Abstract
Objective
Prior studies have shown a low rate of accurate identification by primary care physicians of mental health disorders in youth. This study tested the psychometric properties of two brief mental health screening questionnaires, the Mood and Feelings Questionnaire – Short Form (MFQ-SF) and Childhood Anxiety Sensitivity Index (ASI), in a large sample of youth.
Methods
In a sample of 1375 youth age 11 to 17 (779 with asthma, 596 randomly selected controls) enrolled in an HMO, the psychometric properties (optimum cutoffs on Receiver Operating Curve (ROC) curves, sensitivity, specificity, positive and negative predictive values) of two brief anxiety and depression screens were examined versus a “gold standard” structured psychiatric interview.
Results
Both the MFQ-SF and ASI performed well on ROC analysis for screening youth for one or more DSM-IV anxiety or depressive disorders. The MFQ-SF performed better on ROC analysis than the ASI for youth with major depression (area under the curve of 0.84 vs 0.77). For screening youth with anxiety disorders ROC curves showed that both the MFQ-SF and ASI only performed in the fair range (area under the curve of 0.76).
Conclusion
The MFQ-SF and ASI are two relatively brief questionnaires that performed well for screening youth for one or more DSM-IV anxiety or depressive disorders. The MFQ-SF performed better than the ASI for screening youth with major depression. Use of these instruments could increase the accuracy of identification of mental health disorders in youth by primary care physicians.
Keywords: anxiety, depression screening, chronic illness, asthma
Anxiety and depressive disorders affect approximately 10% of youth and increase in prevalence in teenage years.1, 2 Youth with medical disorders such as asthma and diabetes are at especially high risk with prevalence rates of meeting criteria for anxiety and depressive disorders that are two-fold higher than controls.3, 4 Anxiety and depressive disorders in youth are associated with unexplained physical symptoms such as abdominal pain and headaches5, impairment in social roles6, and increased risk for smoking, and obesity,7, 8 which may lead to increased medical utilization and costs.3
The primary care system provides an opportunity for early detection and treatment of anxiety and depressive disorders in youth. Unfortunately, despite the high prevalence of these disorders and their association with impairment in health and social roles, primary care physicians often fail to detect these disorders.9, 10 Studies of youth with anxiety and depressive disorders suggest that only about 20 to 30% are accurately identified by primary care physicians.9, 10 Among youth with chronic medical disorders who have more visits to primary care physicians, rates of accurate diagnosis may go up to 40%.10
Given the low rates of accurate diagnosis, brief anxiety and depression screening measures may enhance detection rates in primary care. A recent review found that self-report depression scales improved accuracy of diagnosis of depression in youth more than physician depression training programs alone.11 A recent study also suggested that universal screening of youth for depression in one, large private practice was feasible with both parents and practitioners, reporting high levels of satisfaction with screening.12 Yet compared to the extensive data on anxiety and depressive screening measures in adults13, 14, far less research on primary care mental health screening has been completed in youth. A recent review found only five studies with adequate data to assess the psychometric properties and validity of depression screens in youth in primary care settings.12
Because anxiety and depressive disorders are each extremely prevalent and often occur together in youth, a brief questionnaire that could screen for both disorders would be optimal for primary care physicians. In addition, researchers as well as organizations involved in quality improvement efforts may want to screen for only one of these two common disorders. Therefore, this paper will describe the sensitivity, specificity and positive and negative predictive value for the telephone administered Childhood Anxiety Sensitivity Index (ASI)15 and Mood and Feelings Questionnaire Short Form (MFQ-SF)16 in screening for meeting DSM-IV criteria for either an anxiety or depressive disorder as well as screening for one of these two disorders in a large sample of youth receiving care in a health maintenance organization (HMO). This large sample of youth were recruited as part of a study to determine the prevalence of anxiety and depressive disorders in youth with asthma versus controls without this common medical condition.17 Asthma was chosen because it is the most common chronic disorder in youth, is responsible for high utilization of primary care, and is associated with higher rates of anxiety and depressive disorders.3
METHODS
Setting
Group Health Cooperative (GHC) is a nonprofit HMO in Washington State with 25 GHC-owned primary care clinics as well as 75 contracted clinics. The study protocol was reviewed and approved by the institutional review board of GHC.
