Abstract
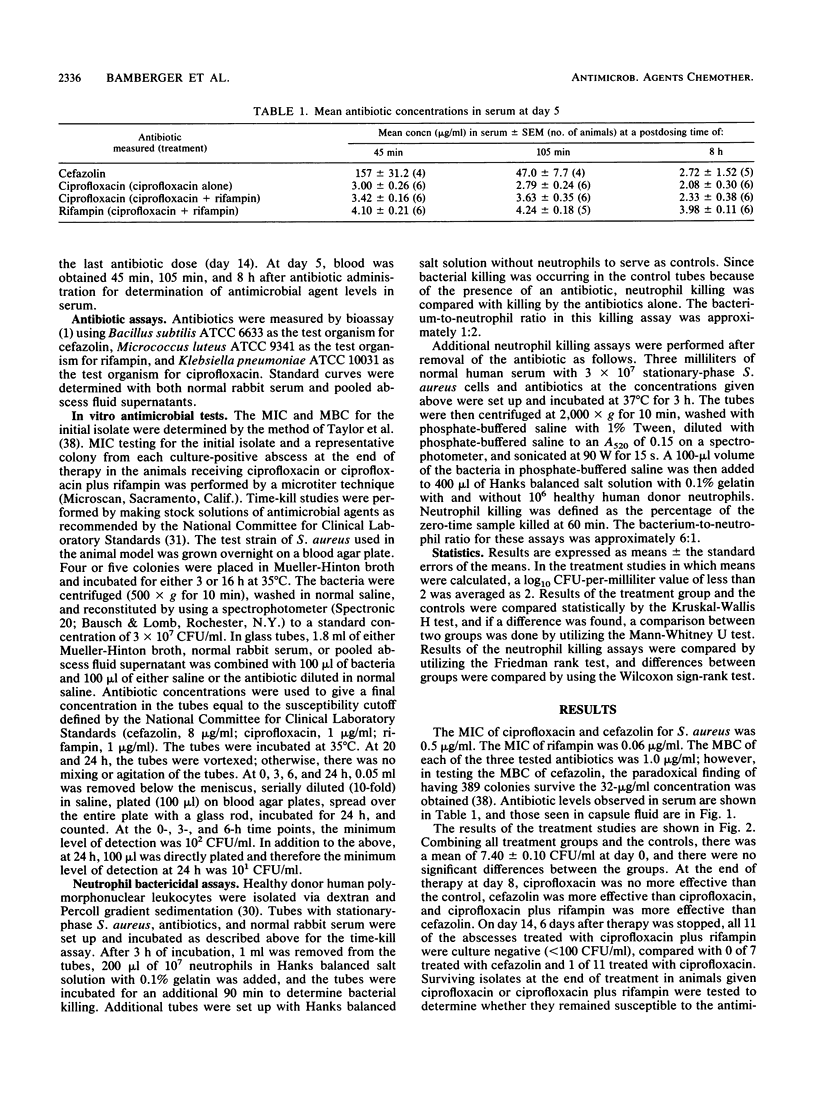
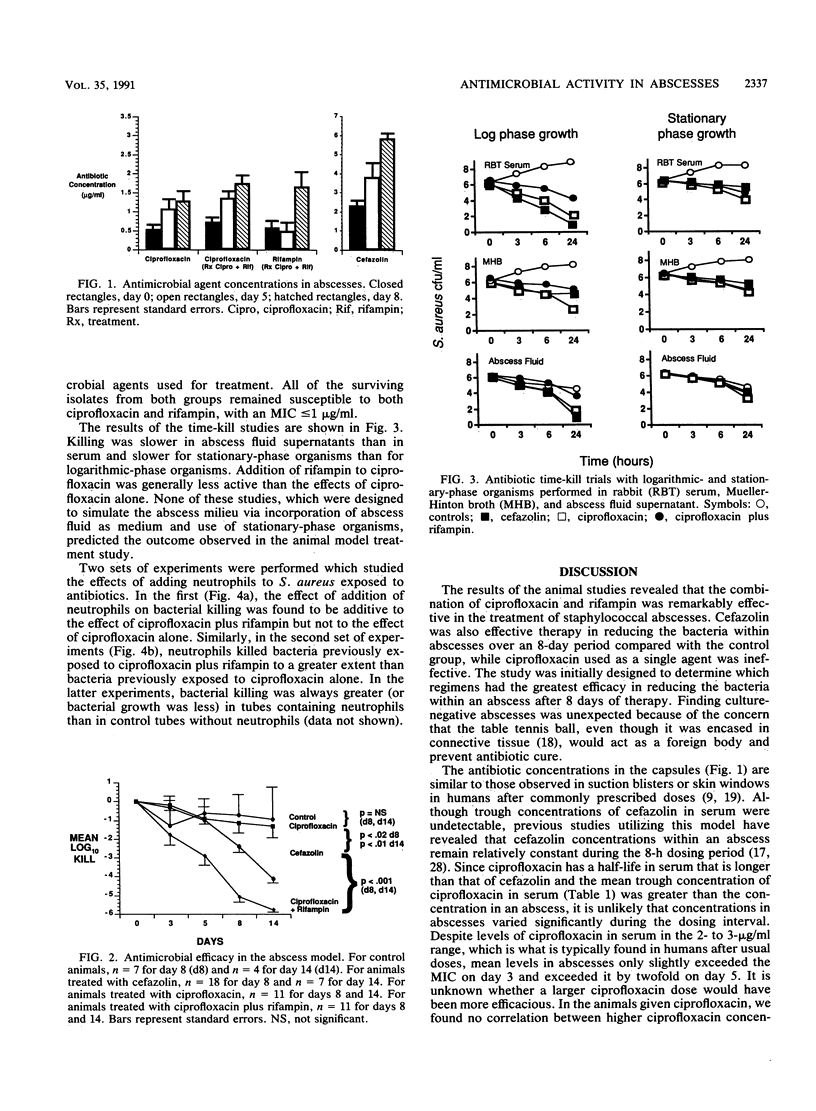
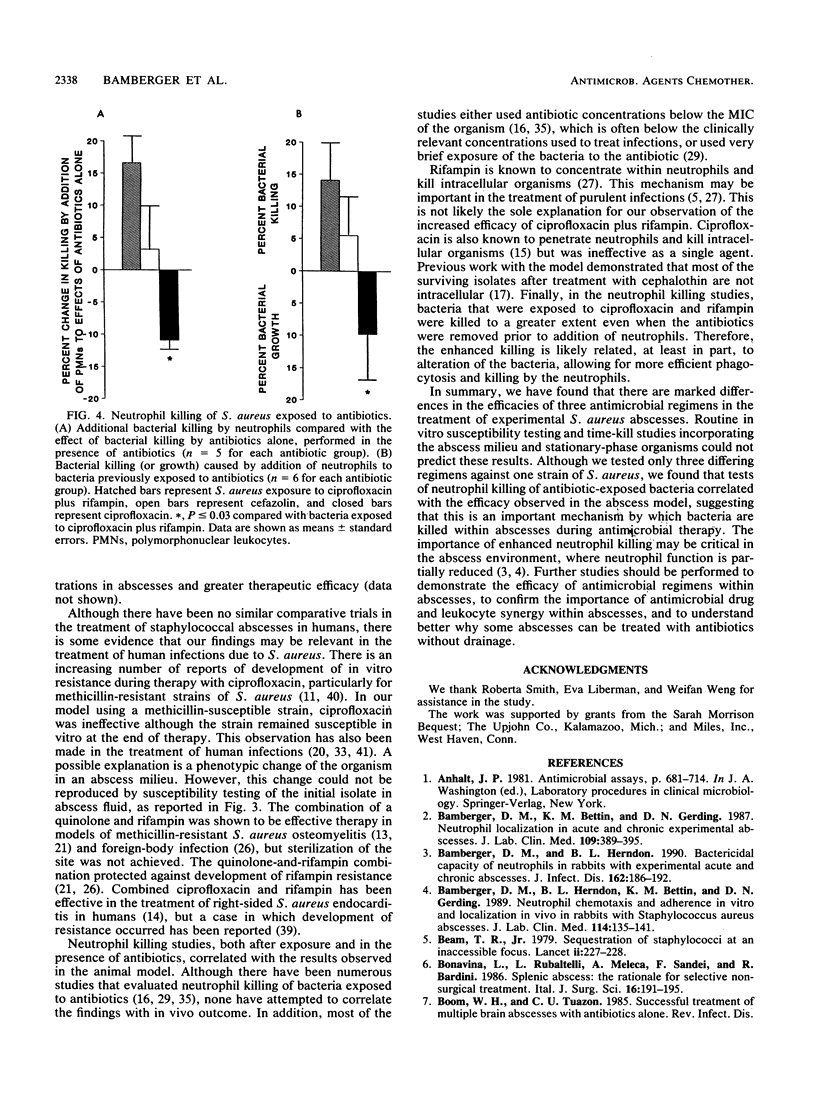
A rabbit perforated-capsule model was utilized to study antimicrobial efficacy in treating 2-week-old Staphylococcus aureus abscesses. Animals received either ciprofloxacin (30 mg/kg), cefazolin (100 mg/kg), or ciprofloxacin (30 mg/kg) plus rifampin (20 mg/kg) every 8 h for 8 days or no antibiotic. Antibiotic levels within the abscess exceeded the MIC for the test organism. At the end of treatment, ciprofloxacin was no more effective than the control, animals receiving cefazolin had a mean log10 fall of 2.41 CFU/ml, and animals receiving ciprofloxacin plus rifampin had a mean log10 reduction of 5.06 CFU/ml (P = less than 0.01). Six days after completion of therapy, all abscesses in animals receiving ciprofloxacin plus rifampin were culture negative. Surviving organisms in animals receiving ciprofloxacin or rifampin did not develop resistance to the treatment antibiotics. In vitro time-kill curves performed with logarithmic- and stationary-phase organisms in broth, serum, and abscess fluid supernatants did not correlate with the in vivo results. Neutrophil killing studies of S. aureus pretreated with antibiotics revealed greater killing of organisms pretreated with ciprofloxacin plus rifampin than of those pretreated with cefazolin or ciprofloxacin alone. In conclusion, ciprofloxacin plus rifampin was effective therapy in this staphylococcal abscess model, compared with the moderate efficacy of cefazolin and no effect observed with ciprofloxacin alone. Enhanced neutrophil killing of S. aureus pretreated with antibiotics may be an important mechanism by which bacteria are killed in suppurative infections.
