Abstract
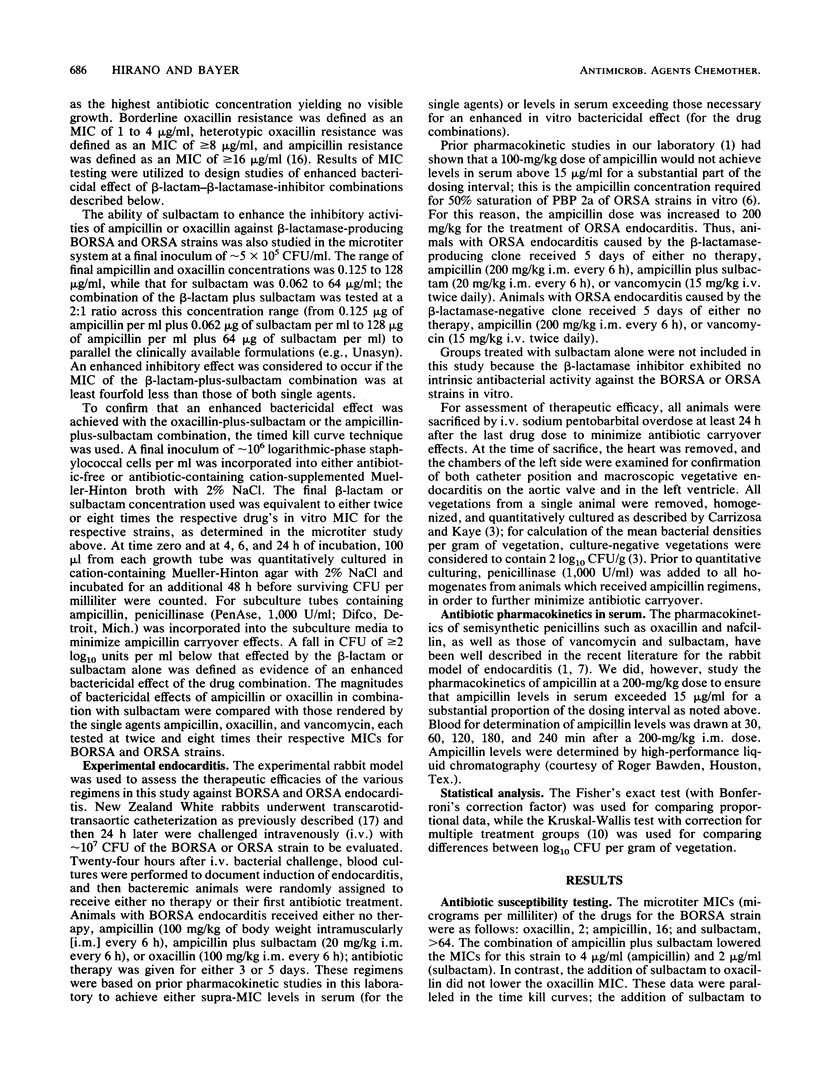
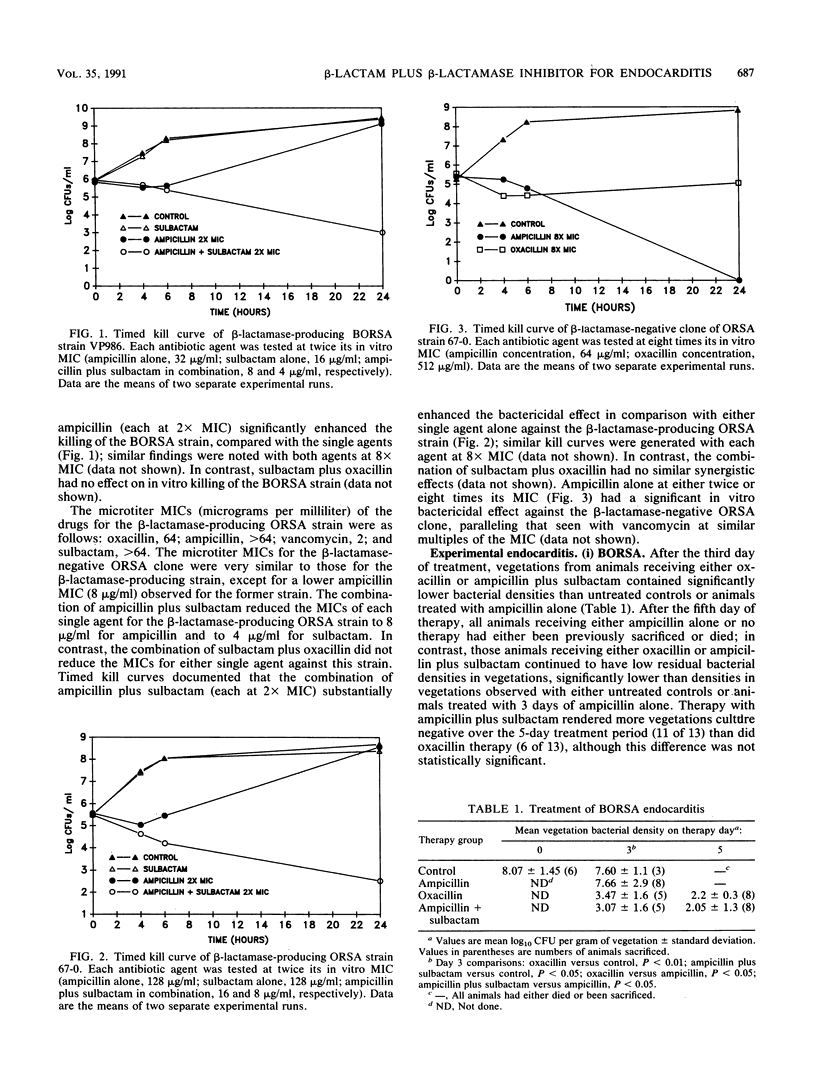
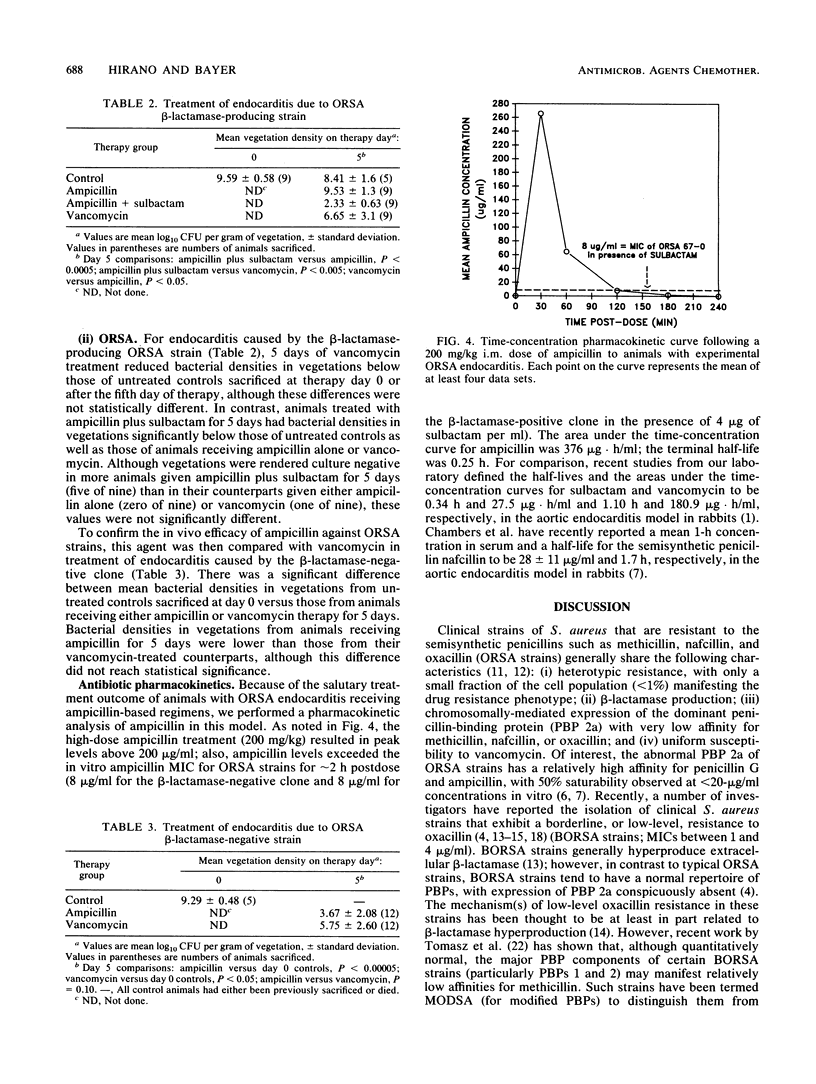
Optimal therapeutic strategies for serious infections caused by borderline and heterotypic oxacillin-resistant Staphylococcus aureus (BORSA and ORSA) strains have not been fully characterized. Recent evidence suggests that the dominant penicillin-binding protein of ORSA strains (PBP 2a) shows good affinity for ampicillin and that these strains commonly produce beta-lactamase. Therefore, we compared the in vivo efficacy of the combination of ampicillin plus sulbactam with that of vancomycin against ORSA strains. Also, the moderate resistance of BORSA strains appears to be attributable mainly to the hyperproduction of beta-lactamase. Therefore, we also studied the in vivo efficacy of ampicillin plus sulbactam against such organisms. Experimental aortic endocarditis was induced in rabbits by the following three strains: beta-lactamase-producing BORSA strain VP-986, beta-lactamase-producing ORSA strain 67-0, and its beta-lactamase-negative clone. In animals with BORSA endocarditis, ampicillin plus sulbactam and oxacillin were highly effective in reducing mean intravegetation bacterial densities, with each being significantly better than either ampicillin alone or no therapy. In animals with endocarditis caused by the beta-lactamase-producing ORSA strain, ampicillin plus sulbactam was significantly better at reducing mean vegetation bacterial densities than the other regimens. For endocarditis caused by the beta-lactamase-negative ORSA clone, ampicillin