Subjects and Recruitment
Potential subjects between 11 and 17 years of age who were enrolled in GHC ≥6 months were identified from administrative data. All youth with asthma identified via GHC automated data based on physician ICD-9 asthma diagnoses and asthma medication prescriptions were approached for interview.17 The control sample of youth was required to have no evidence of asthma medication use or an ICD-9 diagnosis of asthma in the last 12 months. In each 4 to 6 week recruitment wave, each eligible control youth was assigned a unique number and the youth with the lowest 100 numbers were chosen. Following receipt of a letter inviting participation in the study and providing consent, subjects completed a telephone interview that included a 20-minute parent interview and 45- to 75-minute child/adolescent interview. For subjects who were aged 13 to 17 years, written informed consent was obtained for both the parent and the youth. Parental consent alone was obtained for youth younger than 13 years.
Data Collection
The parent interview included questions about demographics, asthma and child anxiety and depressive symptoms. The youth interview included the following measures of anxiety and depression. The Childhood Anxiety Sensitivity Index (ASI)15 is a 16-item self report measure that has been shown to have high reliability and validity.15, 18–20 The ASI assesses fear of anxiety symptoms and catastrophic cognitions regarding bodily sensations. Each item is rated on a 0 to 4 scale (“a little” to “very much”) with a range of 0 to 64. Scores on the ASI have been shown to be significantly higher in patients with anxiety and depressive disorders compared to controls.18–20 The Mood and Feelings Questionnaire Short Form (MFQ-SF)16 is a 13-item questionnaire that codes symptoms on a 3-point scale (“true”, “sometimes true”, “not true”) with a range of 0 to 26. This scale has been found to have high reliability and validity and the short form is made up of items that best discriminated depressed and non-depressed children in field trials using structured psychiatric interviews.16
All interviewers had at least a high school education and received 12 hours of classroom and hands-on training and additional, project-specific training on the C-DISC-4.0. Interview quality was continuously assessed through silent monitors installed on all telephones. Written feedback on errors, and corrective instruction were provided.
All youth also completed a telephone version of the Diagnostic Interview Schedule for Children NIMH DISC-4.0, a reliable and valid structured interview designed for lay interviewers, which includes algorithms to diagnose DSM-IV disorders in children and adolescents.21 Telephone versions of structured psychiatric interviews in both adults22 and youth23 have been found to have a high correlation with in-person interviews. To decrease patient burden, only selected DISC-4.0 depression modules (major depression, dysthymia) and anxiety modules (panic disorder, separation anxiety, social phobia, generalized anxiety disorder and agoraphobia) were used.
Statistical Analyses
We created standardized z scores (score-mean/standard deviation) on the 2 scales to account for different numbers of items and compared group means of standardized scores with the paired t-test. In order to determine the best screening cutoffs for the MFQ-SF and the ASI, we conducted psychometric analyses of the scales’ ability to classify a large sample of youth into those with either a DSM-IV-R depression and/or anxiety diagnosis in comparison to those youth not meeting criteria for a C-DISC diagnosis. We also conducted two separate psychometric analyses of each scale’s ability to classify the sample of youth into those with major depression (with or without anxiety) or those with an anxiety disorder (with or without a depressive disorder) in comparison to those not meeting these C-DISC diagnoses. The C-DISC DSM-IV-R diagnostic grouping was used as the gold standard for the ROC and other psychometric analyses.
All analyses were performed using STATA 8.0. We calculated the area under the receiver operator characteristic (ROC) curve as a quantification of the sensitivity and specificity of the self-report questionnaires’ ability to classify youths into the diagnostic categories. Standards have been set for interpreting the area under the curve: 0.90–1 = excellent; 0.80–0.90 = good (B); 0.70–0.80 = fair; 0.60–0.70 = poor; and 0.50–0.60 = fail (http://gim.unmc.edu/dxtests/Default.htm)
We used a Chi-square statistic to test the differences between the ROC curves for the two scales. A significant test at p < 0.05 would imply that one questionnaire had significantly better sensitivity and specificity than the other scale.