Full text
PDF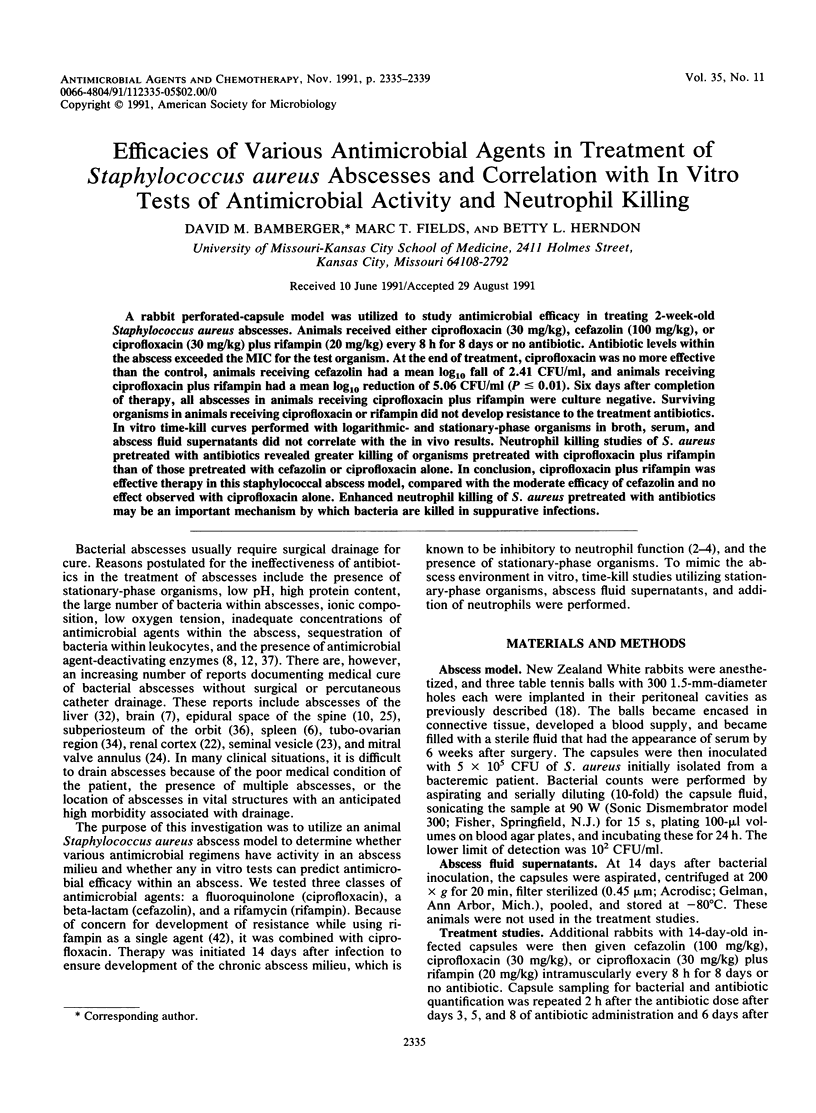
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bamberger D. M., Bettin K. M., Gerding D. N. Neutrophil localization in acute and chronic experimental abscesses. J Lab Clin Med. 1987 Apr;109(4):389–395. [PubMed] [Google Scholar]
- Bamberger D. M., Herndon B. L. Bactericidal capacity of neutrophils in rabbits with experimental acute and chronic abscesses. J Infect Dis. 1990 Jul;162(1):186–192. doi: 10.1093/infdis/162.1.186. [DOI] [PubMed] [Google Scholar]
- Bamberger D. M., Herndon B. L., Bettin K. M., Gerding D. N. Neutrophil chemotaxis and adherence in vitro and localization in vivo in rabbits with Staphylococcus aureus abscesses. J Lab Clin Med. 1989 Aug;114(2):135–141. [PubMed] [Google Scholar]
- Beam T. R., Jr Sequestration of staphylococci at an inaccessible focus. Lancet. 1979 Aug 4;2(8136):227–228. doi: 10.1016/s0140-6736(79)90239-3. [DOI] [PubMed] [Google Scholar]
- Bonavina L., Rubaltelli L., Meleca A., Sandei F., Bardini R. Splenic abscess: the rationale for selective non-surgical treatment. Ital J Surg Sci. 1986;16(3):191–195. [PubMed] [Google Scholar]
- Crump B., Wise R., Dent J. Pharmacokinetics and tissue penetration of ciprofloxacin. Antimicrob Agents Chemother. 1983 Nov;24(5):784–786. doi: 10.1128/aac.24.5.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danner R. L., Hartman B. J. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987 Mar-Apr;9(2):265–274. doi: 10.1093/clinids/9.2.265. [DOI] [PubMed] [Google Scholar]
