Abstract
OBJECTIVE—Women with diabetes have a high incidence and complication rate of urinary tract infections (UTIs). Our aims were to compare current treatment strategies with respect to recurrence rates in women with diabetes with those without diabetes.
RESEARCH DESIGN AND METHODS—We used a Dutch registration database containing pharmacy dispensing data. A total of 10,366 women with diabetes (17.5% premenopausal) (aged ≤55 years) and 200,258 women without diabetes (68% premenopausal) who received a first course of trimethoprim, nitrofurantoin, fosfomycin, or norfloxacin between January 1999 and January 2006 were included. We compared short (≤5 days) with long (>5 days) prescriptions and norfloxacin with trimethoprim, nitrofurantoin, and fosfomycin. A recurrence was defined as a second prescription for one of the above-mentioned agents or a first with amoxicillin (clavulanic acid), fluoroquinolones, or trimethoprim/sulfamethoxazole between 6 and 30 days after inclusion.
RESULTS—Premenopausal women with diabetes more often received a long (26.5 vs. 19.2%; P < 0.001) treatment with norfloxacin (10.7 vs. 6.2%; P < 0.001) but still had a higher recurrence rate (16.1 vs. 12.2%; P = 0.003) compared with those without diabetes. Similarly, postmenopausal women with diabetes more often received a longer (32.8 vs. 28.8%; P < 0.001) treatment with norfloxacin (15.2 vs. 12.7%; P < 0.001) but had a higher recurrence rate (19.1 vs. 16.4%; P < 0.001) compared with those without diabetes.
CONCLUSIONS—Despite the fact that patients with diabetes more often received longer and more potent initial treatment than patients without diabetes, pre- and postmenopausal women with diabetes more often had recurrences of their UTIs.
Diabetes is an increasingly important endocrine disease. Incidence of infections is increased in diabetic (type 1 and type 2) patients compared with control subjects (1,2), and the urinary tract is the most prevalent site of these infections (3). Furthermore, diabetic patients with a urinary tract infection (UTI) more often develop severe and rare complications, such as emphysematous cystitis and papillary necrosis (4,5). Studies addressing differences in UTI recurrence rates between diabetic patients and control subjects show contradictory results for uncomplicated lower (2,6) and upper (7,8) UTIs. Currently, there are no controlled clinical trials investigating the optimal antimicrobial treatment strategy in diabetic patients with UTIs. Current recommendations rely on the opinion of experts (5,9). It is generally recommended to treat UTIs in diabetic patients with antibiotics with high tissue penetration for 7–14 days. Importantly, we lack data on the clinical practice of how diabetic patients with a UTI are actually treated, to assess recurrence rates.
The aims of this study are to describe the treatments (duration and agents) for uncomplicated UTIs in women with and without diabetes in the Netherlands and to analyze recurrence rates of these UTIs within 30 days after the last treatment.
RESEARCH DESIGN AND METHODS
Database
Data were obtained from the PHARMO Record Linkage System. The PHARMO Institute is an independent scientific research organization dedicated to studying drug use and outcomes in daily practice in the Netherlands. The PHARMO Record Linkage System includes, among other databases, the drug dispensing records from community pharmacies linked to hospital discharge records of more than 2 million community-dwelling inhabitants of 40 demographically well-defined Dutch regions. For all residents, the computerized drug dispensing histories contain data concerning the dispensed drug, prescriber specialty, dispensing date, dispensed amount, prescribed dose regimens, and the legend duration of use (prescription length). All drugs are coded according to the Anatomical Therapeutic Chemical Classification. The hospital records include detailed information concerning the primary and secondary diagnoses, procedures, and dates of hospital admission and discharge. All diagnoses are coded according to the ICD-9-CM (available at http://www.pharmo.nl/). Data between 1 January 1999 and 31 December 2005 were used.
Inclusion criteria
Data of all women aged >12 years, receiving at least one prescription of trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin (6) in the period after the first of January 1999 and first of January 2006 with follow-up data of at least 30 days, were extracted.
Following the Dutch guidelines, trimethoprim/sulfamethoxazole, amoxicillin, and fluorquinolones other than norfloxacin are rarely prescribed for uncomplicated UTIs because of the high resistance rates (available at http://www.swab.nl) in the Netherlands or due to the advice to preserve these antibiotics for complicated UTIs.
