Abstract
The transition from a fluid filled lung to one filled with air in a very short period of time is one of the biggest challenges a newborn faces after birth. Respiratory morbidity as a result of failure to clear fetal lung fluid is not uncommon, and can be particularly problematic in some infants delivered by elective cesarean section (ECS) without being exposed to labor. The increasing rates of cesarean deliveries in the United States and worldwide, have the potential for a significant impact on public health and health care costs due to the morbidity associated with this subgroup. Whereas the occurrence of birth asphyxia, trauma, and meconium aspiration is reduced by elective cesarean delivery, the risk of respiratory distress secondary to transient tachypnea of the newborn, surfactant deficiency, and pulmonary hypertension is increased. It is clear that physiologic events in the last few weeks of pregnancy coupled with the onset of spontaneous labor are accompanied by changes in the hormonal milieu of the fetus and its mother, resulting in preparation of the fetus for neonatal transition. Rapid clearance of fetal lung fluid is a key part of these changes, and is mediated in large part by transepithelial sodium reabsorption through amiloride-sensitive sodium channels in the alveolar epithelial cells, with only a limited contribution from mechanical factors and Starling forces. In this chapter we discuss the respiratory morbidity associated with ECS, the physiologic mechanisms underlying fetal lung fluid absorption and potential strategies for facilitating neonatal transition when infants are delivered by ECS before the onset of spontaneous labor.
The changing landscape for human deliveries
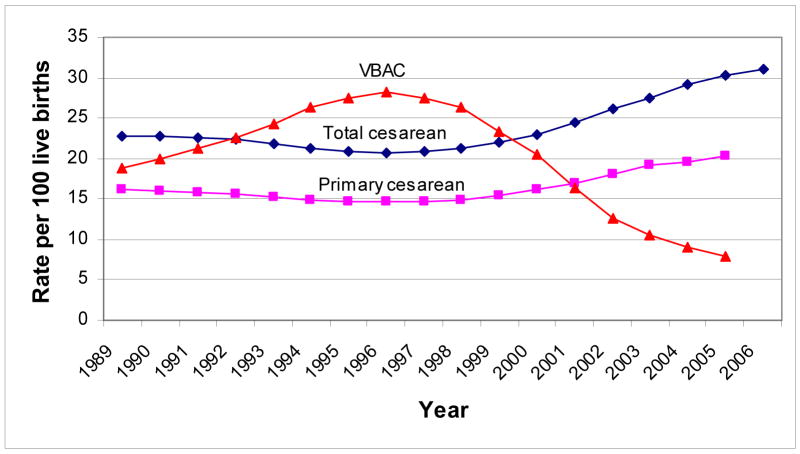
Cesarean births rose for an tenth straight year in 2006 to a record 31.1% of all deliveries in the United States; this rate is more than 50% higher than in 1996 and is accompanied by a significant drop in the number of women attempting vaginal birth after a previous cesarean delivery (VBAC).56(Fig. 1) Most of the overall increase can be attributed to the increase in the primary cesarean rates, from 14.6% in 1996 to 20.3% in 2005. This rise in the primary cesarean rate coupled with the decrease in the VBAC rate (7.9% in 2005) means that women who have a primary cesarean section have a greater than 90% chance of having a repeat cesarean section, further increasing the overall cesarean rate in the future.90 Among the many reasons cited for this increase are older women giving birth, multiple gestations from fertility treatments, as well as the concerns of physicians and mothers about the risks of vaginal birth. Cesarean births in low risk or “no risk” mothers where no medical indication can be identified are on the rise and are often referred to as Cesarean Delivery at Maternal Request (CDMR). Cesarean birth rates are considerably higher in some other parts of the world, especially in Latin America.8,14,15,84,128 Although indications for the high rate of operative deliveries can vary by regions and by maternal choice, up to 35% of these procedures may be performed because the woman has had a previous cesarean delivery.5,56,95
Fig 1.
The Total cesarean, Primary cesarean and vaginal birth after cesarean rates in the United States from 1989 to 2006. Source: U.S. National Center for Health Statistics (Note: for comparability, 2004 and 2005 primary cesarean and VBAC rates are limited to 37 jurisdictions with unrevised birth certificates, encompassing 69% of 2005 births; 2006 total cesarean rate is preliminary).
There have been efforts to reduce this high rate of repeat cesarean sections through attempts at trial of labor (vaginal birth after cesarean delivery, VBAC). In 1980, a consensus development conference on cesarean sections convened by the National Institutes of Health (NIH)concluded that vaginal delivery after previous low transverse cesarean delivery was a safe and acceptable option.1 A consensus conference in Canada in 1985 also arrived at a similar conclusion.3 The American College of Obstetrics and Gynecology has recommended a trial of labor, and there was a trend, albeit short-lived, toward increased VBACs, increasing from 24% in 1980 to 31% in 1991.5 However, VBAC rates have fallen by 72% since 199690,96 (National Vital Statistics Report, 2005), driven by the fear that trial of labor is associated with more perinatal morbidity and mortality than was previously believed. A large study by McMahon and coworkers95 showed that major maternal complications (such as uterine rupture) were twice as likely among women who underwent a trial of labor as compared with those who had a second elective cesarean section (ECS). These authors suggest that trial of labor is more likely to be successful in a special subset of women, but offer no definitive method for predicting which mothers fall into this group.
Similarly, Smith and coworkers120 reported a population based study from Scotland including 313,238 singleton births between 37 and 43 weeks. They concluded that, whereas the absolute risk of perinatal death associated with trial of labor following previous cesarean delivery was low, the risk was substantially higher (OR 11.6; 95% CI 1.6–86.7) than that associated with planned repeat cesarean delivery, and there was a “marked excess of deaths due to uterine rupture compared with other women in labor.” Further, 85% of delivery related perinatal deaths at term among women having a trial of labor occurred at or after 39 weeks gestation, as did a majority of the ante partum stillbirths (at or after 39 weeks gestation). A more recent study by Landon and coworkers78 similarly showed that a trial of labor after prior cesarean delivery is associated with a greater perinatal risk than is elective repeat cesarean delivery without labor, although the absolute risks by any delivery method was low. A further analysis of the same data done by Spong and coworkers123 confirmed those findings and found increased risks for uterine rupture among women with an indication for cesarean section with or without labor (0.28%, 0.08%), presence of labor (0.15%) and trial of labor (0.74%), with ECS without labor having the lowest risk (0%). The risk for hypoxic ischemic encephalopathy was higher in the trial of labor group and for those with an indication for cesarean section. Recently Villar and colleagues looked at 97,095 deliveries in a prospective cohort study within the 2005 WHO global survey on maternal and perinatal health and found that among deliveries with cephalic presentation, there was a trend towards a reduced odds ratio for fetal death with elective cesarean section (OR 0.65; 95% CI 0.43 to 0.98) and a larger protective effect with breech presentation.127 These issues will be covered in greater detail in a fortcoming issue of the Clinics.
Maternal Choice: “Too Posh to Push”
Although difficult to quantify, it has been estimated that nearly 4% to 18% of all cesarean deliveries worldwide are done upon maternal request.132 In the United States cesarean delivery on maternal request is estimated to be between 2.6% and 5.5%.37 A recent NIH state of the science consensus seminar “Cesarean Delivery on Maternal Request” reiterates the fact that maternal request is increasingly playing an important role in the obstetricians decisions to perform cesarean sections.4
The tabloids and news media have helped to publicize the fact that celebrities like Madonna, Britney Spears, Gwyneth Paltrow and Kate Hudson have chosen “elective cesarean” section as their preferred birthing option and have accused them of being “Too Posh to Push”.30,94 Many obstetricians believe that celebrity pop culture has influenced some women to opt for cesareans without any medical indications, but there are others who believe that there is no credible evidence or study that proves this fact. McCourt and colleagues in their critical review of literature did not find any evidence for an increasing trend in maternal request.94 Organizations such as Childbirth Connection through their surveys have found that only 1 in 1600 women surveyed planned an elective cesarean section, and maternal requests or changing demographics of childbearing women are not the cause of rising cesarean rates.36,38 Rather it is the changing practice standards of medical professionals and their willingness to perform cesarean section either due to their perceived safety or fear of malpractice litigation is the cause. In fact nearly one fourth of the mothers surveyed who underwent cesarean section reported pressure from medical personnel to have a cesarean.6
Most patients and healthcare providers who prefer cesarean section over vaginal delivery cite the fear of perineal injury, including anal and urinary incontinence, sexual dysfunction, fetal injury, control and convenience.63 There is not enough evidence or only weak evidence for increased maternal mortality with ECS, since maternal mortality is such a rare occurrence nowadays but there are certainly increased risks for serious maternal morbidity. A British survey of clinicians found that almost half the obstetricians thought that women should be offered their choice of delivery method and 33% of obstetricians in this survey considered a ECS for themselves or their spouses.79 Their preference for cesarean delivery is due to perceived benefits such as decreased risk of postpartum hemorrhage, less short term stress urinary incontinence, lower fetal mortality, hypoxic ischemic encephalopathy, and brachial plexus injury. Table 1 Shows the summary of risks and benefits of Cesarean delivery, from the NIH state of the science consensus conference on Cesarean Delivery on Maternal Request (CDMR).
Table 1.
