid income growth adversely affects diet quality in China--particularly for the poor! Social Science and Medicine. 2004;59(7):1505–1515. doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 11.Du S, et al. Rapid income growth adversely affects diet quality in China--particularly for the poor! 2004 doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 12.Delgado CL, et al. Livestock to 2020: The Revolution Continues. Paper presented at the annual meetings of the International Agricultural Trade Research Consortium (IATRC); Auckland, New Zealanded. 2001. [Google Scholar]; Delgado CL. Rising consumption of meat and milk in developing countries has created a new food revolution. Journal of Nutrition. 2003;133(11 Suppl 2):3907S–3910S. doi: 10.1093/jn/133.11.3907S. [DOI] [PubMed] [Google Scholar]
- 13.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. Journal of Nutrition. 2003;133(11 Suppl 2):3898S–3906S. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. 2003 doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]; Du S, et al. Rapid income growth adversely affects diet quality in China--particularly for the poor. 2004 doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]; Guo X, et al. Structural changes in the impact of income on food consumption in China, 1989–93. Economic Development and Cultural Change. 2000;48:737–760. [Google Scholar]
- 15.Brownell K, Horgan K. Food fight: The inside story of the food industry, America’s obesity crisis, and what we can do about it. New York: Contemporary Books; 2004. [Google Scholar]; Adair LS, Popkin BM. Are child eating patterns being transformed globally? Obesity Research. 2005;13(7):1281–1299. doi: 10.1038/oby.2005.153. [DOI] [PubMed] [Google Scholar]
- 16.Reardon T, Berdegué JA. The rapid rise of supermarkets in Latin America: challenges and opportunities for development. Development and Policy Review. 2002;20:371–388. [Google Scholar]
- 17.Hu D, et al. The emergence of supermarkets with Chinese characteristics: challenges and opportunities for China’s agricultural development. Development and Policy Review. 2004;22:557–686. [Google Scholar]
- 18.Hu D, et al. The emergence of supermarkets with Chinese characteristics: challenges and opportunities for China’s agricultural development. 2004 [Google Scholar]
- 19.Adair LS. Are child eating patterns being transformed globally? 2005 doi: 10.1038/oby.2005.153. [DOI] [PubMed] [Google Scholar]
- 20.Adair LA, Popkin BM. Are child eating patterns being transformed globally? Obesity Research. 2005;13(7):1281–1299. doi: 10.1038/oby.2005.153. [DOI] [PubMed] [Google Scholar]
- 21.Popkin BM. Urbanization, lifestyle changes and the nutrition transition. World Development. 1999;27:1905–1916. [Google Scholar]
- 22.Bell AC, et al. Weight gain and its predictors in Chinese adults. International Journal of Obesity and Related Metabolic Disorders. 2001;25(7):1079–1086. doi: 10.1038/sj.ijo.0801651. [DOI] [PubMed] [Google Scholar]
- 23.Bell AC, et al. Weight gain and its predictors in Chinese adults. 2001. [DOI] [PubMed] [Google Scholar]; Monda KL, Popkin BM. Longitudinal relationships between occupational and domestic physical activity patterns and overweight status in China. Chapel Hill: Carolina Population Center; 2006. Unpublished manuscript. [Google Scholar]
- 24.Bell AC, et al. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obesity Research. 2002;10(4):277–283. doi: 10.1038/oby.2002.38. [DOI] [PubMed] [Google Scholar]
- 25.Du S, et al. A new stage of the nutrition transition in China. 2002 doi: 10.1079/PHN2001290. [DOI] [PubMed] [Google Scholar]
- 26.Popkin BM. An overview on the nutrition transition and its health implications: the Bellagio meeting. Public Health Nutrition. 2002;5(1A):93–103. doi: 10.1079/phn2001280. [DOI] [PubMed] [Google Scholar]; Popkin BM. The nutrition transition in the developing world. Development Policy Review. 2003;21(5):581–597. [Google Scholar]
- 27.Cole TJ, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]; Popkin BM, et al. Is there a lag globally in overweight trends for children as compared to adults? Obesity. 2006;14:1846–1853. doi: 10.1038/oby.2006.213. [DOI] [PubMed] [Google Scholar]
- 28.Popkin BM, et al. Is there a lag globally in overweight trends for children as compared to adults? 2006 doi: 10.1038/oby.2006.213. [DOI] [PubMed] [Google Scholar]
- 29.Monteiro CA, et al. Obesity and inequities in health in the developing world. International Journal of Obesity and Related Metabolic Disorders. 2004;28(9):1181–1186. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]; Monteiro CA, et al. Socioeconomic status and obesity in adult populations of developing countries: a review. Bulletin World Health Organization. 2004;82(12):940–946. [PMC free article] [PubMed] [Google Scholar]
- 30.Monteiro CA, et al. Obesity and inequities in health in the developing world. 2004 doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 31.Du S, et al. Rapid income growth adversely affects diet quality in China--particularly for the poor. 2004 doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]; Guo, et al. Structural changes in the impact of income on food consumption in China, 1989–93. 2000 [Google Scholar]