Exclusion criteria
To limit the study population to women with uncomplicated UTIs, we wanted to exclude all women with possible recurrent UTIs because of secondary diseases or underlying abnormalities. Therefore, all factors that belong to the definition of complicated UTIs (10) were considered exclusion criteria:
Pregnancy (delivery during the follow-up period or folic acid prescription in the preceding year and during the follow-up).
Patients with known anatomical abnormalities, for example, indwelling urinary catheter or hospitalization for a urethral stricture in the follow-up period.
The use of the following medication in the preceding year and during the follow-up: antiretroviral treatment for HIV; immune suppressive drugs; chemotherapy; and medication for renal insufficiency, such as calcium binding agents.
Patients receiving a first prescription with duration of >30 days.
Patients with a second prescription within 5 days after their first prescription, indicating acute side effects or loss of recipe or medication.
Patients receiving in the preceding year trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin, indicating prophylaxis for recurrent UTIs.
Outcome parameters
The primary outcome was the prescription for a second antibiotic course or a hospitalization admission for a UTI during the follow-up period.
Definitions
The cohort entry date was defined as the day that the patient received her first prescription trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin. The history period was defined as 1 year before study inclusion. The follow-up period was defined as the duration of the first prescription plus 30 days after the cohort entry date. Patients with diabetes were defined by prescription of one or more glucose-lowering medications (tablets or insulin) in the history or in the follow-up period.
Premenopausal women were defined as aged ≤55 years at the dispensing date of their first prescription. Postmenopausal women were women aged >55 years at the moment of the dispensing date of their first prescription. This is a conservative definition of postmenopausal women, since the worldwide mean age of menopause is 49.2 years.
A “new” diagnosis of UTI (inclusion criteria for this study) was defined as a patient with no prescription for trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin in the history (1 year) and a first prescription for trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin in the period from 1 January 1999 to 31 December 2005. The first prescription is always one of the following antibiotics: trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin. A recurrent UTI was defined as a prescription for trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin or amoxicillin, fluoroquinolones, amoxicillin/clavulanic acid, or trimethoprim/sulfamethoxazole in the follow-up period (5 days after the first prescription until 30 days after the end of the first prescription) or hospitalization admission with the diagnosis of a UTI. These recurrences could be relapses (second infection with the same organism) or reinfections (second infection with a different organism). Hospital admissions were included as cases diagnosed according to the ICD-9 system with either a kidney infection (590), cystitis (595), urethritis (not sexually transmitted) (597), urethral syndrome (597), or other disorders of urethra and urinary tract (599).
Some of the above-mentioned antibiotics for a recurrent UTI could also be used for other diseases than UTIs. To exclude antibiotics prescriptions for other infections than a UTI, all analyses were repeated with the use of comedication, defined as medication given at the same moment as the antibiotic for a recurrent UTI from one of the following anatomical therapeutic chemical groups: A (gastrointestinal), D (skin), R (respiratory), and S (ear or eye). Similarly, analyses were repeated with prescriptions from other specialties than general practitioners excluded.
Aggressive treatment for a UTI was defined as a treatment with an antibiotic that has high tissue penetration (in kidney and prostate). For the first prescription agents only, norfloxacin has this potency.
Statistical analyses and ethics
Data were analyzed using SPSS software for Windows, version 14.0. Medication use and recurrence rate were compared between women with and without diabetes. Analyses were done with a χ2 test. We corrected for age by comparing different age strata. A P value <0.05 was considered to be statistically significant.
Ethical approval was not necessary because all data were anonymized before entering the PHARMO database. Researchers only have information on sex and age of the patient. All other identifying information is deleted after the linkage with the hospital records from the national registry. This approach has been approved by the Dutch Data Protection Authority (6).