- Daum T. E., Schaberg D. R., Terpenning M. S., Sottile W. S., Kauffman C. A. Increasing resistance of Staphylococcus aureus to ciprofloxacin. Antimicrob Agents Chemother. 1990 Sep;34(9):1862–1863. doi: 10.1128/aac.34.9.1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin R. J., Lee B. L., Sande M. A., Chambers H. F. Treatment of right-sided Staphylococcus aureus endocarditis in intravenous drug users with ciprofloxacin and rifampicin. Lancet. 1989 Nov 4;2(8671):1071–1073. doi: 10.1016/s0140-6736(89)91083-0. [DOI] [PubMed] [Google Scholar]
- Dworkin R., Modin G., Kunz S., Rich R., Zak O., Sande M. Comparative efficacies of ciprofloxacin, pefloxacin, and vancomycin in combination with rifampin in a rat model of methicillin-resistant Staphylococcus aureus chronic osteomyelitis. Antimicrob Agents Chemother. 1990 Jun;34(6):1014–1016. doi: 10.1128/aac.34.6.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easmon C. S., Crane J. P. Uptake of ciprofloxacin by human neutrophils. J Antimicrob Chemother. 1985 Jul;16(1):67–73. doi: 10.1093/jac/16.1.67. [DOI] [PubMed] [Google Scholar]
- Elliott G. R., Peterson P. K., Verbrugh H. A., Freiberg M. R., Hoidal J. R., Quie P. G. Influence of subinhibitory concentrations of penicillin, cephalothin, and clindamycin on Staphylococcus aureus growth in human phagocytic cells. Antimicrob Agents Chemother. 1982 Nov;22(5):781–784. doi: 10.1128/aac.22.5.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerding D. N., Bean B., Peterson L. R., Moody J., Bettin K. Cephalothin clearance of Staphylococcus aureus from two experimental infection sites in the presence and absence of local phagocytic cells. J Antimicrob Chemother. 1987 Nov;20(5):685–695. doi: 10.1093/jac/20.5.685. [DOI] [PubMed] [Google Scholar]
