Abstract
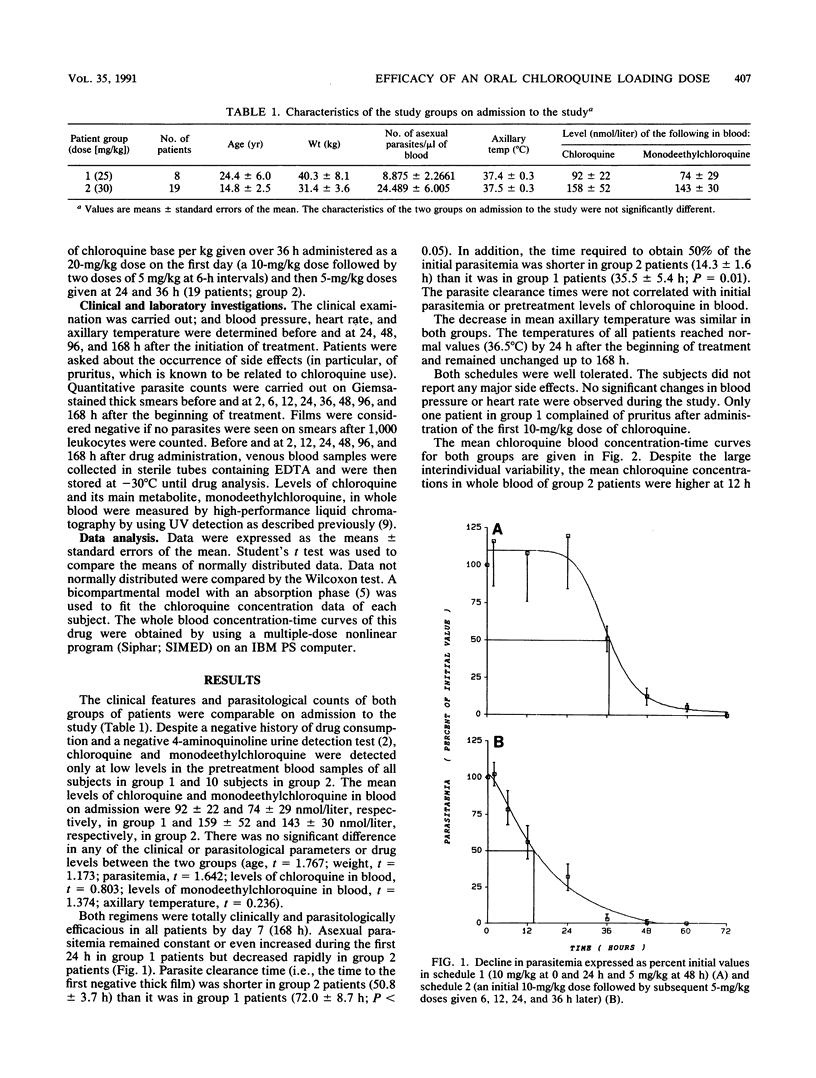
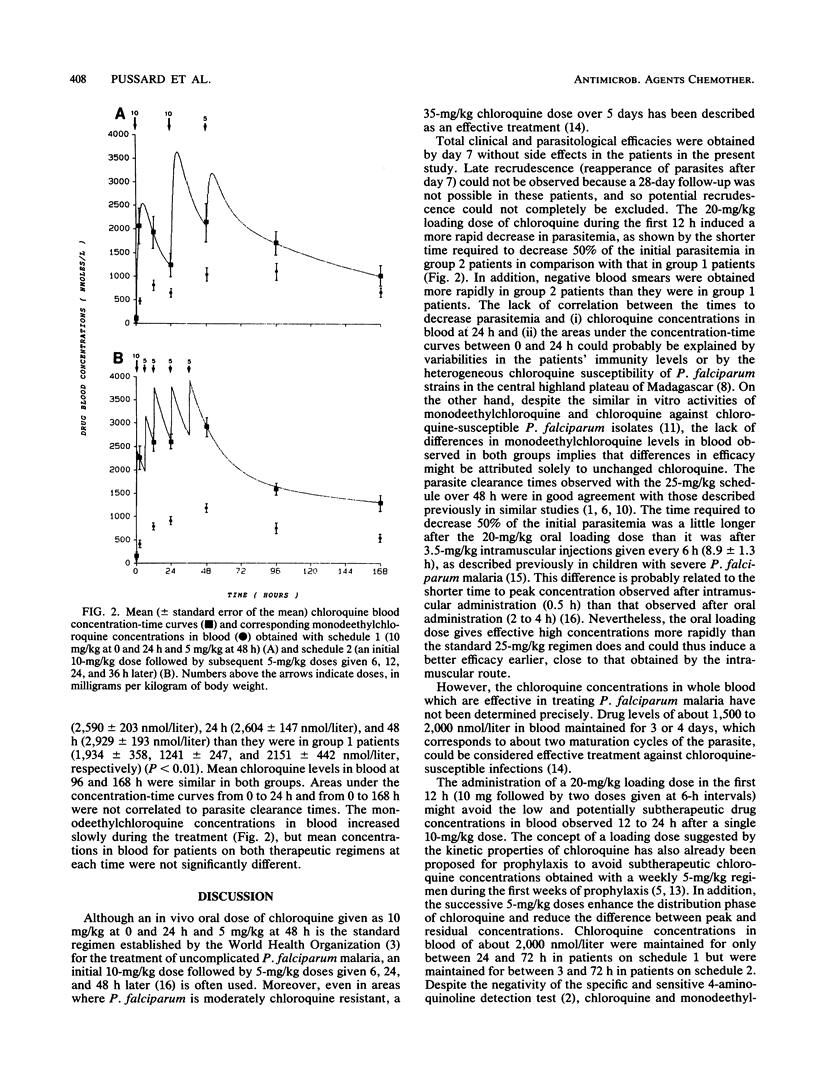
The efficacy of a loading dose of 20 mg of chloroquine per kg of body weight per os given at intervals during the first day was evaluated in 27 patients in Madagascar with Plasmodium falciparum malaria. The conventional regimen of 25 mg/kg over 3 days (schedule 1) was thus compared with a regimen of 30 mg/kg over 2 days (schedule 2; one dose of 10 mg/kg followed by two doses of 5 mg/kg at 6-h intervals on the first day and two doses of 5 mg/kg at 12-h intervals on the second day) in terms of their clinical and parasitological efficacies, tolerance, and drug concentration-time curves. At 24 h schedule 2 gave higher chloroquine levels in blood, which induced a more rapid decrease in parasitemia. The time required for a 50% decrease in the initial parasitemia was shorter in patients on schedule 2 (14.3 +/- 1.6 h) than it was in patients on schedule 1 (35.5 +/- 5.4 h; P less than 0.01). Moreover, negative blood smears were obtained more rapidly with schedule 2 (50.8 +/- 3.7 h) than with schedule 1 (72 +/- 8.7 h). As predicted by the drug concentration-time curve, no high, potentially toxic peak drug concentration appeared and no adverse effects were observed with the loading dose regimen (schedule 2). These findings support the idea that a loading dose of 20 mg/kg given at intervals during the first 12 h is well tolerated and can be used to obtain a more rapid decrease in parasitemia and to shorten the treatment time of uncomplicated chloroquine-susceptible falciparum malaria in the field.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adelusi S. A., Dawodu A. H., Salako L. A. Kinetics of the uptake and elimination of chloroquine in children with malaria. Br J Clin Pharmacol. 