RESULTS
Inclusion criteria
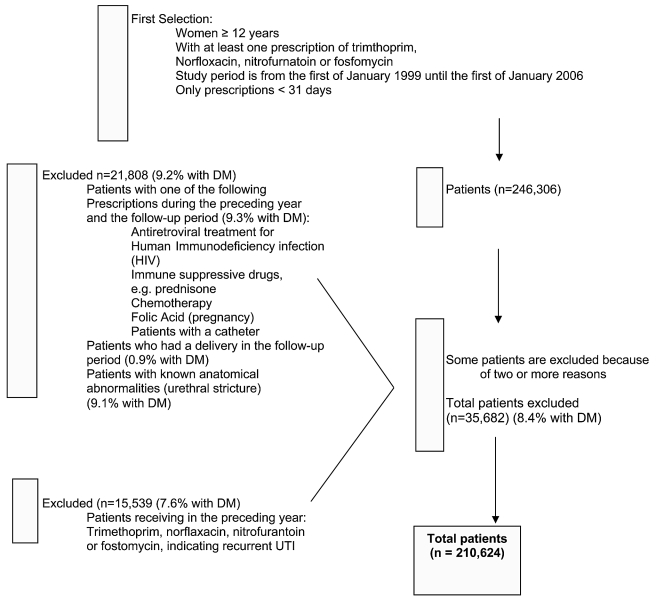
Initially, the database consisted of 246,306 women who were aged ≥12 years and received a prescription for trimethoprim, norfloxacin, nitrofurantoin, or fosfomycin in the study period (Fig. 1).
Figure 1—
Numbers of included and excluded women in the total study group.
Exclusion criteria
A total of 21,808 women were excluded for different reasons (Fig. 1), and another 15,539 women were excluded because they had a UTI in the year before the cohort entry date. Finally, the study included 210,624 women: 10,366 women with diabetes (17.5% premenopausal women aged ≤55 years) and 200,258 women without diabetes (68% premenopausal).
Premenopausal women
Baseline characteristics of the premenopausal women are shown in Table 1. Percentage of prescriptions with norfloxacin were significantly higher and the treatment duration was significantly longer in premenopausal women with diabetes compared with those without. The recurrence rate (Table 2) was significantly higher in premenopausal women with diabetes: 16.1% in women with diabetes and 12.2% in women without diabetes (P = 0.002). There was no significant difference between hospitalization of women with and without diabetes (0.1 vs. 0.1%, P = 0.790). In both analyses, the results were similar in age strata.
Table 1—
Treatment of UTIs in pre- and postmenopausal women with and without diabetes
| Premenopausal women
|
Postmenopausal women
|
|||||
|---|---|---|---|---|---|---|
| With diabetes | Without diabetes | P value | With diabetes | Without diabetes | P value | |
| n | 1,817 | 136,195 | 8,549 | 64,063 | ||
| Age (years) | 47 (38–52) | 34 (23–44) | 75 (67–81) | 70 (62–79) | ||
| Use of insulin (%) | 892 (49.1) | 0 | 2,830 (33.1) | 0 | ||
| Use of oral antidiabetes medications (%) | 1,163 (64.0) | 0 | 6,841 (80.0) | 0 | ||
| Trimethoprim (%) | 773 (42.5) | 63,094 (46.3) | 0.001 | 3,499 (40.9) | 27,573 (43.0) | <0.001 |
| Nitrofurantoin (%) | 847 (46.6) | 64,357 (47.3) | 0.588 | 3,737 (43.7) | 28,239 (44.1) | 0.520 |
| Fosfomycin (%) | 2 (0.1) | 245 (0.2) | 0.484 | 15 (0.2) | 136 (0.2) | 0.483 |
| Norfloxacin (%) | 195 (10.7) | 8,499 (6.2) | <0.001 | 1,298 (15.2) | 8,115 (12,7) | <0.001 |
| Treatment duration ≤5 days | 1,336 (73.5) | 110,024 (80.8) | <0.001 | 5,748 (67.2) | 45,617 (71.2) | <0.001 |
| Treatment duration >5 days | 481 (26.5) | 26,171 (19.2) | <0.001 | 2,801 (32.8) | 18,446 (28.8) | <0.001 |
Data are n (%) or median (25th to 75th percentile).