was better than vancomycin in reducing mean intravegetation bacterial densities. These data show that infections caused by beta-lactamase-producing BORSA strains respond therapeutically in a manner similar to that of infections caused by oxacillin-susceptible strains, with both oxacillin and ampicillin plus sulbactam being highly efficacious. Moreover, high-dose ampicillin treatment strategies were effective in the therapy of ORSA endocarditis; this efficacy is presumably related to the relatively high affinity profile of this compound (compare with that of oxacillin) for the functionally dominant ORSA PBP 2a.
Full text
PDF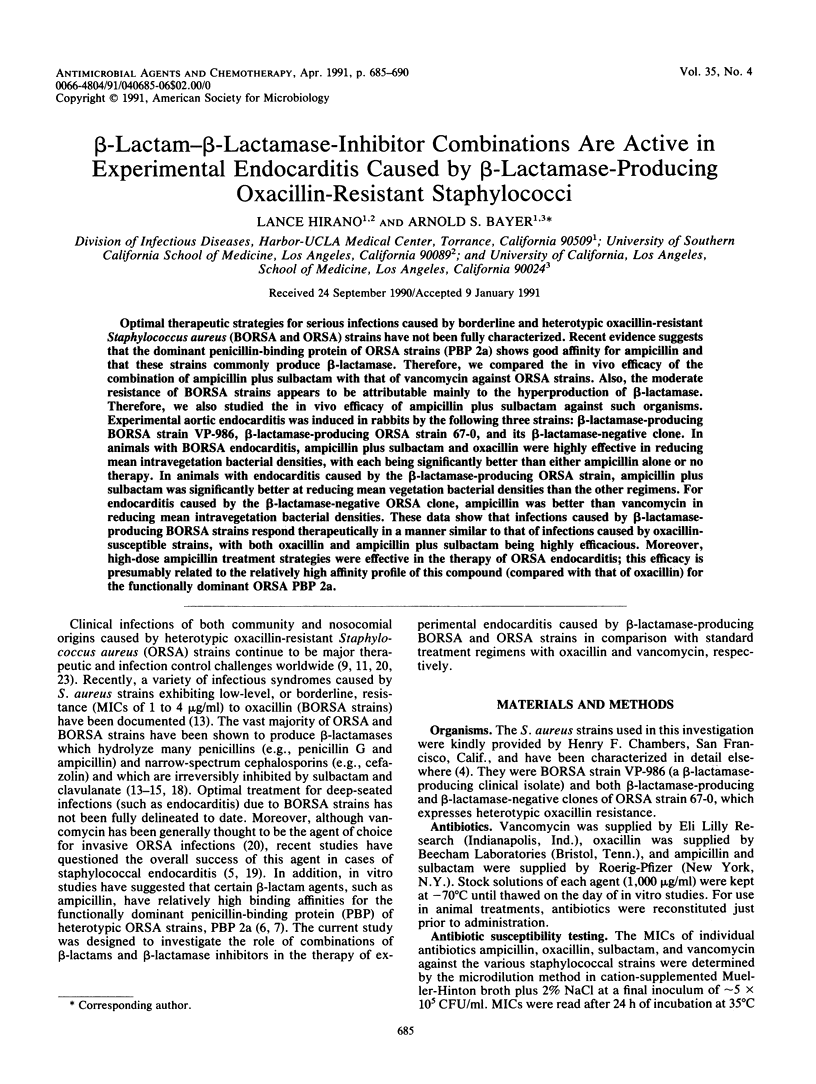

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bayer A. S., Tu J. Chemoprophylactic efficacy against experimental endocarditis caused by beta-lactamase-producing, aminoglycoside-resistant enterococci is associated with prolonged serum inhibitory activity. Antimicrob Agents Chemother. 1990 Jun;34(6):1068–1074. doi: 10.1128/aac.34.6.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantoni L., Wenger A., Glauser M. P., Bille J. Comparative efficacy of amoxicillin-clavulanate, cloxacillin, and vancomycin against methicillin-sensitive and methicillin-resistant Staphylococcus aureus endocarditis in rats. J Infect Dis. 1989 May;159(5):989–993. doi: 10.1093/infdis/159.5.989. [DOI] [PubMed] [Google Scholar]
- Carrizosa J., Kaye D. Antibiotic synergism in enterococcal endocarditis. J Lab Clin Med. 1976 Jul;88(1):132–141. [PubMed] [Google Scholar]