- 32.Wang H, et al. Trends in the distribution of body mass index among Chinese adults, aged 20–45 years (1989–2000) International Journal of Obesity. 2007;31:272–278. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- 33.Du S, et al. Rapid income growth adversely affects diet quality in China--particularly for the poor. 2004 doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]; Guo et al. Structural changes in the impact of income on food consumption in China, 1989–93. 2000 [Google Scholar]
- 34.Beaglehole R. Global cardiovascular disease prevention: time to get serious. Lancet. 2001;358(9282):661–663. doi: 10.1016/S0140-6736(01)05784-1. [DOI] [PubMed] [Google Scholar]; Ezzati M, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]; Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349(9061):1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 35.Popkin BM. Understanding Global Nutrition Dynamics as a step toward controlling cancer morbidity and mortality. Nature Reviews Cancer. 2007;247:61–67. doi: 10.1038/nrc2029. [DOI] [PubMed] [Google Scholar]; Critchley J, et al. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation. 2004;110(10):1236–1244. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]; Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. Lancet. 1998;352(9143):1801–1807. [PubMed] [Google Scholar]; Bell A, et al. Ethnic differences in the association between body mass index and hypertension. American Journal of Epidemiology. 2002;155(4):346–353. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 36.Blumenthal D. Privatization and its discontents--the evolving Chinese health care system. 2005 doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 37.Blumenthal D. Privatization and its discontents--the evolving Chinese health care system. 2005 doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 38.Popkin BM, et al. Trends in diet, nutritional status, and diet-related noncommunicable diseases in China and India: the economic costs of the nutrition transition. Nutrition Reviews. 2001;59(12):379–390. doi: 10.1111/j.1753-4887.2001.tb06967.x. [DOI] [PubMed] [Google Scholar]; Popkin BM, et al. The nutrition transition and prevention of diet-related chronic diseases in Asia and the Pacific. Food and Nutrition Bulletin. 2001;22(4 suppl):1–58. [Google Scholar]; Popkin BM, et al. Measuring the full economic costs of diet, physical activity, and obesity-related chronic diseases. Obesity Reviews. 2006;7(3):271–293. doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 39.Popkin BM. Measuring the full economic costs of diet, physical activity, and obesity-related chronic diseases. 2006 doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 40.Popkin BM. Measuring the full economic costs of diet, physical activity, and obesity-related chronic diseases. 2006 doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 41.Blumenthal D. Privatization and its discontents--the evolving Chinese health care system. 2005 doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 42.Popkin BM. The nutrition transition in the developing world. 2003 [Google Scholar]
- 43.Mendez M, et al. Overweight exceeds underweight among women in most developing countries. American Journal of Clinical Nutrition. 2005;81(3):714–721. doi: 10.1093/ajcn/81.3.714. [DOI] [PubMed] [Google Scholar]
- 44.Popkin BM. The nutrition transition in the developing world. 2003 [Google Scholar]
- 45.Blumenthal D. Privatization and its discontents--the evolving Chinese health care system. 2005 doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 46.Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. 1998 [PubMed] [Google Scholar]; Bell A. Ethnic differences in the association between body mass index and hypertension. 2002 doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 47.Bray GA, Popkin BM. Dietary fat intake does affect obesity! American Journal of Clinical Nutriton. 1998;68(6):1157–1173. doi: 10.1093/ajcn/68.6.1157. [DOI] [PubMed] [Google Scholar]; Willett WC. Is dietary fat a major determinant of body fat?” American. Journal of Clinical Nutrition. 1998;67(3 suppl):556S–562S. doi: 10.1093/ajcn/67.3.556S. [DOI] [PubMed] [Google Scholar]
- 48.WHO/FAO. Expert Consultation on Diet, Nutrition and the Prevention of Chronic DiseasesReport of the joint WHO/FAO expert consultation. Geneva: World Health Organization; 2003. [Google Scholar]
- 49.Panel on Dietary Reference Intakes for Micronutrients. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: The National Academies Press; 2002. [DOI] [PubMed] [Google Scholar]
- 50.Coitinho D, et al. What Brazil is doing to promote healthy diets and active lifestyles. Public Health Nutrition. 2002;5(1A):263–267. doi: 10.1079/phn2001302. [DOI] [PubMed] [Google Scholar]; Zhai F, et al. What is China doing in policy-making to push back the negative aspects of the nutrition transition? Public Health Nutrition. 2002;5(1A):269–273. doi: 10.1079/phn2001303. [DOI] [PubMed] [Google Scholar]
- 51.Puska P, et al. Influencing public nutrition for non-communicable disease prevention: from community intervention to national programme- experiences from Finland. Public Health Nutrition. 2002;5(1A):245–251. [PubMed] [Google Scholar]