- Gerding D. N., Hall W. H., Schierl E. A., Manion R. E. Cephalosporin and aminoglycoside concentrations in peritoneal capsular fluid in rabbits. Antimicrob Agents Chemother. 1976 Dec;10(6):902–911. doi: 10.1128/aac.10.6.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg R. N., Wilson K. M., Brusca P. A. Intravenous and oral ciprofloxacin treatment of 52 infections. Am J Med. 1989 Nov 30;87(5A):238S–239S. doi: 10.1016/0002-9343(89)90068-5. [DOI] [PubMed] [Google Scholar]
- Henry N. K., Rouse M. S., Whitesell A. L., McConnell M. E., Wilson W. R. Treatment of methicillin-resistant Staphylococcus aureus experimental osteomyelitis with ciprofloxacin or vancomycin alone or in combination with rifampin. Am J Med. 1987 Apr 27;82(4A):73–75. [PubMed] [Google Scholar]
- Kaver I., Merimsky E., Shilo R., Braf Z. F. Conservative approach in treating acute renal carbuncle. Isr J Med Sci. 1985 Feb;21(2):157–162. [PubMed] [Google Scholar]
- Kennelly M. J., Oesterling J. E. Conservative management of a seminal vesicle abscess. J Urol. 1989 Jun;141(6):1432–1433. doi: 10.1016/s0022-5347(17)41337-1. [DOI] [PubMed] [Google Scholar]
- Kunis R. L., Sherrid M. V., McCabe J. B., Grieco M. H., Dwyer E. M., Jr Successful medical therapy of mitral anular abscess complicating infective endocarditis. J Am Coll Cardiol. 1986 Apr;7(4):953–955. doi: 10.1016/s0735-1097(86)80364-3. [DOI] [PubMed] [Google Scholar]
- Leys D., Lesoin F., Viaud C., Pasquier F., Rousseaux M., Jomin M., Petit H. Decreased morbidity from acute bacterial spinal epidural abscesses using computed tomography and nonsurgical treatment in selected patients. Ann Neurol. 1985 Apr;17(4):350–355. doi: 10.1002/ana.410170408. [DOI] [PubMed] [Google Scholar]
