Abstract
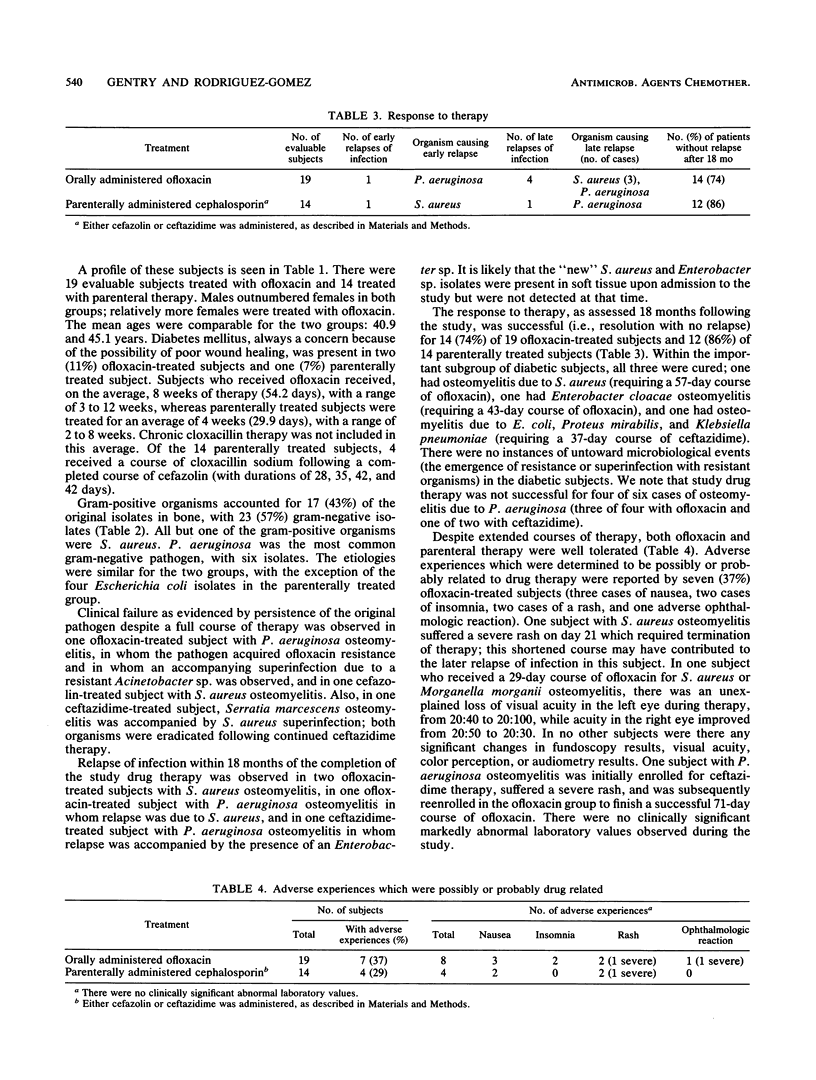
We conducted a randomized comparison of oral ofloxacin (400 mg twice a day) and parenteral agents (cefazolin, 1.0 g intravenously every 8 h, or ceftazidime, 2.0 g intravenously every 12 h) in biopsy-confirmed, nonprosthesis osteomyelitis. A total of 19 subjects received ofloxacin for an average of 8 weeks, and 14 received parenteral antibiotics for an average of 4 weeks; both therapies were well tolerated. Infections were due to Staphylococcus aureus (40%), Enterococcus spp. (3%), Pseudomonas aeruginosa (15%), and other gram-negative organisms (42%). At the completion of therapy, one P. aeruginosa infection in the ofloxacin group persisted and the organism acquired resistance, accompanied by a resistant Acinetobacter superinfection. In the parenteral group, one S. aureus infection persisted, and there was a resolved superinfection due to S. aureus as well. Eighteen-month follow-up data have been obtained. Among those treated with ofloxacin, four subjects whose initial response to therapy was successful suffered relapses of infection, three due to S. aureus and one due to P. aeruginosa, while in the parenteral group, one subject with a P. aeruginosa infection relapsed. Long-term response to therapy was successful for 14 of 19 (74%) subjects who received ofloxacin and 12 of 14 (86%) who received parenteral antibiotics; the difference was not significant. Oral ofloxacin appears comparable to parenteral antibiotics in chronic osteomyelitis due to susceptible organisms, and oral ofloxacin offers advantages in economics and convenience.
