Abstract
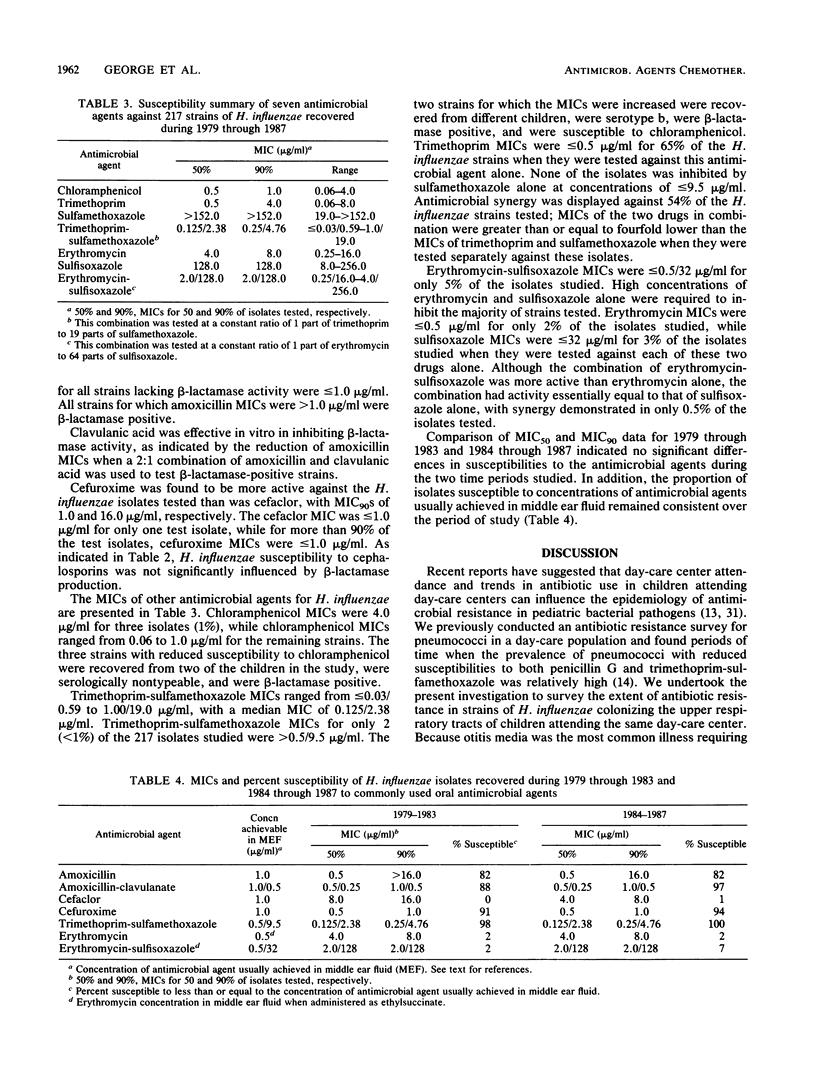
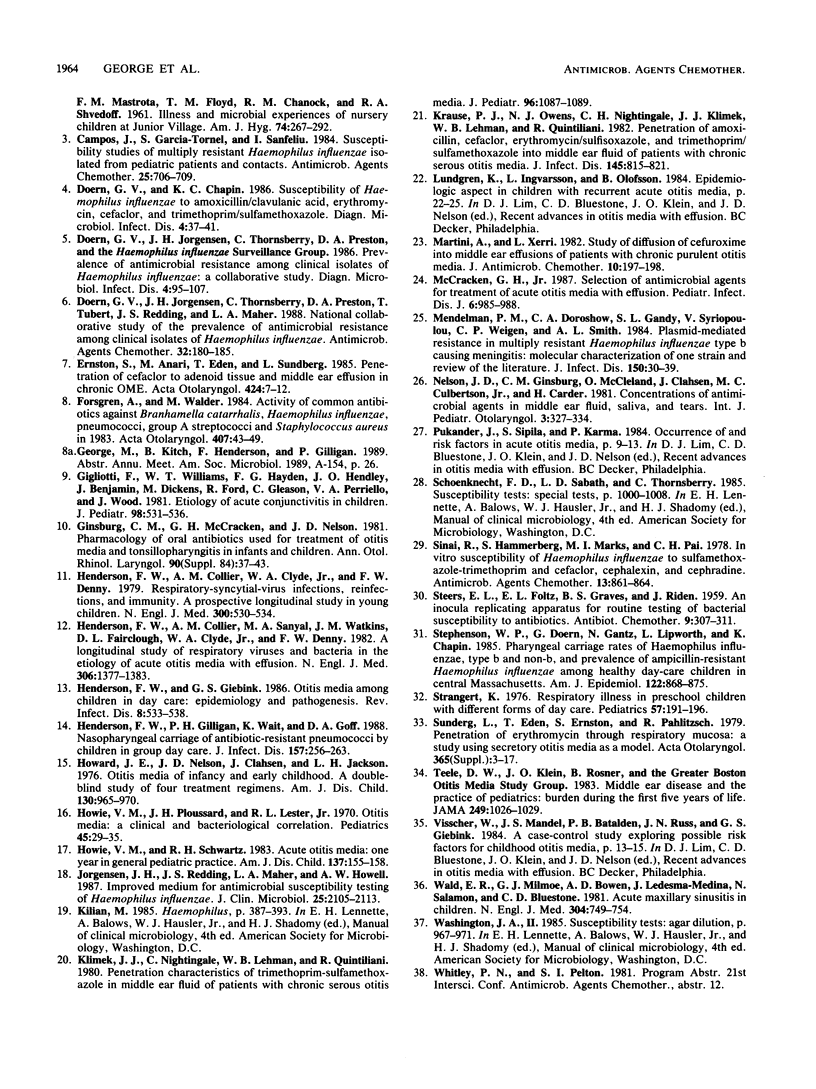
To determine whether the prevalence of resistance to commonly used oral antimicrobial agents varied over time, we compared the in vitro susceptibilities of 217 strains of Haemophilus influenzae recovered from nasopharyngeal secretions of children in a day-care center studied longitudinally between 1979 and 1987. The overall rate of beta-lactamase production in these strains was 18%, with rates of 57% in type b isolates (n = 21) and 14% in non-type b isolates (n = 196). The percentages of isolates for which MICs were less than or equal to 1.0 micrograms/ml for amoxicillin alone, amoxicillin in combination with clavulanic acid, and cefuroxime alone were 82, 92, and 93%, respectively. The percentage of strains for which cefaclor MICs were less than or equal to 1.0 micrograms/ml was only 0.5%. Isolates for which chloramphenicol MICs were greater than 2.0 micrograms/ml or for which trimethoprim-sulfamethoxazole MICs were greater than 0.5/9.5 micrograms/ml were uncommon: 1 and less than 1%, respectively. High concentrations of erythromycin alone and in combination with sulfisoxazole were required to inhibit the majority of test strains; there was no evidence of erythromycin-sulfisoxazole synergy. In vitro susceptibility to commonly used oral antimicrobial agents remained at a constant level when H. influenzae isolates collected from children in a day-care center during 1979 through 1983 were compared with strains collected during 1984 through 1987.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bass J. W., Steele R. W., Wiebe R. A., Dierdorff E. P. Erythromycin concentrations in middle ear exudates. Pediatrics. 1971 Sep;48(3):417–422. [PubMed] [Google Scholar]
- Campos J., Garcia-Tornel S., Sanfeliu I. Susceptibility studies of multiply resistant Haemophilus influenzae isolated from pediatric patients and contacts. Antimicrob Agents Chemother. 1984 Jun;25(6):706–709. doi: 10.1128/aac.25.6.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doern G. V., Chapin K. C. Susceptibility of Haemophilus influenzae to amoxicillin/clavulanic acid, erythromycin, cefaclor, and trimethoprim/sulfamethoxazole. Diagn Microbiol Infect Dis. 1986 Jan;4(1):37–41. doi: 10.1016/0732-8893(86)90054-4. [DOI] [PubMed] [Google Scholar]