Cutoffs for the two questionnaire total scores were determined using the cut point that maximized the sensitivity and specificity. Sensitivity is the probability of a positive screening test given that the person has the disorder and specificity is the probability of having a negative screening test given that the patient does not have the disorder. If more than 1 cutoff had similar properties, we tested both of them. After optimum cutoffs were chosen using ROC analysis, the positive predictive value (PPV) and negative predictive value (NPV) of the cutoffs were calculated. The PPV is the probability of having the disease given a positive test and the NPV is the probability of not having the disease given a negative test. These indices are a function of both test properties and the prevalence of the disorder in the study population.24 The percent correctly classified is defined as those who have a disorder and were identified as having the disorder plus those who did not have a disorder and were classified not having the disorder divided by the total sample. It is related to the sensitivity and specificity of a measure in the following way: Rate of correct classification = (sensitivity × prevalence of disease) + (specificity × 1-prevalence of disease).
RESULTS
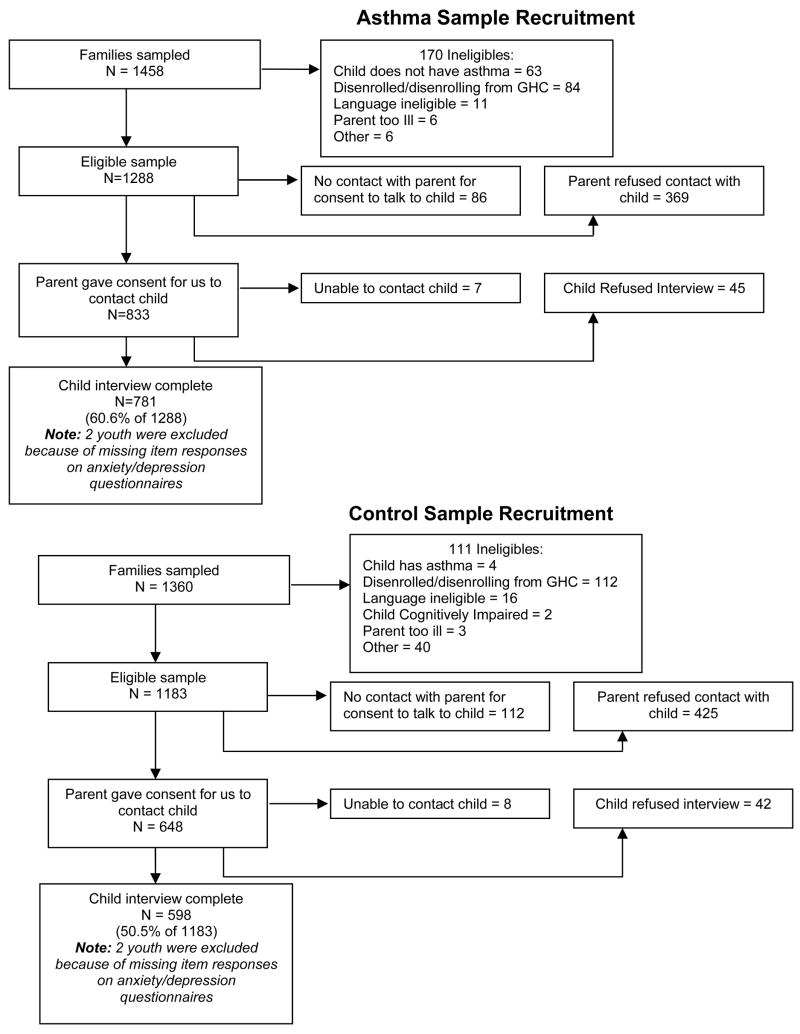
Of the 1458 youth with asthma in the initial sample, 1288 proved eligible (Figure 1) and 833 eligible parents gave consent for us to contact their child/adolescent with asthma. Of these, we completed 781 child/adolescent interviews for a final recruitment rate of 60.6%. Of the 1360 control youth without asthma, 1183 proved eligible and 648 eligible parents gave consent to contact their child/adolescent without asthma. We completed 598 control youth interviews for a recruitment rate of 50.5%. From the total sample of 1379, two youths with asthma and two control youth were missing too many item responses to be used in this analysis, so our sample in this paper included 1375 youth (N = 779 with asthma, N = 596 controls). A total of 652 (47%) were female, the mean age was 14.0 ± 1.9, and 1080 (78%) were Caucasian.