Summary of the evidence based review from the NIH State of the Science Conference on CDMR.
| Maternal | Neonatal | |
|---|---|---|
| Moderate Quality Evidence | ||
| Favors planned Vaginal | Reduced length of hospital stay | Less respiratory morbidity |
| Favors planned C-section | Less risk of postpartum hemorrhage | |
|
| ||
| Weak Quality Evidence | ||
| Favors planned Vaginal | Lower infection rates
Fewer anesthetic complications, less subsequent placenta previa Higher breastfeeding rate |
Less iatrogenic prematurity
Shorter hospital stays Lower fetal mortality |
| Favors planned C-section | Less short-term stress urinary incontinence and fewer surgical complications compared to unplanned cesarean deliveries | Less IVH, neonatal asphyxia, encephalopathy, brachial plexus injury, and neonatal infection |
| Sensitive to parity, family size | Subsequent uterine rupture
Hysterectomy Number of pregnancies |
|
|
| ||
| Weak Evidence: Neither delivery route affords any advantages on these issues | Mortality
Anorectal function Sexual function Pelvic organ prolapse Subsequent stillbirth |
Mortality
Long-term outcomes |
From Hibbard J, Torre MD: Grand Rounds: When mom requests a cesarean. Contemporary OB/GYN:38, 2006, with permission
Until a reliable method is available that can predict the likelihood of success of trial of labor with minimum morbidity and mortality, and/or dramatic changes occur in the cultural, medicolegal, and economic forces, the rate of ECS is likely to stay high and maternal choice is likely to play an increasing role.
Respiratory Morbidity in Infants Delivered by Cesarean Delivery
Several studies have documented the high incidence of respiratory distress and NICU admissions in infants born by cesarean delivery before the onset of spontaneous labor.7,10,32,40,42,47,50,53,58,59,62,75,77,85,86,89,94,96,97,109,116,117,125,127,135,137 In contrast, however, the incidence of birth asphyxia, trauma, and meconium aspiration is lower, and these advantages of elective cesarean delivery have been reviewed elsewhere in this issue of Clinics.
Accurate data about the occurrence of respiratory failure and long-term outcomes in term and near-term infants are hard to obtain because of the lack of large databases such as those available for preterm infants; however, it is estimated that a significant number of term infants delivered by ECS are admitted to neonatal intensive care units each year in the US9 with the diagnosis of transient tachypnea of the newborn,10,40,46,54,59,64,77,81,97,114,115,136 respiratory distress syndrome,40,59,64,77,81,114,136 and severe persistent pulmonary hypertension of the newborn (PPHN)/hypoxic respiratory failure.59,62,75,117 Some of these reports also show higher rates of mechanical ventilation, oxygen therapy, extra corporeal membrane oxygenation (ECMO), and death. Madar and coworkers87 and Roth-Kleiner and coworkers117 showed that, in infants who develop respiratory distress after ECS, the need for mechanical ventilation was dramatically higher.
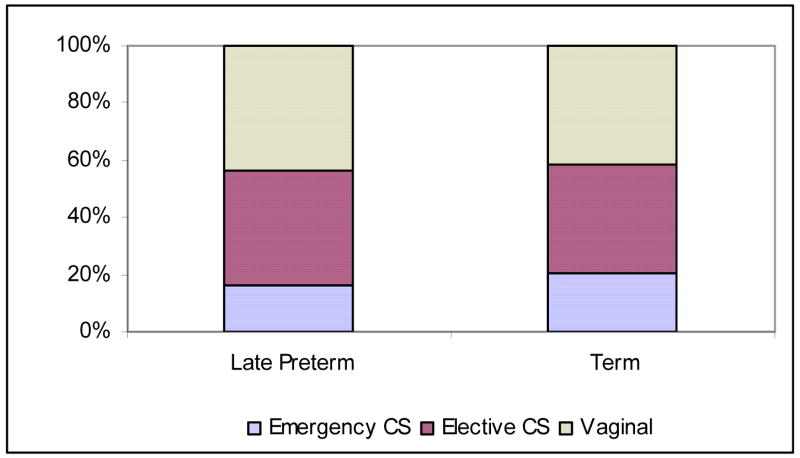
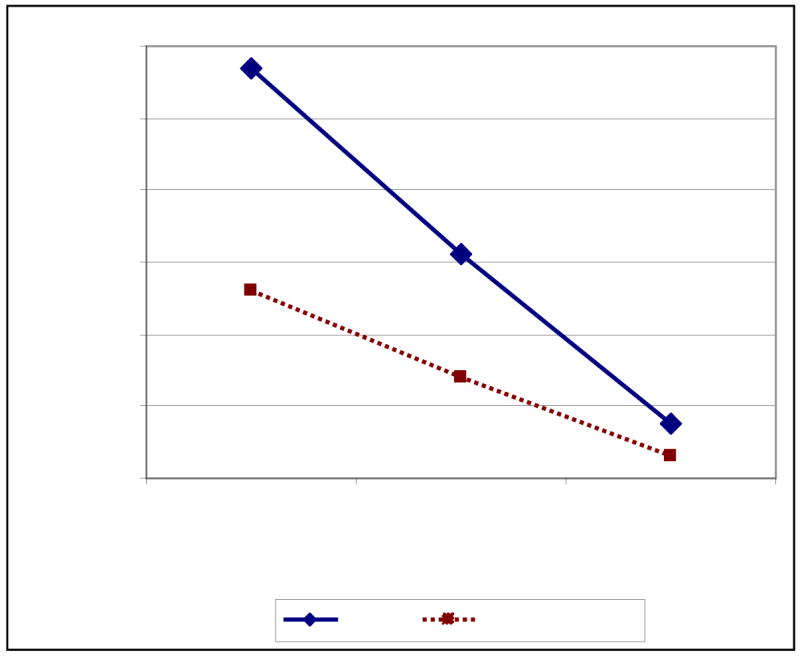
Why do elective cesarean deliveries carry a higher risk for the neonate? Since ECS is commonly performed between 37 and 40 weeks gestation,54 it was believed that at least some of the respiratory morbidity in newborns delivered by ECS was secondary to iatrogenic prematurity.35 Indeed, studies evaluating large series of patients have shown a higher rate of prematurity49,53,88 and surfactant deficiency87,117 in these patients. Several studies have shown that respiratory morbidity in ECS is inversely related to gestational age at the time of ECS.40,59,97 Hansen and coworkers in a prospective cohort study looking at infants delivered between 37–41 weeks gestation found that the odds of respiratory morbidity and serious respiratory morbidity were higher among 37,38 and 39 weeks gestation infants delivered by ECS when compared to those delivered vaginally. (Fig. 2)
Fig 2. Neonatal respiratory morbidity after elective caesarean section and intended vaginal delivery for 34 458 pregnancies at Aarhus University Hospital, Denmark, 1998–2006. Infants with meconium aspiration syndrome, sepsis, or pneumonia excluded.
Adjusted for smoking, alcohol intake, parity, body mass index, marital status, maternal age, and years of schooling.
Adapted from Hansen AK, Wisborg K, Uldbjerg N, et al: Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. Bmj 336:85, 2008, with permission
To minimize the occurrence of iatrogenic respiratory distress syndrome (RDS), fetal lung maturity testing was initially recommended before elective cesarean delivery, but this is seldom done, given the perception of risks associated with amniocentesis. Also amniotic fluid testing for fetal lung maturity does not reliably exclude the risk for respiratory distress, as surfactant deficiency is not its sole cause. Changes in the pulmonary vasculature, such as slowing of smooth muscle cell replication and involution at birth, increase in the small pulmonary blood vessels (up to 40 times) in the 3rd trimester, and changes in the epithelial sodium channels with increased ability to clear fetal lung fluid at term and with labor, all play an important role. Delaying ECS to 38 to 40 weeks has been shown to decrease the risk of respiratory distress, but this carries the risk of the patient going into spontaneous labor and the risk of still births.57 Further, it is clear that, in addition to prematurity and RDS, infants delivered by ECS are at higher risk for developing transient tachypnea of the newborn (Type II RDS, Wet lung syndrome) and persistent pulmonary hypertension unrelated to their gestational age at the time of delivery. Although respiratory distress is generally considered to be transient with full recovery without any long-term consequences, a significant number of infants progress to severe respiratory failure.75 These infants not only require prolonged hospitalization, but also are at increased risk for chronic lung disease and death.75 In addition, there is a higher incidence of respiratory depression at birth (low Apgar scores),64 thought to be related to fluid-logged lungs making the transition to air breathing more difficult.
In an effort to reduce the occurrence of iatrogenic prematurity associated with ECS deliveries, ACOG (Guidelines for Perinatal Care, 5th edition, p 148) recommends scheduling ECS at 39 weeks or later on the basis of menstrual dates, or waiting for the onset of spontaneous labor. It also lays down the criteria for establishing fetal maturity before ECS. However, as alluded to earlier, the safety of this approach in mothers with previous cesarean section deliveries has not been established in rigorous trials. Some population-based studies120,123 point to an increased risk of uterine rupture and perinatal death in mothers with previous cesarean section who went into spontaneous labor after 39 weeks. It should also be noted that a vast majority of operative and spontaneous deliveries in the US occur at community hospitals; 2461 community hospitals have delivery service as compared with 260 academic centers (American Medical Association, 2005). There is little data about the accuracy of dating of pregnancies at rural hospitals with small delivery services and in pregnancies where prenatal care is initiated late. It is also not clear how rigorously ACOG guidelines for elective cesarean delivery at 39 weeks or later are followed. Such findings, as well as factors related to the convenience of scheduled ECS deliveries for both families as well as the providers, will continue to influence the timing of ECS.