Table 2—
Recurrence rates and treatment of a recurrent UTI in pre- and postmenopausal women with and without diabetes
| Premenopausal women
|
Postmenopausal women
|
|||||
|---|---|---|---|---|---|---|
| With diabetes | Without diabetes | P value | With diabetes | Without diabetes | P value | |
| n | 1,817 | 136,195 | 8,549 | 64,063 | ||
| Second prescription (%) | 292 (16.1) | 16,586 (12.2) | 0.002 | 1,636 (19.1) | 10,498 (16.4) | <0.001 |
| Hospitalization (%) | 2 (0.1) | 124 (0.1) | 0.790 | 25 (0.3) | 97 (0.2) | 0.003 |
| Trimethoprim (%)* | 53 (18.2) | 3,176 (19.1) | 0.667 | 306 (18.7) | 1,871 (17.8) | 0.387 |
| Nitrofurantoin (%)* | 82 (28.1) | 5,848 (35.3) | 0.011 | 476 (29.1) | 3,153 (30.0) | 0.440 |
| Fosfomycin (%)* | 0 (0.0) | 37 (0.2) | 0.419 | 1 (0.1) | 24 (0.2) | 0.165 |
| Norfloxacin (%)* | 54 (18.5) | 2,449 (14.8) | 0.076 | 351 (21.5) | 2,252 (21.5) | 0.998 |
| Amoxicillin (%)* | 28 (9.6) | 1,603 (9.7) | 0.965 | 112 (6.8) | 664 (6.3) | 0.423 |
| Amoxicillin/clavulanic acid (%)* | 26 (8.9) | 1,192 (7.2) | 0.261 | 129 (7.9) | 716 (6.8) | 0.116 |
| Trimethoprim/sulfamethoxazole (%)* | 22 (7.5) | 1,183 (7.1) | 0.792 | 97 (5.9) | 784 (7.5) | 0.026 |
| Ciprofloxacin (%)* | 17 (5.8) | 783 (4.7) | 0.380 | 120 (7.3) | 774 (7.4) | 0.957 |
| Fluoroquinolones (%)*† | 10 (3.4) | 315 (1.9) | 0.060 | 44 (2.7) | 260 (2.5) | 0.608 |
Data are n (%).
Percentages from second prescription.
Without norfloxacin and ciprofloxacin.
Postmenopausal women
Baseline characteristics of the postmenopausal women are shown in Table 1. Percentage prescriptions with norfloxacin were significantly higher and the treatment duration was significantly longer in postmenopausal patients with diabetes compared with those without. The recurrence rate (Table 2) was significantly higher in postmenopausal women with diabetes: 19.1% in women with and 16.4% in women without diabetes (P < 0.001). There was a significant difference in hospitalization frequency between postmenopausal women with and without diabetes (0.3 vs. 0.2%, P = 0.003). A total of 23 the postmenopausal women with diabetes and 83 without diabetes were hospitalized because they had an infection of the kidneys or other disorder of the urinary tract. In both analyses, the results were similar in age strata.
Secondary analyses
Therapeutic courses given to diabetic (DM+ group) or nondiabetic (DM− group) pre- or postmenopausal women were consistent with the Dutch guidelines (see conclusions) in 71% (premenopausal DM+ women), 79.8% (premenopausal DM− women), 51.8% (postmenopausal DM+ women), and 55.4% (postmenopausal DM− women) of the cases.
General practitioners prescribed 92.0–96.1% of the antimicrobials in all patient groups. When all analyses were repeated with only the prescriptions by the general practitioners, similar results were found. The same was true when all analyses were repeated after excluding patients who were using comedication at the time of the antibiotic prescription.
CONCLUSIONS—
In this study, we found that both pre- and postmenopausal women with diabetes receive longer and more potent antimicrobial treatment for uncomplicated UTIs compared with pre- and postmenopausal women without diabetes. However, despite this more aggressive treatment, both pre- and postmenopausal women with diabetes had more recurrences of their UTIs than women without diabetes. Besides that, hospitalization for complications of the UTI was significantly more often seen in postmenopausal women with diabetes.
The choice for a more potent antibiotic was not to treat a recurrent UTI, since all patients with a UTI in the previous 12 months were excluded. The percentages of women with a recurrent UTI were comparable with the results found by Lawrenson et al. (7), who demonstrated that overall 14% of 75,045 newly treated patients with a UTI (0.7% of all patients had diabetes) received a second antibiotic within 28 days.
The longer prescription period for diabetic patients with an uncomplicated UTI with norfloxacin is not in accordance with the national Dutch guideline in use in the study period. The recommendation in the national Dutch guideline 1999 in use during the study period for an uncomplicated UTI was a 3-day oral antimicrobial regimen with either 100 mg nitrofurantoin three times daily or 300 mg trimethoprim once daily for patients with and without diabetes (11). There were no differences in antimicrobial resistance percentages of causative uropathogens, isolated in the same period as the data of the present study, between women with and without diabetes (12). Treating physicians may have been chosen for longer treatment duration and a more aggresive antibiotic due to the higher risk of complications of UTIs.