Figure 1.
Recruitment of Youth with Asthma and Controls
The prevalence of anxiety and/or depression diagnosis on the C-DISC was 13.4% (95% CI = 11.5% –15.2%) in this sample. As previously reported, 17.1% of youth with asthma and 8.6% of controls met criteria for ≥1 anxiety or depression diagnoses17 with 145 meeting criteria for an anxiety disorder, 83 for major depression or dysthymia (only 1 met criteria for dysthymia), and 45 for both, for a total of 183 with ≥1 anxiety and/or depression disorders.
Screening for Either a DSM-IV Anxiety or Depressive Disorder (Table 1)
Table 1.
Screening for anxiety or depression: psychometric properties of the Mood Feelings Questionnaire and the Anxiety Sensitivity Index in screening for either a DSM-IV anxiety or depressive disorder* in a combined sample of youth with and without asthma [Total N = 1375; N = 183 (13.3%) with ≥1 anxiety or depressive disorder]
| Mood Feelings | ASI | |
|---|---|---|
| Number of Items (response scoring option for each item) | 13 (0 – 2) | 16 (0 – 4) |
| Mean (SD) Median | 3.4 (4.5) | 11.0 (8.9) |
| 2.0 | 9.0 | |
| Internal Consistency Reliability – Coefficient Alpha | .88 | .88 |
| Area Under the Receiver Operating Curve† | .81 (95% CI,.77 –.84) | .79 (95% CI,.75 –.82) |
| Cutpoint Determined by Receiver | ||
| Operating Curve | ≥ 4 | ≥ 13 |
| Sensitivity | .77 (95% CI,.75 –.79) | .75 (95% CI,.73 –.77) |
| Specificity | .73 (95% CI,.70 –.75) | .70 (95% CI,.67 –.72) |
| Positive Predictive Value (%) (PPV) | 30.3 (95% CI, 27.9 – 34.7) | 27.6 (95% CI, 25.2 – 30.0) |
| Negative Predictive Value (%) (NPV) | 95.4 (95% CI, 94.3 – 96.5) | 94.7 (95% CI, 93.6 – 96.0) |
| Total % Correctly Classified | 73.3% | 70.3 |
| % Youth with Anxiety or Depression Correctly Classified | 72.8% | 69.6% |
| % Youth without Anxiety or Depression Correctly Classified | 77% | 75% |
Using the C-DISC any anxiety or depression as the gold standard
x2 (1) = 0.66, p = 0.42
The MFQ-SF is shorter than the ASI (13 compared to 16 items), however, both scales have similar distributions and psychometric properties. The differences in mean standardized scores between those with and without ≥1 anxiety or depression diagnoses were similar for both measures (paired group t test), indicating that they are both equally sensitive to mean group differences. Both demonstrate very good internal consistency reliability (Cronbach’s alpha = 0.88) and using cut points of ≥4 for the MFQ-SF and ≥13 for the ASI, both demonstrate good sensitivity and specificity (ROC area approximately 0.80) for ≥1 anxiety or depression diagnoses based on the C-DISC. The Chi square for the differences between the ROC curves was not statistically significant (p = 0.66).
At the above cutpoints, both scales have relatively low PPVs in the 30% range, with the MFQ-SF being slightly more predictive. NPVs were excellent for both instruments (95%). This corresponds to a correct classification rate of about 70% for those with an anxiety or depression diagnosis and about 76% correct classification for youth without a diagnosis.
Screening for Major Depression with or without Anxiety
Table 2 describes the performance of the MFQ-SF (the cutoff score of ≥ 6 was optimal for depression based on ROC analysis) and ASI in detecting youth with major depression or dysthymia (with or without anxiety disorders). The table shows that the MFQ-SF performs significantly better on the ROC analysis and demonstrates better sensitivity, specificity, PPV, and has a higher rate of correct classification compared to the ASI. The PPV is relatively low for both scales (12% to 22%), but the NPV is high (97% to 98%). The percent of youth (both DSM-IV cases and controls) correctly classified was 81% for the MFQ-SF and 66% for the ASI.
Table 2.