We72 have recently obtained data from the Cesarean Section Registry maintained by the Maternal Fetal Medicine Units Network (MFMU). These data support previously published data on higher occurrence of respiratory distress in infants delivered by elective repeat cesarean section (ERCS) versus those delivered by VBAC. The MFMU Registry tracks infants ≥37 weeks gestation who had an ERCS without any trial of labor, as compared with infants delivered successfully by VBAC. Among infants delivered by ERCS, 6.2% developed respiratory distress and 11.1% required NICU admission, compared with 3.3% respiratory distress and 7.5% NICU admissions in the VBAC group. The Registry does not maintain data on the occurrence of PPHN, ECMO usage, and death, making it difficult to estimate the exact occurrence of hypoxic respiratory failure.
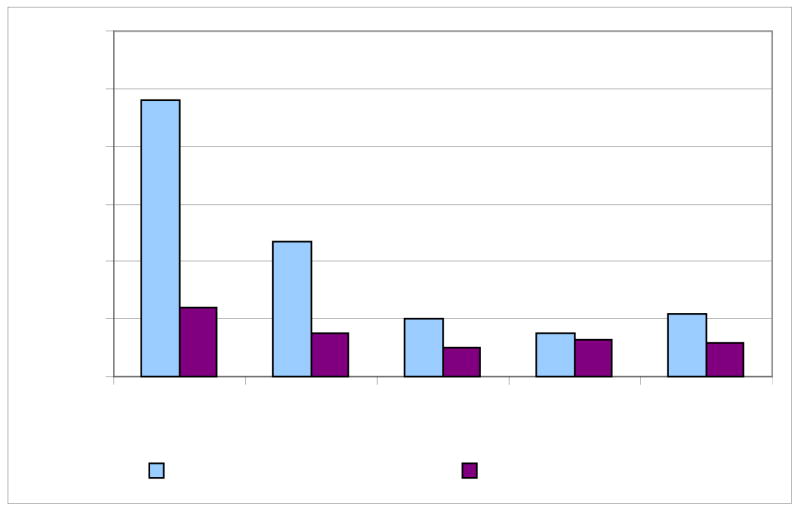
The general impression among clinicians about transient tachypnea of the newborn (TTN) and “wet lung syndrome” is that of a benign self-limited illness that requires minimal intervention. Although respiratory distress due to TTN and other causes is frequently seen in infants delivered by ECS, it is not clearly known how important this is clinically and how many of these infants become seriously ill and require significant intervention. One approach would be to evaluate the true occurrence of severe hypoxic respiratory failure in this population.55 Heritage and Cunningham62 and Keszler and coworkers75 reported severe respiratory morbidity and resulting mortality in infants born by ECS who developed pulmonary hypertension, hence the term “malignant TTN.” A significant number of these infants required ECMO.75 Previous estimates of ECS-delivered infants in the ECMO population include 16.5%,75 15%,62 and 17%.80 We recently reviewed data from the ELSO registry to see if this trend had continued since the appearance of reports of ECMO usage in infants delivered by ERCS. From 1986 to 2006, a total of 14,603 infants ≥34 weeks gestation who were treated with ECMO for respiratory failure (excluding diaphragmatic hernia) were analyzed. Infants ≥34 weeks and <37 weeks were labeled as “Late Preterm” and those ≥37 weeks were classified as “Term”. A total of 39.5% of late preterm infants and 37.7% of term infants with hypoxic respiratory failure on ECMO were delivered by ECS. (Fig. 3)
Figure 3.
The mode of delivery of 14,603 infants ≥34 weeks who required ECMO in the US for respiratory failure between 1986 and 2006. Infants with congenital anomalies like congenital diaphragmatic hernia were excluded. A total of 2,145 infants were late preterm (defined as ≥34 and <37 weeks GA) and 12,458 term (≥37 weeks GA). Infants born by ECS constituted a large fraction of ECMO infants in both subgroups. In contrast, the ECS rates for the study period for the rest of the population were ~10%.
The etiology of persistent pulmonary hypertension in newborns delivered by ECS is unclear. Most infants start off as being normal or have mild TTN with minimal oxygen requirement and chest x-rays suggestive of retained lung fluid. However, in a subset of infants, there is a gradual increase in oxygen requirement and subsequent evidence of PPHN. Prematurity is not a significant issue, and these infants do not respond well to surfactant administration.75 There is considerable evidence, especially in the anesthesia literature, that breathing 100% oxygen predisposes patients to atelectasis.16,118,119 Looking at adult patients Rothen and coworkers showed that atelectasis occurs within 5 minutes of breathing 100% oxygen.119 Benoit and coworkers16 in a similar study confirmed these findings. It is common practice to treat mild respiratory distress in term neonates with oxygen hoods or nasal cannula; however, these infants are prone to developing progressive absorption atelectasis, especially when the fraction of inspired oxygen is high. Pulmonary hypertension develops secondarily, and it is not unusual for such infants be in 100% oxygen tents for variable periods of time before they get intubated. A recent Australian study looking at early CPAP Vs oxygen hoods found that infants on oxygen hoods requiring high oxygen concentrations were more likely to fail treatment and require a higher level of intensive care than those on CPAP with lower oxygen concentrations.27
Role of Retained Fetal Lung Fluid in Neonatal Respiratory Morbidity
The fetus has an interesting challenge presented to it at birth.72 Often at short notice, sometimes with no notice at all, it is asked to rapidly clear its air spaces of the fluid that it has been secreting through much of the pregnancy. The ability of a neonate to self-resuscitate itself at birth after remaining “submerged” in fluid for much of its life is truly remarkable, considering victims of near-drowning faced with similar amounts of fluid in the lungs do so poorly.67,72,106 The lung epithelium is a key player in this process, engineering the switch from placental to pulmonary gas exchange.21–25,66,103,104,107 For effective gas exchange to occur, alveolar spaces must be cleared of excess fluid and pulmonary blood flow increased to match ventilation with perfusion. Failure of either of these events can jeopardize neonatal transition and cause the infant to develop respiratory distress. We are still far from a complete understanding of the mechanisms(s) by which fetal lungs are able to clear themselves of excessive fluid at birth.71 It is clear though that traditional explanations which relied on “Starling forces” and “vaginal squeeze” can only account for a fraction of the fluid absorbed.11,17–20,67 Amiloride-sensitive sodium transport by lung epithelia through epithelial sodium channels (ENaC) has emerged as a key event in the transepithelial movement of alveolar fluid.22,23,70,100–105,107 Disruption of this process has been implicated in several disease states, including transient tachypnea of the newborn51 and hyaline membrane disease.13 In later life, pulmonary edema can result either from excessive movement of water and solute across the alveolar capillary membrane, or from failure of reabsorption of lung fluid.91,93 (Fig. 4) Depicts a schematic model for assembly and regulation of amiloride-sensitive sodium channels in the lung.
Figure 4. A schematic model for assembly and regulation of amiloride-sensitive sodium channels in the lung. Alveolar environment, particularly oxygen tension, steroid exposure, and alveolar distension, are likely to influence assembly of ENaC subunits. Signal transduction pathways mediated by several protein kinases including A, G, and C regulate each of these channel types in different ways. T1 and T2 cells with different channel types (and, therefore, different regulation) will have very different levels of sodium transport that will respond quite differently to hormonal and transmitter agents.
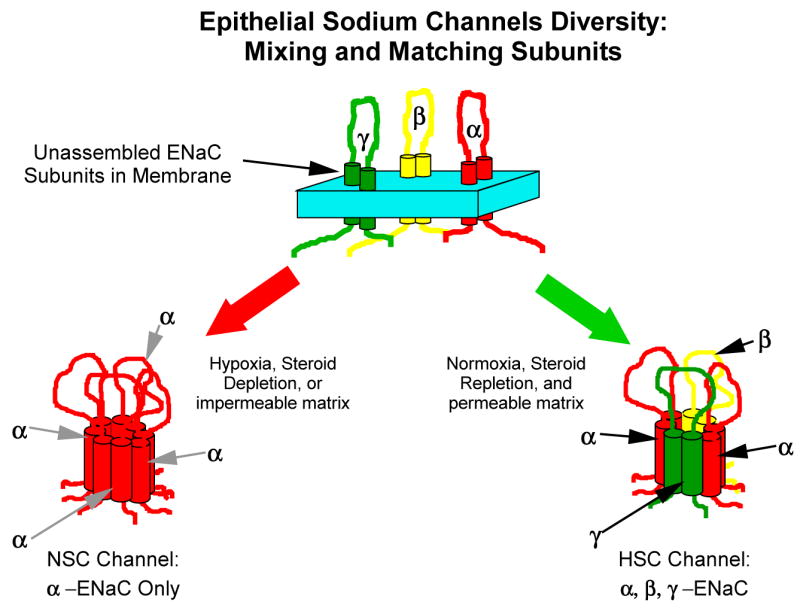
From Jain L, Eaton DC: Physiology of fetal lung fluid clearance and the effect of labor. Semin Perinatol 30:37, 2006 with permission
A large fraction of what we know about fetal lung fluid dynamics is owed to the fetal lamb model. Orzaleski and coworkers108 have shown that, in fetal lambs, lung water content remains fairly constant at 90% to 95% of total lung weight through much of the third trimester. Kitterman and coworkers76 and others26,39 found that, in fetal sheep, lung fluid production begins to decrease a few days before spontaneous vaginal delivery and alveolar fluid volume decreases from approximately 25 to 18 mL/kg. Bland and coworkers21,24,25 showed that preterm delivery and operative delivery without prior labor result in excessive retention of lung fluid in preterm rabbits and in fetal lambs. Sola and Gregory122 showed that colloid oncotic pressure varies with mode of delivery and experience of labor, and may influence epithelial fluid absorption. More recently, Berger and coworkers18 evaluated the effect of lung liquid volume on respiratory performance after cesarean delivery in lamb fetuses. Using chronically catheterized fetal lambs, the investigators found that lambs born with reduced lung liquid volume improved their arterial blood gas and acid base status quicker than those lambs born without a prenatal decrease in their lung liquid volume. This study also confirmed that the experience of vaginal delivery greatly enhances respiratory performance, and this effect is greater than that achieved by simple reduction of lung liquid volume to half in fetuses delivered without enduring labor.