1982 Oct;14(4):483–487. doi: 10.1111/j.1365-2125.1982.tb02016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergqvist Y., Hed C., Funding L., Suther A. Determination of chloroquine and its metabolites in urine: a field method based on ion-pair extraction. Bull World Health Organ. 1985;63(5):893–898. [PMC free article] [PubMed] [Google Scholar]
- Frisk-Holmberg M., Bergqvist Y., Termond E., Domeij-Nyberg B. The single dose kinetics of chloroquine and its major metabolite desethylchloroquine in healthy subjects. Eur J Clin Pharmacol. 1984;26(4):521–530. doi: 10.1007/BF00542151. [DOI] [PubMed] [Google Scholar]
- Hellgren U., Kihamia C. M., Mahikwano L. F., Björkman A., Eriksson O., Rombo L. Response of Plasmodium falciparum to chloroquine treatment: relation to whole blood concentrations of chloroquine and desethylchloroquine. Bull World Health Organ. 1989;67(2):197–202. [PMC free article] [PubMed] [Google Scholar]
- Lepers J. P., Deloron P., Fontenille D., Coulanges P. Reappearance of falciparum malaria in central highland plateaux of Madagascar. Lancet. 1988 Mar 12;1(8585):586–586. doi: 10.1016/s0140-6736(88)91375-x. [DOI] [PubMed] [Google Scholar]
- Lepers J. P., Deloron P., Mouden J. C., Le Bras J., Coulanges P. Sudden increase in number of isolates of Plasmodium falciparum resistant to chloroquine in Madagascar. Trans R Soc Trop Med Hyg. 1989 Jul-Aug;83(4):491–492. doi: 10.1016/0035-9203(89)90263-0. [DOI] [PubMed] [Google Scholar]
- Pussard E., Verdier F., Blayo M. C. Simultaneous determination of chloroquine, amodiaquine and their metabolites in human plasma, red blood cells, whole blood and urine by column liquid chromatography. J Chromatogr. 1986 Jan 10;374(1):111–118. doi: 10.1016/s0378-4347(00)83258-2. [DOI] [PubMed] [Google Scholar]