Postmenopausal women with diabetes were significantly more often admitted to the hospital than women without diabetes. These results are comparable with those from a Canadian study that demonstrated that patients with diabetes more often had a hospitalization or physician claims for an infectious disease than patients without diabetes (1). However, in contrast to the mortality rate outside the hospital, the mortality rate inside the hospital is not higher in patients with diabetes (1,3). Therefore, it seems possible that physicians refer patients with diabetes faster and treat them more aggressively in the hospital compared with patients without diabetes.
To our knowledge, this is the first study of its kind with this amount of (more than 200,000) patients. In addition, in contrast to most earlier studies in which the recurrence rate of UTIs were described (2,6,7), we also compared the different treatment strategies between women with and without diabetes and analyzed pre- and postmenopausal women separately. The risk factors for UTIs are partly different in pre- and postmenopausal women (13,14), and therefore they should not be regarded as identical entities. Furthermore, it is only possible to interpret the recurrence rates when the initial treatment strategies of the two groups are known.
This study has several limitations. In the first place, it is retrospective and we do not have records on what the reasons of the treating physician were when prescribing a specific antimicrobial agent or a longer treatment duration. It can be possible that diabetic patients more often had symptoms of a UTI with tissue invasion (pyelonephritis or urosepsis) (15,16). We have shown before that only 0.5% of diabetic patients with a UTI had clinical symptoms of a pyelonephritis (17) compared with 0.2% in control subjects. Others have demonstrated that the risk ratio for pyelonephritis in patients with compared with those without diabetes ranges from 1.86 to 4.4 (18,19). These numbers make clear that even when more women with diabetes had clinical symptoms of a pyelonephritis and therefore were treated with norfloxacin during a longer period, this cannot totally explain the demonstrated differences. It therefore seems likely that the physician took diabetes status into account when prescribing antibiotic therapy. Based on drug-dispensing data, we may have missed diabetic women treated with diet and exercise only. On the other hand, we know that many patients with diabetes are not diagnosed (20), so any definition of diabetes in this type of database research has imperfections. Furthermore, it is not possible to distinguish between type 1 and type 2 diabetes because patients in both groups could receive a treatment with insulin. This division is, for this study, not that important because in an earlier study (21) we showed a comparable incidence of UTI in patients with type 1 and type 2 diabetes. Unfortunately, because we did not have urine culture results, we were not able to distinguish between a relapse and a reinfection, which could have influenced the subsequent treatment decision.
Furthermore, because follow-up was only 30 days, it is possible that pregnant women might have been misclassified (delivery after >30 days). Another limitation is that the level of sexual activity was unknown despite the fact that this is an important risk factor for UTI in premenopausal women. However, we do not expect that a higher percentage of pregnant women (and therefore women with a complicated UTI) were included in the diabetic women group or that diabetic women had a higher frequency of sexual intercourse. Moreover, pregnant women with a UTI are mostly treated with amoxicillin/clavulanic acid or a cephalosporin in the Netherlands and therefore would not have been included in this study at all. Therefore, it is unlikely that this possible misclassification or lack of information on risk factors would have influenced our results.
Furthermore, no differences were found after analyzing only the prescriptions of the general practitioners. Another limitation is that women with a recurrence could have underlying anatomical abnormalities like bladder neuropathy. Therefore, we excluded all women who had a UTI in the previous year to minimize this group.
In conclusion, we showed that both pre- and postmenopausal women with diabetes and a UTI receive a more aggressive and longer treatment but still have more recurrences of their UTIs than women without diabetes. Whether therapy with a longer duration or an antibiotic with high tissue penetration contributes to lower recurrence rates needs further investigation. Therefore, a prospective randomized control trial with different treatment strategies must determine which treatment strategy is optimal in diabetic women with a UTI.