Removal of lung fluid thus started before birth continues postnatally with fluid being carried away by several possible pathways, including pulmonary lymphatics,25,65 blood vessels,112 upper airway, mediastinum, and pleural space.34 There is also recent evidence to show that fetal lung fluid clearance is facilitated by ciliary function99 and that term neonates with genetic defects of cilia structure and/or function (Primary Cliary Dyskinesia, PCD) have a high prevalence of neonatal respiratory disease.99
How is the Fetal Lung Fluid Cleared?
It is now clear that active sodium transport across the pulmonary epithelium drives liquid from lung lumen to the interstitium, with subsequent absorption into the vasculature.71,72 In the lung, sodium reabsorption is a two-step process.92 The first step is passive movement of sodium from lumen across the apical membrane into the cell through sodium permeable ion channels. The second step is active extrusion of sodium from the cell across the basolateral membrane into the serosal space. Several investigators have demonstrated that the initial entry step involves amiloride-sensitive sodium channels. O’Brodovich and coworkers,103 using newborn guinea pigs, have shown that intraluminal instillation of amiloride delays lung fluid clearance. More recent studies using the patch-clamp technique have confirmed the role of AT-I and AT-II cells in the vectorial transport of sodium from the apical surface.70,100,129 Indeed, cDNAs that encode amiloride-sensitive sodium channels in other sodium transporting epithelia have also been cloned from airway epithelial cells.28,29,129 The lung epithelium is believed to switch from a predominantly chloride secreting membrane at birth to a predominantly sodium absorbing membrane after birth.
Studies in human neonates have also shown that immaturity of sodium transport mechanisms contribute to the development of TTN and respiratory distress syndrome.13,51 Gowen and coworkers51 were the first to show that human neonates with TTN had an immaturity of the lung epithelial transport, measured as amiloride-induced drop in potential difference between the nasal epithelium and subcutaneous space. The potential difference was reduced in infants with TTN (suggesting a defect in sodium transport), and recovery from TTN in 1 to 3 days was associated with an increase in potential difference to normal level. Similar studies have now been conducted in premature newborns with hyaline membrane disease (HMD), and the results are consistent with impaired sodium transport in these infants.13 Barker and coworkers13 measured nasal transepithelial potential difference in 31 premature infants<30 weeks gestation. Nasal potential difference is a good measure of the net electrogenic transport of sodium and chloride (dominant ion) across the epithelial layer (PD=resistance × current), and has been shown to mirror image ion transport occurring in the lower respiratory tract. It is recorded as the potential difference between the mucosal surface of a specific region of the nasal epithelium and the subcutaneous space. Authors found that maximal nasal epithelial potential difference increased with birthweight and was lower in infants with RDS. Premature infants without RDS had nasal potential difference similar to normal fullterm infants. Further, the ability of amiloride to affect the potential difference was lower in preterm infants with RDS on day 1 of life, reflecting lower amiloride-sensitive sodium transport. This study provides important evidence for the role of decreased sodium channel activity in the pathogenesis of RDS and the accompanying pulmonary edema. There is additional evidence that the ability of various agents to increase lung fluid absorption in fetal lambs is gestational age-dependent.12,13,26,110,126,130,131 The mechanism for poor response of immature lungs to agents that stimulate sodium transport is not known. Deficiencies could exist in one or more of several steps, including β-receptor, GTP-binding proteins, adenyl cyclase, PK-A, or the sodium channel and its regulatory proteins. Studies have shown that the expression of α-ENaC is developmentally regulated in rats101 and in humans.126
Developmental changes in transepithelial ion and fluid movement in the lung can thus be viewed as occurring in three distinct stages.72 In the first (fetal) stage, the lung epithelium remains in a secretory mode, relying on active chloride secretion via chloride channels and relatively low reabsorption activity of sodium channels. Why the sodium channels remain inactive through much of fetal life is unclear. The second (transitional) stage involves a reversal in the direction of ion and water movement. A multitude of factors may be involved in this transition, including exposure of epithelial cells to an air interface and to high concentrations of steroids and cyclic nucleotides. This stage involves not only increased expression of sodium channels in the lung epithelia, but possibly a switch from nonselective cation channels to highly selective sodium channels. The net increase in sodium movement into the cell can also cause a change in resting membrane potential, leading to a slowing, and eventually a reversal of the direction of chloride movement through chloride channels. The third and final (adult) stage represents lung epithelia with predominantly sodium reabsorption through sodium channels and possibly chloride reabsorption through chloride channels, with a fine balance between the activity of ion channels and tight junctions. Such an arrangement can help ensure adequate humidification of alveolar surface while preventing excessive build up of fluid.
What Causes the Neonatal Lung Epithelium to Switch to an Absorptive Mode?
Our basic science investigations have focused on physiologic changes that trigger the change in lung epithelia from a chloride secretory to a sodium reabsorption mode.67–72 Although several endogenous mediators, including catecholamines, vasopressin, and prolactin, have been proposed to increase lung fluid absorption, none explains this switch convincingly.31,130 Mechanical factors, like stretch and exposure of the epithelial cells to air interface, are other probable candidates that have not been well studied. Jain and coworkers70 have shown that alveolar expression of highly selective sodium channels in the lung epithelia is regulated by the lung microenvironment, especially the presence of glucocorticoids and air interface. Further, regulation of sodium channels is mediated through these factors in a tissue-specific manner.113 For example, aldosterone is a major factor in the kidney and colon, but probably not in the lung.41 In the kidneys, it works by activating transcription of genes for ENaC subunits.41 Of the several factors that have been proposed to have lung-specific effect on sodium reabsorption, some have been investigated, including glucocorticoids, oxygen, β-adrenergics, and surfactant.31,52,68 Key factors in the lung “microenvironment” are steroids, catecholamines, and oxygen.45,70,98,126 Of these factors, based on our animal data and human data from previous studies dealing with preterm gestations, it appears that the most effective strategy for accelerating reabsorption of fetal lung fluid would be the administration of exogenous glucocorticoids.43,48,83,111
High doses of glucocorticoids have been shown to stimulate transcription of ENaC in several sodium transporting epithelia as well as in the lung.126 In the alveolar epithelia, glucocorticoids were found to induce lung sodium reabsorption in the late gestation fetal lung.126 In addition to increasing transcription of sodium channel subunits, steroids increase the number of available channels by decreasing the rate at which membrane associated channels are degraded, and increase the activity of existing channels. Glucocorticoids have also been shown to enhance the responsiveness of lungs to β-adrenergic agents and thyroid hormones.74 The enhanced sodium reabsorption induced by glucocorticoids can be blocked by amiloride, suggesting a role for ENaC. This effect was not observed with triiodothyronine (T3) or with cAMP. Glucocorticoid induction was found to be receptor-mediated and primarily transcriptional. This observation is important because it provides an alternate explanation for the beneficial effect of antenatal steroids on the lung. This study also confirmed the presence of all three subunits of ENaC in the human fetal lung. In the rat fetal lung, O’Brodovich and coworkers101,103 have previously shown that the expression of α-ENaC is markedly increased at ~20 days gestation (corresponding to the saccular stage of lung development) and can be accelerated by exposure to dexamethasone and increased levels of thyroid hormone. Such an effect would translate into accelerated fetal lung fluid reabsorption at birth. Jain and coworkers70 have shown that steroids are highly effective in enhancing the expression of highly selective sodium channels in lung epithelial cells. Under conditions of steroid deprivation, alveolar cells express predominantly a nonselective cation channel that is unlikely to transport the large load of sodium and alveolar fluid clearance imposed at birth. However, when these steroid-deprived (both fetal and adult) cells are exposed to dexamethasone, there is rapid transition to highly selective sodium channels, which are readily seen in other sodium and fluid-transporting systems, such as the kidney and colon.70 In addition, steroids have been shown to have beneficial effects on the surfactant system as well as pulmonary mechanics.43,74,111,121,133,134
Can Rescue Strategies Work once an Infant has Become Symptomatic?