- Doern G. V., Jorgensen J. H., Thornsberry C., Preston D. A. Prevalence of antimicrobial resistance among clinical isolates of Haemophilus influenzae: a collaborative study. Diagn Microbiol Infect Dis. 1986 Feb;4(2):95–107. doi: 10.1016/0732-8893(86)90143-4. [DOI] [PubMed] [Google Scholar]
- Doern G. V., Jorgensen J. H., Thornsberry C., Preston D. A., Tubert T., Redding J. S., Maher L. A. National collaborative study of the prevalence of antimicrobial resistance among clinical isolates of Haemophilus influenzae. Antimicrob Agents Chemother. 1988 Feb;32(2):180–185. doi: 10.1128/aac.32.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernstson S., Anari M., Edén T., Sundberg L. Penetration of cefaclor to adenoid tissue and middle ear effusion in chronic OME. Acta Otolaryngol Suppl. 1985;424:7–12. doi: 10.3109/00016488509121604. [DOI] [PubMed] [Google Scholar]
- Forsgren A., Walder M. Activity of common antibiotics against Branhamella catarrhalis, Haemophilus influenzae, pneumococci, group A streptococci and Staphylococcus aureus in 1983. Acta Otolaryngol Suppl. 1984;407:43–49. doi: 10.3109/00016488409124964. [DOI] [PubMed] [Google Scholar]
- Gigliotti F., Williams W. T., Hayden F. G., Hendley J. O., Benjamin J., Dickens M., Gleason C., Perriello V. A., Wood J. Etiology of acute conjunctivitis in children. J Pediatr. 1981 Apr;98(4):531–536. doi: 10.1016/s0022-3476(81)80754-8. [DOI] [PubMed] [Google Scholar]
- Ginsburg C. M., McCracken G. H., Jr, Nelson J. D. Pharmacology of oral antibiotics used for treatment of otitis media and tonsillopharyngitis in infants and children. Ann Otol Rhinol Laryngol Suppl. 1981 May-Jun;90(3 Pt 3):37–43. doi: 10.1177/00034894810903s210. [DOI] [PubMed] [Google Scholar]
- Henderson F. W., Collier A. M., Clyde W. A., Jr, Denny F. W. Respiratory-syncytial-virus infections, reinfections and immunity. A prospective, longitudinal study in young children. N Engl J Med. 1979 Mar 8;300(10):530–534. doi: 10.1056/NEJM197903083001004. [DOI] [PubMed] [Google Scholar]
- Henderson F. W., Collier A. M., Sanyal M. A., Watkins J. M., Fairclough D. L., Clyde W. A., Jr, Denny F. W. A longitudinal study of respiratory viruses and bacteria in the etiology of acute otitis media with effusion. N Engl J Med. 1982 Jun 10;306(23):1377–1383. doi: 10.1056/NEJM198206103062301. [DOI] [PubMed] [Google Scholar]