- Chambers H. F., Archer G., Matsuhashi M. Low-level methicillin resistance in strains of Staphylococcus aureus. Antimicrob Agents Chemother. 1989 Apr;33(4):424–428. doi: 10.1128/aac.33.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers H. F., Miller R. T., Newman M. D. Right-sided Staphylococcus aureus endocarditis in intravenous drug abusers: two-week combination therapy. Ann Intern Med. 1988 Oct 15;109(8):619–624. doi: 10.7326/0003-4819-109-8-619. [DOI] [PubMed] [Google Scholar]
- Chambers H. F., Sachdeva M. Binding of beta-lactam antibiotics to penicillin-binding proteins in methicillin-resistant Staphylococcus aureus. J Infect Dis. 1990 Jun;161(6):1170–1176. doi: 10.1093/infdis/161.6.1170. [DOI] [PubMed] [Google Scholar]
- Cremieux A. C., Maziere B., Vallois J. M., Ottaviani M., Azancot A., Raffoul H., Bouvet A., Pocidalo J. J., Carbon C. Evaluation of antibiotic diffusion into cardiac vegetations by quantitative autoradiography. J Infect Dis. 1989 May;159(5):938–944. doi: 10.1093/infdis/159.5.938. [DOI] [PubMed] [Google Scholar]
- Crossley K., Loesch D., Landesman B., Mead K., Chern M., Strate R. An outbreak of infections caused by strains of Staphylococcus aureus resistant to methicillin and aminoglycosides. I. Clinical studies. J Infect Dis. 1979 Mar;139(3):273–279. doi: 10.1093/infdis/139.3.273. [DOI] [PubMed] [Google Scholar]
- Hackbarth C. J., Chambers H. F. Methicillin-resistant staphylococci: detection methods and treatment of infections. Antimicrob Agents Chemother. 1989 Jul;33(7):995–999. doi: 10.1128/aac.33.7.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackbarth C. J., Chambers H. F. Methicillin-resistant staphylococci: genetics and mechanisms of resistance. Antimicrob Agents Chemother. 