There is considerable evidence to show that high levels of endogenous catecholamines at birth may be important for accelerating alveolar fluid clearance.11,19,45 We31 have shown that β-agonists increase the activity of sodium channels in the lung through a cAMP–PKA-mediated mechanism. It would be logical to conclude, that in the absence of an endogenous surge in fetal catecholamines, exogenous catecholamines would be effective in initiating fetal lung fluid clearance. However, recent studies (surprisingly) show that exogenous addition of epinephrine in guinea pigs failed to stimulate fluid clearance in the newborn lungs.45 There are several possible explanations for this finding. First, catecholamines work on fetal sodium channel (mostly nonselective) by increasing its activity, not by increasing the gene transcription or translation of the proteins required to assemble the channel.31,72 Thus, if the developmentally regulated ENaC channels are not available in adequate numbers at birth, no amount of extra catecholamines is going to make a difference. Steroids, on the other hand, increase the transcription of the ENaC genes, and through another mechanism involving proteosomal degradation, increase the total number of ENaC channels available at birth; however, a longer duration (4–24 hours) of exposure is required for such an effect. Indeed, if these in vitro findings were to hold true in vivo, then neonates exposed to antenatal steroids would be more responsive to other exogenous agents that enhance Sodium channel activity (ie, catecholamines). We60,61 have recently shown that dopamine can greatly enhance sodium channel activity working via a non-cAMP-dependent posttranslational mechanism. Since a reduction (~40%) in fetal lung fluid occurs before spontaneous delivery, and rapid clearance of the remaining fluid within hours after birth is essential for successful transition of the fetus, it is doubtful if postnatal steroid treatment initiated after the infant has become symptomatic will be a successful alternate strategy.
If Cesarean Sections are Here to Stay, Can We Make Them Safer?
As mentioned earlier, delaying elective cesarean birth until 39 weeks seems to be the first logical step in reducing iatrogenic prematurity and excess risk of respiratory distress. Risk of respiratory distress and NICU admissions is inversely proportional to the gestational age. Recent analysis of the MFMU network cesarean section registry by Tito et al confirms this. We believe that antenatal glucocorticoids now have an established role in reducing/preventing life-threatening complications such as hyaline membrane disease related to preterm delivery, after having been introduced in 1972 to enhance fetal lung maturity.33,82 The recommended regimens consist of two 12-mg doses of betamethasone IM given 12 hours apart or four 6-mg doses of dexamethasone IM given 4 hours apart.2 In 1994, an NIH consensus panel strongly recommended the use of antenatal glucocorticoids2 for preterm pregnancies. In recent years, there has been concern about the exposure of early gestation preterm fetuses to repeated courses of antenatal steroids,73 but a single course has been deemed safe.2 There has been only one therapeutic trial evaluating the potential use of antenatal betamethasone in term gestation deliveries by ECS. Stutchfield and coworkers124 recently reported a randomized pragmatic trial evaluating the efficacy of betamethasone in preventing respiratory distress in infants delivered by ECS. Their results show that two doses of betamethasone given in the 48 hours before delivery significantly decreased admissions due to respiratory distress (0.051 in control, 0.024 in the treatment group; RR 0.46, 95% CI 0.23–0.93) (Fig 5). Similarly, Finer and coworkers44 have reported their experience with a protocolized approach to congenital diaphragmatic hernia in which congenital diaphragmatic hernia mothers received antenatal dexamethasone at term followed by elective cesarean delivery. Although no control group without these interventions is available for comparison, the authors reported 78% survival rate. We are currently investigating the safety and efficacy of an antepartum course of betamethasone given for prevention of respiratory morbidity in infants born by ECS.
Figure 5.
Logistic regression model predicting the probability of admission to special care baby unit with respiratory distress by gestation, from a randomised trial of 998 mothers scheduled for ECS at term (≥37 weeks). Mothers in the treatment arm (n=508) received 2 doses of betamethasone 48 hours before delivery. Adapted from Stutchfield P, Whitaker R, Russell I: Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarean section: pragmatic randomised trial. Bmj 331:665,2005, with permission
Summary
In the United States, a significant number of babies each year are delivered by cesarean delivery before onset of spontaneous labor. Although the occurrence of complications such as birth asphyxia, meconium aspiration, and hypoxic ischemic encephalopathy is reduced, a significant number of these infants develop respiratory distress due to failed transition and may require additional treatments like ventilation, surfactant, inhaled nitric oxide, and ECMO. There is an urgent need for preventive and therapeutic interventions that can help to optimize the outcome of this vulnerable population.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Institutes of Health. Cesarean Childbirth. 82–2067. 1981. p. 351. [Google Scholar]
- 2.Effect of corticosteroids for fetal maturation on perinatal outcomes. NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. Jama. 1995;273:413. doi: 10.1001/jama.1995.03520290065031. [DOI] [PubMed] [Google Scholar]
- 3.Indications for cesarean section: final statement of the panel of the National Consensus Conference on Aspects of Cesarean Birth. Cmaj. 1986;134:1348. [PMC free article] [PubMed] [Google Scholar]
- 4.National Institutes of Health state-of-the-science conference statement. Cesarean delivery on maternal request March 27–29, 2006. Obstet Gynecol. 2006;107:1386. [PubMed] [Google Scholar]
- 5.Rates of cesarean delivery-United States: 1991. MMWR Morb Mortal Wkly Rep. 1993;42:285. [PubMed] [Google Scholar]
- 6.Why Does the National U.S. Cesarean Section Rate Keep Going Up? 2007 www.childbirthconnection.org.
- 7.Alderdice F, McCall E, Bailie C, et al. Admission to neonatal intensive care with respiratory morbidity following ‘term’ elective caesarean section. Ir Med J. 2005;98:170. [PubMed] [Google Scholar]
- 8.Althabe F, Belizan JM. Caesarean section: the paradox. Lancet. 2006;368:1472. doi: 10.1016/S0140-6736(06)69616-5. [DOI] [PubMed] [Google Scholar]
- 9.Angus DC, Linde-Zwirble WT, Clermont G, et al. Epidemiology of neonatal respiratory failure in the United States: projections from California and New York. Am J Respir Crit Care Med. 2001;164:1154. doi: 10.1164/ajrccm.164.7.2012126. [DOI] [PubMed] [Google Scholar]
- 10.Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995;149:862. doi: 10.1001/archpedi.1995.02170210036006. [DOI] [PubMed] [Google Scholar]
- 11.Baines DL, Folkesson HG, Norlin A, et al. The influence of mode of delivery, hormonal status and postnatal O2 environment on epithelial sodium channel (ENaC) expression in perinatal guinea-pig lung. J Physiol 522 Pt. 2000;1:147. doi: 10.1111/j.1469-7793.2000.t01-2-00147.xm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barker PM, Brown MJ, Ramsden CA, et al. The effect of thyroidectomy in the fetal sheep on lung liquid reabsorption induced by adrenaline or cyclic AMP. J Physiol. 1988;407:373. doi: 10.1113/jphysiol.1988.sp017421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barker PM, Gowen CW, Lawson EE, et al. Decreased sodium ion absorption across nasal epithelium of very premature infants with respiratory distress syndrome. J Pediatr. 1997;130:373. doi: 10.1016/s0022-3476(97)70198-7. [DOI] [PubMed] [Google Scholar]
- 14.Belizan JM, Althabe F, Barros FC, et al. Rates and implications of caesarean sections in Latin America: ecological study. Bmj. 1999;319:1397. doi: 10.1136/bmj.319.7222.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belizan JM, Althabe F, Cafferata ML. Health consequences of the increasing caesarean section rates. Epidemiology. 2007;18:485. doi: 10.1097/EDE.0b013e318068646a. [DOI] [PubMed] [Google Scholar]