- Lucet J. C., Herrmann M., Rohner P., Auckenthaler R., Waldvogel F. A., Lew D. P. Treatment of experimental foreign body infection caused by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 1990 Dec;34(12):2312–2317. doi: 10.1128/aac.34.12.2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell G. L. The antimicrobial activity of rifampin: emphasis on the relation to phagocytes. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S463–S467. doi: 10.1093/clinids/5.supplement_3.s463. [DOI] [PubMed] [Google Scholar]
- Matsui H., Okuda T. Penetration of cefpiramide and cefazolin into peritoneal capsular fluid in rabbits. Antimicrob Agents Chemother. 1988 Jan;32(1):33–36. doi: 10.1128/aac.32.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald P. J., Wetherall B. L., Pruul H. Postantibiotic leukocyte enhancement: increased susceptibility of bacteria pretreated with antibiotics to activity of leukocytes. Rev Infect Dis. 1981 Jan-Feb;3(1):38–44. doi: 10.1093/clinids/3.1.38. [DOI] [PubMed] [Google Scholar]
- Reynolds T. B. Medical treatment of pyogenic liver abscess. Ann Intern Med. 1982 Mar;96(3):373–374. doi: 10.7326/0003-4819-96-3-373. [DOI] [PubMed] [Google Scholar]
- Righter J. Ciprofloxacin treatment of Staphylococcus aureus infections. J Antimicrob Chemother. 1987 Oct;20(4):595–597. doi: 10.1093/jac/20.4.595. [DOI] [PubMed] [Google Scholar]
- Roberts W., Dockery J. L. Operative and conservative treatment of tubo-ovarian abscess due to pelvic inflammatory disease. South Med J. 1984 Jul;77(7):860–863. doi: 10.1097/00007611-198407000-00018. [DOI] [PubMed] [Google Scholar]
- Root R. K., Isturiz R., Molavi A., Metcalf J. A., Malech H. L. Interactions between antibiotics and human neutrophils in the killing of staphylococci. J Clin Invest. 1981 Jan;67(1):247–259. doi: 10.1172/JCI110020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin S. E., Rubin L. G., Zito J., Goldstein M. N., Eng C. Medical management of orbital subperiosteal abscess in children. J Pediatr Ophthalmol Strabismus. 1989 Jan-Feb;26(1):21–27. doi: 10.3928/0191-3913-19890101-06. [DOI] [PubMed] [Google Scholar]
