Abstract
Background
The ability of office-based functional performance measures to predict mortality in patients with lower extremity peripheral arterial disease (PAD) is unknown. Among persons with PAD, we determined whether objective measures of walking performance predict mortality, independently of the ankle brachial index (ABI).
Methods
Participants were 444 persons with PAD followed prospectively for 4.8 years. The six-minute walk and four-meter walks at usual and fastest pace were measured at baseline. Cox proportional hazard models were used to assess relations between baseline measures of lower extremity performance with mortality, adjusting for confounders.
Results
127 patients (28.6%) died during follow-up. Adjusting for age, sex, race, comorbidities, ABI, and other confounders, participants in the poorest baseline quartile of six-minute walk performance had significantly increased total mortality (hazard ratio (HR) = 2.36 (95% Confidence Interval (CI) = 1.33–4.18)) and cardiovascular mortality ((HR) = 5.59 (95% CI = 1.97–15.9)) compared to the best quartile of baseline performance. Participants in the poorest baseline quartile of normal-paced four meter walking speed had significantly increased total mortality (hazard ratio (HR) = 1.86 (95% CI = 1.06–3.29)) and cardiovascular mortality ((HR) = 2.55 (95% CI = 1.01–6.46)) compared to the best quartile of baseline performance.
Conclusions
This study demonstrates for the first time that performance based measures, which can be administered in an office setting, provide prognostic information regarding mortality in persons with PAD beyond that provided by the ABI.
CONDENSED ABSTRACT
Among 444 persons with lower extremity peripheral arterial disease (PAD), poorer baseline performance on the six-minute walk test and slower baseline walking velocity over four meters were associated with significantly increased all-cause mortality and cardiovascular disease mortality at 4.8 year follow-up, adjusting for the ankle brachial index (ABI), comorbidities, and other confounders. Results indicate that performance based measures, which can be administered in a clinical office setting, provide prognostic information regarding mortality beyond that provided by the ABI among persons with PAD.
Lower extremity peripheral arterial disease (PAD) affects eight million men and women in the United States (U.S.) (1). Men and women with PAD have significantly increased all-cause and cardiovascular mortality rates compared to persons without PAD (2). Among persons with PAD, lower ankle brachial index (ABI) values are associated with increased mortality compared to higher ABI values (3).
In addition, men and women with PAD have poorer performance on objective measures of lower extremity functioning compared to persons without PAD (4–6). Currently, the prognostic significance of functional impairment for total and cardiovascular mortality in persons with PAD is unknown. Therefore, in a prospective observational study, we assessed whether lower extremity performance predicts total and cardiovascular disease mortality in persons with PAD. We hypothesized that among persons with PAD, those with poorer functional performance at baseline would have higher mortality during follow-up, independent of the ABI and other confounders. Associations of functional performance with mortality were also studied in a cohort of participants without PAD, to determine whether associations of functional performance and mortality were similar in persons with vs. without PAD.
Functional performance measures, such as the six-minute walk test and usual walking speed over four meters, are reliable, objective measures of lower extremity functioning that can be administered in the office setting (7,8). They require minimal time and only a stopwatch to administer. If functional performance predicts mortality, then clinicians could potentially use functional performance to identify persons with PAD who are at increased risk for mortality.
METHODS
Participant Identification
The institutional review boards of Northwestern University and Catholic Health Partners Hospital approved the protocol.
Participants gave written informed consent. Participants were part of the Walking and Leg Circulation Study (WALCS) (4,5), a prospective, observational study designed to identify predictors of functional decline and mortality in PAD. Participants with PAD were identified from among consecutive patients age 55 and older in three Chicago-area non-invasive vascular laboratories. Participants without PAD were identified from among consecutive persons with normal lower extremity arterial studies in the three non-invasive vascular laboratories and from a large general internal medicine practice at Northwestern. Median follow-up for this report was 57.7 months (interquartile range 37.5–62.0 months). Participants with PAD had an ABI < 0.90 at their baseline visit. Participants without PAD had an ABI of 0.90 to 1.50. Exclusion criteria have been reported (5). In addition, in the WALCS cohort of 460 participants with PAD and 280 without PAD, four PAD participants who did not undergo baseline functional performance data were excluded. An additional 12 PAD and 8 non-PAD participants were excluded because they had missing data for covariates in our fully adjusted model.