- Sexton J. D., Deloron P., Bugilimfura L., Ntilivamunda A., Neill M. Parasitologic and clinical efficacy of 25 and 50 mg/kg of chloroquine for treatment of Plasmodium falciparum malaria in Rwandan children. Am J Trop Med Hyg. 1988 Mar;38(2):237–243. doi: 10.4269/ajtmh.1988.38.237. [DOI] [PubMed] [Google Scholar]
- Verdier F., Le Bras J., Clavier F., Hatin I. Blood levels and in vitro activity of desethylchloroquine against Plasmodium falciparum. Lancet. 1984 May 26;1(8387):1186–1187. doi: 10.1016/s0140-6736(84)91436-3. [DOI] [PubMed] [Google Scholar]
- Walker O., Dawodu A. H., Adeyokunnu A. A., Salako L. A., Alvan G. Plasma chloroquine and desethylchloroquine concentrations in children during and after chloroquine treatment for malaria. Br J Clin Pharmacol. 1983 Dec;16(6):701–705. doi: 10.1111/j.1365-2125.1983.tb02244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White N. J. Drug treatment and prevention of malaria. Eur J Clin Pharmacol. 1988;34(1):1–14. doi: 10.1007/BF01061409. [DOI] [PubMed] [Google Scholar]
- White N. J., Krishna S., Waller D., Craddock C., Kwiatkowski D., Brewster D. Open comparison of intramuscular chloroquine and quinine in children with severe chloroquine-sensitive falciparum malaria. Lancet. 1989 Dec 2;2(8675):1313–1316. doi: 10.1016/s0140-6736(89)91918-1. [DOI] [PubMed] [Google Scholar]
- White N. J. Loading dose in antimalarial prophylaxis. Trans R Soc Trop Med Hyg. 1985;79(5):742–742. doi: 10.1016/0035-9203(85)90218-4. [DOI] [PubMed] [Google Scholar]
- White N. J., Watt G., Bergqvist Y., Njelesani E. K. Parenteral chloroquine for treating falciparum malaria. J Infect Dis. 1987 Feb;155(2):192–201. doi: 10.1093/infdis/155.2.192. [DOI] [PubMed] [Google Scholar]