Screening for depression: psychometric properties of the Mood and Feelings Questionnaire and the Anxiety Sensitivity Index using the C-DISC depression diagnosis (with or without anxiety) as the gold standard in the combined sample of youth with and without asthma (Total N = 1375 with 83 (6.0%) with major depression).
| Mood Feelings | ASI | |
|---|---|---|
| Area Under the Receiver Operating Curve* | .84 (95% CI,.79 –.90) | .77 (95% CI,.72 –.82) |
| Cutpoint Determined by Receiver Operating Curve | ≥6 | ≥13 |
| Sensitivity | .80 (95% CI,.69 –.88) | .74 (95% CI,.73 –.77) |
| Specificity | .81 (95% CI,.77 –.84) | .66 (95% CI,.63 –.69) |
| Positive Predictive Value (%) (PPV) | 21.6 (95% CI, 17.1 – 26.6) | 12.2 (95% CI 9.5 – 15.4) |
| Negative Predictive Value (%) (NPV) | 98.4 (95% CI, 97.5 – 99.1) | 97.5 (95% CI, 96.2 – 98.4) |
| Total % Correctly Classified | 81.3% | 66.4% |
| % Youth with Depression Classified | 75.9 | 73.5% |
| % Youth without Depression Correctly Classified | 81.4% | 66.0% |
x2 (1) = 5.66, p = 0.02; MFQ > ASI
Screening for Anxiety Disorders with or without Depression
Table 3 describes the performance of the MFQ-SF and ASI in youth with anxiety (with and without depression). Both questionnaires performed similarly on the ROC analysis (ROC area = 0.76, within the fair range) and both had relatively poor PPVs (14.7% to 17.5%), but high NPVs. The percent of youth correctly classified was 65% for the MFQ-SF and 70% for the ASI.
Table 3.
Screening for anxiety: psychometric properties of the Mood and Feelings Questionnaire and the Anxiety and Sensitivity Index using the C-DISC anxiety disorder (with or without depression) as the gold standard in a combined sample of youth with and without asthma [Total N = 1375 with N = 145 (10.5%) with an anxiety diagnosis]
| Mood Feelings | ASI | |
|---|---|---|
| Area Under the Receiver Operating Curve* | .76 (95% CI,.72 –.81) | .76 (95% CI,.74–.79 |
| Cutpoint Determined by Receiver Operating Curve | ≥4 | ≥13 |
| Sensitivity | .73 (95% CI,.71 –.76) | .76 (95% CI,.74 –.79) |
| Specificity | .64 (95% CI,.61 –.67) | .70 (95% CI,.67 –.72) |
| Positive Predictive Value (%) (PPV) | 14.7 (95% CI, 12.8 – 16.7) | 17.5 (95% CI, 15.5 – 19.6) |
| Negative Predictive Value (%) (NPV) | 96.6 (95% CI, 95.6 – 97.6) | 97.2 (95% CI, 96.3 – 98.1) |
| Total % Correctly Classified | 64.8% | 70.1% |
| % Youth with Anxiety Correctly Classified | 64.0% | 76.2% |
| % Youth without Anxiety Correctly Classified | 64.0% | 69.6% |
x2 (1) = 0.59, p = 0.44; MFQ = ASI
Sensitivity Analyses
We computed the sensitivity and specificity of the ASI and MFQ-SF in the asthma and control cohorts separately for screening for ≥1 anxiety or depressive disorders. In the asthma cohort, the sensitivity and specificity of the ASI was .79 and .69, respectively, and the sensitivity and specificity of the MFQ-SF was .78 and .71, respectively. In the controls, the sensitivity and specificity of the ASI was .65 and .70, and the sensitivity and specificity of the MFQ-SF was .73 and .75, respectively.
We also computed the PPVs for detecting youth with ≥1 anxiety or depressive diagnosis using the prevalence of anxiety and/or depression in each cohort: 8.6% prevalence in controls and 17.1% prevalence in youth with asthma. Given the estimated 10% prevalence of asthma, we also estimated that if the controls included youth with asthma, the prevalence of one or more anxiety and depressive disorders would have been slightly higher, i.e. 9.5%. We then estimated the PPV of the two questionnaires based on the inclusion in the control group of a 10% sample of youth with asthma. Among controls, the PPV was 24% for the MFQ-SF and 19% for the ASI. Among youth with asthma, the PPV was 41% for the MFQ-SF and 34% for the ASI. Among controls enriched with a 10% sample of youth with asthma, the PPV was 23% for the MFQ-SF and 23% for the ASI. The values in Table 1 essentially represent the average of these cohort PPVs.