Ankle Brachial Index Measurement
A hand-held Doppler probe (Nicolet Vascular Pocket Dop II; Nicolet Biomedical Inc, Golden, Colo) was used to obtain systolic pressures in the right and left brachial, dorsalis pedis, and posterior tibial arteries (4,5). Each pressure was measured twice. The ABI was calculated by dividing the mean of the dorsalis pedis and posterior tibial pressures in each leg by the mean of the 4 brachial pressures (9). Average brachial pressures in the arm with highest pressure were used when 1 brachial pressure was higher than the opposite brachial pressure in both measurement sets and the 2 brachial pressures differed by 10 mm Hg or more in at least 1 measurement set, since in such cases subclavian stenosis was possible (4,5). Zero values for the dorsalis pedis or posterior tibial vessels (n = 29) were excluded from the ABI calculation. The lowest leg ABI was used in analyses.
Comorbidities
Comorbidities assessed were diabetes, angina, myocardial infarction, heart failure, cancer, chronic lung disease, and stroke. Disease-specific algorithms that combine data from patient report, medical record review, medications, laboratory values, and a questionnaire completed by the participant’s primary care physician were used to verify and document baseline and incident comorbidities, based on criteria previously developed (10).
Other Measures
Body mass index (BMI) was calculated as weight (kilograms)/(height (meters))2. Pack years of cigarette smoking and history of hypertension were determined with patient report.
Functional Measures
Six-Minute Walk
Following a standardized protocol (4,5,11), participants walked up and down a 100-ft hallway for 6 minutes after instructions to cover as much distance as possible.
Repeated chair rises
Participants sit in a straight-backed chair with arms folded across their chest and stand five times consecutively as quickly as possible. Time to complete five chair rises was measured (7,8).
Standing balance
Participants were asked to hold three increasingly difficult standing positions for ten seconds each: standing with feet together side-by-side and parallel (side-by-side stand), standing with feet parallel with the toes of one foot adjacent to and touching the heel of the opposite foot (semi-tandem stand), and standing with one foot directly in front of the other (tandem stand) (7,8).
Four-meter walking velocity
Walking velocity was measured with a four-meter walk performed at “usual” and “fastest” pace (4,5,7,8). For the “usual” paced walk, participants were instructed to walk at their usual pace, “as if going down the street to the store.” Each walk was performed twice. The faster walk in each pair was used in analyses (7,8).
Short Physical Performance Battery
The Short Physical Performance Battery (SPPB) combines data from the usual paced four-meter walking velocity, time to rise from a seated position five times, and standing balance. Individuals receive a zero score for each task they are unable to complete. Scores of one to four are assigned for remaining tasks, based upon quartiles of performance for over 6,000 participants in the Established Populations for the Epidemiologic Study of the Elderly (7,8). Scores are summed to obtain the SPPB, ranging from 0 to 12.
Patient Reported Physical Activity Measures
At the initial visit participants were asked, “During the last week, how many city blocks or their equivalent did you walk? Let 12 city blocks equal one mile.” Participants were also asked, “In the last week, about how many flights of stairs did you climb up? A flight is 10 steps.” Participants were asked to report the number of times they went walking for exercise during the prior week. These measures of patient-reported physical activity have been previously shown to be highly correlated with objectively-assessed physical activity measured with vertical accelerometers (12).
Death
We used the Social Security Administration death database to search for deaths through 6/27/05. At baseline, each participant provided names of three proxies not living with them to assist with ascertaining complete follow-up data. Information on deaths was also obtained from family members, proxies, and primary care physicians. Death certificates were obtained from the State of Illinois or from the patients’ medical record. Cardiovascular disease deaths were those with International Classification of Disease-10 codes in the range I01.0 through I99.9, including deaths due to coronary heart disease, stroke, peripheral vascular disease, and other cardiovascular disease.
Statistical Analyses
Among persons with PAD, baseline characteristics between decedents and survivors were compared using general linear models for continuous variables and chi-square tests for categorical variables, adjusting for age and sex (Table 1). Next, proportional hazards analyses were used to compare differences in all-cause mortality across categories of baseline lower extremity performance. In these proportional hazards analyses, categories of lower extremity performance (independent variables of interest) were defined as follows. Among persons with and without PAD, respectively, performance on the six-minute walk and usual and fast-paced four-meter walking velocity test was categorized into quartiles. The fourth quartile represented best functional performance and the first quartile represented the poorest functional performance. A priori, the baseline SPPB was categorized as follows: category 1 (SPPB = 0–4), category 2 (SPPB = 5–8), category 3 (SPPB = 9–11), category 4 (SPPB = 12). Among participants with and without PAD, respectively, proportional hazards analyses were performed to determine associations of these baseline categories of functional performance with all-cause mortality, adjusting for age and sex. Next, these proportional hazards analyses were repeated with additional adjustment for race, comorbidities (diabetes, angina, myocardial infarction, heart failure, cancer, lung disease, and stroke), cigarette smoking (pack-years), BMI, and ABI (PAD participants only). These fully adjusted proportional hazards analyses were repeated among participants with PAD after excluding deaths during the first year of follow-up and after excluding participants with baseline ABI < 0.40, respectively.