- 16.Benoit Z, Wicky S, Fischer JF, et al. The effect of increased FIO(2) before tracheal extubation on postoperative atelectasis. Anesth Analg. 2002;95:1777. doi: 10.1097/00000539-200212000-00058. [DOI] [PubMed] [Google Scholar]
- 17.Berger PJ, Kyriakides MA, Smolich JJ, et al. Massive decline in lung liquid before vaginal delivery at term in the fetal lamb. Am J Obstet Gynecol. 1998;178:223. doi: 10.1016/s0002-9378(98)80004-5. [DOI] [PubMed] [Google Scholar]
- 18.Berger PJ, Smolich JJ, Ramsden CA, et al. Effect of lung liquid volume on respiratory performance after caesarean delivery in the lamb. J Physiol. 1996;492:905. doi: 10.1113/jphysiol.1996.sp021356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berthiaume Y, Broaddus VC, Gropper MA, et al. Alveolar liquid and protein clearance from normal dog lungs. J Appl Physiol. 1988;65:585. doi: 10.1152/jappl.1988.65.2.585. [DOI] [PubMed] [Google Scholar]
- 20.Berthiaume Y, Staub NC, Matthay MA. Beta-adrenergic agonists increase lung liquid clearance in anesthetized sheep. J Clin Invest. 1987;79:335. doi: 10.1172/JCI112817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bland RD. Dynamics of pulmonary water before and after birth. Acta Paediatr Scand Suppl. 1983;305:12. doi: 10.1111/j.1651-2227.1983.tb09853.x. [DOI] [PubMed] [Google Scholar]
- 22.Bland RD. Loss of liquid from the lung lumen in labor: more than a simple “squeeze”. Am J Physiol Lung Cell Mol Physiol. 2001;280:L602. doi: 10.1152/ajplung.2001.280.4.L602. [DOI] [PubMed] [Google Scholar]
- 23.Bland RD. Lung epithelial ion transport and fluid movement during the perinatal period. Am J Physiol. 1990;259:L30. doi: 10.1152/ajplung.1990.259.2.L30. [DOI] [PubMed] [Google Scholar]
- 24.Bland RD, Bressack MA, McMillan DD. Labor decreases the lung water content of newborn rabbits. Am J Obstet Gynecol. 1979;135:364. doi: 10.1016/0002-9378(79)90706-3. [DOI] [PubMed] [Google Scholar]
- 25.Bland RD, Hansen TN, Haberkern CM, et al. Lung fluid balance in lambs before and after birth. J Appl Physiol. 1982;53:992. doi: 10.1152/jappl.1982.53.4.992. [DOI] [PubMed] [Google Scholar]
- 26.Brown MJ, Olver RE, Ramsden CA, et al. Effects of adrenaline and of spontaneous labour on the secretion and absorption of lung liquid in the fetal lamb. J Physiol. 1983;344:137. doi: 10.1113/jphysiol.1983.sp014929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buckmaster AG, Arnolda G, Wright IM, et al. Continuous positive airway pressure therapy for infants with respiratory distress in non tertiary care centers: a randomized, controlled trial. Pediatrics. 2007;120:509. doi: 10.1542/peds.2007-0775. [DOI] [PubMed] [Google Scholar]
- 28.Canessa CM, Horisberger JD, Rossier BC. Epithelial sodium channel related to proteins involved in neurodegeneration [see comments] Nature. 1993;361:467. doi: 10.1038/361467a0. [DOI] [PubMed] [Google Scholar]
- 29.Canessa CM, Schild L, Buell G, et al. Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature. 1994;367:463. doi: 10.1038/367463a0. [DOI] [PubMed] [Google Scholar]
- 30.Chang L. WebMD. 2008. Elective Cesarean: Babies on Demand. [Google Scholar]
- 31.Chen XJ, Eaton DC, Jain L. Beta-adrenergic regulation of amiloride-sensitive lung sodium channels. Am J Physiol Lung Cell Mol Physiol. 2002;282:L609. doi: 10.1152/ajplung.00356.2001. [DOI] [PubMed] [Google Scholar]
- 32.Clark RH. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25:251. doi: 10.1038/sj.jp.7211242. [DOI] [PubMed] [Google Scholar]
- 33.Crowley PA. Antenatal corticosteroid therapy: a meta-analysis of the randomized trials, 1972 to 1994. Am J Obstet Gynecol. 1995;173:322. doi: 10.1016/0002-9378(95)90222-8. [DOI] [PubMed] [Google Scholar]
- 34.Cummings J, et al. Lung luminal liquid is not removed via the pleural space in health newborn lambs. Physiologist. 1989;32:202. [Google Scholar]
- 35.Davidoff MJ, Dias T, Damus K, et al. Changes in the gestational age distribution among U.S. singleton births: impact on rates of late preterm birth, 1992 to 2002. Semin Perinatol. 2006;30:8. doi: 10.1053/j.semperi.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 36.Declercq E, Menacker F, Macdorman M. Maternal risk profiles and the primary cesarean rate in the United States, 1991–2002. Am J Public Health. 2006;96:867. doi: 10.2105/AJPH.2004.052381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Declercq E, Menacker F, MacDorman M. Rise in “no indicated risk” primary caesareans in the United States, 1991–2001: cross sectional analysis. Bmj. 2005;330:71. doi: 10.1136/bmj.38279.705336.0B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Declercq E, Sakala C, Corry M, et al. Listening to Mothers II: The Second National U.S. Survey of Women’s Childbearing Experiences. New York: Childbirth Connection; 2006. p. 1. [Google Scholar]
- 39.Dickson KA, Maloney JE, Berger PJ. Decline in lung liquid volume before labor in fetal lambs. J Appl Physiol. 1986;61:2266. doi: 10.1152/jappl.1986.61.6.2266. [DOI] [PubMed] [Google Scholar]
- 40.Donaldsson SF, Dagbjartsson A, Bergsteinsson H, et al. [Respiratory dysfunction in infants born by elective cesarean section without labor] Laeknabladid. 2007;93:675. [PubMed] [Google Scholar]
- 41.Eaton D, Ohara A, Ling BN. Cellular regulation of amiloride blockable Na+ channels. Biomed Res. 1991;12:31. [Google Scholar]
- 42.Ersch J, Roth-Kleiner M, Baeckert P, et al. Increasing incidence of respiratory distress in neonates. Acta Paediatr. 2007;96:1577. doi: 10.1111/j.1651-2227.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- 43.Ervin MG, Berry LM, Ikegami M, et al. Single dose fetal betamethasone administration stabilizes postnatal glomerular filtration rate and alters endocrine function in premature lambs. Pediatr Res. 1996;40:645. doi: 10.1203/00006450-199611000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Finer NN, Tierney A, Etches PC, et al. Congenital diaphragmatic hernia: developing a protocolized approach. J Pediatr Surg. 1998;33:1331. doi: 10.1016/s0022-3468(98)90001-x. [DOI] [PubMed] [Google Scholar]
- 45.Finley N, Norlin A, Baines DL, et al. Alveolar epithelial fluid clearance is mediated by endogenous catecholamines at birth in guinea pigs. J Clin Invest. 1998;101:972. doi: 10.1172/JCI1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fisler RE, Cohen A, Ringer SA, et al. Neonatal outcome after trial of labor compared with elective repeat cesarean section. Birth. 2003;30:83. doi: 10.1046/j.1523-536x.2003.00225.x. [DOI] [PubMed] [Google Scholar]
- 47.Gerten KA, Coonrod DV, Bay RC, et al. Cesarean delivery and respiratory distress syndrome: does labor make a difference? Am J Obstet Gynecol. 2005;193:1061. doi: 10.1016/j.ajog.2005.05.038. [DOI] [PubMed] [Google Scholar]
- 48.Goldenberg RL, Jobe AH. Prospects for research in reproductive health and birth outcomes. Jama. 2001;285:633. doi: 10.1001/jama.285.5.633. [DOI] [PubMed] [Google Scholar]
- 49.Goldenberg RL, Nelson K. Iatrogenic respiratory distress syndrome. An analysis of obstetric events preceding delivery of infants who develop respiratory distress syndrome. Am J Obstet Gynecol. 1975;123:617. [PubMed] [Google Scholar]
- 50.Gouyon JB, Ribakovsky C, Ferdynus C, et al. Severe respiratory disorders in term neonates. Paediatr Perinat Epidemiol. 2008;22:22. doi: 10.1111/j.1365-3016.2007.00875.x. [DOI] [PubMed] [Google Scholar]
- 51.Gowen CW, Jr, Lawson EE, Gingras J, et al. Electrical potential difference and ion transport across nasal epithelium of term neonates: correlation with mode of delivery, transient tachypnea of the newborn, and respiratory rate. J Pediatr. 1988;113:121. doi: 10.1016/s0022-3476(88)80545-6. [DOI] [PubMed] [Google Scholar]
- 52.Guidot DM, Modelska K, Lois M, et al. Ethanol ingestion via glutathione depletion impairs alveolar epithelial barrier function in rats. Am J Physiol Lung Cell Mol Physiol. 2000;279:L127. doi: 10.1152/ajplung.2000.279.1.L127. [DOI] [PubMed] [Google Scholar]
- 53.Hack M, Fanaroff AA, Klaus MH, et al. Neonatal respiratory distress following elective delivery. A preventable disease? Am J Obstet Gynecol. 1976;126:43. doi: 10.1016/0002-9378(76)90462-2. [DOI] [PubMed] [Google Scholar]
- 54.Hales KA, Morgan MA, Thurnau GR. Influence of labor and route of delivery on the frequency of respiratory morbidity in term neonates. Int J Gynaecol Obstet. 1993;43:35. doi: 10.1016/0020-7292(93)90271-w. [DOI] [PubMed] [Google Scholar]
- 55.Halliday HL. Elective delivery at “term”: implications for the newborn. Acta Paediatr. 1999;88:1180. doi: 10.1080/080352599750030257. [DOI] [PubMed] [Google Scholar]