- Henderson F. W., Giebink G. S. Otitis media among children in day care: epidemiology and pathogenesis. Rev Infect Dis. 1986 Jul-Aug;8(4):533–538. doi: 10.1093/clinids/8.4.533. [DOI] [PubMed] [Google Scholar]
- Henderson F. W., Gilligan P. H., Wait K., Goff D. A. Nasopharyngeal carriage of antibiotic-resistant pneumococci by children in group day care. J Infect Dis. 1988 Feb;157(2):256–263. doi: 10.1093/infdis/157.2.256. [DOI] [PubMed] [Google Scholar]
- Howard J. E., Nelson J. D., Clahsen J., Jackson L. H. Otitis media of infancy and early childhood. A double-blind study of four treatment regimens. Am J Dis Child. 1976 Sep;130(9):965–970. doi: 10.1001/archpedi.1976.02120100055008. [DOI] [PubMed] [Google Scholar]
- Howie V. M., Ploussard J. H., Lester R. L., Jr Otitis media: a clinical and bacteriological correlation. Pediatrics. 1970 Jan;45(1):29–35. [PubMed] [Google Scholar]
- Howie V. M., Schwartz R. H. Acute otitis media. One year in general pediatric practice. Am J Dis Child. 1983 Feb;137(2):155–158. [PubMed] [Google Scholar]
- Jorgensen J. H., Redding J. S., Maher L. A., Howell A. W. Improved medium for antimicrobial susceptibility testing of Haemophilus influenzae. J Clin Microbiol. 1987 Nov;25(11):2105–2113. doi: 10.1128/jcm.25.11.2105-2113.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimek J. J., Bates T. R., Nightingale C., Lehmann W. B., Ziemniak J. A., Quintiliani R. Penetration characteristics of trimethoprim-sulfamethoxazole in middle ear fluid of patients with chronic serous otitis media. J Pediatr. 1980 Jun;96(6):1087–1089. doi: 10.1016/s0022-3476(80)80650-0. [DOI] [PubMed] [Google Scholar]
- Krause P. J., Owens N. J., Nightingale C. H., Klimek J. J., Lehmann W. B., Quintiliani R. Penetration of amoxicillin, cefaclor, erythromycin-sulfisoxazole, and trimethoprim-sulfamethoxazole into the middle ear fluid of patients with chronic serous otitis media. J Infect Dis. 1982 Jun;145(6):815–821. doi: 10.1093/infdis/145.6.815. [DOI] [PubMed] [Google Scholar]
- Martini A., Xerri L. Study of diffusion of cefuroxime into middle ear effusions of patients with chronic purulent otitis media. J Antimicrob Chemother. 1982 Sep;10(3):197–198. doi: 10.1093/jac/10.3.197. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr Selection of antimicrobial agents for treatment of acute otitis media with effusion. Pediatr Infect Dis J. 1987 Oct;6(10):985–988. doi: 10.1097/00006454-198710000-00039. [DOI] [PubMed] [Google Scholar]