Table 1.
Age and Sex Adjusted Characteristics of Participants with Peripheral Arterial Disease According to Survivor Status*
| All PAD participants (N=444) | Survivors (N=317) | Decedents (N=127) | P value† | |
|---|---|---|---|---|
| African-American Race (%) | 15.5 | 13.4 | 21.0 | 0.058 |
| Ankle brachial index* | 0.65 | 0.66 (0.008) | 0.63 (0.013) | 0.048 |
| Body mass index (kg/m2)* | 27.3 | 27.5 (0.268) | 26.7 (0.427) | 0.119 |
| Cigarette smoking
(pack-years)* |
39.4 | 38.8 (1.90) | 40.7 (3.02) | 0.608 |
| Cardiac or Cerebrovascular diseases (%) | 59.7 | 55.4 | 70.3 | 0.006 |
| Cancer (%) | 16.3 | 13.1 | 24.4 | 0.006 |
| Pulmonary disease (%) | 32.4 | 29.0 | 41.0 | 0.020 |
| Diabetes (%) | 30.7 | 25.7 | 43.3 | 0.001 |
| Number of blocks walked during the past seven days.* | 33.4 | 34.7 (3.13) | 30.0(5.00) | 0.424 |
| Number of stair flights climbed during the past seven days.* | 17.39 | 18.4 (1.50) | 14.8 (2.39) | 0.196 |
For ankle brachial index, body mass index, cigarette smoking, and physical activity levels, values shown are mean and (standard error). Categorical variables are expressed in percentage.
The proportional hazards analyses described above were repeated among participants with and without PAD, respectively, for the dependent variable of cardiovascular mortality. Again, quartiles of baseline performance on the six-minute walk test and the four-meter walking velocity tests (usual and fastest pace) were independent variables of interest for analyses of PAD and non-PAD participants, respectively. Because of few cardiovascular deaths among participants with baseline SPPB scores of 0–4, the lowest (poorest) category for the SPPB in these analyses was defined as SPPB = 0–8. Proportional hazards analyses were performed among persons with and without PAD, respectively, to determine associations of baseline categories of lower extremity performance with cardiovascular disease mortality, adjusting for age and sex. These proportional hazards analyses were repeated with additional adjustment for race, comorbidities (diabetes, angina, myocardial infarction, heart failure, cancer, lung disease, and stroke), cigarette smoking (pack-years), BMI, and ABI (PAD participants only). The causes of 23 out of 127 deaths in participants with PAD and nine of 47 deaths in persons without PAD were unknown because of missing death certificates. We employed multiple imputation methods (ten repeated imputations were used in the analyses) in competing risk analyses to handle the missing cause of death when death certificates were unobtainable (14). Missing data were considered missing at random in that the conditional probability of cardiovascular death among participants with missing death certificates can be modeled using logistic regression with a set of baseline covariates as independent variables. We repeated analyses for cardiovascular mortality first assuming that none of the missing causes of death were due to cardiovascular disease and then assuming that all missing causes of death were due to cardiovascular disease. Analyses were performed using SAS statistical software (version 9.1, SAS Institute Inc, Cary, NC).
RESULTS
Of the 444 PAD participants included in analyses, 127 (28.6%) died during follow-up. Among the PAD participants with known cause of death, 43% were due to cardiovascular disease and 29% were due to cancer. Of the 272 participants without PAD, 47 (17.3%) died during follow-up. Among the non-PAD participants with known cause of death, 36% were due to cardiovascular disease.
The average age of participants was 71.9 ± 8.4 for those with PAD and 69.4 ± 8.1 for those without PAD. Among PAD participants, 40.1% were women, 16.2% were African-American, and 31.5% had diabetes mellitus. Among participants without PAD, 48.2% were women, 18.8% were African-American, and 21.0% had diabetes mellitus.