DISCUSSION
Our results suggest that both the MFQ-SF and the ASI have relatively high sensitivity and specificity and performed moderately well on the ROC analysis for screening youth for one or more DSM-IV anxiety or depressive disorders. These screening tools also have the advantage of being brief and easy to administer. The majority of primary care physicians report that it is their responsibility to identify anxiety and depression in youth25, but few are using standardized tools to screen for the disorders26. Our results may help primary care physicians choose optimal screening tools. When used as a screening measure for either anxiety or depression, the MFQ-SF has slightly superior psychometric properties in comparison to the longer ASI, but the results are so similar as to make the choice more theoretical than psychometric. That is, the primary care physician or researcher should use the scale that makes the most empirical sense given their population or the study questions. These are important findings for primary care physicians because approximately 10% to 20% of youth meet DSM-IV criteria for ≥1 anxiety or depressive disorders1, 2, 6, 17, anxiety and depressive disorders frequently co-occur, and longitudinal studies show that youth with anxiety disorders are particularly vulnerable to developing depressive episodes27.
Researchers or clinics that only want to screen for major depression should note that the MFQ-SF performed significantly better than the ASI on the ROC analysis (0.84 vs. 0.77) with better sensitivity (0.80 vs. 0.74) and specificity (0.81 vs. 0.66). In screening for anxiety disorders, both the ASI and MFQ-SF only performed in the “fair” range on ROC analysis (0.76) and had a relatively poor PPV (14.7% to 17.5%).
Although our data suggests that screening for depression and anxiety could lead to more accurate identification of DSM-IV psychiatric disorders, the relatively low PPVs for both instruments also suggest that screening will lead to some degree of burden of false positive results. However, community-based studies of children and adolescents suggest that 5% to 10% report subsyndromal symptoms of anxiety or depression, which are associated with considerable psychosocial impairment, high familial loading for depression, and an increased risk for suicide attempts and developing a full-blown depressive disorder.28 Therefore, “false positives” may still be a population of youth that needs further interview to determine reasons for less severe psychological distress.
Our sensitivity analysis suggests that there is higher PPV in screening youth with asthma compared to controls because of the higher prevalence of meeting criteria for ≥1 anxiety or depression disorders in youth with this chronic illness. For systems of care that are concerned about the burden of false positives, targeting screening to high risk subgroups such as youth with a chronic medical illness may be more efficient. The sensitivity and specificity of the MFQ-SF was similar in the asthma and control cohorts for screening for ≥1 anxiety or depressive disorders whereas the ASI had higher sensitivity (.79 vs. .65) but similar specificity (.69 vs. .70) in youth with asthma compared to controls.
The finding of the current study that the MFQ-SF cutoff of ≥6 had 80% sensitivity and 81% specificity to the C-DISC diagnosis of major depression was similar to results from previous, smaller studies. Previous studies used a cutoff of 8 on the MFQ-SF, but in our study a cutoff of 6 on the MFQ-SF was optimal based on the ROC analysis, whereas a cutoff of 8 resulted in 0.42 sensitivity and 0.92 specificity for the combined anxiety and depression group. Our population was generally larger and more representative than the four prior populations studied.29–32 Lower cutoff scores are often found in community and primary care populations compared to specialty mental health populations. Four studies have compared the MFQ-SF at cutoff of 8 to evidence of meeting criteria for major depression on structured interviews.29–32 Angold et al. (1995) examined the child report MFQ-SF compared to a C-DISC interview in a sample of 125 7- to 11-year-olds and found that a cutoff of ≥8 achieved 60% sensitivity and 85% specificity.29 Thapar and McGuffin (1998) examined the child-report MFQ-SF compared to a diagnosis of depression based on a structured psychiatric interview in 43 adolescents.30 The cutoff-point of 8 on the MFQ-SF yielded a sensitivity of 75% and a specificity of 74%. Kuo et al. (2005) administered the MFQ-SF to adolescents in a juvenile detention facility and showed 100% sensitivity and 67% specificity at the cutoff of 8 compared to the C-DISC diagnosis of major depression in a representative sample of 50 of the adolescents.31 Simpson et al. (2004) described in the Developmental Pathways Project a sensitivity of 55% and specificity of 87% at the MFQ-SF score of ≥8 among 11- to 12-year-olds using a C-DISC diagnosis of major depression.32