- Mendelman P. M., Doroshow C. A., Gandy S. L., Syriopoulou V., Weigen C. P., Smith A. L. Plasmid-mediated resistance in multiply resistant Haemophilus influenzae type b causing meningitis: molecular characterization of one strain and review of the literature. J Infect Dis. 1984 Jul;150(1):30–39. doi: 10.1093/infdis/150.1.30. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Ginsburg C. M., Mcleland O., Clahsen J., Culbertson M. C., Jr, Carder H. Concentrations of antimicrobial agents in middle ear fluid, saliva and tears. Int J Pediatr Otorhinolaryngol. 1981 Dec;3(4):327–334. doi: 10.1016/0165-5876(81)90057-4. [DOI] [PubMed] [Google Scholar]
- Sinai R., Hammerberg S., Marks M. I., Pai C. H. In vitro susceptibility of Haemophilus influenzae to sulfamethoxazole-trimethoprim and cefaclor, cephalexin, and cephradine. Antimicrob Agents Chemother. 1978 May;13(5):861–864. doi: 10.1128/aac.13.5.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson W. P., Doern G., Gantz N., Lipworth L., Chapin K. Pharyngeal carriage rates of Haemophilus influenzae, type b and non-b, and prevalence of ampicillin-resistant Haemophilus influenzae among healthy day-care children in central Massachusetts. Am J Epidemiol. 1985 Nov;122(5):868–875. doi: 10.1093/oxfordjournals.aje.a114169. [DOI] [PubMed] [Google Scholar]
- Strangert K. Respiratory illness in preschool children with different forms of day care. Pediatrics. 1976 Feb;57(2):191–196. [PubMed] [Google Scholar]
- Sundberg L., Edén T., Ernstson S., Pahlitzsch R. Penetration of erythromycin through respiratory mucosa. A study using secretory otitis media as a model. Acta Otolaryngol Suppl. 1979;365:1–17. doi: 10.3109/00016487909124940. [DOI] [PubMed] [Google Scholar]
- Teele D. W., Klein J. O., Rosner B., Bratton L., Fisch G. R., Mathieu O. R., Porter P. J., Starobin S. G., Tarlin L. D., Younes R. P. Middle ear disease and the practice of pediatrics. Burden during the first five years of life. JAMA. 1983 Feb 25;249(8):1026–1029. [PubMed] [Google Scholar]
- Wald E. R., Milmoe G. J., Bowen A., Ledesma-Medina J., Salamon N., Bluestone C. D. Acute maxillary sinusitis in children. N Engl J Med. 1981 Mar 26;304(13):749–754. doi: 10.1056/NEJM198103263041302. [DOI] [PubMed] [Google Scholar]