Table 1 shows baseline characteristics of survivors and decedents with PAD, adjusting for age and sex. Among participants with PAD, survivors were older (74.1 ± 8.78 vs. 71.0 ± 8.03 years, p =0.003) and were likely to be men (68.5% vs. 56.5%, p=0.019) compared to decedents. Decedents had lower ABI values and higher prevalences of cardiac or cerebrovascular diseases, cancer, pulmonary disease, and diabetes.
Functional performance and mortality in persons without peripheral arterial disease
Among participants without PAD, poorer baseline six-minute walk performance was associated significantly with higher all-cause mortality and cardiovascular disease mortality in proportional hazards analyses adjusting for age and sex (P trend =0.03 and 0.01, respectively). Among participants without PAD, there were no other significant associations between baseline functional performance and all-cause or cardiovascular disease mortality either in proportional hazards analyses that adjusted for age and sex or in proportional hazards analyses adjusting for age, sex, race, comorbidities, BMI, and cigarette smoking (data not shown). Results for cardiovascular mortality were similar when the missing causes of death were assumed to be non-cardiovascular disease related, when missing causes of death were all assumed to be due to cardiovascular disease, and when cause of death was imputed for those missing (data not shown). There were no significant interactions between presence vs. absence of PAD and the association of functional performance measures with mortality (data not shown).
Functional performance and mortality in persons with peripheral arterial disease
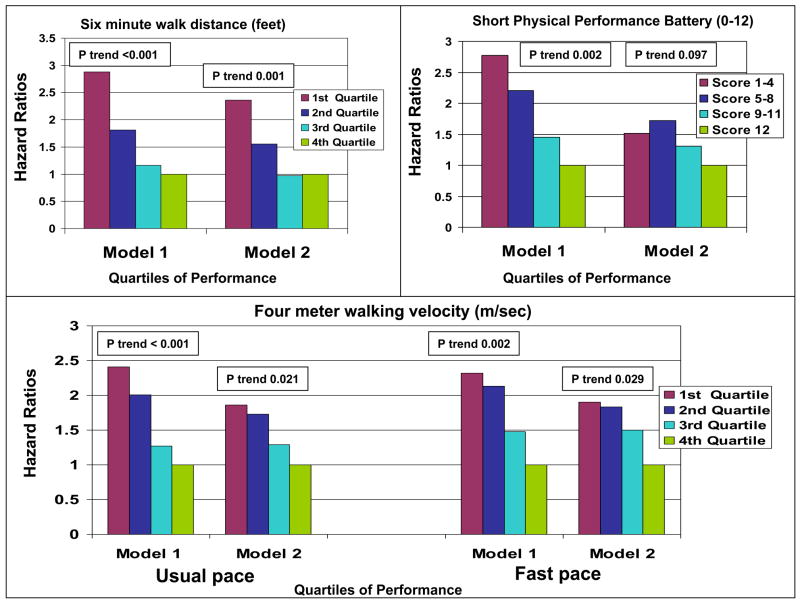
In proportional hazards analyses of PAD participants adjusting for age and sex, significant, linear associations between poorer baseline performance and higher all-cause mortality were observed for the six-minute walk (p trend < 0.001), usual paced four-meter walking velocity (p trend < 0.001), fast paced four-meter walking velocity (p trend =0.002), and the SPPB (p trend =0.002) (Figure 1, Model 1). In proportional hazards analyses of PAD participants adjusting for age, sex, race, ABI, BMI, smoking, and comorbidities, significant, linear associations between poorer baseline performance and higher all-cause mortality were observed for six-minute walk performance (p trend =0.001), usual paced four-meter walking velocity (p trend =0.021), and fast paced four-meter walking velocity (p trend =0.029) (Figure 1, Model II).
Figure 1. Total Mortality.
Associations of functional performance with all-cause mortality among persons with peripheral arterial disease (N = 444).
Model 1- Results of proportional hazards analyses adjusting for age and sex.
Model 2- Results of proportional hazards analyses adjusting for age, sex, race, comorbidities (cardiovascular diseases, pulmonary disease, cancer, and diabetes), body mass index, cigarette smoking history, and the ankle brachial index.