- 56.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl vital stat rep. 2007;56:1. [PubMed] [Google Scholar]
- 57.Hankins GD, Longo M. The role of stillbirth prevention and late preterm (near-term) births. Semin Perinatol. 2006;30:20. doi: 10.1053/j.semperi.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 58.Hansen AK, Wisborg K, Uldbjerg N, et al. Elective caesarean section and respiratory morbidity in the term and near-term neonate. Acta Obstet Gynecol Scand. 2007;86:389. doi: 10.1080/00016340601159256. [DOI] [PubMed] [Google Scholar]
- 59.Hansen AK, Wisborg K, Uldbjerg N, et al. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. Bmj. 2008;336:85. doi: 10.1136/bmj.39405.539282.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Helms MN, Chen XJ, Ramosevac S, et al. Dopamine regulation of amiloride-sensitive sodium channels in lung cells. Am J Physiol Lung Cell Mol Physiol. 2006;290:L710. doi: 10.1152/ajplung.00486.2004. [DOI] [PubMed] [Google Scholar]
- 61.Helms MN, Self J, Bao HF, et al. Dopamine activates amiloride-sensitive sodium channels in alveolar type I cells in lung slice preparations. Am J Physiol Lung Cell Mol Physiol. 2006;291:L610. doi: 10.1152/ajplung.00426.2005. [DOI] [PubMed] [Google Scholar]
- 62.Heritage CK, Cunningham MD. Association of elective repeat cesarean delivery and persistent pulmonary hypertension of the newborn. Am J Obstet Gynecol. 1985;152:627. doi: 10.1016/s0002-9378(85)80034-x. [DOI] [PubMed] [Google Scholar]
- 63.Hibbard J, Torre MD. Contemporary OB/GYN. Vol. 38. 2006. Grand Rounds: When mom requests a cesarean. [Google Scholar]
- 64.Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997;100:348. doi: 10.1542/peds.100.3.348. [DOI] [PubMed] [Google Scholar]
- 65.Humphreys P, et al. Pulmonary lymph flow and the uptake of liquid from the lungs of lamb at the start of breathing. J Physiol. 1967;193:1. doi: 10.1113/jphysiol.1967.sp008340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jain L. Alveolar fluid clearance in developing lungs and its role in neonatal transition. Clin Perinatol. 1999;26:585. [PubMed] [Google Scholar]
- 67.Jain L. Alveolar fluid clearance in developing lungs and its role in neonatal transition. Clin Perinatol. 1999;26:585. [PubMed] [Google Scholar]
- 68.Jain L, Chen XJ, Brown LA, et al. Nitric oxide inhibits lung sodium transport through a cGMP-mediated inhibition of epithelial cation channels. Am J Physiol. 1998;274:L475. doi: 10.1152/ajplung.1998.274.4.L475. [DOI] [PubMed] [Google Scholar]
- 69.Jain L, Chen XJ, Malik B, et al. Antisense oligonucleotides against the alpha-subunit of ENaC decrease lung epithelial cation-channel activity. Am J Physiol. 1999;276:L1046. doi: 10.1152/ajplung.1999.276.6.L1046. [DOI] [PubMed] [Google Scholar]
- 70.Jain L, Chen XJ, Ramosevac S, et al. Expression of highly selective sodium channels in alveolar type II cells is determined by culture conditions. Am J Physiol Lung Cell Mol Physiol. 2001;280:L646. doi: 10.1152/ajplung.2001.280.4.L646. [DOI] [PubMed] [Google Scholar]
- 71.Jain L, Eaton DC. Alveolar fluid transport: a changing paradigm. Am J Physiol Lung Cell Mol Physiol. 2006;290:L646. doi: 10.1152/ajplung.00496.2005. [DOI] [PubMed] [Google Scholar]
- 72.Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Semin Perinatol. 2006;30:34. doi: 10.1053/j.semperi.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 73.Jobe AH. Glucocorticoids in perinatal medicine: Misguided rockets? The Journal of Pediatrics. 2000;137:1. doi: 10.1067/mpd.2000.107801. [DOI] [PubMed] [Google Scholar]
- 74.Jobe AH, Ikegami M, Padbury J, et al. Combined effects of fetal beta agonist stimulation and glucocorticoids on lung function of preterm lambs. Biol Neonate. 1997;72:305. doi: 10.1159/000244497. [DOI] [PubMed] [Google Scholar]
- 75.Keszler M, Carbone MT, Cox C, et al. Severe respiratory failure after elective repeat cesarean delivery: a potentially preventable condition leading to extracorporeal membrane oxygenation. Pediatrics. 1992;89:670. [PubMed] [Google Scholar]
- 76.Kitterman JA, Ballard PL, Clements JA, et al. Tracheal fluid in fetal lambs: spontaneous decrease prior to birth. J Appl Physiol. 1979;47:985. doi: 10.1152/jappl.1979.47.5.985. [DOI] [PubMed] [Google Scholar]
- 77.Kolas T, Saugstad OD, Daltveit AK, et al. Planned cesarean versus planned vaginal delivery at term: comparison of newborn infant outcomes. Am J Obstet Gynecol. 2006;195:1538. doi: 10.1016/j.ajog.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 78.Landon MB, Hauth JC, Leveno KJ, et al. Maternal and Perinatal Outcomes Associated with a Trial of Labor after Prior Cesarean Delivery. N Engl J Med. 2004;351:2581. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 79.Lavender T, Kingdon C, Hart A, et al. Could a randomised trial answer the controversy relating to elective caesarean section? National survey of consultant obstetricians and heads of midwifery. Bmj. 2005;331:490. doi: 10.1136/bmj.38560.572639.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Leder M, Hirschfeld S, Fanaroff A. Persistent fetal circulation: an epidemiologic study. Pediatr Res. 1980;14:490. [Google Scholar]
- 81.Levine EM, Ghai V, Barton JJ, et al. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol. 2001;97:439. doi: 10.1016/s0029-7844(00)01150-9. [DOI] [PubMed] [Google Scholar]
- 82.Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50:515. [PubMed] [Google Scholar]
- 83.Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50:515. [PubMed] [Google Scholar]
- 84.M. Maurice Abitbol UBT-RPTBET. Effect of modern obstetrics on mothers from third-world countries. The Journal of Maternal-Fetal Medicine. 1997;6:276. doi: 10.1002/(SICI)1520-6661(199709/10)6:5<276::AID-MFM7>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 85.MacDorman MF, Declercq E, Menacker F, et al. Infant and neonatal mortality for primary cesarean and vaginal births to women with “no indicated risk,” United States, 1998–2001 birth cohorts. Birth. 2006;33:175. doi: 10.1111/j.1523-536X.2006.00102.x. [DOI] [PubMed] [Google Scholar]
- 86.Macdorman MF, Declercq E, Menacker F, et al. Neonatal mortality for low-risk women by method of delivery. Birth. 2007;34:101. doi: 10.1111/j.1523-536X.2006.00155_3.x. [DOI] [PubMed] [Google Scholar]
- 87.Madar J, Richmond S, Hey E. Surfactant-deficient respiratory distress after elective delivery at ‘term’. Acta Paediatr. 1999;88:1244. doi: 10.1080/080352599750030365. [DOI] [PubMed] [Google Scholar]
- 88.Maisels MJ, Rees R, Marks K, et al. Elective delivery of the term fetus. An obstetrical hazard Jama. 1977;238:2036. [PubMed] [Google Scholar]
- 89.Many A, Helpman L, Vilnai Y, et al. Neonatal respiratory morbidity after elective cesarean section. J Matern Fetal Neonatal Med. 2006;19:75. doi: 10.1080/14767050500333868. [DOI] [PubMed] [Google Scholar]
- 90.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007;56:1. [PubMed] [Google Scholar]
- 91.Matthay MA, Berthiaume Y, Staub NC. Long-term clearance of liquid and protein from the lungs of unanesthetized sheep. J Appl Physiol. 1985;59:928. doi: 10.1152/jappl.1985.59.3.928. [DOI] [PubMed] [Google Scholar]
- 92.Matthay MA, Folkesson HG, Verkman AS. Salt and water transport across alveolar and distal airway epithelia in the adult lung. Am J Physiol. 1996;270:L487. doi: 10.1152/ajplung.1996.270.4.L487. [DOI] [PubMed] [Google Scholar]
- 93.Matthay MA, Landolt CC, Staub NC. Differential liquid and protein clearance from the alveoli of anesthetized sheep. J Appl Physiol. 1982;53:96. doi: 10.1152/jappl.1982.53.1.96. [DOI] [PubMed] [Google Scholar]
- 94.McCourt C, Weaver J, Statham H, et al. Elective cesarean section and decision making: a critical review of the literature. Birth. 2007;34:65. doi: 10.1111/j.1523-536X.2006.00147.x. [DOI] [PubMed] [Google Scholar]
- 95.McMahon MJ, Luther ER, Bowes WA, et al. Comparison of a Trial of Labor with an Elective Second Cesarean Section. N Engl J Med. 1996;335:689. doi: 10.1056/NEJM199609053351001. [DOI] [PubMed] [Google Scholar]
- 96.Menacker F, Declercq E, Macdorman MF. Cesarean delivery: background, trends, and epidemiology. Semin Perinatol. 2006;30:235. doi: 10.1053/j.semperi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 97.Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995;102:101. doi: 10.1111/j.1471-0528.1995.tb09060.x. [DOI] [PubMed] [Google Scholar]
- 98.Mustafa SB, DiGeronimo RJ, Petershack JA, et al. Postnatal glucocorticoids induce alpha-ENaC formation and regulate glucocorticoid receptors in the preterm rabbit lung. Am J Physiol Lung Cell Mol Physiol. 2004;286:L73. doi: 10.1152/ajplung.00342.2002. [DOI] [PubMed] [Google Scholar]