Published ahead of print at http://care.diabetesjournals.org on 24 March 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Shah BR, Hux JE: Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care 26:510–513, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Muller LM, Gorter KJ, Hak E: Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis 41:281–288, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Carton JA, Maradona JA, Nuno FJ: Diabetes mellitus and bacteraemia: a comparative study between diabetic and non-diabetic patients. Eur J 1:281–287, Med 1992 [PubMed] [Google Scholar]
- 4.Nicolle LE: Asymptomatic bacteriuria in diabetic women. Diabetes Care 23:722–723, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Nicolle LE: A practical guide to antimicrobial management of complicated urinary tract infection. Drugs 18:243–254, Aging 2001 [DOI] [PubMed] [Google Scholar]
- 6.Goettsch WG, Janknegt R, Herings RM: Increased treatment failure after 3-days' courses of nitrofurantoin and trimethoprim for urinary tract infections in women: a population-based retrospective cohort study using the PHARMO database. Br J Clin Pharmacol 58:184–189, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawrenson RA, Logie JW: Antibiotic failure in the treatment of urinary tract infections in young women. J Antimicrob Chemother 48:895–901, 2001 [DOI] [PubMed] [Google Scholar]
- 8.Carrie AG, Metge CJ, Collins DM, Harding GK, Zhanel GG: Use of administrative healthcare claims to examine the effectiveness of trimethoprim-sulfamethoxazole versus fluoroquinolones in the treatment of community-acquired acute pyelonephritis in women. J Antimicrob Chemother 53:512–517, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Meiland R, Geerlings SE, Hoepelman AI: Management of bacterial urinary tract infections in adult patients with diabetes mellitus. Drugs 62:1859–1868, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Rubenstein JN, Schaeffer AJ: Managing complicated urinary tract infections: the urologic view. Infect Dis Clin North Am 17:333–351, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Timmermans AE, Baselier PJAM, Winkens RAG, Arets H, Wiersma TJ: NHG standaard Urineweginfecties (eerste herziening). Huisarts Wet 42:613–622, 1999 [Google Scholar]
- 12.Meiland R, Geerlings SE, De Neeling AJ, Hoepelman AI: Diabetes mellitus in itself is not a risk factor for antibiotic resistance in Escherichia coli isolated from patients with bacteriuria. Diabet Med 21:1032–1034, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Hooton TM, Scholes D, Hughes JP, Winter C, Roberts PL, Stapleton AE, Stergachis A, Stamm WE: A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med 335:468–474, 1996 [DOI] [PubMed] [Google Scholar]
- 14.Hu KK, Boyko EJ, Scholes D, Normand E, Chen CL, Grafton J, Fihn SD: Risk factors for urinary tract infections in postmenopausal women. Arch Intern Med 164:989–993, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Hoepelman AI, Meiland R, Geerlings SE: Pathogenesis and management of bacterial urinary tract infections in adult patients with diabetes mellitus. Int J Antimicrob Agents 22(Suppl. 2):35–43, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Stapleton A: Urinary tract infections in patients with diabetes. Am J Med 113 (Suppl. 1A):80S–84S, 2002 [DOI] [PubMed] [Google Scholar]
- 17.Geerlings SE, Stolk RP, Camps MJ, Netten PM, Collet JT, Schneeberger PM, Hoepelman AI: Consequences of asymptomatic bacteriuria in women with diabetes mellitus. Arch Intern Med 161:1421–1427, 2001 [DOI] [PubMed] [Google Scholar]
- 18.Nicolle LE: Urinary tract infection in diabetes. Curr Opin Infect Dis 18:49–53, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Scholes D, Hooton TM, Roberts PL, Gupta K, Stapleton AE, Stamm WE: Risk factors associated with acute pyelonephritis in healthy women. Ann Intern Med 142:20–27, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stolk RP, Pols HA, Lamberts SW, de Jong PT, Hofman A, Grobbee DE: Diabetes mellitus, impaired glucose tolerance, and hyperinsulinemia in an elderly population: the Rotterdam Study. Am J Epidemiol 145:24–32, 1997 [DOI] [PubMed] [Google Scholar]
- 21.Geerlings SE, Stolk RP, Camps MJ, Netten PM, Hoekstra JB, Bouter KP, Bravenboer B, Collet JT, Jansz AR, Hoepelman AI: Asymptomatic bacteriuria may be considered a complication in women with diabetes: Diabetes Mellitus Women Asymptomatic Bacteriuria Utrecht Study Group. Diabetes Care 23:744–749, 2000 [DOI] [PubMed] [Google Scholar]