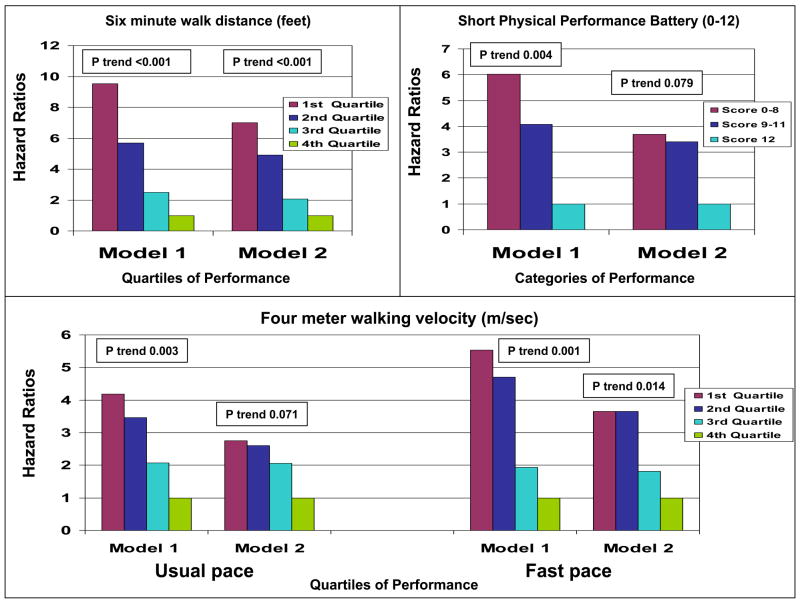
In Cox proportional hazards analyses adjusting for age and sex, significant, linear associations between poorer baseline performance and higher cardiovascular mortality rates were observed for the six-minute walk test (p trend < 0.001), usual paced four-meter walking velocity (p trend = 0.003), fast paced four-meter walking velocity (p trend =0.001), and the SPPB (p trend =0.026) (Figure 2, Model 1). Among PAD participants, associations of poorer six-minute walk performance with greater cardiovascular disease mortality remained statistically significant in Cox proportional hazards analyses adjusting for age, sex, race, ABI, BMI, smoking, diabetes, angina, myocardial infarction, heart failure, cancer, lung disease, and stroke (p trend <0.001). Significant associations of slower fast paced four-meter walking velocity with higher cardiovascular mortality rates were also observed in fully adjusted proportional hazard analyses (p trend = 0.014) (Figure 2, Model 2). Results for cardiovascular mortality were similar when the missing causes of death were all assumed to be non-cardiovascular disease related, when missing causes of death were all assumed to be due to cardiovascular disease, and when cause of death was imputed for those missing (data not shown).
Figure 2. Cardiovascular Disease Mortality.
Associations of functional performance with cardiovascular disease mortality among persons with peripheral arterial disease (N = 444).
Model 1- Results of proportional hazards analyses adjusting for age and sex.
Model 2- Results of proportional hazards analyses adjusting for age, sex, race, comorbidities (cardiovascular diseases, pulmonary disease, cancer, and diabetes), body mass index, cigarette smoking history, and the ankle brachial index.
Because of a small number of cardiovascular deaths in patients with short physical performance battery (SPPB) scores of 0–4, this category was combined with the category of participants with an SPPB of 5–8.
Table 2 shows results of proportional hazards analyses performed to identify associations of functional performance measures with all-cause and cardiovascular disease mortality among persons with PAD, adjusting for physical activity levels in addition to age, sex, race, ABI, BMI, smoking, and comorbidities. Among participants with PAD, associations of poorer six-minute walk performance with higher all-cause and cardiovascular disease mortality remained statistically significant in these analyses that included adjustment for physical activity (Table 2). Associations of slower usual-paced and fast-paced walking velocity with increased all-cause mortality remained statistically significant in these analyses that included adjustment for physical activity (Table 2). Associations of usual and fast-paced four meter walking speed with cardiovascular disease mortality were no longer statistically significant in these proportional hazards analyses that included additional adjustment for physical activity (Table 2).
Table 2.