The relatively poor PPV of both the MFQ-SF or the ASI for screening for anxiety disorders compared to major depressive disorder is probably explained by the variability of symptoms in the five anxiety disorders assessed (i.e. social anxiety, separation anxiety, agoraphobia, panic and generalized anxiety disorder). We believe it is difficult for one screening measure to effectively screen for the diversity of symptoms in these five disorders whereas the MFQ-SF can more effectively include in a short screen most of the nine DSM-IV symptoms of major depression. Other epidemiologic studies of young adults have also found that anxiety questionnaires have relatively poor PPV compared to structured psychiatric interviews in diagnosing anxiety disorders.33
One limitation was that the study took place in one large HMO in the northwest region of the United States. Future studies will need to validate the optimal cutoffs on depression and anxiety scales in other samples. Our response rates of 61% and 51% in youth with asthma and controls, respectively, may have also influenced our results because nonresponders may have different rates of anxiety and depressive disorders. It is also possible that phone, rather than in-person, administration of anxiety and depression questionnaires may have provided different results from previous studies. Also, the current study oversampled youth with asthma. However, asthma is the most common chronic disorder in youth, is responsible for high utilization of primary care and is associated with 2-fold higher rates of anxiety and depressive disorders.17 In addition, our sensitivity analysis allowed estimation of PPV in both groups separately. Strengths of the study include the large sample size and the use of well validated youth anxiety and depressive self-report measures and structured psychiatric interviews.
CONCLUSION
Multiple studies have found low rates of recognition of anxiety and depressive disorders by pediatricians9, 10 Screening for anxiety and depressive disorders could improve detection, but improved patient-level outcomes will probably require changes in the way primary care is organized. One large study showed that when screening for depression was coupled with a primary care based quality improvement program aimed at enhanced exposure of youth to evidence based treatment, there was evidence of improved depression outcomes.34 Our data suggests optimal cutoffs for two brief questionnaires that could be utilized for effective screening of youth with one or more anxiety and depressive disorders. The MFQ-SF is briefer and has better psychometric properties than the ASI for screening youth for major depression. More research is needed in order to develop a short screening questionnaire for anxiety disorders in youth.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health to Dr. Katon (MH-067587 and MH-069741).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 3.Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosom Med. 2004;66:349–355. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- 4.Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: rates and risk factors. Diabetes Care. 1997;20:36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- 5.Garber J, Walker L, Zeman J. Somatization symtpoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychol Assessment. 1991;3:588–595. [Google Scholar]
- 6.Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004;61:85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- 7.Richardson LP, Davis R, Poulton R, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157:739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 8.Bush T, Richardson L, Katon W, et al. Anxiety and depressive disorders are associated with smoking in adolescents with asthma. J Adolesc Health. 2007;40:425–432. doi: 10.1016/j.jadohealth.2006.11.145. [DOI] [PubMed] [Google Scholar]
- 9.Horwitz SM, Leaf PJ, Leventhal JM, Forsyth B, Speechley KN. Identification and management of psychosocial and developmental problems in community-based, primary care pediatric practices. Pediatrics. 1992;89:480–485. [PubMed] [Google Scholar]
- 10.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44:1064–1072. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 11.Zuckerbrot RA, Jensen PS. Improving recognition of adolescent depression in primary care. Arch Pediatr Adolesc Med. 2006;160:694–704. doi: 10.1001/archpedi.160.7.694. [DOI] [PubMed] [Google Scholar]