- 99.Noone PG, Leigh MW, Sannuti A, et al. Primary ciliary dyskinesia: diagnostic and phenotypic features. Am J Respir Crit Care Med. 2004;169:459. doi: 10.1164/rccm.200303-365OC. [DOI] [PubMed] [Google Scholar]
- 100.O’Brodovich H. Epithelial ion transport in the fetal and perinatal lung. Am J Physiol. 1991;261:C555. doi: 10.1152/ajpcell.1991.261.4.C555. [DOI] [PubMed] [Google Scholar]
- 101.O’Brodovich H, Canessa C, Ueda J, et al. Expression of the epithelial Na+ channel in the developing rat lung. Am J Physiol. 1993;265:C491. doi: 10.1152/ajpcell.1993.265.2.C491. [DOI] [PubMed] [Google Scholar]
- 102.O’Brodovich H, Hannam V, Rafii B. Sodium channel but neither Na(+)-H+ nor Na-glucose symport inhibitors slow neonatal lung water clearance. Am J Respir Cell Mol Biol. 1991;5:377. doi: 10.1165/ajrcmb/5.4.377. [DOI] [PubMed] [Google Scholar]
- 103.O’Brodovich H, Hannam V, Seear M, et al. Amiloride impairs lung water clearance in newborn guinea pigs. J Appl Physiol. 1990;68:1758. doi: 10.1152/jappl.1990.68.4.1758. [DOI] [PubMed] [Google Scholar]
- 104.O’Brodovich HM. Immature epithelial Na+ channel expression is one of the pathogenetic mechanisms leading to human neonatal respiratory distress syndrome. Proc Assoc Am Physicians. 1996;108:345. [PubMed] [Google Scholar]
- 105.O’Brodovich HM. Respiratory distress syndrome: the importance of effective transport. J Pediatr. 1997;130:342. [PubMed] [Google Scholar]
- 106.O’Brodovich HM. Respiratory distress syndrome: the importance of effective transport [editorial; comment] J Pediatr. 1997;130:342. [PubMed] [Google Scholar]
- 107.O’Brodovich HM. The role of active Na+ transport by lung epithelium in the clearance of airspace fluid. New Horiz. 1995;3:240. [PubMed] [Google Scholar]
- 108.Orzalesi M, et al. The development of the lung of lambs. Pediatrics. 1965;35:373. [PubMed] [Google Scholar]
- 109.Parilla BV, Dooley SL, Jansen RD, et al. Iatrogenic respiratory distress syndrome following elective repeat cesarean delivery. Obstet Gynecol. 1993;81:392. [PubMed] [Google Scholar]
- 110.Perks AM, Cassin S. The effects of arginine vasopressin and epinephrine on lung liquid production in fetal goats. Can J Physiol Pharmacol. 1989;67:491. doi: 10.1139/y89-078. [DOI] [PubMed] [Google Scholar]
- 111.Pillow JJ, Hall GL, Willet KE, et al. Effects of gestation and antenatal steroid on airway and tissue mechanics in newborn lambs. Am J Respir Crit Care Med. 2001;163:1158. doi: 10.1164/ajrccm.163.5.9906098. [DOI] [PubMed] [Google Scholar]
- 112.Raj JU, Bland RD. Lung luminal liquid clearance in newborn lambs. Effect of pulmonary microvascular pressure elevation. Am Rev Respir Dis. 1986;134:305. doi: 10.1164/arrd.1986.134.2.305. [DOI] [PubMed] [Google Scholar]
- 113.Renard S, Voilley N, Bassilana F, et al. Localization and regulation by steroids of the alpha, beta and gamma subunits of the amiloride-sensitive Na+ channel in colon, lung and kidney. Pflugers Arch. 1995;430:299. doi: 10.1007/BF00373903. [DOI] [PubMed] [Google Scholar]
- 114.Richardson BS, Czikk MJ, daSilva O, et al. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. 2005;192:219. doi: 10.1016/j.ajog.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 115.Riskin A, Abend-Weinger M, Riskin-Mashiah S, et al. Cesarean section, gestational age, and transient tachypnea of the newborn: timing is the key. Am J Perinatol. 2005;22:377. doi: 10.1055/s-2005-872594. [DOI] [PubMed] [Google Scholar]
- 116.Ross MG, Beall MH. Cesarean section and transient tachypnea of the newborn. Am J Obstet Gynecol. 2006;195:1496. doi: 10.1016/j.ajog.2006.01.089. [DOI] [PubMed] [Google Scholar]
- 117.Roth-Kleiner M, Wagner BP, Bachmann D, et al. Respiratory distress syndrome in near-term babies after caesarean section. Swiss Med Wkly. 2003;133:283. doi: 10.4414/smw.2003.10121. [DOI] [PubMed] [Google Scholar]
- 118.Rothen HU, Sporre B, Engberg G, et al. Reexpansion of atelectasis during general anaesthesia may have a prolonged effect. Acta Anaesthesiol Scand. 1995;39:118. doi: 10.1111/j.1399-6576.1995.tb05602.x. [DOI] [PubMed] [Google Scholar]
- 119.Rothen HU, Sporre B, Engberg G, et al. Influence of gas composition on recurrence of atelectasis after a reexpansion maneuver during general anesthesia. Anesthesiology. 1995;82:832. doi: 10.1097/00000542-199504000-00004. [DOI] [PubMed] [Google Scholar]
- 120.Smith GCS, Pell JP, Cameron AD, et al. Risk of Perinatal Death Associated With Labor After Previous Cesarean Delivery in Uncomplicated Term Pregnancies. JAMA. 2002;287:2684. doi: 10.1001/jama.287.20.2684. [DOI] [PubMed] [Google Scholar]
- 121.Smith LM, Ervin MG, Wada N, et al. Antenatal glucocorticoids alter postnatal preterm lamb renal and cardiovascular responses to intravascular volume expansion. Pediatr Res. 2000;47:622. doi: 10.1203/00006450-200005000-00011. [DOI] [PubMed] [Google Scholar]
- 122.Sola A, Gregory GA. Colloid osmotic pressure of normal newborns and premature infants. Crit Care Med. 1981;9:568. doi: 10.1097/00003246-198108000-00002. [DOI] [PubMed] [Google Scholar]
- 123.Spong CY, Landon MB, Gilbert S, et al. Risk of uterine rupture and adverse perinatal outcome at term after cesarean delivery. Obstet Gynecol. 2007;110:801. doi: 10.1097/01.AOG.0000284622.71222.b2. [DOI] [PubMed] [Google Scholar]
- 124.Stutchfield P, Whitaker R, Russell I. Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarean section: pragmatic randomised trial. Bmj. 2005;331:662. doi: 10.1136/bmj.38547.416493.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.van den Berg A, van Elburg RM, van Geijn HP, et al. Neonatal respiratory morbidity following elective caesarean section in term infants. A 5-year retrospective study and a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2001;98:9. doi: 10.1016/s0301-2115(01)00292-5. [DOI] [PubMed] [Google Scholar]
- 126.Venkatesh VC, Katzberg HD. Glucocorticoid regulation of epithelial sodium channel genes in human fetal lung. Am J Physiol. 1997;273:L227. doi: 10.1152/ajplung.1997.273.1.L227. [DOI] [PubMed] [Google Scholar]
- 127.Villar J, Carroli G, Zavaleta N, et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. Bmj. 2007;335:1025. doi: 10.1136/bmj.39363.706956.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Villar J, Valladares E, Wojdyla D, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367:1819. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 129.Voilley N, Lingueglia E, Champigny G, et al. The lung amiloride-sensitive Na+ channel: biophysical properties, pharmacology, ontogenesis, and molecular cloning. Proc Natl Acad Sci U S A. 1994;91:247. doi: 10.1073/pnas.91.1.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wallace MJ, Hooper SB, Harding R. Regulation of lung liquid secretion by arginine vasopressin in fetal sheep. Am J Physiol. 1990;258:R104. doi: 10.1152/ajpregu.1990.258.1.R104. [DOI] [PubMed] [Google Scholar]
- 131.Walters DV, Ramsden CA, Olver RE. Dibutyryl cAMP induces a gestation-dependent absorption of fetal lung liquid. J Appl Physiol. 1990;68:2054. doi: 10.1152/jappl.1990.68.5.2054. [DOI] [PubMed] [Google Scholar]
- 132.Wax JR, Cartin A, Pinette MG, et al. Patient choice cesarean: an evidence-based review. Obstet Gynecol Surv. 2004;59:601. doi: 10.1097/01.ogx.0000133942.76239.57. [DOI] [PubMed] [Google Scholar]
- 133.Willet KE, Jobe AH, Ikegami M, et al. Lung morphometry after repetitive antenatal glucocorticoid treatment in preterm sheep. Am J Respir Crit Care Med. 2001;163:1437. doi: 10.1164/ajrccm.163.6.2003098. [DOI] [PubMed] [Google Scholar]
- 134.Willet KE, Jobe AH, Ikegami M, et al. Antenatal endotoxin and glucocorticoid effects on lung morphometry in preterm lambs. Pediatr Res. 2000;48:782. doi: 10.1203/00006450-200012000-00014. [DOI] [PubMed] [Google Scholar]
- 135.Zanardo V, Padovani E, Pittini C, et al. The influence of timing of elective cesarean section on risk of neonatal pneumothorax. J Pediatr. 2007;150:252. doi: 10.1016/j.jpeds.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 136.Zanardo V, Simbi AK, Franzoi M, et al. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatrica. 2004;93:643. doi: 10.1111/j.1651-2227.2004.tb02990.x. [DOI] [PubMed] [Google Scholar]
- 137.Zanardo V, Simbi AK, Franzoi M, et al. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr. 2004;93:643. doi: 10.1111/j.1651-2227.2004.tb02990.x. [DOI] [PubMed] [Google Scholar]