Associations of functional performance measures with total and cardiovascular mortality among participants with peripheral arterial disease after additional adjustment for physical activity levels*
| Baseline six-minute walk quartiles | Additional adjustment for blocks walked during the past week. | Additional adjustment for stair flights climbed during the past week | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% Confidence Interval) | p- value | p- trend | Hazard Ratio (95% Confidence Interval) | p- value | p- trend | |
| Total Mortality | ||||||
| 1st quartile (<897) | 2.40 (1.32 to 4.38) | 0.004 | 0.001 | 2.33 (1.31 to 4.16) | 0.004 | 0.001 |
| 2nd quartile
(<1158) |
1.57 (0.86 to 2.86) | 0.141 | 1.54 (0.86 to 2.76) | 0.149 | ||
| 3rd quartile
(<1400) |
0.98 (0.53 to 1.81) | 0.951 | 0.97 (0.53 to 1.76) | 0.912 | ||
| 4th quartile
(1400+) |
1.0 (Referent) | NA | 1.0 (Referent) | NA | ||
| Cardiovascular Mortality | ||||||
| 1st quartile (<897) | 5.36 (1.95 to 14.8) | 0.001 | <0.001 | 5.30 (1.79 to 15.7) | 0.003 | <0.001 |
| 2nd quartile
(<1158) |
3.80 (1.40 to 10.3) | 0.009 | 3.82 (1.35 to 10.8) | 0.012 | ||
| 3rd quartile
(<1400) |
1.60 (0.58 to 4.45) | 0.363 | 1.62 (0.57 to 4.60) | 0.369 | ||
| 4th quartile
(1400+) |
1.0 (Referent) | NA | 1.0 (Referent) | NA | ||
| Normal paced four-meter walking velocity | Additional adjustment for blocks walked during the past week. | Additional adjustment for stair flights climbed during the past week. | ||||
| Hazard Ratio (95% Confidence Interval) | p- value | p- trend | Hazard Ratio (95% Confidence Interval) | p- value | p- trend | |
| Total Mortality | ||||||
| 1st quartile (<0.759) | 1.85 (1.04 to 3.29) | 0.037 | 0.025 | 1.87 (1.06 to 3.30) | 0.031 | 0.022 |
| 2nd quartile
(<0.879) |
1.72 (0.99 to 2.97) | 0.054 | 1.73 (1.001 to 2.98) | 0.0497 | ||
| 3rd quartile
(<1.010) |
1.29 (0.72 to 2.32) | 0.400 | 1.32 (0.73 to 2.39) | 0.356 | ||
| 4th quartile
(1.010+) |
1.00 (Referent) | NA | 1.00 (Referent) | NA | ||
| Cardiovascular Mortality | ||||||
| 1st quartile (<0.759) | 2.33 (0.91 to 5.97) | 0.078 | 0.146 | 2.59 (1.04 to 6.44) | 0.041 | 0.139 |
| 2nd quartile
(<0.879) |
2.22 (0.96 to 5.15) | 0.063 | 2.35 (1.01 to 5.44) | 0.046 | ||
| 3rd quartile
(<1.010) |
2.09 (0.91 to 4.80) | 0.081 | 2.33 (1.01 to 5.36) | 0.047 | ||
| 4th quartile
(1.010+) |
1.0 (Referent) | NA | 1.0 (Referent) | NA | ||
| Fast-Paced Four Meter Walking Velocity | Additional adjustment for blocks walked during the past week. | Additional adjustment for stair flights climbed during the past week. | ||||
| Hazard Ratio (95% Confidence Interval) | p- value | p-trend | Hazard Ratio (95% Confidence Interval) | p-value | p-trend | |
| Total Mortality | ||||||
| 1st quartile (<1.034) | 1.88 (1.03 to 3.43) | 0.041 | 0.035 | 1.89 (1.04 to 3.44) | 0.036 | 0.032 |
| 2nd quartile
(<1.223) |
1.82 (1.04 to 3.17) | 0.036 | 1.82 (1.05 to 3.17) | 0.034 | ||
| 3rd quartile
(<1.379) |
1.50 (0.84 to 2.68) | 0.176 | 1.53 (0.85 to 2.74) | 0.156 | ||
| 4th quartile
(1.379+) |
1.0 (Referent) | NA | 1.0 (Referent) | NA | ||
| Cardiovascular Mortality | ||||||
| 1st quartile (<1.034) | 2.29 (0.84 to 6.25) | 0.106 | 0.087 | 2.54 (0.94 to 6.89) | 0.067 | 0.071 |
| 2nd quartile
(<1.223) |
2.40 (0.97 to 5.94) | 0.057 | 2.50 (1.01 to 6.14) | 0.047 | ||
| 3rd quartile
(<1.379) |
1.37 (0.48 to 3.92) | 0.554 | 1.49 (0.51 to 4.36) | 0.470 | ||
| 4th quartile
(1.379+) |
1.0 (Referent) | NA | 1.0 (Referent) | NA | ||
Hazard ratios are shown with (95% confidence intervals). Analyses adjust for age, sex, race, comorbidities, cigarette smoking, body mass index, and the ankle brachial index in addition to the physical activity measures listed at the top of each column.