- 12.Zuckerbrot RA, Maxon L, Pagar D, et al. Adolescent depression screening in primary care: feasibility and acceptability. Pediatrics. 2007;119:101–108. doi: 10.1542/peds.2005-2965. [DOI] [PubMed] [Google Scholar]
- 13.Mulrow CD, Williams JW, Jr, Gerety MB, et al. Case-finding instruments for depression in primary care settings. Ann Intern Med. 1995;122:913–921. doi: 10.7326/0003-4819-122-12-199506150-00004. [DOI] [PubMed] [Google Scholar]
- 14.Gilbody SM, House AO, Sheldon TA. Routinely administered questionnaires for depression and anxiety: systematic review. BMJ. 2001;322:406–409. doi: 10.1136/bmj.322.7283.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverman W, Flergig W, Rabian B, Peterson R. Childhood Anxiety Sensitivity Index. J Clin Child Psychology. 1995;20:162–168. [Google Scholar]
- 16.Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Katon W, Lozano P, Russo J, et al. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared to controls. J Adolesc Health. 2007;41:455–463. doi: 10.1016/j.jadohealth.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weems CF, Hammond-Laurence K, Silverman WK, Ferguson C. The relation between anxiety sensitivity and depression in children and adolescents referred for anxiety. Behav Res Ther. 1997;35:961–966. doi: 10.1016/s0005-7967(97)00049-1. [DOI] [PubMed] [Google Scholar]
- 19.Taylor S, Koch WJ, Woody S, McLean P. Anxiety sensitivity and depression: how are they related? J Abnorm Psychol. 1996;105:474–479. doi: 10.1037//0021-843x.105.3.474. [DOI] [PubMed] [Google Scholar]
- 20.Rector NA, Szacun-Shimizu K, Leybman M. Anxiety sensitivity within the anxiety disorders: Disorder-specific sensitivities and depression comorbidity. Behav Res Ther. 2007;45:1967–1975. doi: 10.1016/j.brat.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 21.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Wells KB, Burnam MA, Leake B, Robins LN. Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1988;22:207–220. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- 23.Wasserman GA, McReynolds LS, Lucas CP, Fisher P, Santos L. The voice DISC-IV with incarcerated male youths: prevalence of disorder. J Am Acad Child Adolesc Psychiatry. 2002;41:314–321. doi: 10.1097/00004583-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Ingelfinger J, Mosteller F, Thibodeau L, Ware J. Biostatistics in Clinical Medicine. 2. New York: McMillan Publishing Co.; 1987. [Google Scholar]
- 25.Olson AL, Kelleher KJ, Kemper KJ, et al. Primary care pediatricians’ roles and perceived responsibilities in the identification and management of depression in children and adolescents. Ambul Pediatr. 2001;1:91–98. doi: 10.1367/1539-4409(2001)001<0091:pcprap>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 26.Gardner W, Kelleher KJ, Pajer KA, Campo JV. Primary care clinicians’ use of standardized tools to assess child psychosocial problems. Ambul Pediatr. 2003;3:191–195. doi: 10.1367/1539-4409(2003)003<0191:pccuos>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 27.Merikangas KR, Zhang H, Avenevoli S, et al. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 28.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 29.Angold A, Costello E, Messer S, et al. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Intern J Method Psychiatr Res. 1995;5:237–249. [Google Scholar]
- 30.Thapar A, McGuffin P. Validity of the shortened Mood and Feelings Questionnaire in a community sample of children and adolescents: a preliminary research note. Psychiatry Res. 1998;81:259–268. doi: 10.1016/s0165-1781(98)00073-0. [DOI] [PubMed] [Google Scholar]
- 31.Kuo ES, Stoep AV, Stewart DG. Using the short mood and feelings questionnaire to detect depression in detained adolescents. Assessment. 2005;12:374–383. doi: 10.1177/1073191105279984. [DOI] [PubMed] [Google Scholar]
- 32.Simpson A, Vander Stoep A, Tsuang D, Weiss N, McCauley E. Department of Epidemiology. Seattle, WA: University of Washington; 2004. Evaluating the validity of the Short Mood and Feelings Questionnaire and one- and two-question screens in a community sample of youths. [Google Scholar]
- 33.Hoyer J, Becker ES, Neumer S, Soeder U, Margraf J. Screening for anxiety in an epidemiological sample: predictive accuracy of questionnaires. J Anxiety Disord. 2002;16:113–134. doi: 10.1016/s0887-6185(01)00094-9. [DOI] [PubMed] [Google Scholar]
- 34.Asarnow JR, Jaycox LH, Duan N, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA. 2005;293:311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]