1989 Jul;33(7):991–994. doi: 10.1128/aac.33.7.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massanari R. M., Pfaller M. A., Wakefield D. S., Hammons G. T., McNutt L. A., Woolson R. F., Helms C. M. Implications of acquired oxacillin resistance in the management and control of Staphylococcus aureus infections. J Infect Dis. 1988 Oct;158(4):702–709. doi: 10.1093/infdis/158.4.702. [DOI] [PubMed] [Google Scholar]
- McDougal L. K., Thornsberry C. The role of beta-lactamase in staphylococcal resistance to penicillinase-resistant penicillins and cephalosporins. J Clin Microbiol. 1986 May;23(5):832–839. doi: 10.1128/jcm.23.5.832-839.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montanari M. P., Tonin E., Biavasco F., Varaldo P. E. Further characterization of borderline methicillin-resistant Staphylococcus aureus and analysis of penicillin-binding proteins. Antimicrob Agents Chemother. 1990 May;34(5):911–913. doi: 10.1128/aac.34.5.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman B. B., Freedman L. R. Experimental endocarditis. II. Staphylococcal infection of the aortic valve following placement of a polyethylene catheter in the left side of the heart. Yale J Biol Med. 1971 Oct;44(2):206–213. [PMC free article] [PubMed] [Google Scholar]
- Sierra-Madero J. G., Knapp C., Karaffa C., Washington J. A. Role of beta-lactamase and different testing conditions in oxacillin-borderline-susceptible staphylococci. Antimicrob Agents Chemother. 1988 Dec;32(12):1754–1757. doi: 10.1128/aac.32.12.