Because persons with critical limb ischemia have high rates of mortality, proportional hazards analyses among PAD participants were repeated after excluding participants with baseline ABI < 0.40. Again, proportional hazards analyses adjusted for age, sex, race, BMI, ABI, smoking, and comorbidities. Results within this subset of 424 PAD participants were largely unchanged. However, associations of fastest four-meter walking velocity with all-cause and cardiovascular disease mortality were no longer statistically significant in fully adjusted analyses (P trend =0.096 for all-cause mortality, P trend = 0.051 for cardiovascular disease mortality).
Because PAD participants who were ill at baseline were likely to have both poorer functional performance and a higher mortality risk, we repeated proportional hazards analyses after excluding PAD participants who died during the first year of follow-up. Proportional hazards analyses adjusted for age, sex, race, BMI, ABI, smoking, and comorbidities. A similar, significant trend remained between poorer six-minute walk at baseline and increased all-cause mortality (p trend =0.002) and cardiovascular disease mortality (p trend = 0.005), even after excluding individuals who died during the first year of follow-up. In these analyses, the hazard ratio for participants in the lowest vs. highest quartile of six-minute walk performance at baseline was 2.22 [95% CI = 1.21 to 4.09, p=0.010] for all-cause mortality and 3.61 [95% CI = 1.28 to 10.10, p=0.015] for cardiovascular disease mortality.
DISCUSSION
Results reported here show, for the first time, that poorer six-minute walk performance and slower walking velocity identify persons with PAD who are at increased risk for all-cause and cardiovascular mortality. Even after adjustment for confounders including the ABI and comorbidities, poorer six-minute walk performance and slower walking speed at fastest pace remained significantly and independently associated with higher all-cause and cardiovascular disease mortality rates. Similarly, even after adjusting for confounders, slower usual-paced walking speed was associated with higher all-cause mortality rates.
Among participants with PAD, associations of four-meter walking speed with cardiovascular disease mortality were no longer statistically significant after additional adjustment for physical activity levels. This finding suggests that higher physical activity levels among PAD participants with faster four-meter walking speed explained associations of slower four-meter walking speeds with increased rates of cardiovascular mortality.
In contrast to findings for persons with PAD, we did not find significant associations of functional performance measures with mortality in persons without PAD after adjusting for age, sex, race, comorbidities, and other confounders. However, prior large studies of community dwelling men and women without PAD have demonstrated significant associations of slower usual walking speed, poorer SPPB scores, and poorer 400-meter walk performance with higher mortality (7,15). The lack of association of functional performance with mortality in persons without PAD in the WALCS cohort is likely due to the relatively small sample size and fewer deaths in participants without PAD. We did not observe a significant interaction between presence vs. absence of PAD and associations of functional performance with mortality.
Persons with PAD have significantly increased rates of all-cause and cardiovascular disease mortality compared to persons without PAD (2). Clinical practice guidelines for evaluation and management of persons with PAD suggest that the ABI should be used to assess risk of mortality, with lower ABI values being associated with increased risk (16). Results presented here demonstrate that simple measures of lower extremity functional performance provide additional information about mortality risk beyond that provided by the ABI and other confounders. These findings underscore the importance of measuring functional performance in persons with PAD in clinical settings and in research studies including clinical trials. Objective measures of functional performance can be administered by trained health care personnel with minimal time and effort.
Previous studies demonstrate that better performance on objective measures of lower extremity functioning is associated with higher physical activity levels and lower rates of mobility loss in persons with PAD (17,18). Higher levels of physical activity are associated with lower mortality in persons with PAD (12). Results presented here suggest that optimal management of patients with PAD should include efforts to improve functional performance. Previous study demonstrates that supervised walking exercise programs improve six-minute walk performance in persons with PAD and intermittent claudication (19). Based on findings presented here, future study is indicated to determine whether improving functional performance is associated with lower mortality in persons with PAD.
Reasons for the independent associations of functional performance with mortality even after adjusting for mortality risk factors could not be discerned from the data presented here. However, one possible explanation is that the performance measures provide more sensitive information regarding severity of PAD, severity of concomitant cardiovascular disease, and perhaps other unmeasured risk factors compared to the ABI and other clinical characteristics studied.
This study has limitations. First, PAD participants were identified from academic medical centers in Chicago. These findings may not be generalizable to other PAD patients. However, there is no reason to believe that the relationships reported here would not be observed in other PAD populations. Second, death certificates were not obtained for 18.1% of decedents with PAD. However, a statistical imputation method was performed to account for missing causes of death. Findings for our imputation method were similar to those in which participants without a cause of death were excluded from these analyses. Third, the WALCS cohort does not include a measure of renal function, which is a potential confounder of associations reported here.