- Stuart-Harris C. Amantadine--what next? J Antimicrob Chemother. 1978 Jul;4(4):295–297. doi: 10.1093/jac/4.4.295. [DOI] [PubMed] [Google Scholar]
- Taylor P. C., Schoenknecht F. D., Sherris J. C., Linner E. C. Determination of minimum bactericidal concentrations of oxacillin for Staphylococcus aureus: influence and significance of technical factors. Antimicrob Agents Chemother. 1983 Jan;23(1):142–150. doi: 10.1128/aac.23.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebas P., Martinez Ruiz R., Roman F., Mendaza P., Rodriguez Diaz J. C., Daza R., de Letona J. M. Early resistance to rifampin and ciprofloxacin in the treatment of right-sided Staphylococcus aureus endocarditis. J Infect Dis. 1991 Jan;163(1):204–205. doi: 10.1093/infdis/163.1.204-a. [DOI] [PubMed] [Google Scholar]
- Trucksis M., Hooper D. C., Wolfson J. S. Emerging resistance to fluoroquinolones in staphylococci: an alert. Ann Intern Med. 1991 Mar 1;114(5):424–426. doi: 10.7326/0003-4819-114-5-424. [DOI] [PubMed] [Google Scholar]
- Wood M. J., Logan M. N. Ciprofloxacin for soft tissue infections. J Antimicrob Chemother. 1986 Nov;18 (Suppl 500):159–164. doi: 10.1093/jac/18.supplement_d.159. [DOI] [PubMed] [Google Scholar]
- Zak O., Scheld W. M., Sande M. A. Rifampin in experimental endocarditis due to Staphylococcus aureus in rabbits. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S481–S490. doi: 10.1093/clinids/5.supplement_3.s481. [DOI] [PubMed] [Google Scholar]
- de Louvois J. Antimicrobial chemotherapy in the treatment of brain abscess. J Antimicrob Chemother. 1983 Sep;12(3):205–207. doi: 10.1093/jac/12.3.205. [DOI] [PubMed] [Google Scholar]