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small P. M., Chambers H. F. Vancomycin for Staphylococcus aureus endocarditis in intravenous drug users. Antimicrob Agents Chemother. 1990 Jun;34(6):1227–1231. doi: 10.1128/aac.34.6.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorrell T. C., Packham D. R., Shanker S., Foldes M., Munro R. Vancomycin therapy for methicillin-resistant Staphylococcus aureus. Ann Intern Med. 1982 Sep;97(3):344–350. doi: 10.7326/0003-4819-97-3-344. [DOI] [PubMed] [Google Scholar]
- Thauvin-Eliopoulos C., Rice L. B., Eliopoulos G. M., Moellering R. C., Jr Efficacy of oxacillin and ampicillin-sulbactam combination in experimental endocarditis caused by beta-lactamase-hyperproducing Staphylococcus aureus. Antimicrob Agents Chemother. 1990 May;34(5):728–732. doi: 10.1128/aac.34.5.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasz A., Drugeon H. B., de Lencastre H. M., Jabes D., McDougall L., Bille J. New mechanism for methicillin resistance in Staphylococcus aureus: clinical isolates that lack the PBP 2a gene and contain normal penicillin-binding proteins with modified penicillin-binding capacity. Antimicrob Agents Chemother. 1989 Nov;33(11):1869–1874. doi: 10.1128/aac.33.11.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward T. T., Winn R. E., Hartstein A. I., Sewell D. L. Observations relating to an inter-hospital outbreak of methicillin-resistant Staphylococcus aureus: role of antimicrobial therapy in infection control. Infect Control. 1981 Nov-Dec;2(6):453–459. doi: 10.1017/s0195941700055715. [DOI] [PubMed] [Google Scholar]