In conclusion, these findings indicate that simple, objective measures of performance provide prognostic information regarding mortality in persons with PAD that are not available from other clinical data studied. Further study is needed to determine whether interventions that improve functional performance also improve survival among persons with PAD.
Acknowledgments
Supported by R01-HL58099, R01-HL64739, R01-HL071223, and R01-HL076298 from the National Heart Lung and Blood Institute and by grant #RR-00048 from the National Center for Research Resources, National Institutes of Health (NIH). Supported in part by the Intramural Research Program, National Institutes on Aging, NIH.
ABBREVIATIONS
- ABI
Ankle brachial index
- BMI
Body mass index
- PAD
Peripheral arterial disease
- SPPB
Short physical performance battery
- WALCS
Walking and leg circulation study
Footnotes
Conflicts of Interest. There are no conflicts of interest to report.
Financial Disclosures. There are no financial disclosures to report.
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;115:e69–71. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Heald CL, Fowkes FG, Murray GD, Price JF Ankle-brachial index collaboration. Risk of mortality and cardiovascular disease associated with the ankle- brachial index: Systematic review. Atherosclerosis. 2006;189:61–9. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Sikkink CJ, van Asten WN, van’t Hof MA, van Langen H, van der Vliet JA. Decreased ankle/brachial indices in relation to morbidity and mortality in patients with peripheral arterial disease. Vasc Med. 1997;2:169–173. doi: 10.1177/1358863X9700200302. [DOI] [PubMed] [Google Scholar]
- 4.McDermott MM, Greenland P, Liu K, et al. Leg symptoms commonly reported by men and women with lower extremity peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 5.McDermott MM, Greenland P, Liu K, et al. The ankle brachial index as a measure of leg functioning and physical activity in peripheral arterial disease: the walking and leg circulation study. Ann Intern Med. 2002;136:873–83. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- 6.McDermott MM, Fried L, Simonsick E, Ling S, Guralnik JM. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: The Women’s Health and Aging Study. Circulation. 2000;101:1007–1012. doi: 10.1161/01.cir.101.9.1007. [DOI] [PubMed] [Google Scholar]
- 7.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Ferrucci L, Simonsick E, Salive ME, Wallace RB. Lower extremity function in persons over 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDermott MM, Criqui MH, Liu K, et al. The lower ankle brachial index calculated by averaging the dorsalis pedis and posterior tibial arterial pressures is most closely associated with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32:1164–1171. doi: 10.1067/mva.2000.108640. [DOI] [PubMed] [Google Scholar]
- 10.Guralnik JM, Fried LP, Simonsick EM, et al. The Women’s Health and Aging Study: health and social characteristics of older women with disability. Bethesda, MD: National Institute on Aging; 1995. NIH publication 95–4009, Appendix E. [Google Scholar]
- 11.Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46:706–711. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- 12.Garg PK, Tian L, Criqui MH, et al. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006;114:242–248. doi: 10.1161/CIRCULATIONAHA.105.605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 14.Lu K, Tsiatis AA. Multiple imputation methods for estimating regression coefficients in the competing risks model with missing cause of failure. Biometrics. 2001;57:1191–7. doi: 10.1111/j.0006-341x.2001.01191.x. [DOI] [PubMed] [Google Scholar]
- 15.Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 16.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease. Circulation. 2006;113:e463–654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 17.McDermott MM, Greenland P, Ferrucci L, Criqui MH, Liu K, Sharma L, et al. Lower extremity performance is associated with daily life physical activity in individuals with and without peripheral arterial disease. J Am Geriatr Soc. 2002;50:247–255. doi: 10.1046/j.1532-5415.2002.50055.x. [DOI] [PubMed] [Google Scholar]
- 18.McDermott MM, Guralnik JM, Tian L, et al. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol. 2007;50:974–982. doi: 10.1016/j.jacc.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner AW, Katzel LI, Sorkin JD, Bradham DD, Hochberg MC, Flinn Wr, et al. Exercise rehabilitation improves functional outcomes and peripheral circulation in patients with intermittent claudication: A randomized controlled trial. J Am Geriatr Soc. 2001;49:755–62. doi: 10.1046/j.1532-5415.2001.49152.x. [DOI] [PubMed] [Google Scholar]