Full text
PDF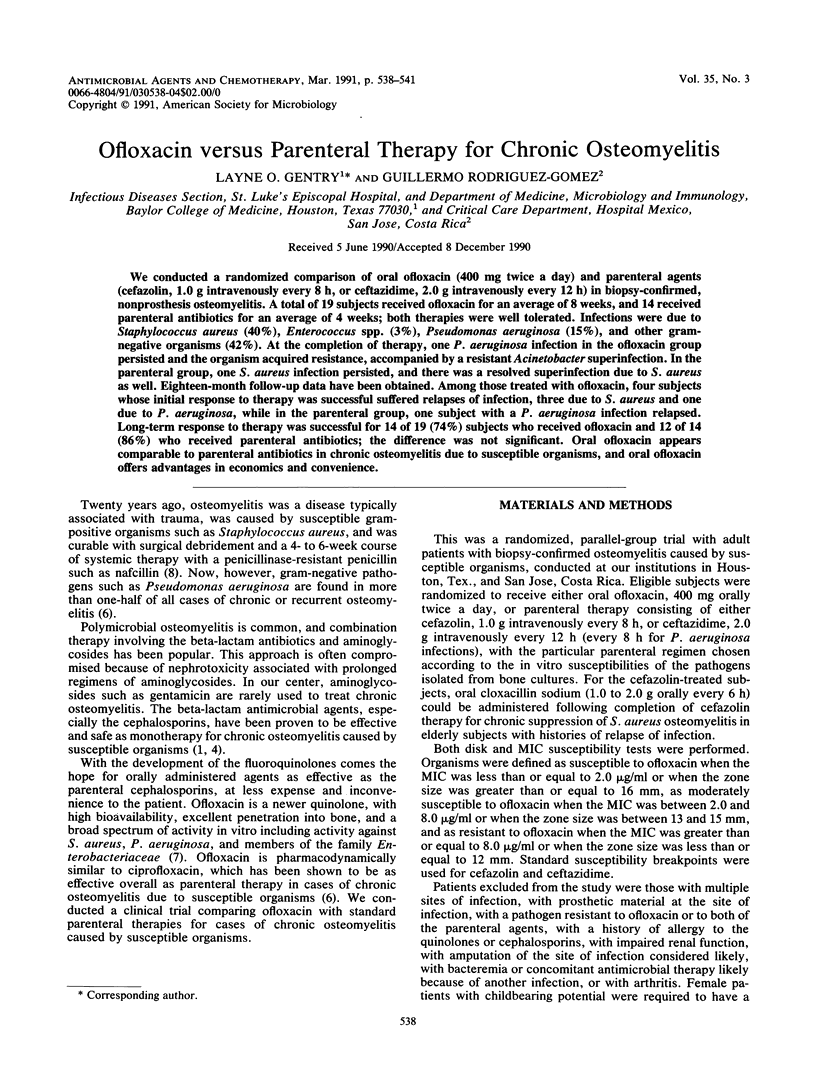

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bach M. C., Cocchetto D. M. Ceftazidime as single-agent therapy for gram-negative aerobic bacillary osteomyelitis. Antimicrob Agents Chemother. 1987 Oct;31(10):1605–1608. doi: 10.1128/aac.31.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalkley L. J., Koornhof H. J. Antimicrobial activity of ciprofloxacin against Pseudomonas aeruginosa, Escherichia coli, and Staphylococcus aureus determined by the killing curve method: antibiotic comparisons and synergistic interactions. Antimicrob Agents Chemother. 1985 Aug;28(2):331–342. doi: 10.1128/aac.28.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fass R. J. Treatment of osteomyelitis and septic arthritis with cefazolin. Antimicrob Agents Chemother. 1978 Mar;13(3):405–411. doi: 10.1128/aac.13.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentry L. O. Approach to the patient with chronic osteomyelitis. Curr Clin Top Infect Dis. 1987;8:62–83. [PubMed] [Google Scholar]
- Gentry L. O., Rodriguez G. G. Oral ciprofloxacin compared with parenteral antibiotics in the treatment of osteomyelitis. Antimicrob Agents Chemother. 1990 Jan;34(1):40–43. doi: 10.1128/aac.34.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldvogel F. A., Medoff G., Swartz M. N. Osteomyelitis: a review of clinical features, therapeutic considerations and unusual aspects (second of three parts). N Engl J Med. 1970 Jan 29;282(5):260–266. doi: 10.1056/NEJM197001292820507. [DOI] [PubMed] [Google Scholar]


